Methodology
Surgical Part
This was a case report study, done at Almubarik hospital from April 2024 to July 2024. Ethical approval was taken from the National Center for Neurological Sciences. Almubarik hospital is located in Kassala city, the distance between Kassala and Khartoum about 600 km. Almubarik hospital contains 6 departments, general surgery, pediatric, obstetrical and gynecology, general medicine, orthopedics and recently neurosurgery. There is a sharing emergency unit for all departments. The theater contains 3 operating rooms, one of them for neurosurgery. There is small ICU contains 2 beds and one ventilator. Almubarik hospital is embracing most of the medical staff (surgeons, Anesthesiologist, nurses, medical engineer, scrub nurse and others) coming from Khartoum and Gazera states.
To achieve adequate operative outcome, not only depend on the surgeon's technical skill and handiness, but also on a massive amount of details that interrelated to precise diagnosis and watchful preoperative planning. All patients and their families were informed about the contemplated operation and clearly be supposed to understand the related side effects and risks.
The operating room at Almubarik hospital includes X-ray viewing box, operating table, this table is design for obstetrical and gynecology operation. In neurosurgery, patient positioning is a critical step; to overcome this we used a bellow to obtain a suitable position.
Good operative results requires: careful selection of instruments for the macrosurgical portion of the operation performed with the naked eye, and the microsurgical part require operating microscope. [
2,
3]
Nevertheless, during this armed conflict, commonly, we used orthopedic cranial drill for making a series of burr holes, the burr holes were manually connected to a Gigli saw, then after that, bone flap was completed, defiantly this process is very hard and requires a great strength. Instead of using curette, we used bone gutter for removal of the last shell of bone between the drill surface and neural or vascular structures.
After elevation of the bone flap, dura was tacked to the bony margin using different size proline as suture material, so as to control the extra dural bleeding.
In fact we used very limited instruments for completing the surgery; a trend is to select instruments with handles and tactile characteristics suitable for both
macrosurgery and microsurgery and to change only the size of the instrument tip which was happen in the past before the area for operative microscope which is not available. For example the instruments which we used; forceps with the same size, scissors which were not fitting with macrosurgery or microsurgery. In adding to this, there was only one straight dissector, this dissector is bayonet and bigger in size, which was not only used for separation of the tumor from the cortex, it was used here for elevating the bone flap. For suturing, instead of using delicate suture material for closing the dura, we used what were available (nylon or prolene) sutures. In addition to these challenges, the needle holders were not fitting with the needle itself. When we came to the suction tube, certainly we have, but not Dandy designed. We have no Self-retaining retraction systemsn, which are routinely used for most intracranial operations [
4]
In the normal neurosurgical setting, bipolar coagulation is routinely used to control bleeding from the scalp margins, on the dura, and at intracranial Sites. [
5] Fortunately we have unipolar and bipolar coagulation with different forceps.
In adding to this, we have oxidized regenerated cellulose which is frequently used for coagulation the brain side. [
6] Furthermore, we used application of surgical and cover with simple cotton for some time to control venous bleeding which in line with the international one [
7].
Anesthetic Part
In the ideal situation in excision or debulking of brain tumor, the time of this procedure ranging from 1 to 8 hours, pain control, position varying; supine with head up tilt, lateral decubitus or prone. Blood loss may reach up to 2000 L, this beside practical technique ETT (Endo tracheal Tube), IPPV (Invasive Positive Pressure Ventilation), arterial line and CVP Central Venous Pressure).
Anesthesia preparation divided into three period, the first one is pre operative clinical assessment of the patient and all basic investigations, premedication , blood donation, DVT Deep Vein Thrombosis) prophylaxis.
The intra operative period which is the second one divided into 3 phases; phase one is the induction; in which the patient needs standard monitoring ( pulse oximeter, non invasive blood pressure, capnograph and ECG), beside invasive BP monitoring, CVP, core temperature and urinary catheter.
In this new situation there is no invasive BP, CVP, core temperature or even capnograph, all this made difficulties in monitoring the patient, in this regard, we tried to deal with it by more focusing on the basic monitoring. When we came to the anesthetics drugs, thiopental 3 mg/ kg or propofol 2-3 mg/ kg combined with remifontanil ( 0.2-0.5microgram/kg/min), non depolarizing muscle relaxant and armer ETT for induction, however, in this conflict period, due to the lake of monitoring of the drugs and inappropriate storage, we used to give IV propofol 1-2 mg/kg +IV midasolam 0.05mg /kg + IV morphine 0.01 -0.05 mg/kg+ lidocaine 1.5mg/kg+ nondepolrising muscle relaxant. In addition to this, we used regular ETT size 7 for all adult patients as it is the only big size available.
In phase 2 which is the monitoring, volatile agent ( servofurax/isofluranx<1 MAC (Minimal Alveolar Concentration)) or propofol infusion 3-6 microgram/ml + runifnftanil 0.15-0.25micro/kg/ minute. in this war conflict situation, we used halothane 0.4- 0.6 MAC as volatile agent with propofol infusion ( 200 mg in 500 ml normal saline) titrated according to patient vitals, pracetamol 1gm – magnisum sulphate 2gm are given as analgesia
For positing there is special table and head rest are design for neurosurgical patients in particular in prone position. What is actually done in this critical period of Sudan, for positing we manipulate our operating table by adding special head rest which was manually made from iron par and semi firm bellows are constructed on it tightly, so prone position was made. Lastly in phase 3, recovery, in this phase no differences, we used recovered agent atropine, neostagmine and monitoring the vital signs
The last period in anesthesia is the post operative, here the patients were transferred to the ICU, either on mechanical ventilator or without, this is based on her/ his per operative condition, we used analgesia inform of paracetamol , NSAID (Non Steroidal Anti inflammatory Drugs) if no contraindication+ or- opioiod ( morphine). [
8]
Ethical Approval
The ethical approval was obtained from the ethical committee at the national center for neurological science, Khartoum, Sudan.
Written consent was obtained from each participant.
Cases:
#Case 1:
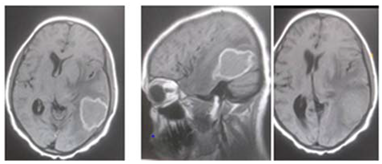
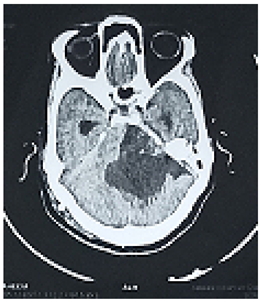
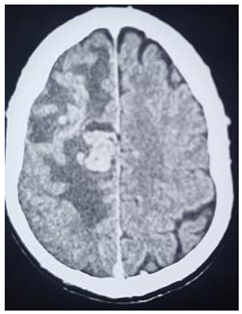
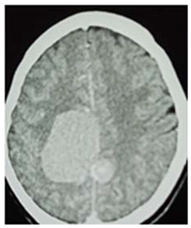
This is 18years Sudanese young female, university student, an otherwise healthy before, presented to neurosurgery emergency unit with history of rabidly progressing headache for 6 months duration, few weeks before her appearance she exhibit visual blurring that end in decrease visual acuity in both eyes, she has inability to walk steady.
Neurological examination, revealed conscious patient, with just perception to light and there was increase tone and exaggerated reflexes on both lower limbs.
Operation: Before the decision of surgery, we talked to the patient and her family clearly about the surgery complications and post operative outcome. Through left tempro- parito-occipital craniotomy, the tumor was macroscopically totally resects. It was sub cortical, well circumscribed ill define capsule, extended deeply to the underlining temporal horn of the lateral ventricle .Dural graft was taken from the tempralis fascia and was closed in water tide.
Patient was fully recovered from anesthesia and was taken to the ICU on nasal oxygen mask.
Histopathology
Brain tubeclomata ( extra pulmonary tuberculosis)
Patient was put on anti-tuberculosis according to the international protocol, and discharged free of headache, can see objects.
#Case 2:
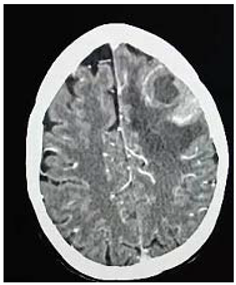
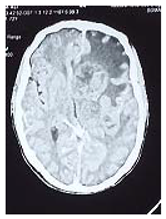
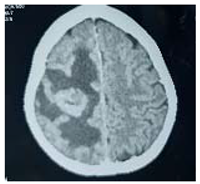
This is 16 years male, off school, experiences history of febrile illness and headache for long duration, presented to neurosurgery emergency unit with convulsions and deterioration level of consciousness this was 4 months before his presentation.
On examination: he was unwell, severe loss of weight, dry skin with multiple café aulate spots all over his body; there was bilateral eye globe proptosis.
Patient was admitted to ER and resuscitation was done
Operation: After clear counseling to the family, subsequently Left fronto –tempro-parietal craniotomy was done, operative findings: very thin bone with multiple eaten parts, the dura was very thin and adherent to the over lining bone, the tumor itself was multi in components, mucus like material and solid parts and cystic part which contained yellow fluid
In closing the dura, graft from the temporalis fascia was taken and closed in water tide.
Patient was recovered from anesthesia well, taken to the ICU on nasal oxygen
In the first post operative day, the patient showed dramatic improvements in his level of conscious, free of headache. Few weeks post operative; patient came to the clinic walking and looks happy.
Histopathology
Pilocystic astrocytoma
#Case 3:
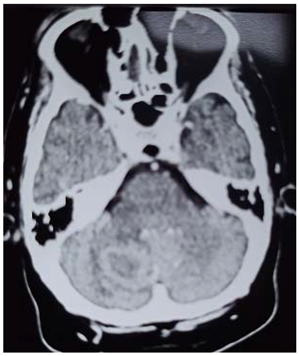
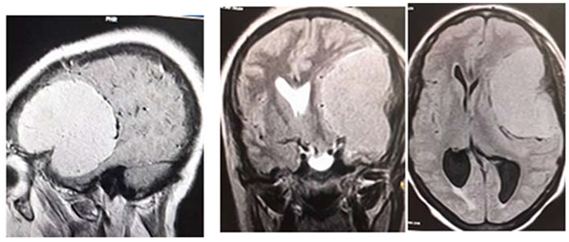
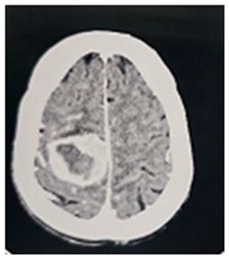
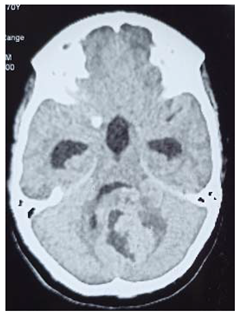
This is 50 years male, empolayer, heavy smoker, presented to neurosurgery emergency unit with history of rabidly progressing headache, unsteady gait and deterioration level of consciousness for few months duration.
On examination: obese, his GCS was 14/15, moving his limbs adequately but irritable.
Consequent to resuscitation, and clear counseling to the family, the patient prepared for surgical decompression.
Operation: through Rt par median sub occipital craniectomy, macroscopic excision of the tumor was done. The tumor was lobulated well circumscribed, less vascular and extending to the cistern magna.
Patient showed good recovery after the completion of surgery, taken to the ICU on nasal oxygen, and 48 hours released to the general word.
Histopathology
Revealed brain tuberclomata ( extra pulmonary tuberculosis)
Patient was put on anti-tuberculosis according to the program.
In the 7th day post operative, the patient developed high grade fever with respiratory distress, the diagnosis of pneumonia was made and eventually intravenous antibiotic was given, unfortunately, 3 days following he developed Rt lower limb cellulites that complicated with shortness of breath and emergency intubation was done and put on mechanical ventilation but few hours following he died.
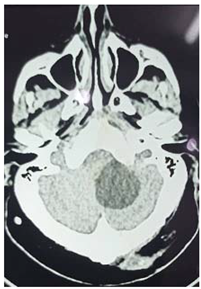
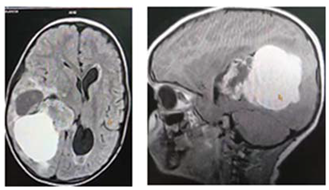
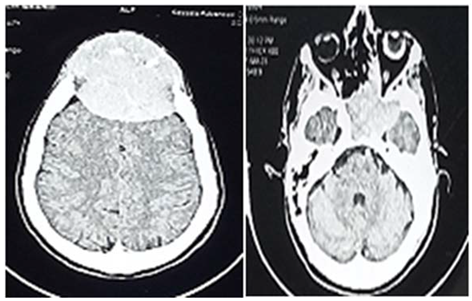
#Case 4:
This is 54 years male, driver, and an otherwise healthy before, presented to neurosurgery emergency unit with history of few weeks headache and blurring of vision.
On examination; he was unwell, but conscious, there was Rt side weakness that power was grade 4 in both upper and lower limbs.
An urgent VP shunt anterior approach was done, after which the patient showed improvement concerning headache, but few weeks followed he developed unsteady gait and dizziness
When we counseled the patient and his family, the decision of surgery was made and the patient was prepared for excision of the cyst.
Operation: Through Rt para median craniectomy, intra operative; there was cyst containing oily like fluid and soft tissue, thus macroscopic excision was done.
Histopathology
Showed low grade oligodendroglioma.
Patient discharge home in a good condition, but presented with superficial wound infection consequently debridement was done.
#Case 5:
70 years man, known case of GBM, presented to neurosurgery emergency unit with history of defective speech and progressing Rt side weakness.
We talk to the family and explained the prognosis of the disease,
Operation: through re opening of the previous bone flap, the tumor was invading the dura, adequate macroscopic debulking was made.
Patient was taken to the ICU with oxygen mask, recovered well, showed insignificant improvement in his speech but no change in his weakness,
Histopathology
not obtained.
# Case 6
This 40 years middle age man, worker, experienced history of convulsions, mood change and visual hallucinations over 6 months duration, few day before his presentation, he developed Lt side weakness.
Before surgery, we speak to the patient himself and his family clearly, regarding the complication of surgery and the tumor prognosis.
Operation: Patient was prepared for surgery, and through Rt posterior parietal craniotomy it was found that, highly vascular tumor, with thromboses blood vessels, nearly macroscopic total excision was completed.
Patient was recovered from anesthesia and taken to the ICU
Histopathology
Shows GBM, and eventually the patient was planned for adjuvant therapy, chemotherapy and radiotherapy and eventually sent to Merowe town isotope center.
#Case 7:
This 40 years male, off work, experience history of long duration headache and impaired hearing over the last few years, few months before his coming, he developed difficult in swallowing, nasal regurgitations and diminish hearing in his Rt ear.
On clinical evaluation; patient looks unwell, severe loss of weight, slurred speech spastic Rt side hemiplegia that the power grade 3.
Operation: Ventricuol-perotenial (VP) shunt anterior approach was done, patient showed good recovery from anesthesia but few hour post operative he developed drop in the level of consciousness that GCS was 7/15and agitated. After speaking to the family clearly about the new situation and explain the complications of the coming surgery, the decision of crainectomy was made. Patient was taken urgently to the operating room, and on lateral side position, and through far lateral craniectomy, intra operative; cyst containing oily like fluid and soft part. Macroscopic total excision was made.
Post operative, the patient recovered well from anesthesia, taken to the ICU on nasal oxygen mask. In the first post operative day, he regains his conscious, communicate with the surrounding.
Histopathology
Pilocystic astrocytoma.
Patient discharge in good condition, NG for feeding to prevail over the nasal regurgitations and improve gastric feeding, but still having Rt side weakness.
#Case 8
This 60 years old female, house wife, presented to neurosurgery clinic with rabidly progressing illness which was headache, convulsions and decrease level of consciousness. She is not known to be hypertensive or diabetic or having other chronic illness. Clinical evaluation exposed that,GCS9/15moving her Rt limbs less in response to pain.
Operation: Once clear counseling to the family was done. Consequently Lt craniotomy, macroscopic subtotal excision of the tumor was done, the tumor was deeply seated, lobulated pink in color and less vascular.
Patient recovered from anesthesia, taken to the ICU in nasal oxygen, in the first post operative day she showed improvement in the level of consciousness, start to communicate but still having weakness .Unfortunately in the 5th post operative day the patient developed loss of consciousness flowed by sudden arrest and died.
Histopathology
Ependymoma
#Case 9:
This 65 years old female, she exhibit history of headache, convulsions and Rt side weakness. There is multiple café aulate spots all over the body with multiple neurofibromas
Operation: Before preparing the patient for surgery, obvious counseling to the family was made. Accordingly through Left front- parietal craniotomy macroscopic excision of the tumor was completed, tumor was mixed in components, that contained solid and soft part
Patient recovered well from anesthesia and taken to the ICU
Histopathology
Astrocytoma grade 1
# Case10:
This 40 years middle age female, house wife, presented to neurosurgery emergency unit with history of progressing Rt side weakness and decrease visual acuity for few months duration. She experience history of chronic headache over years.
Operation; After speak with the patient and family, therefore Lt fronto –temporal craniotomy was completed and macroscopic subtotal excision of the tumor was done. It was huge tumor with ill defined capsule, extended arises from the medial sphenoid wing. The Sylvain vessels were displaced inferiorly
Patient recovered from anesthesia and was taken to the ICU on oxygen, in the first post operative day she showed slight improvement in her vision
Histopathology
Meningiothelial meningioma WHO grade 1
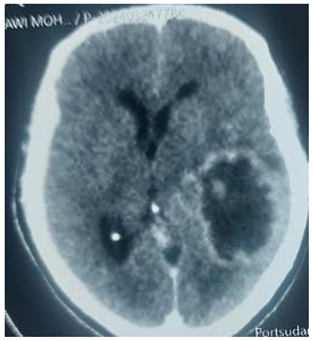
#Case 11:
This 5 years male child an otherwise healthy before, he has history of rabidly progressing headache , convulsions and lt upper limbs. Before his presentation, he became sleepy refused feeding. On clinical evaluations; confused child, moving his Lt upper limb less, pupil were dilated but reactive to light.
Operation: After clear counseling to the parent, decision of surgery was made. Through Rt craniotomy, huge lobulated mass multi-components, adherent to the wall of ipsilateral lateral ventricle, it was highly vascular, nearly total macroscopic excision was done.
Patient recovered from anesthesia and was taken to the ICU, in the following post operative day, he become fully conscious and showed improvement in his upper limb weakness and has no headache.
Histopathology
choroid plexuses papilloma WHO grade 1
#Case 12:
This 21 year young female, housewife, experience history of one years duration, headache, vomiting and unsteady gait, few days before her presentation to the emergency unit, she developed shortness of breath. On examination; she was unwell, exaggerated reflexes on all limbs.
Operation: Urgent ventrculo- protenial (VP) shunt was done; patient not recovered from anesthesia, immediately shunt ligation was done, and was put on mechanical ventilator in the first post operative day, no clinical improving. Following clear counseling to the family and explain the surgical outcome, patient was planned for debulking of the tumor.
Through midline sub- occipital craniotectomy the dura was opened , tumor came spontaneously , it was soft, mucus like, contained clotted blood. cerebellum become pulsating.
Patient left on the ventilator, but recovered from anesthetic drugs, on the second post operative day, she had good response to command, moving her limbs freely. Unfortunately, in the next 36 hours she developed hypotension that not response to inotropes and suddenly arrested and died.
Histopathology
Not obtained
#Case 13:
This 54 years female, known case of Rt CPA tumor, presented to neurosurgery department with history of severe headache ,unsteady gait and bulbar palsy that disturbing her feeding.
Operation: Once clear counseling, patient was prepared for surgery; reopening of the previous flap was done, the tumot was cyst containing solid part that was highly vascular, macroscopic excision was done.
Patient recovered from anesthesia and was taken to the ICU on oxygen
Histopathology
Pilocystic astrocytoma
#Case 14:
This 55 years middle age man, worker, experience history of rabidly progressing headache, convulsions, unsteady gait, mood change and left side weakness.
Investigations in attempt to search for the primary were done but all are negative
Operation: Before surgery, clear counseling to the patient and his family about the complications and post operative recover. And before skin flap ligation of the ipsilateral RT superficial veins was done and through Rt parietal craniotomy macroscopic nearly total excision of the tumor was done, it was highly vascular contained mesh like blood vessel.
Post recovering, the patient developed convulsions that controlled with the diazepam, taken to the ICU on nasal oxygen mask
In the first post operative day, he is free of headache but became depressed, no improvement in his weakness. In the third post operative day he developed signs of DVT on his Lt lower limb that complicated pulmonary embolism, resuscitation was done, oxygen anticoagulant were given, he recovered well.
Histopathology
Grade 11 astrocytoma
Patient is planned for adjuvant therapy at Merowe town isotope center.
#Case 15:
This 60 years male presented to the neurosurgery emergency unit with history of decreased level of consciousness. One month before his presentation, he has headache, fever, convulsion and urine incontinence . On clinical examination; GCS 13/15pupil bilaterally reactive to light, chest abdomen were free
Operation: After speaking to the family the decision of surgery was made.
Through craniotomy macroscopic excision of the tumor was done, it was highly vascular lobulated mass extended to the temporal lobe
Patient recovered from anesthesia well taken to the ICU
On the first post operative day he showed improvement in the level of consciousness, eventually in the coming day he start to communicate with the surrounding and walk freely.
Histopathology:
Heamangioblastoma
Patient was sent for adjuvant therapy at Merowe town isotope center.
#Case 16:
This 60 years male, worker, he presented with history of headache and convulsions for few months, few days before his presentation, he developed Lt side weakness.
Operation: After clear counseling to the patient, Rt craniotomy was done, macroscopic nearly total excision of the tumor was completed
Patient recovered well m taken to the ICU
Histopathology
Psammomatus meningioma
#Case 17:
This 45 years man, worker, experienced history of long duration headache and orbital pain over the left eye that associated with ipsilateral tooth pain. Few weeks before his presentation to the emergency unit; he developed frontal swelling that preceded by minor truma. On clinical examination; LT eye is totally blind and there is loss of smell . on examination; swelling was soft not pulsatile with elevated bony edges surrounding
Operation: We speak clearly to the patient about the complications and the post operative functionally recovery, patient was prepared to surgical excision, combined surgery with the fascio maxillary surgeon,
Through bi coronal skin flap; the tumor destructed the bone entirely, it was mixed in components, the sagittal sinus was inferiorly compressed by the tumor, .macroscopic total excision was done. The part of the tumor in the Let mandible was excised by the fascio maxillar surgeon., but the part in the infra temporal fossae was left.
Patient recovered from anesthesia taken to the ICU, in the first post operative day NG tube was inserted for feeding in ordered to make the oral cavity free from the sources of infection
Histopathology
Not obtained
# Case 18:
This 56 years female, worker, she exhibit history of generalize convulsions for the last 3 months it render her to lose her conscious, when she was evaluated at the emergency unit, she was conscious, no neurological deficit but having headache.
Operation: After counseling her and talk to her family, the descion of surgery was made.
Rt posterior parietal craniotomy was done, the tumor invaded the dura, arise from the posterior falx, thin capsule, macroscopic total excision was done. Dural graft was made from the fascia and close in water tide.
Patient recovered from anesthesia and taken to the ICU
Patient discharged in a good condition,one week later, she presented with symptoms of pulmonary embolism, thus treatment was handle by medical physician and after which discharged home.
Histopathology
Meningiothelial meningioma WHO grade 1
# Case 19:
This 37 years female, employer, has history of recurrence uterine fibroid, presented to neurosurgery emergency unit, with history of rabidly progressing focal convulsions and Lt side weakness over few weeks before her presentation. On examination, there is Lt side weakness with power grade II
Operation: Before surgery, we speak to the patient and her family and explained the outcome of surgery, Rt parietal craniotomy was done, the tumor sub cortical located, capsulated with massive brain edema surrounding, macroscopic total excision was done.
After recovering, she developed focal fits ipsilateral to the lesion, and thus IV diazepam was given to abort the fit.
Patient was taken to the ICU
She showed mild improvement in the motor power
Histopathology
Metastatic carcinoma, ultimately patient was planned to be evaluated at Merowe town isotope center.
#Case 20:
This 14 years young female, presented to emergency unit with history of long duration headache, vomiting, dizziness and unsteady gait this over the last year. She has been treated as the case of complicated severe malaria. On clinical examination; she was conscious, there is loss of co-ordination in both upper and lower limbs, hypotonia with hyper reflexia in her lower limbs.
Operation: Urgent ventriculo- peritoneal (VP)shunt was done anterior approach, patient in the first post operative day shows improvement in her gait and no headache
After clear counseling to the family regarding the complications and prognosis, the decision of the second section was made.
On prone position and through midline crainectomy, macroscopic subtotal removal of the tumor was done, dura flap was done and closed in water tide .
Patient has delay recovered from anesthesia, but she recovered and taken to the ICU on nasal oxygen
In the first post operative day she developed strider, agitation and fluctuation in the level of consciousness and poly urea ( 600 ml/ hour), thus injectable form of Dysmopresin was given. .In the 4th post operative day she developed apnea with shortness of breathing, hence connecting to mechanical ventilator but no muscle relaxant. Patient in the coming 2 days post ventilator; showed good recovery, she start to moving her limbs, responding well to the command.
Histopathology
Medulloblastoma WHO grade 1V, sooner the patient was planned for adjuvant therapy at Merowe town isotope center.