Submitted:
08 October 2024
Posted:
09 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
- Measure 25(OH)D concentrations and include participants with low concentrations appropriate for the outcome of interest.
- Give a vitamin D dose large enough to raise 25(OH)D concentrations to levels at which beneficial effects are expected.
- Measure achieved 25(OH)D concentrations.
- Analyze results with respect to achieved vitamin D concentrations.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Clarke, R.; Shipley, M.; Lewington, S.; Youngman, L.; Collins, R.; Marmot, M.; Peto, R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol 1999, 150, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Jorde, R.; Sneve, M.; Hutchinson, M.; Emaus, N.; Figenschau, Y.; Grimnes, G. Tracking of serum 25-hydroxyvitamin D levels during 14 years in a population-based study and during 12 months in an intervention study. Am J Epidemiol 2010, 171, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B. Effect of interval between serum draw and follow-up period on relative risk of cancer incidence with respect to 25-hydroxyvitamin D level: Implications for meta-analyses and setting vitamin D guidelines. Dermatoendocrinol 2011, 3, 199–204. [Google Scholar] [CrossRef]
- Grant, W.B. Effect of follow-up time on the relation between prediagnostic serum 25-hydroxyvitamin D and all-cause mortality rate. Dermatoendocrinol 2012, 4, 198–202. [Google Scholar] [CrossRef]
- McCullough, M.L.; Zoltick, E.S.; Weinstein, S.J.; Fedirko, V.; Wang, M.; Cook, N.R.; Eliassen, A.H.; Zeleniuch-Jacquotte, A.; Agnoli, C.; Albanes, D. , et al. Circulating Vitamin D and Colorectal Cancer Risk: An International Pooling Project of 17 Cohorts. J Natl Cancer Inst 2019, 111, 158–169. [Google Scholar] [CrossRef]
- Munoz, A.; Grant, W.B. Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef]
- Zhang, X.X.; Wang, H.R.; Meng, W.; Hu, Y.Z.; Sun, H.M.; Feng, Y.X.; Jia, J.J. Association of Vitamin D Levels with Risk of Cognitive Impairment and Dementia: A Systematic Review and Meta-Analysis of Prospective Studies. J Alzheimers Dis 2024, 98, 373–385. [Google Scholar] [CrossRef]
- Grant, W.B. Follow-up period affects the association between serum 25-hydroxyvitamin D concentration and incidence of dementia, Alzheimer’s disease, and cognitive impairment. Nutrients 2024, 16, 3211. [Google Scholar] [CrossRef] [PubMed]
- Saini, V.; Guada, L.; Yavagal, D.R. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology 2021, 97, S6–S16. [Google Scholar] [CrossRef]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef]
- Tong, T.Y.N.; Appleby, P.N.; Key, T.J.; Dahm, C.C.; Overvad, K.; Olsen, A.; Tjonneland, A.; Katzke, V.; Kuhn, T.; Boeing, H. , et al. The associations of major foods and fibre with risks of ischaemic and haemorrhagic stroke: a prospective study of 418 329 participants in the EPIC cohort across nine European countries. Eur Heart J 2020, 41, 2632–2640. [Google Scholar] [CrossRef] [PubMed]
- Su, C.; Jin, B.; Xia, H.; Zhao, K. Association between Vitamin D and Risk of Stroke: A PRISMA-Compliant Systematic Review and Meta-Analysis. Eur Neurol 2021, 84, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Zhao, C.; Li, J.; Li, Y. A systematic review and meta-analysis of the linkage between low vitamin D and the risk as well as the prognosis of stroke. Brain Behav 2024, 14, e3577. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Cockcroft, J.R.; Elwood, P.C.; Pickering, J.E.; Lovegrove, J.A.; Givens, D.I. Vitamin D intake and risk of CVD and all-cause mortality: evidence from the Caerphilly Prospective Cohort Study. Public Health Nutr 2017, 20, 2744–2753. [Google Scholar] [CrossRef]
- Leu Agelii, M.; Lehtinen-Jacks, S.; Zetterberg, H.; Sundh, V.; Bjorkelund, C.; Lissner, L. Low vitamin D status in relation to cardiovascular disease and mortality in Swedish women - Effect of extended follow-up. Nutr Metab Cardiovasc Dis 2017, 27, 1143–1151. [Google Scholar] [CrossRef]
- Zittermann, A.; Morshuis, M.; Kuhn, J.; Pilz, S.; Ernst, J.B.; Oezpeker, C.; Dreier, J.; Knabbe, C.; Gummert, J.F.; Milting, H. Vitamin D metabolites and fibroblast growth factor-23 in patients with left ventricular assist device implants: association with stroke and mortality risk. Eur J Nutr 2016, 55, 305–313. [Google Scholar] [CrossRef]
- Anderson, J.L.; May, H.T.; Horne, B.D.; Bair, T.L.; Hall, N.L.; Carlquist, J.F.; Lappe, D.L.; Muhlestein, J.B.; Intermountain Heart Collaborative Study, G. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am J Cardiol 2010, 106, 963–968. [Google Scholar] [CrossRef]
- Judd, S.E.; Morgan, C.J.; Panwar, B.; Howard, V.J.; Wadley, V.G.; Jenny, N.S.; Kissela, B.M.; Gutierrez, O.M. Vitamin D deficiency and incident stroke risk in community-living black and white adults. Int J Stroke 2016, 11, 93–102. [Google Scholar] [CrossRef]
- Drechsler, C.; Pilz, S.; Obermayer-Pietsch, B.; Verduijn, M.; Tomaschitz, A.; Krane, V.; Espe, K.; Dekker, F.; Brandenburg, V.; Marz, W. , et al. Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur Heart J 2010, 31, 2253–2261. [Google Scholar] [CrossRef]
- Bolland, M.J.; Bacon, C.J.; Horne, A.M.; Mason, B.H.; Ames, R.W.; Wang, T.K.; Grey, A.B.; Gamble, G.D.; Reid, I.R. Vitamin D insufficiency and health outcomes over 5 y in older women. Am J Clin Nutr 2010, 91, 82–89. [Google Scholar] [CrossRef]
- Perna, L.; Schottker, B.; Holleczek, B.; Brenner, H. Serum 25-hydroxyvitamin D and incidence of fatal and nonfatal cardiovascular events: a prospective study with repeated measurements. J Clin Endocrinol Metab 2013, 98, 4908–4915. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, T.; Kaaks, R.; Teucher, B.; Hirche, F.; Dierkes, J.; Weikert, C.; Katzke, V.; Boeing, H.; Stangl, G.I.; Buijsse, B. Plasma 25-hydroxyvitamin D and its genetic determinants in relation to incident myocardial infarction and stroke in the European prospective investigation into cancer and nutrition (EPIC)-Germany study. PLoS One 2013, 8, e69080. [Google Scholar] [CrossRef] [PubMed]
- Welles, C.C.; Whooley, M.A.; Karumanchi, S.A.; Hod, T.; Thadhani, R.; Berg, A.H.; Ix, J.H.; Mukamal, K.J. Vitamin D deficiency and cardiovascular events in patients with coronary heart disease: data from the Heart and Soul Study. Am J Epidemiol 2014, 179, 1279–1287. [Google Scholar] [CrossRef]
- Afzal, S.; Nordestgaard, B.G. Vitamin D, Hypertension, and Ischemic Stroke in 116 655 Individuals From the General Population: A Genetic Study. Hypertension 2017. [Google Scholar] [CrossRef]
- Marniemi, J.; Alanen, E.; Impivaara, O.; Seppanen, R.; Hakala, P.; Rajala, T.; Ronnemaa, T. Dietary and serum vitamins and minerals as predictors of myocardial infarction and stroke in elderly subjects. Nutr Metab Cardiovasc Dis 2005, 15, 188–197. [Google Scholar] [CrossRef]
- Skaaby, T.; Husemoen, L.L.; Pisinger, C.; Jorgensen, T.; Thuesen, B.H.; Fenger, M.; Linneberg, A. Vitamin D status and incident cardiovascular disease and all-cause mortality: a general population study. Endocrine 2013, 43, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Leung, R.Y.; Han, Y.; Sing, C.W.; Cheung, B.M.; Wong, I.C.; Tan, K.C.; Kung, A.W.; Cheung, C.L. Serum 25-hydroxyvitamin D and the risk of stroke in Hong Kong Chinese. Thromb Haemost 2017, 117, 158–163. [Google Scholar] [CrossRef]
- Berghout, B.P.; Fani, L.; Heshmatollah, A.; Koudstaal, P.J.; Ikram, M.A.; Zillikens, M.C.; Ikram, M.K. Vitamin D Status and Risk of Stroke: The Rotterdam Study. Stroke 2019, 50, 2293–2298. [Google Scholar] [CrossRef] [PubMed]
- Schierbeck, L.L.; Rejnmark, L.; Tofteng, C.L.; Stilgren, L.; Eiken, P.; Mosekilde, L.; Kober, L.; Jensen, J.E. Vitamin D deficiency in postmenopausal, healthy women predicts increased cardiovascular events: a 16-year follow-up study. Eur J Endocrinol 2012, 167, 553–560. [Google Scholar] [CrossRef]
- Sheerah, H.A.; Eshak, E.S.; Cui, R.; Imano, H.; Iso, H.; Tamakoshi, A.; Japan Collaborative Cohort Study, G. Relationship Between Dietary Vitamin D and Deaths From Stroke and Coronary Heart Disease: The Japan Collaborative Cohort Study. Stroke 2018, 49, 454–457. [Google Scholar] [CrossRef]
- Schneider, A.L.; Lutsey, P.L.; Selvin, E.; Mosley, T.H.; Sharrett, A.R.; Carson, K.A.; Post, W.S.; Pankow, J.S.; Folsom, A.R.; Gottesman, R.F. , et al. Vitamin D, vitamin D binding protein gene polymorphisms, race and risk of incident stroke: the Atherosclerosis Risk in Communities (ARIC) study. Eur J Neurol 2015, 22, 1220–1227. [Google Scholar] [CrossRef] [PubMed]
- Kojima, G.; Bell, C.; Abbott, R.D.; Launer, L.; Chen, R.; Motonaga, H.; Ross, G.W.; Curb, J.D.; Masaki, K. Low dietary vitamin D predicts 34-year incident stroke: the Honolulu Heart Program. Stroke 2012, 43, 2163–2167. [Google Scholar] [CrossRef] [PubMed]
- Blood Pressure Lowering Treatment Trialists, C. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 2021, 397, 1625–1636. [Google Scholar] [CrossRef]
- Grandi, N.C.; Breitling, L.P.; Brenner, H. Vitamin D and cardiovascular disease: systematic review and meta-analysis of prospective studies. Prev Med 2010, 51, 228–233. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, P.; Jie, Y.; Sun, Y.; Wang, X.; Fan, Y. Predictive value of 25-hydroxyvitamin D level in patients with coronary artery disease: A meta-analysis. Front Nutr 2022, 9, 984487. [Google Scholar] [CrossRef]
- De Metrio, M.; Milazzo, V.; Rubino, M.; Cabiati, A.; Moltrasio, M.; Marana, I.; Campodonico, J.; Cosentino, N.; Veglia, F.; Bonomi, A. , et al. Vitamin D plasma levels and in-hospital and 1-year outcomes in acute coronary syndromes: a prospective study. Medicine (Baltimore) 2015, 94, e857. [Google Scholar] [CrossRef]
- Beska, B.; Chan, D.; Gu, S.; Qiu, W.; Mossop, H.; Neely, D.; Kunadian, V. The association between vitamin D status and clinical events in high-risk older patients with non-ST elevation acute coronary syndrome undergoing invasive management. PLoS One 2019, 14, e0217476. [Google Scholar] [CrossRef]
- Ng, L.L.; Sandhu, J.K.; Squire, I.B.; Davies, J.E.; Jones, D.J. Vitamin D and prognosis in acute myocardial infarction. Int J Cardiol 2013, 168, 2341–2346. [Google Scholar] [CrossRef]
- Verdoia, M.; Nardin, M.; Rolla, R.; Negro, F.; Gioscia, R.; Afifeh, A.M.S.; Viglione, F.; Suryapranata, H.; Marcolongo, M.; De Luca, G. , et al. Prognostic impact of Vitamin D deficiency in patients with coronary artery disease undergoing percutaneous coronary intervention. Eur J Intern Med 2021, 83, 62–67. [Google Scholar] [CrossRef]
- Wang, T.J.; Pencina, M.J.; Booth, S.L.; Jacques, P.F.; Ingelsson, E.; Lanier, K.; Benjamin, E.J.; D’Agostino, R.B.; Wolf, M.; Vasan, R.S. Vitamin D deficiency and risk of cardiovascular disease. Circulation 2008, 117, 503–511. [Google Scholar] [CrossRef]
- Grandi, N.C.; Breitling, L.P.; Vossen, C.Y.; Hahmann, H.; Wusten, B.; Marz, W.; Rothenbacher, D.; Brenner, H. Serum vitamin D and risk of secondary cardiovascular disease events in patients with stable coronary heart disease. Am Heart J 2010, 159, 1044–1051. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Chen, H.; Zhang, Y.; Li, J.; Fu, K.; Xue, W.; Teng, W.; Tian, L. 25-Hydroxyvitamin D level, vitamin D intake, and risk of stroke: A dose-response meta-analysis. Clin Nutr 2020, 39, 2025–2034. [Google Scholar] [CrossRef]
- Grant, W.B.; Fakhoury, H.M.A.; Karras, S.N.; Al Anouti, F.; Bhattoa, H.P. Variations in 25-Hydroxyvitamin D in Countries from the Middle East and Europe: The Roles of UVB Exposure and Diet. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Rostami, M.; Tehrani, F.R.; Simbar, M.; Bidhendi Yarandi, R.; Minooee, S.; Hollis, B.W.; Hosseinpanah, F. Effectiveness of Prenatal Vitamin D Deficiency Screening and Treatment Program: A Stratified Randomized Field Trial. J Clin Endocrinol Metab 2018, 103, 2936–2948. [Google Scholar] [CrossRef]
- Marti-Soler, H.; Gonseth, S.; Gubelmann, C.; Stringhini, S.; Bovet, P.; Chen, P.C.; Wojtyniak, B.; Paccaud, F.; Tsai, D.H.; Zdrojewski, T. , et al. Seasonal variation of overall and cardiovascular mortality: a study in 19 countries from different geographic locations. PLoS One 2014, 9, e113500. [Google Scholar] [CrossRef] [PubMed]
- Hypponen, E.; Power, C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr 2007, 85, 860–868. [Google Scholar] [CrossRef]
- Kroll, M.H.; Bi, C.; Garber, C.C.; Kaufman, H.W.; Liu, D.; Caston-Balderrama, A.; Zhang, K.; Clarke, N.; Xie, M.; Reitz, R.E. , et al. Temporal relationship between vitamin D status and parathyroid hormone in the United States. PLoS One 2015, 10, e0118108. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Garland, C.F. The association of solar ultraviolet B (UVB) with reducing risk of cancer: multifactorial ecologic analysis of geographic variation in age-adjusted cancer mortality rates. Anticancer Res 2006, 26, 2687–2699. [Google Scholar]
- Garland, C.F.; Gorham, E.D. Dose-response of serum 25-hydroxyvitamin D in association with risk of colorectal cancer: A meta-analysis. J Steroid Biochem Mol Biol 2017, 168, 1–8. [Google Scholar] [CrossRef]
- McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Baggerly, L.L.; Garland, C.F.; Gorham, E.D.; Hollis, B.W.; Trump, D.L.; Lappe, J.M. Breast cancer risk markedly lower with serum 25-hydroxyvitamin D concentrations >/=60 vs <20 ng/ml (150 vs 50 nmol/L): Pooled analysis of two randomized trials and a prospective cohort. PLoS One 2018, 13, e0199265. [Google Scholar] [CrossRef]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D’Agostino, D. , et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med 2019, 380, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Jia, J.; Hu, J.; Huo, X.; Miao, R.; Zhang, Y.; Ma, F. Effects of vitamin D supplementation on cognitive function and blood Abeta-related biomarkers in older adults with Alzheimer’s disease: a randomised, double-blind, placebo-controlled trial. J Neurol Neurosurg Psychiatry 2019, 90, 1347–1352. [Google Scholar] [CrossRef]
- Jamilian, H.; Amirani, E.; Milajerdi, A.; Kolahdooz, F.; Mirzaei, H.; Zaroudi, M.; Ghaderi, A.; Asemi, Z. The effects of vitamin D supplementation on mental health, and biomarkers of inflammation and oxidative stress in patients with psychiatric disorders: A systematic review and meta-analysis of randomized controlled trials. Prog Neuropsychopharmacol Biol Psychiatry 2019, 94, 109651. [Google Scholar] [CrossRef] [PubMed]
- Vellekkatt, F.; Menon, V.; Rajappa, M.; Sahoo, J. Effect of adjunctive single dose parenteral Vitamin D supplementation in major depressive disorder with concurrent vitamin D deficiency: A double-blind randomized placebo-controlled trial. J Psychiatr Res 2020, 129, 250–256. [Google Scholar] [CrossRef]
- Ghaderi, A.; Rasouli-Azad, M.; Farhadi, M.H.; Mirhosseini, N.; Motmaen, M.; Pishyareh, E.; Omidi, A.; Asemi, Z. Exploring the Effects of Vitamin D Supplementation on Cognitive Functions and Mental Health Status in Subjects Under Methadone Maintenance Treatment. J Addict Med 2020, 14, 18–25. [Google Scholar] [CrossRef]
- Castle, M.; Fiedler, N.; Pop, L.C.; Schneider, S.J.; Schlussel, Y.; Sukumar, D.; Hao, L.; Shapses, S.A. Three Doses of Vitamin D and Cognitive Outcomes in Older Women: A Double-Blind Randomized Controlled Trial. J Gerontol A Biol Sci Med Sci 2020, 75, 835–842. [Google Scholar] [CrossRef]
- Rooney, M.R.; Harnack, L.; Michos, E.D.; Ogilvie, R.P.; Sempos, C.T.; Lutsey, P.L. Trends in Use of High-Dose Vitamin D Supplements Exceeding 1000 or 4000 International Units Daily, 1999-2014. JAMA 2017, 317, 2448–2450. [Google Scholar] [CrossRef] [PubMed]
- Alhabeeb, H.; Kord-Varkaneh, H.; Tan, S.C.; Gaman, M.A.; Otayf, B.Y.; Qadri, A.A.; Alomar, O.; Salem, H.; Al-Badawi, I.A.; Abu-Zaid, A. The influence of omega-3 supplementation on vitamin D levels in humans: a systematic review and dose-response meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr 2022, 62, 3116–3123. [Google Scholar] [CrossRef]
- Perez-Lopez, F.R.; Chedraui, P.; Pilz, S. Vitamin D supplementation after the menopause. Ther Adv Endocrinol Metab 2020, 11, 2042018820931291. [Google Scholar] [CrossRef]
- Ikonen, H.; Lumme, J.; Seppala, J.; Pesonen, P.; Piltonen, T.; Jarvelin, M.R.; Herzig, K.H.; Miettunen, J.; Niinimaki, M.; Palaniswamy, S. , et al. The determinants and longitudinal changes in vitamin D status in middle-age: a Northern Finland Birth Cohort 1966 study. Eur J Nutr 2021, 60, 4541–4553. [Google Scholar] [CrossRef]
- Engelsen, O. The relationship between ultraviolet radiation exposure and vitamin D status. Nutrients 2010, 2, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Chalcraft, J.R.; Cardinal, L.M.; Wechsler, P.J.; Hollis, B.W.; Gerow, K.G.; Alexander, B.M.; Keith, J.F.; Larson-Meyer, D.E. Vitamin D Synthesis Following a Single Bout of Sun Exposure in Older and Younger Men and Women. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Crowe, F.L.; Steur, M.; Allen, N.E.; Appleby, P.N.; Travis, R.C.; Key, T.J. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study. Public Health Nutr 2011, 14, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Jorde, R.; Sneve, M.; Emaus, N.; Figenschau, Y.; Grimnes, G. Cross-sectional and longitudinal relation between serum 25-hydroxyvitamin D and body mass index: the Tromso study. Eur J Nutr 2010, 49, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Maghfour, J.; Boothby-Shoemaker, W.; Lim, H.W. Evaluating the USA population’s interest in sunscreen: a Google Trends analysis. Clin Exp Dermatol 2022, 47, 757–759. [Google Scholar] [CrossRef]
- Ngoc, L.T.N.; Tan, V.V.; Moon, J.Y.; Chae, M.; Park, D.; Lee, Y.-C. Recent Trends of Sunscreen Cosmetic: An Update Review. Cosmetics 2019, 6, 64. [Google Scholar] [CrossRef]
- Makariou, S.E.; Michel, P.; Tzoufi, M.S.; Challa, A.; Milionis, H.J. Vitamin D and stroke: promise for prevention and better outcome. Curr Vasc Pharmacol 2014, 12, 117–124. [Google Scholar] [CrossRef]
- Haussler, M.R.; Haussler, C.A.; Jurutka, P.W.; Thompson, P.D.; Hsieh, J.C.; Remus, L.S.; Selznick, S.H.; Whitfield, G.K. The vitamin D hormone and its nuclear receptor: molecular actions and disease states. J Endocrinol 1997, 154 Suppl, S57–73. [Google Scholar]
- Kiraly, S.J.; Kiraly, M.A.; Hawe, R.D.; Makhani, N. Vitamin D as a neuroactive substance: review. ScientificWorldJournal 2006, 6, 125–139. [Google Scholar] [CrossRef]
- Shirvani, A.; Kalajian, T.A.; Song, A.; Holick, M.F. Disassociation of Vitamin D’s Calcemic Activity and Non-calcemic Genomic Activity and Individual Responsiveness: A Randomized Controlled Double-Blind Clinical Trial. Sci Rep 2019, 9, 17685. [Google Scholar] [CrossRef]
- Timms, P.M.; Mannan, N.; Hitman, G.A.; Noonan, K.; Mills, P.G.; Syndercombe-Court, D.; Aganna, E.; Price, C.P.; Boucher, B.J. Circulating MMP9, vitamin D and variation in the TIMP-1 response with VDR genotype: mechanisms for inflammatory damage in chronic disorders? QJM 2002, 95, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Li, X.; Feng, Y.; Dong, G.; Wang, Y.; Yang, J. The Role of Matrix Metalloproteinase-9 in Atherosclerotic Plaque Instability. Mediators Inflamm 2020, 2020, 3872367. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Yu, X.; Ou, S.; Liu, X.; Yuan, J.; Tan, X.; Chen, Y. Adherence to Antihypertensive Medications and Stroke Risk: A Dose-Response Meta-Analysis. J Am Heart Assoc 2017, 6. [Google Scholar] [CrossRef]
- Zhang, Y.; Tan, H.; Tang, J.; Li, J.; Chong, W.; Hai, Y.; Feng, Y.; Lunsford, L.D.; Xu, P.; Jia, D. , et al. Effects of Vitamin D Supplementation on Prevention of Type 2 Diabetes in Patients With Prediabetes: A Systematic Review and Meta-analysis. Diabetes Care 2020, 43, 1650–1658. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, M.; Begerow, B.; Minne, H.W.; Nachtigall, D.; Hansen, C. Effects of a short-term vitamin D(3) and calcium supplementation on blood pressure and parathyroid hormone levels in elderly women. J Clin Endocrinol Metab 2001, 86, 1633–1637. [Google Scholar] [CrossRef]
- Forman, J.P.; Scott, J.B.; Ng, K.; Drake, B.F.; Suarez, E.G.; Hayden, D.L.; Bennett, G.G.; Chandler, P.D.; Hollis, B.W.; Emmons, K.M. , et al. Effect of vitamin D supplementation on blood pressure in blacks. Hypertension 2013, 61, 779–785. [Google Scholar] [CrossRef]
- Sluyter, J.D.; Camargo, C.A., Jr.; Stewart, A.W.; Waayer, D.; Lawes, C.M.M.; Toop, L.; Khaw, K.T.; Thom, S.A.M.; Hametner, B.; Wassertheurer, S. , et al. Effect of Monthly, High-Dose, Long-Term Vitamin D Supplementation on Central Blood Pressure Parameters: A Randomized Controlled Trial Substudy. J Am Heart Assoc 2017, 6. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Vatanparast, H.; Kimball, S.M. The Association between Serum 25(OH)D Status and Blood Pressure in Participants of a Community-Based Program Taking Vitamin D Supplements. Nutrients 2017, 9. [Google Scholar] [CrossRef]
- Latic, N.; Erben, R.G. Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure. Int J Mol Sci 2020, 21. [Google Scholar] [CrossRef]
- Della Nera, G.; Sabatino, L.; Gaggini, M.; Gorini, F.; Vassalle, C. Vitamin D Determinants, Status, and Antioxidant/Anti-inflammatory-Related Effects in Cardiovascular Risk and Disease: Not the Last Word in the Controversy. Antioxidants (Basel) 2023, 12. [Google Scholar] [CrossRef]
- Marek, K.; Cichon, N.; Saluk-Bijak, J.; Bijak, M.; Miller, E. The Role of Vitamin D in Stroke Prevention and the Effects of Its Supplementation for Post-Stroke Rehabilitation: A Narrative Review. Nutrients 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Meza, C.A.; Clarke, H.; Kim, J.S.; Hickner, R.C. Vitamin D and Endothelial Function. Nutrients 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Contreras-Bolivar, V.; Garcia-Fontana, B.; Garcia-Fontana, C.; Munoz-Torres, M. Mechanisms Involved in the Relationship between Vitamin D and Insulin Resistance: Impact on Clinical Practice. Nutrients 2021, 13. [Google Scholar] [CrossRef]
- Surdu, A.M.; Pinzariu, O.; Ciobanu, D.M.; Negru, A.G.; Cainap, S.S.; Lazea, C.; Iacob, D.; Saraci, G.; Tirinescu, D.; Borda, I.M. , et al. Vitamin D and Its Role in the Lipid Metabolism and the Development of Atherosclerosis. Biomedicines 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Yarlagadda, K.; Ma, N.; Dore, S. Vitamin D and Stroke: Effects on Incidence, Severity, and Outcome and the Potential Benefits of Supplementation. Front Neurol 2020, 11, 384. [Google Scholar] [CrossRef]
- Legarth, C.; Grimm, D.; Kruger, M.; Infanger, M.; Wehland, M. Potential Beneficial Effects of Vitamin D in Coronary Artery Disease. Nutrients 2019, 12. [Google Scholar] [CrossRef]
- de la Guia-Galipienso, F.; Martinez-Ferran, M.; Vallecillo, N.; Lavie, C.J.; Sanchis-Gomar, F.; Pareja-Galeano, H. Vitamin D and cardiovascular health. Clin Nutr 2021, 40, 2946–2957. [Google Scholar] [CrossRef]
- Dawson-Hughes, B.; Staten, M.A.; Knowler, W.C.; Nelson, J.; Vickery, E.M.; LeBlanc, E.S.; Neff, L.M.; Park, J.; Pittas, A.G.; Group, D.d.R. Intratrial Exposure to Vitamin D and New-Onset Diabetes Among Adults With Prediabetes: A Secondary Analysis From the Vitamin D and Type 2 Diabetes (D2d) Study. Diabetes Care 2020, 43, 2916–2922. [Google Scholar] [CrossRef]
- Nudy, M.; Krakowski, G.; Ghahramani, M.; Ruzieh, M.; Foy, A.J. Vitamin D supplementation, cardiac events and stroke: A systematic review and meta-regression analysis. Int J Cardiol Heart Vasc 2020, 28, 100537. [Google Scholar] [CrossRef]
- Cui, P.; Hou, H.; Song, B.; Xia, Z.; Xu, Y. Vitamin D and ischemic stroke - Association, mechanisms, and therapeutics. Ageing Res Rev 2024, 96, 102244. [Google Scholar] [CrossRef]
- Heaney, R.P. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr Rev 2014, 72, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Boucher, B.J.; Bhattoa, H.P.; Lahore, H. Why vitamin D clinical trials should be based on 25-hydroxyvitamin D concentrations. J Steroid Biochem Mol Biol 2018, 177, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; Trummer, C.; Theiler-Schwetz, V.; Grubler, M.R.; Verheyen, N.D.; Odler, B.; Karras, S.N.; Zittermann, A.; Marz, W. Critical Appraisal of Large Vitamin D Randomized Controlled Trials. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Grant, W.B.; Boucher, B.J.; Al Anouti, F.; Pilz, S. Comparing the Evidence from Observational Studies and Randomized Controlled Trials for Nonskeletal Health Effects of Vitamin D. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Wang, L.; Song, Y.; Manson, J.E.; Pilz, S.; Marz, W.; Michaelsson, K.; Lundqvist, A.; Jassal, S.K.; Barrett-Connor, E.; Zhang, C. , et al. Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: a meta-analysis of prospective studies. Circ Cardiovasc Qual Outcomes 2012, 5, 819–829. [Google Scholar] [CrossRef]
- Palacios, C.; Kostiuk, L.L.; Cuthbert, A.; Weeks, J. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev 2024, 7, CD008873. [Google Scholar] [CrossRef]
- Hill, A.B. The Environment and Disease: Association or Causation? Proc R Soc Med 1965, 58, 295–300. [Google Scholar] [CrossRef]
- Potischman, N.; Weed, D.L. Causal criteria in nutritional epidemiology. Am J Clin Nutr 1999, 69, 1309S–1314S. [Google Scholar] [CrossRef] [PubMed]
- Lesko, C.R.; Fox, M.P. An evolved interpretation of Austin Bradford Hill’s causal viewpoints and their influence on epidemiologic methods. Am J Epidemiol 2024. [Google Scholar] [CrossRef]
- Weyland, P.G.; Grant, W.B.; Howie-Esquivel, J. Does sufficient evidence exist to support a causal association between vitamin D status and cardiovascular disease risk? An assessment using Hill’s criteria for causality. Nutrients 2014, 6, 3403–3430. [Google Scholar] [CrossRef]
- Barbarawi, M.; Kheiri, B.; Zayed, Y.; Barbarawi, O.; Dhillon, H.; Swaid, B.; Yelangi, A.; Sundus, S.; Bachuwa, G.; Alkotob, M.L. , et al. Vitamin D Supplementation and Cardiovascular Disease Risks in More Than 83 000 Individuals in 21 Randomized Clinical Trials: A Meta-analysis. JAMA Cardiol 2019, 4, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Quan, Q.L.; Yoon, K.N.; Lee, J.S.; Kim, E.J.; Lee, D.H. Impact of ultraviolet radiation on cardiovascular and metabolic disorders: The role of nitric oxide and vitamin D. Photodermatol Photoimmunol Photomed 2023, 39, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Pludowski, P.; Kos-Kudla, B.; Walczak, M.; Fal, A.; Zozulinska-Ziolkiewicz, D.; Sieroszewski, P.; Peregud-Pogorzelski, J.; Lauterbach, R.; Targowski, T.; Lewinski, A. , et al. Guidelines for Preventing and Treating Vitamin D Deficiency: A 2023 Update in Poland. Nutrients 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Ekwaru, J.P.; Zwicker, J.D.; Holick, M.F.; Giovannucci, E.; Veugelers, P.J. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One 2014, 9, e111265. [Google Scholar] [CrossRef]
| Follow-up (yrs) | Type of stroke | Inc or mor | OR/RR (95% CI) | 25(OH)D comparison (ng/mL) | Ref. |
| NA | 1.41 (0.64‒3.13) | Guo 2017* [14] | |||
| NA | 1.19 (0.79‒1.79) | Leu Agelii 2017* [15] | |||
| 1 | Inc | 0.42 (0.14‒1.28) | ≥10 vs. <10 | Zittermann 2016 [16] | |
| 1.3 | Inc | 0.56 (0.38‒0.84) | >30 vs. ≤15 | Anderson 2010 [17] | |
| 3.1 | Inc | 0.54 (0.34‒0.85) | >30 vs. <20 | Judd 2016 [18] | |
| 4 | Inc | 0.33 (0.15‒0.73) | >30 vs. ≤10 | Drechsler 2010 [19] | |
| 5 | Inc | 0.71 (0.40‒1.25) | ≥20 vs. <20 | Bolland 2010 [20] | |
| 6.8 | Inc + mor | 0.91 (0.81‒1.02) | per +10* | Perna 2013 [21] | |
| 0.76 (0.55‒1.05) | <12 vs. ≥20 | ||||
| 7.6 | Inc | 0.60 (0.59‒1.09) | Q4 (27 median) vs. Q1 (12 median)* |
Kuhn 2013 [22] | |
| 0.65 (0.44‒0.95) | ≥20 vs. <10 | ||||
| 8.0 | Inc | 0.93 (0.46‒1.85) | ≥20 vs. <20 | Welles 2014 [23] | |
| 9.3 | I | Inc | 0.81 (0.70‒0.94) | ≥20 vs. <10 | Afzal 2017 [24] |
| 10 | Inc + mor | 1.00 (0.51‒1.94) | High vs. low tertile | Marniemi 2005 [25] | |
| 0.88 (0.49‒1.61) | Middle vs. low tertile | ||||
| 10 | Inc | 1.13 (0.80‒1.59) | Fourth vs. first quartile | Skaaby 2013 [26] | |
| 10.3 | All | Inc | 0.56 (0.36‒0.86) | Lowest vs. highest quintile | Leung 2017 [27] |
| I | 0.55 (0.35‒0.86) | Middle vs. highest quintile | |||
| 10.6 | Inc | 0.91 (0.75‒1.11) | One 25(OH)D SD increase | Berghout 2019 [28] | |
| 16 | Inc or mor | 0.60 (0.39‒0.91) | ≥20 vs. <20 | Schierbeck 2012 [29] | |
| 19.3 | 0.66 (0.49‒0.89) | >440 vs. <110 IU/day vitamin D |
Sheerah 2018* [30] | ||
| 20 | Inc | 0.75 (0.58‒0.94) | ≥31 vs. <17 | Schneider 2015 [31] | |
| 34 | 0.82 (0.68‒0.99) | >4 vs. <1.1 µg/day | Kojima 2012* [32] |
| Country | Patient characteristics | Mean age (± SD) or range (yrs) | BMI (± SD) (kg/m2) | M, F (%) | Stroke type | NS | NC | Ref. |
| Germany | Left ventricular assist device implants | 62 (37‒81) | 23 ± 3 | 100, 0 | All | 25 | Zittermann 2016 [16] | |
| 57 (49‒66) | 26 ± 5 | 85, 15 | 129 | |||||
| USA | Community hospital | 55 ± 21 | NA | 25, 75 | All | 208 | 25,818 | Anderson 2010 [17] |
| USA | B and W community dwellers | I | 536 | 1069 | Judd 2016 [18] | |||
| Germany | Diabetic and on hemodialysis | 66 ± 8 | 60, 40 | All | 89 | 1019 | Drechsler 2010 [19] | |
| New Zealand | Healthy community-dwelling | 74 ± 4 | NA | 0, 100 | All | 59 | 1412 | Bolland 2010 [20] |
| Germany | Population-based | 65% 50‒65; 35% 65‒74 | 27 ± 5 | 41, 59 | All | 353 | 7356 | Perna 2013 [21] |
| Germany | Population-based | 51 | NA | 42, 58 | All | 471 | 1661 | Kuhn 2013 [22] |
| USA | Stable CVD | 66 ± 11 | 29 | 81, 19 | All | 49 | 897 | Welles 2014 [23] |
| Denmark | General population | 58 (48‒68) | 26 ± 3 | 48, 52 | I | 960 | ~115,000 | Afzal 2017 [24] |
| Finland | Population-based | 65-99 | NA | 48, 52 | All | 70 | 685 | Marniemi 2005 [25] |
| Denmark | General population | 49 (41–73) | 26 | 50, 50 | All | 316 | 8830 | Skaaby 2013 [26] |
| Hong Kong | Osteoporosis study, Chinese | 63 ± 10 |
37, 63 | All | 244 | 3214 | Leung 2017 [27] | |
| I | 205 | 3253 | ||||||
| Netherlands | Population-based | 65 ± 10 | 27 ± 4 | 43, 57 | All | 735 | 8603 | Berghout 2019 [28] |
| Denmark | Osteoporosis study | 50 ± 2 | 25 ± 5 | 0, 100 | All | 89 | 1924 | Schierbeck 2012 [29] |
| USA | Population-based | 57 | NA | 43, 57 | All | 804 | 11,354 | Schneider 2015 [31] |
| Follow-up (yrs) | RR (95% CI) | 25(OH)D comparison (ng/mL) |
Ref. |
| 1.0 | 1.85 (1.25‒2.75) | <9 vs. >9 | de Metrio 2015 [36] |
| 1.0 | 1.20 (0.72‒2.00) | <12 vs. >12 | Beska 2019 [37] |
| 1.5 | 1.61 (1.15‒2.27) | <7.3 vs. >7.3 | Ng 2013 [38] |
| 2.7 | 1.32 (1.07‒1.63) | <12.7; 12.7-21.59; ≥21.6 | Verdoia 2021 [39] |
| 5 | 1.2 (0.7‒2.2) | <20 vs. ≥20 | Bolland 2010 [20] |
| 7.6 | 1.62 (1.11‒2.36) | <15 vs. >15 | Wang 2008 [40] |
| 8.0 | 1.11 (0.85‒1.44) | ≥20 vs. <20 | Welles 2014 [23] |
| 8.1 | 0.83 (0.37‒1.86) | Quartiles | Grandi 2010 [41] |
| Country | Patient characteristics | Mean Age (± SD) or range (yrs) |
BMI (± SD) (kg/m2) | M, F (%) | Type of event | NMCDE | NC | Ref. |
| Italy | ACS | 67 ± 12 | 27 ± 4 | 72, 28 | MCE | 125 | 689 | de Metrio 2015 [36] |
| UK | After non–ST elevation ACS | 81 ± 5 | 27 ± 5 | 62, 38 | MCE | 76 | 224 | Beska 2019 [37] |
| UK | Acute MI | 66 ± 13 | NA | 72, 28 | Nonfatal MCE | 224 | 1035 | Ng 2013 [38] |
| Italy | CAD undergoing percutaneous coronary intervention | 68 ± 11 | 28 ± 5 | 73, 27 | MCE | 174 | 531 | Verdoia 2021 [39] |
| New Zealand | Healthy community-dwelling | 74 ± 4 | NA | 0, 100 | MI | 52 | 1419 | Bolland 2010 [20] |
| USA | General population | Incident CVD | Wang 2008 [40] | |||||
| USA | Stable CVD | 66 ± 11 | 29 | 81, 19 | CVD events | 49 | 897 | Welles 2014 [23] |
| Germany | Stable CHD | CVD events | 148 | 977 | Grandi 2010 [41] |
| Participants | Duration (wks) |
Condition | Intervention | Outcomes | Ref. |
| Meta-analysis of 9 clinical trials, China and Iran | 8‒52 | Mental health | 50,000 IU/wk or 2 wks or higher single dose | Beck Depression Inventory, weighted mean difference, –3.9 (95% CI, –5.2 to –2.7) | [53] |
| 46 patients, India; baseline 25(OH)D: N/A |
12 | Major depressive disorder | Usual treatment or usual treatment plus 3 million IU of vitamin D | Significantly greater improvement in depression score with vitamin D than placebo; also quality of life. | [54] |
| 64 patients under methadone maintenance treatment, Iran. Baseline 25(OH)D: 14 ± 4 ng/mL | 24 | Cognitive function | 50,000 IU or placebo/2 wks | Vitamin D treatment resulted in significant improvement in Iowa Gambling Task, Verbal Fluency Test, Reverse Digit Span, and visual working memory. | [55] |
| 42 women, USA mean age 58 ± 6 years, BMI, 30.0 ± 3.5 kg/m2; baseline 25(OH)D: 23 ± 6 ng/mL | 52 | Cognitive outcome | 600, 2000, or 4000 IU/day of vitamin D3 | 2000-IU/day group had improved visual and working memory and learning; the 4000-IU/day group had slower attention reaction time. | [56] |
| Reason | Ref. |
| For increases in 25(OH)D concentrations | |
| Increased awareness of overall benefits of vitamin D | [57] |
| Increase amount of omega-3 fatty acid supplementation | [58] |
| Increased vitamin D supplementation after menopause | [59] |
| Vitamin D fortification of food instituted countrywide | [60] |
| For variable changes in 25(OH)D concentrations | |
| Change geographic location | [61] |
| Retire from work | |
| Change in physical activity | [2] |
| Change in season from winter/spring to summer/autumn | [46,47] |
| For reductions in 25(OH)D concentrations | |
| Decline with age due to reduced production from solar UVB | [62] |
| Change in diet with reduced meat, fish consumption | [63] |
| Increase in body mass | [64] |
| Increase in use of sunscreen/sunblock, clothing when in sunlight | [65] |
| Increased use of sunscreen in cosmetics | [66] |
| Moving into residential care |
| Mechanism | Ref. |
| Antifibrotic, antihypertrophic signaling | [79] |
| Anti-inflammatory, antioxidant effects | [80] |
| Atherosclerosis progression reduction | [81] |
| Reduces arterial stiffness and narrowing of the vessel lumen due to activation of the renin–angiotensin–aldosterone system | [81] |
| Cellular effects through effects on genes (cell cycle, proliferation, apoptosis, and angiogenesis) | [81] |
| Endothelial function maintenance | [82] |
| Insulin resistance risk reduction | [83] |
| Lipid metabolism regulation | [84] |
| MMP-2 and MMP-9 activity reduced, which reduces acute arterial event risk | [71,72] |
| Neuroprotective growth factor promotion | [85] |
| Reduced risk of plaque instability and acute arterial events | [86] |
| Reduction of blood pressure through vasodilation | [85] |
| Reduction of arterial pressure through effects on endothelial and muscle cells | [87] |
| Type 2 diabetes mellitus risk reduction | [88] |
| Criterion | Strength of finding | Ref. |
|---|---|---|
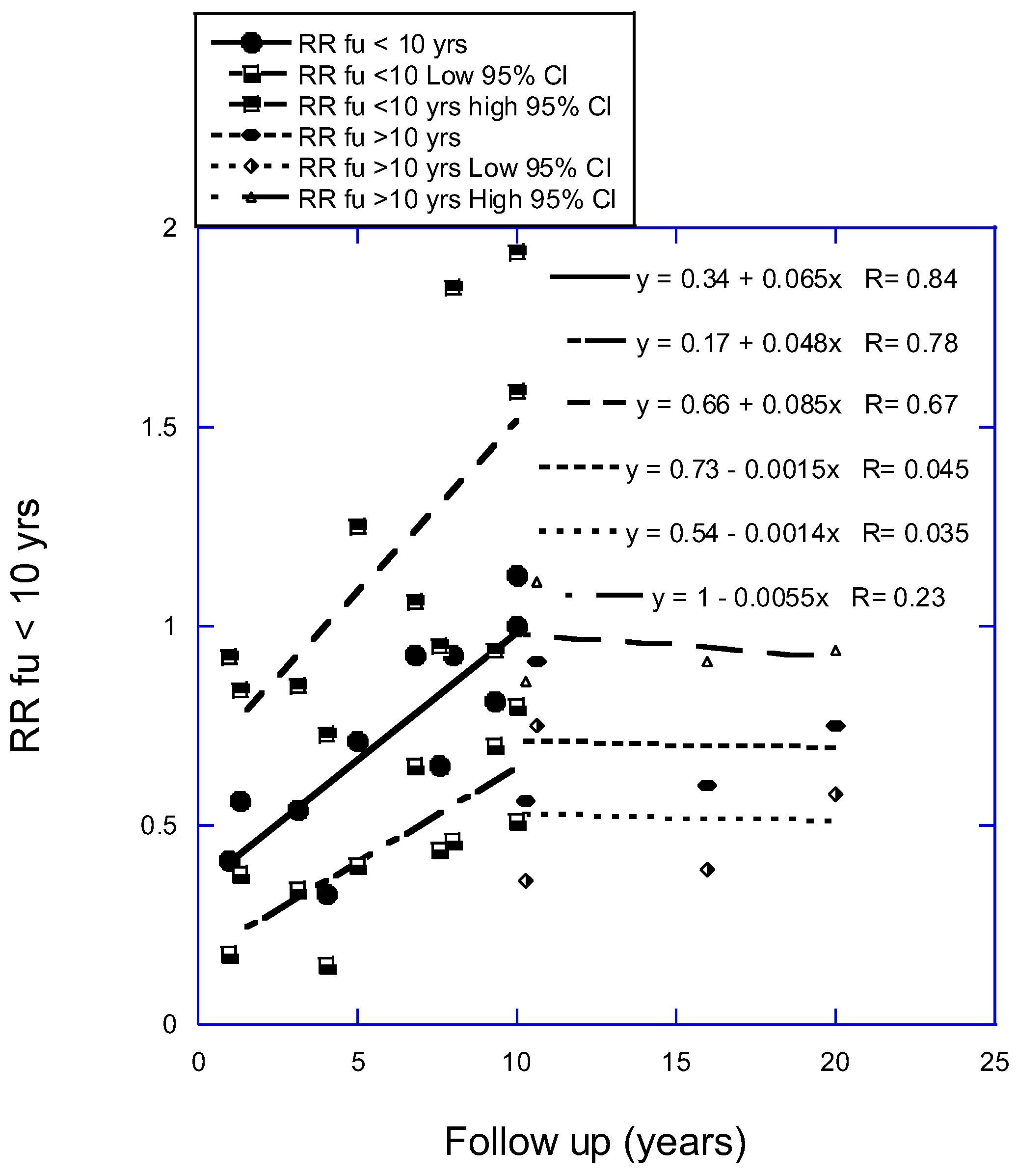
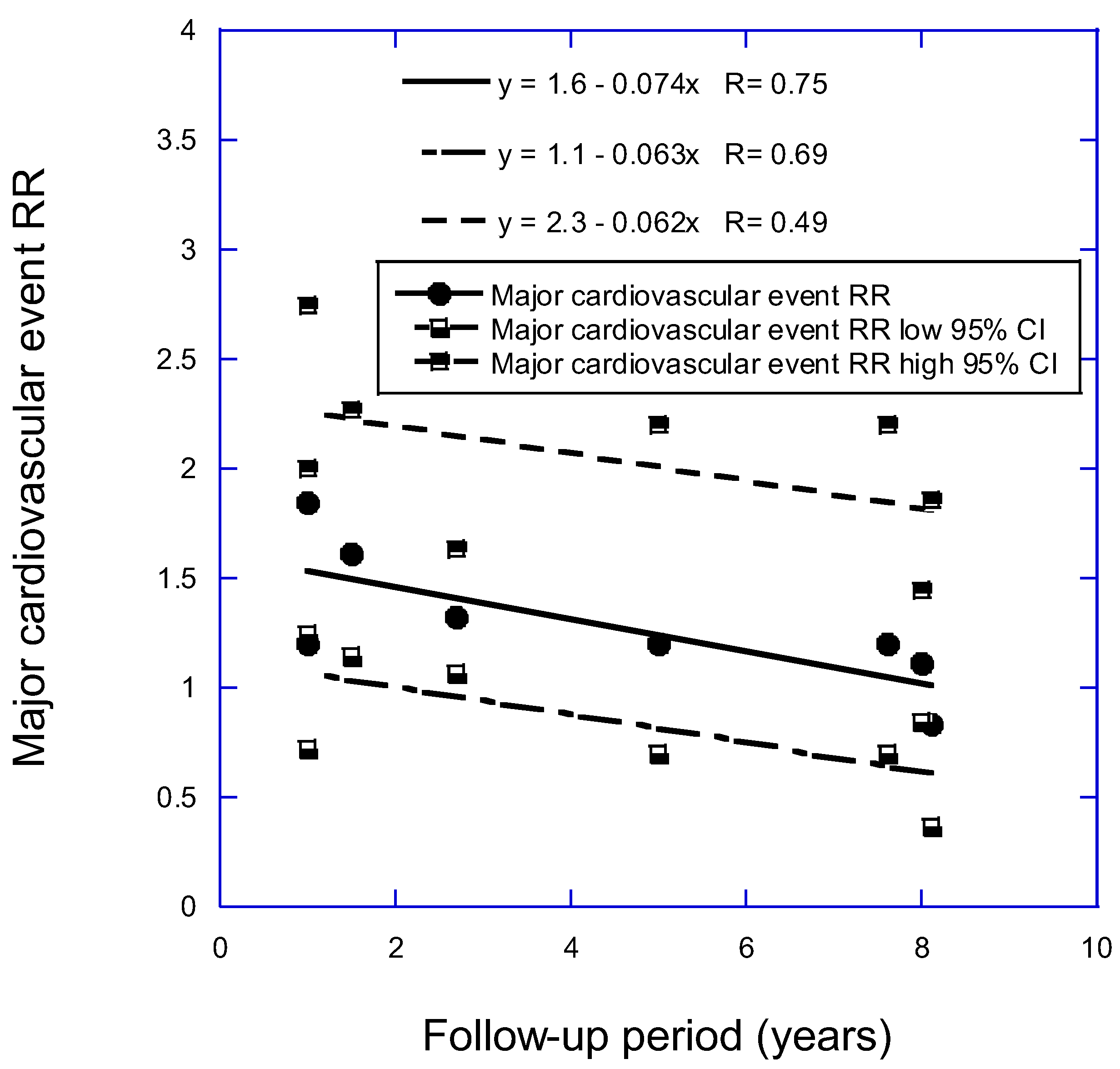
| Strength of association | “Strong” as suggested by Figure 1 and Figure 2. | |
| Consistency | “Strong,” i.e., results from various European countries as well as the United States and Hong Kong were in general agreement with each other. | |
| Temporality | “Strong” as all the prospective cohort studies agreed. | |
| Biological gradient | “Strong” as the serum 25(OH)D concentration–risk relationship is well known across the literature on human health. | [42] |
| Plausibility | “Strong” as many mechanisms have been shown (see Table 7 and preceding text) | |
| Coherence | “Strong” because vitamin D has many mechanisms for maintaining good health, including affecting gene expression and downregulating adverse effects on immune and inflammatory processes in vivo. | [70] |
| Experiment | “Weak” as RCTs have not found that vitamin D supplementation reduces risk of stroke or CVD event, probably from not conducting RCTs of appropriate design (see Discussion). | [93,94,101] |
| Analogy | Similar findings are seen for Alzheimer’s disease, dementia, and cognitive decline. | [8] |
| Confounding factors | A possible confounding factor is release of nitric oxide from subcutaneous nitrate stores through the action of UV irradiation, though strong evidence for that effect is lacking. | [102] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





