Abstract. The RECONNECT project tackles the fragmentation in Ireland's public healthcare systems, aiming to improve service planning and delivery. It integrates complex systems within the Health Service Executive (HSE) for chronic disease management, prioritizes data privacy, and supports future digital resource integration. The methodology includes: (1) structural integration via a Federated Database design to maintain system autonomy while ensuring privacy; (2) semantic integration through a Record Linkage module to enable integration without individual identifiers; and (3) adoption of the HL7-FHIR framework for high interoperability, aligning with the national electronic health record (EHR) and the Integrated Information Service (IIS). The RECONNECT system is unique in Ireland, featuring a generic architecture for loosely coupled systems, adherence to HL7-FHIR for interoperability, efficient reuse of digital assets, and a robust privacy layer. A demonstration system using synthetic data from the Hospital Inpatient Enquiry (HIPE) and Chronic Disease Management (CDM) systems is implemented on Neo4j for visualization.
1. Introduction
Chronic diseases, such as cardiovascular diseases, diabetes, chronic respiratory diseases, and cancer, are the leading causes of mortality and morbidity worldwide. These noncommunicable diseases (NCDs) account for approximately 71% of all deaths globally, equivalent to 41 million deaths each year. Cardiovascular diseases are the most significant contributors, causing an estimated 17.9 million deaths annually, followed by cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million). The burden of these diseases is not evenly distributed; over 85% of premature deaths from NCDs occur in low- and middle-income countries, highlighting significant health disparities [
15,
17].
Historically, many countries have faced challenges in integrating their healthcare systems to improve service planning and delivery. Efforts towards healthcare integration have aimed to create more cohesive and efficient systems, ultimately enhancing the quality of care and management of chronic diseases [
3,
5]. Fragmented healthcare systems can lead to inefficiencies, reduced quality of care, and difficulties in effectively managing chronic diseases [
1,
7]. This fragmentation is particularly problematic as chronic diseases place a significant burden on the healthcare system, necessitating coordinated, long-term management strategies. Efforts to integrate healthcare systems globally have shown that a unified approach can lead to improved outcomes, but achieving such integration remains a complex and ongoing process [
16].
In Ireland, as in many other countries, chronic diseases place a significant burden on the healthcare system, requiring coordinated, long-term management strategies [
5]. The RECONNECT project addresses these issues by proposing a novel method to develop digital health assets with the following objectives: (1) integrating complex, mission-critical systems within the Ireland Health Service Executive related to chronic disease; (2) prioritizing data privacy and governance; and (3) facilitating seamless integration with future digital resources.
Integrating these systems can improve data sharing and coordination among healthcare providers, leading to better patient outcomes [
8]. By prioritizing data privacy and governance, we ensure that patient information is protected, complying with regulations such as the General Data Protection Regulation (GDPR) [
9]. Finally, facilitating seamless integration with future digital resources prepares the system for scalability and adaptability, ensuring long-term viability and continuous improvement in healthcare delivery [
10].
2. Related Work
Chronic disease management continues to challenge fragmented healthcare systems, with integration of diverse data sources being crucial. The RECONNECT project addresses these challenges through a novel application of the HL7-FHIR framework for interoperability and integration. Various studies have explored similar approaches, providing a foundation for comparison.
Häyrinen et al. [
4] survey the significance of interoperability standards like HL7 in improving chronic disease management by facilitating data exchange among healthcare providers. However, their reviewed papers addressed theoretical aspects of standardization without delving deeply into practical implementation challenges, such as integrating loosely coupled systems.
Ayaz et al. [
2] provides a detailed review of FHIR standard, examining its implementations, applications, challenges, and opportunities in healthcare. FHIR aims to enhance interoperability by standardizing data exchange across systems. However, the reviewed literature does not address the practical challenges of integrating multiple data sources for chronic disease management, nor does it fully cover the specific issues related to privacy and data governance in real-world scenarios.
Ross et al. [
13] evaluate the effectiveness of a module in linking patient records across neighboring academic health care centers, focusing on the accuracy of record matching and addressing challenges such as inconsistent data entry and varying standards. However, their study does not address broader concerns related to integration and privacy.
In Scriney at al. [
14], the authors use the FHIR data model as the common model for integration across multiple healthcare systems used to monitor and analyse Covid-19 outbreaks. While researchers adopt a similar approach to ours in using the FHIR data model, they are mainly focused on the multi-disciplinary aspects of healthcare system integration where multiple sectors are involved in creating distributed datasets. In addition, the authors focus on efforts to create synthetic data to provide shareable FHIR datasets.
Paul et al. [
11] offer a broad analysis of the impact of digital technology on healthcare, highlighting significant privacy and security challenges. They emphasize broader cybersecurity issues and recent advancements, offering a wider context for understanding digital healthcare integration. However, they do not offer a targeted solution with a unique architecture for the interoperable integration of healthcare systems
The RECONNECT project distinguishes itself by combining these approaches into a cohesive system designed to handle the complexities of chronic disease management within a fragmented healthcare context. RECONNECT seeks to deliver a federated database design with a privacy layer and a record linkage module, ensuring both effective data integration and stringent privacy protections. This approach enables a more comprehensive solution than previous research, which often focuses on individual aspects of integration or privacy without addressing the full spectrum of practical implementation challenges.
3. Chronic Disease Datasets
Our RECONNECT project comprises four distinct datasets to effectively manage chronic disease information: Hospital In-Patient Enquiry (HIPE), Chronic Disease Management (CDM), Primary Care Eligibility and Reimbursement Scheme (PCeRS), and Diabetic RetinaScreen (RetinaScreen), as illustrated in
Figure 1.
3.1. Hospital In-Patient Enquiry
The HIPE scheme is a key national system in Ireland that collects detailed clinical and administrative data on patient discharges and deaths from acute hospitals. As the primary source of discharge data, HIPE provides valuable insights into hospital activities. The scheme gathers information on both in-patient and day-patient services from participating hospitals. Each time a patient is discharged or dies in a hospital, a HIPE discharge record is generated. This record includes administrative, demographic, and clinical details for each episode of care, which begins with the patient’s admission—whether as an in-patient or day-patient—and ends with their discharge or death within the hospital.
The MRN (Medical Record Number) serves as a unique identifier for querying HIPE. According to the HIPE Data Dictionary 2024, it is assigned by hospitals to track patients within a specific hospital. The MRN is also included in the national dataset, though in an encrypted format to protect patient confidentiality.
3.2. The Chronic Disease Management
The CDM dataset encompasses all clinical data elements necessary for defining chronic diseases within GP systems and supports the CDM project in collaboration with general practitioners. Managed by the HSE’s Office of the Chief Information Officer, this dataset includes national metadata fields such as clinical concepts, descriptions, and relationships. These fields are reviewed and updated every six months to ensure accuracy and relevance.
The
c_patient_ihi (IHI Number) is a unique numeric identifier used to individually distinguish each patient within the system. According to HSE [
6], the IHI National Register includes 4,775,629 records, each associated with a unique IHI number.
3.3. Primary Care Eligibility and Reimbursement Scheme
The PCeRS offers various reports on medical card eligibility and reimbursements. Visitors can access annual reports detailing claims and payments, along with current data on the various primary care services supported by PCRS. Additionally, this data is available on the eHealth Open Data Portal
1.
The
p_patient_refnum (IHI number) is a numeric identifier used to uniquely distinguish each patient in the PCeRS system. It also serves as the unique identifier for patients in the Drug Payments Scheme Refund
2, facilitating the claims process for prescribed medications.
3.4. RetinaScreen
RetinaScreen is designed to reduce the risk of vision loss in individuals with diabetes by identifying and addressing sight-threatening retinopathy early. It comprises two parts: the first is a population register with demographic information of people aged 12 and older diagnosed with Type 1 or Type 2 diabetes, to identify those eligible for screening; the second is clinical data to facilitate follow-up and clinical referrals for individuals requiring treatment.
The rs_contact identifier, referring to a patient's 10-digit mobile number, is used in diabetic retinopathy screening in Ireland. According to the "Framework for the Development of a Diabetic Retinopathy Screening Programme for Ireland" [
12], unique personal identifiers like names and addresses are needed to prevent double counting and correctly link follow-up data. The IHI number in RetinaScreen is another identifier that can be used for different purposes.
4. Integrated Methodology
4.1. Structural Integration
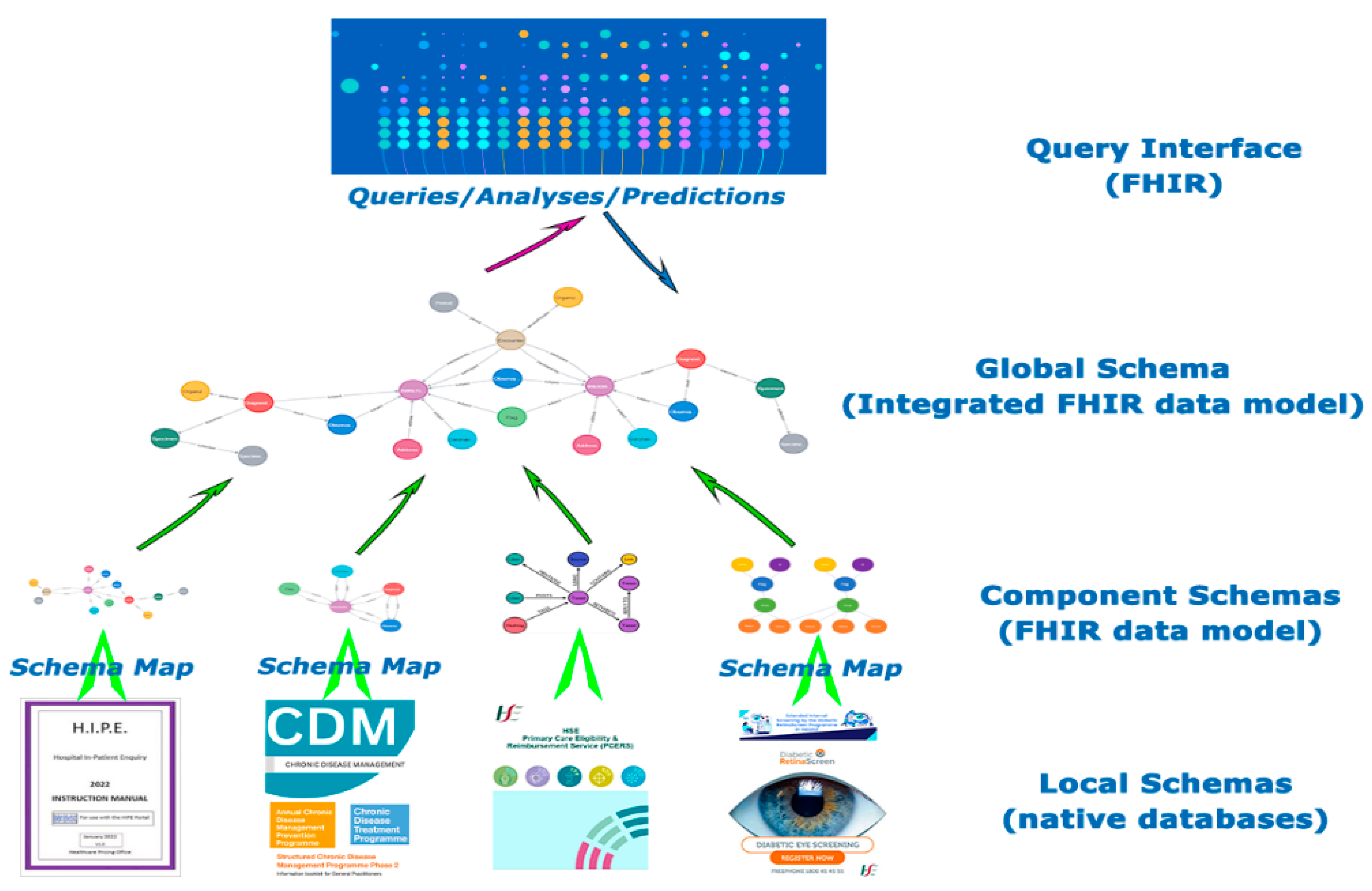
A Federated Database design provides a flexible approach that allows existing systems to retain their autonomy while supporting various levels of privacy and access control. This design is particularly valuable in managing complex, multi-source data environments. For instance,
Figure 2 illustrates the federated architecture used for chronic disease management, which integrates data from four distinct databases: HIPE, CDM, PCeRS, and RetinaScreen. Each database operates with its own local schema, which must be carefully discovered and integrated to ensure seamless interoperability. This integration process involves mapping and aligning the schemas to create a unified framework that facilitates effective data sharing and analysis while maintaining the integrity and security of each individual system. The federated approach thus supports both the autonomy of individual databases and the cohesive functionality of the overall system.
4.2. Semantic Integration
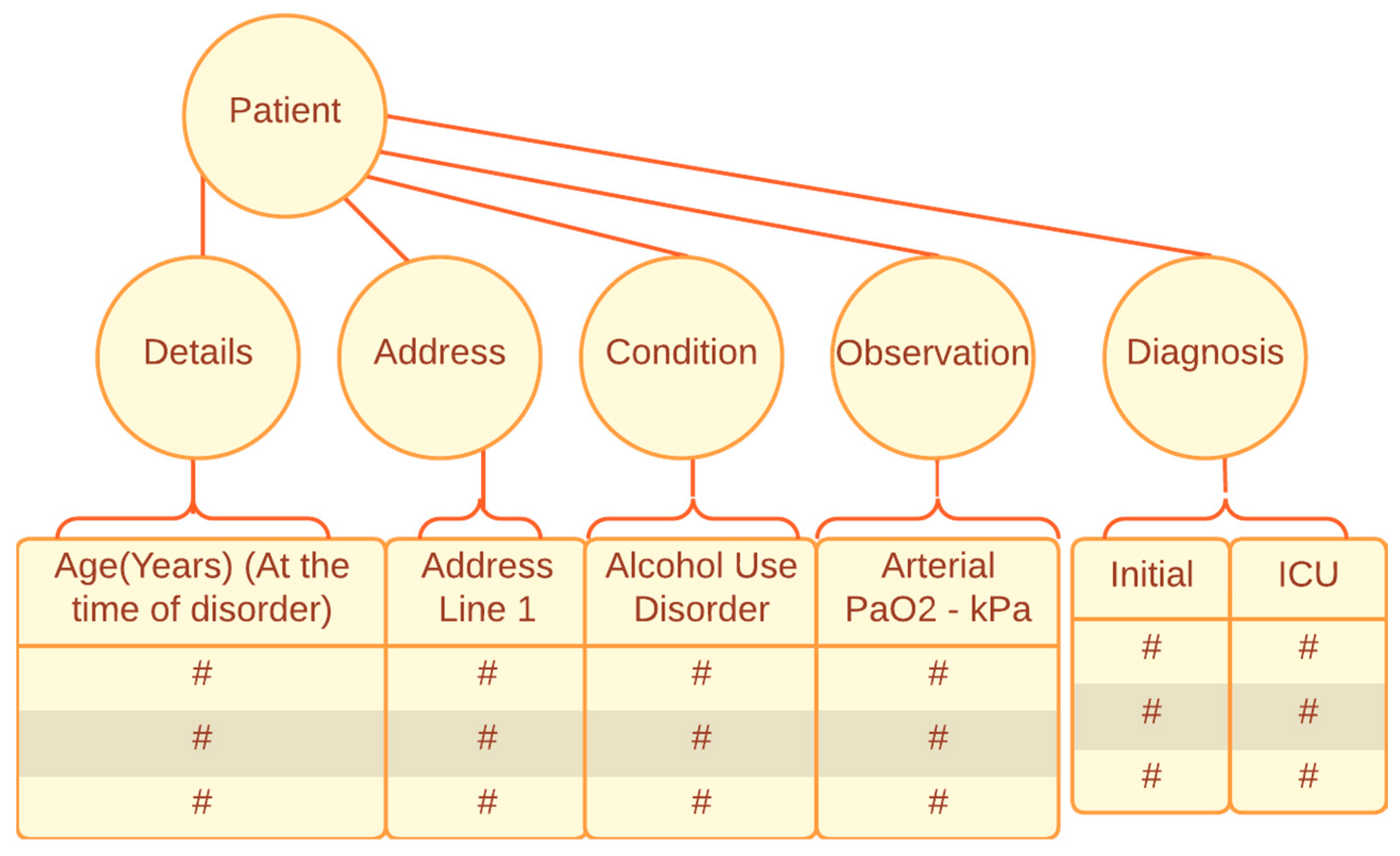
Implementing a Record Linkage module that adheres to data governance policies is crucial for effective integration, especially when individual identifiers are lacking in current healthcare systems. This module is designed to match and link records from disparate data sources without relying on a single, unified identifier. To align with data governance policies, the Record Linkage module must be meticulously crafted to ensure patient data privacy and integrity.
The design process involves developing algorithms that can accurately and securely connect patient records across various systems, using available data points such as demographic information, medical history, and other relevant attributes. This approach addresses the challenge of integrating data from different sources while maintaining compliance with privacy regulations and safeguarding patient information.
Figure 3 provides an example of how a patient can be identified based on non-identifiable attributes.
Additionally, the Record Linkage process helps to bridge the gaps caused by the absence of a pervasive Individual Health Identifier. By systematically analyzing and correlating data, the module enables healthcare providers to achieve a more unified view of patient information, ultimately enhancing the quality of care and decision-making. This integration strategy supports a more holistic approach to patient management, improving both data accessibility and the overall efficiency of healthcare systems.
4.3. Adoption of Standards
We propose a new framework utilizing HL7-FHIR model to enhance interoperability in our integrated FHIR data. This framework is designed to work independently of the participating healthcare systems, allowing for seamless data exchange and integration. By adopting the HL7-FHIR standard, the framework ensures compatibility across various healthcare systems, regardless of their underlying technologies.
The proposed framework also aligns with national electronic health record (EHR) systems and their proxies, such as the Integrated Information Service (IIS). This alignment facilitates integration with broader national health initiatives and standards, ensuring that our framework is in harmony with existing healthcare ecosystems.
Key features of the framework include its scalability and flexibility, allowing it to handle varying data volumes and adapt to evolving healthcare needs. Additionally, the framework incorporates robust mechanisms for data privacy and security, in line with HL7-FHIR standards, to protect patient information while enabling efficient data exchange.
Overall, this framework improves interoperability and data integration across diverse healthcare systems, leveraging the HL7-FHIR model to provide a more extensible solution for better data exchange and collaboration.
5. Results and Conclusion
The RECONNECT integrated chronic disease system represents a significant advancement over existing healthcare systems in Ireland, addressing several key challenges and offering unique value in multiple areas.
Firstly, the system features a generic architecture based on Record Linkage, tailored specifically for environments with loosely coupled information systems. This architecture is designed to enhance integration capabilities by enabling seamless connections between disparate data sources. Unlike traditional systems that often struggle with fragmented data and interoperability issues, the Record Linkage approach in RECONNECT ensures that different healthcare systems can effectively communicate and share information, thus facilitating a more cohesive management of chronic diseases.
Secondly, RECONNECT adheres to the global healthcare standard HL7-FHIR, marking a novel application within the Irish context. The HL7-FHIR standard is renowned for its ability to enhance interoperability across various healthcare systems by providing a common framework for data exchange. By adopting this standard, RECONNECT not only aligns with international best practices but also establishes a robust foundation for future interoperability. This alignment is crucial for ensuring effective communication and integration both within and between healthcare systems, thereby supporting a more integrated approach to chronic disease management.
Additionally, the RECONNECT system is designed with the capability to efficiently reuse and share digital assets when appropriate. This feature allows for the optimal utilization of existing data and resources, which is particularly beneficial in managing chronic diseases that often require longitudinal data and continuous monitoring. By enabling the reuse of digital assets, RECONNECT enhances the efficiency and effectiveness of healthcare delivery, reducing redundancy and improving data utilization.
Furthermore, privacy and data security are paramount in RECONNECT, which incorporates a dedicated privacy layer to safeguard patient information. This layer is essential for maintaining the confidentiality of sensitive health data, addressing concerns about data protection and regulatory compliance. The emphasis on privacy aligns with current data protection regulations and ensures that patient information is handled with the highest level of security.
To demonstrate its capabilities, a prototype of the RECONNECT system has been implemented using synthetic data from the Hospital Inpatient Enquiry (HIPE) system and the Chronic Disease Management (CDM) system. This demonstration, built on the Neo4j platform, provides a visualization of how the system integrates and manages data, offering a practical illustration of its functionalities and potential impact.
Overall, the RECONNECT integrated chronic disease system not only advances the state of healthcare integration in Ireland but also sets a new standard for managing chronic diseases through innovative technology and robust data management practices.
Acknowledgments
The research is part of the RECONNECT project: chRonic disEase: disCOvery, aNalysis aNd prEdiCTive modelling. This research was conducted with the financial support of National Challenge Fund, Science Foundation Ireland, Grant numbers: 22/NCF/DR/11244 and SFI/12/RC/2289_P2 at Insight the SFI Research Centre for Data Analytics at Dublin City University.
References
- Alotaibi, Y. K., & Federico, F. (2017). The impact of health information technology on patient safety. Saudi Medical Journal, 38(12), 1173-1180. [CrossRef]
- Ayaz M, Pasha MF, Alzahrani MY, Budiarto R, Stiawan D. (2021). The Fast Health Interoperability Resources (FHIR) Standard: Systematic Literature Review of Implementations, Applications, Challenges and Opportunities. JMIR Med Inform, 9(7), e21929. [CrossRef]
- Goodwin, N. (2016). Understanding Integrated Care: A Complex Process, a Fundamental Principle. International Journal of Integrated Care, 16(4), 19. [CrossRef]
- Häyrinen, K., Saranto, K., & Nykänen, P. (2008). Definition, structure, content, use and impacts of electronic health records: A review of the research literature. International Journal of Medical Informatics, 77(5), 291-304. [CrossRef]
- Health Service Executive. (2023). Chronic disease management programme. Retrieved from https://www.hse.ie/eng/services/list/2/primarycare/chronic-disease-management-programme/ (accessed 27 July 2024).
- Health Service Executive. (2024). Questions regarding the IHI. Retrieval from https://www.hse.ie/eng/about/who/national-services/individual-health-identifier/questions-regarding-the-individual-health-identifier-ihi-number.pdf (accessed on 20 July 2024).
- Kodner, D. L., & Spreeuwenberg, C. (2002). Integrated care: meaning, logic, applications, and implications – a discussion paper. International Journal of Integrated Care, 2, e12.
- Kruse, C. S., Stein, A., Thomas, H., & Kaur, H. (2016). The use of health information exchange to augment patient handoff communication in acute care: A systematic review. Journal of the American Medical Informatics Association, 23(2), 438-445.
- Gellert, G. A., Webster, G. G., & Gillean, B. D. (2020). Digital transformation of healthcare: Balancing risks and benefits for digital innovation. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 4(1), 25-33.
- Nambiar, D., Mander, H., Bärnighausen, T., Subramanian, S. V., & Laxminarayan, R. (2022). Health system integration and its determinants: A cross-sectional study in India. International Journal for Equity in Health, 21(1), 35.
- Paul, M., Maglaras, L., Ferrag, M. A., & Almomani, I. (2023). Digitization of healthcare sector: A study on privacy and security concerns. ICT Express, 9(4), 571-588. [CrossRef]
- Reilly, O. et al. 2018. Framework for the Development of a Diabetic Retinopathy Screening Programme for Ireland. HSE and the Irish College of Ophthalmologists. Retrieval from https://www.diabetes.ie/wp-content/uploads/2014/11/Framework_for_a_Diabetic_Retinopathy_Screening_Programme_1.pdf (accessed on 20 July 2024).
- Ross, M. K., Sanz, J., Tep, B., Follett, R., Soohoo, S. L., & Bell, D. S. (2020). Accuracy of an Electronic Health Record Patient Linkage Module Evaluated between Neighboring Academic Health Care Centers. Applied clinical informatics, 11(5), 725–732. [CrossRef]
- Scriney, M.; et al. (2023). Engineering Data Assets for Public Health Applications: A Covid-19 Case Study. In the 2023 IEEE International Conference on Big Data, pp. 1853-1862. [CrossRef]
- Stamenic, D.; et al. (2024). Health care utilization and the associated costs attributable to cardiovascular disease in Ireland: a cross-sectional study. European Heart Journal - Quality of Care and Clinical Outcomes, qcae014. [CrossRef]
- World Health Organization. (2017). WHO global strategy on people - centred and integrated health services: interim report. Retrieved from https://www.afro.who.int/sites/default/files/2017-07/who-global-strategy-on-pcihs-main-document_final.pdf (accessed 25 July 2024).
- World Health Organization (2021). Noncommunicable diseases. Retrieved from https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed 20 July 2024).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).