Submitted:
27 September 2024
Posted:
27 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
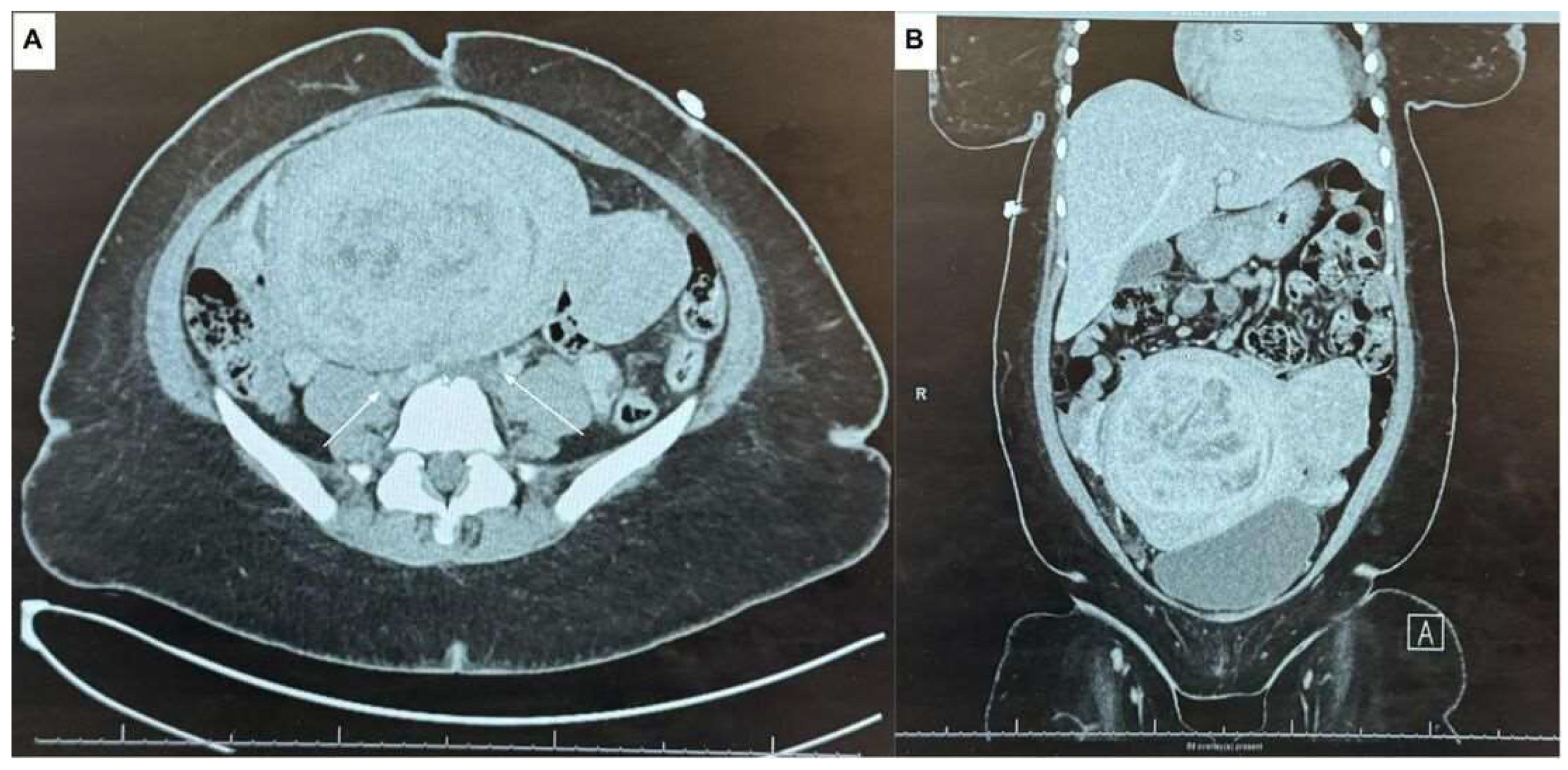
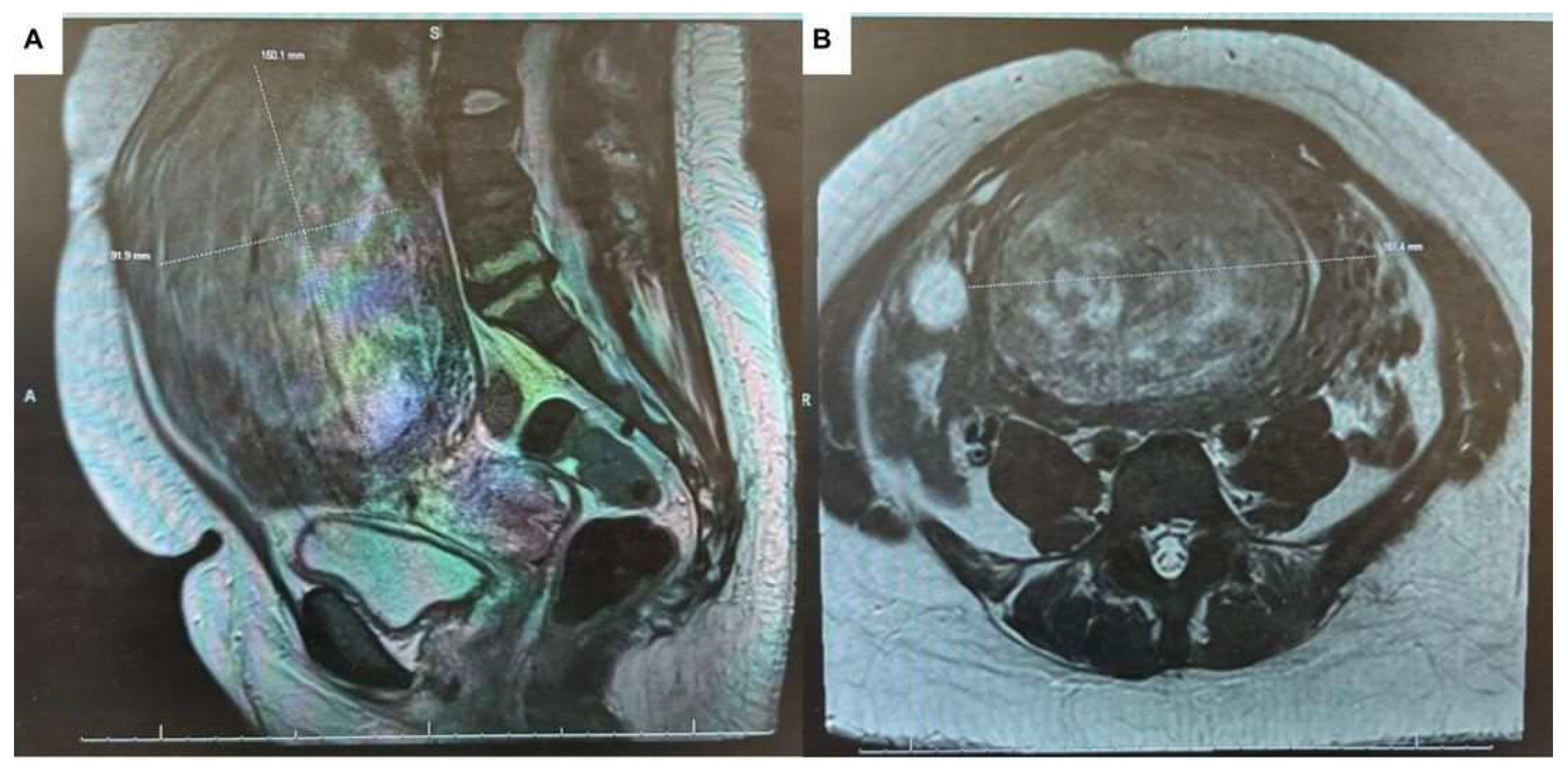
2. Case Presentation
3. Discussion
4. Conclusions
Funding
Informed Consent Statement
Acknowledgments
References
- Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol 2009, 23, 609–17. [Google Scholar] [CrossRef] [PubMed]
- Shiota M, Kotani Y, Umemoto M, et al. Deep-vein thrombosis is associated with large uterine fibroids. Tohoku J Exp Med 2011, 224, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld H and Byard, RW. Lower extremity deep venous thrombosis with fatal pulmonary thromboembolism caused by benign pelvic space-occupying lesions: an overview. J Forensic Sci 2012, 57, 665–668. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa H, Ideishi M, Nishimura T, et al. Deep venous thrombosis and pulmonary thromboembolism associated with a huge uterinemyoma: a case report. Angiology 2000, 51, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Riat R, Chowdary P, Mavrides E, et al. Is there an association between thrombosis and fibroids? A single centre experience and literature review. Int J Lab Hematol 2013, 35, e13–e16. [Google Scholar]
- Ramanan S, Chapman-Wardy J and Watson R. Bleeding versus clotting: a complex case of a large fibroid uterus causing menorrhagia and a DVT. Case Rep Obstet Gynecol 2016, 2016, 4169565. [Google Scholar]
- Fletcher H, Wharfe G, Williams NP, et al. Venous thromboembolism as a complication of uterine fibroids: a retrospective descriptive study. J Obstet Gynaecol 2009, 29, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Vyas, V. , Sankari, A., & Goyal, A. (2024, February 28). Acute pulmonary embolism StatPearls- NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560551/.
- Waheed, S. M. , Kudaravalli, P., & Hotwagner, D. T. (2023, January 19). Deep vein thrombosis StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507708/.
- Vyas, P. , & Douglas, L. Fibroids as a risk factor for Deep vein thrombosis (DVT) at an Urban Academic Institution: A retrospective observational study. Journal of Minimally Invasive Gynecology 2021, 28, S107. [Google Scholar] [CrossRef]
- Massive pulmonary embolism in a woman with leiomyomatous uterus causing pelvic deep venous thrombosis. (2005, June 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/16052843/.
- Young, M. , Coffey, W., & Mikhail, L. N. (2023b, July 3). Uterine fibroid embolization. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519016/.
- Lacharite-Roberge, A. , Raza, F., Bashir, R., Dass, C. A., Moser, G. W., Auger, W. R., Toyoda, Y., Forfia, P. R., & Vaidya, A. Case series of seven women with uterine fibroids associated with venous thromboembolism and chronic thromboembolic disease. Pulmonary Circulation 2018, 9, 1–7. [Google Scholar] [CrossRef]

| Venous Blood Gas | RESULTS |
| FIO2 | 21 |
| Pat Temp | 36.7 |
| PH BG | 7.43 |
| PCO2 | 31 Low |
| PO2 | <17 Low |
| HCO3 | 21 Low |
| B.E. | -3.3 |
| % O2 Hb | 10 Low |
| O2 Sat | 10 Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





