1. Introduction
With the global population gradually entering an aging phase, health issues among the elderly have become a focal point of societal concern[
1]. The high incidence of diseases among the elderly, especially chronic and disabling diseases[
2,
3,
4], has led to a continuous increase in the demand for rehabilitation. According to the World Health Organization (WHO), by 2050, the global population aged 60 and above will reach 2.1 billion, accounting for 22% of the total global population, posing enormous challenges and demands for medical and rehabilitation services[
5,
6].
Rehabilitation medicine plays a crucial role in enhancing the quality of life for the elderly[
7], encompassing not only the recovery of physical functions but also the reconstruction of psychological and social functions[
8,
9]. Franco-Urbano et al.[
10] systematically reviewed the impact of depression on functional recovery in elderly stroke patients, particularly emphasizing the importance of psychological rehabilitation. Comprehensive rehabilitation programs combining physical therapy and psychological interventions can significantly alleviate depressive symptoms, promote overall functional recovery, and improve the quality of life for elderly patients. Elsadek et al.[
11] evaluated the effects of indirect contact with nature on the psychological and physiological health of the elderly using forest imagery to simulate natural environments, finding that this method can significantly improve their psychological state and autonomic nervous system balance. Currently, rehabilitation medicine is gradually shifting from traditional hospital rehabilitation models to community and home rehabilitation[
12,
13]. This transition not only helps reduce the pressure on the medical system but also allows the elderly to receive more personalized and continuous rehabilitation services[
14]. McDonagh et al.[
15] through a randomized controlled trial, compared the effects of home rehabilitation and supervised center-based rehabilitation in adult cardiac patients, finding many similarities and confirming the great potential of future home rehabilitation[
16].
Multimodal sensory experiences, as an innovative design concept, significantly enhance the interaction experience and effectiveness of smart rehabilitation products by combining visual, auditory, tactile, and other sensory feedback. Through tactile feedback systems, patients can better perceive and adjust rehabilitation movements, thereby increasing the effectiveness of training. Additionally, visual and auditory feedback can provide real-time rehabilitation progress and guidance, helping patients complete rehabilitation training more effectively.However, the rehabilitation products and equipment available in the market often fail to meet the diverse needs of elderly users. These products mainly rely on single sensory feedback and cannot provide a comprehensive and multi-dimensional rehabilitation experience.
With the rapid advancement of digital and intelligent technologies, intelligent rehabilitation products offer new opportunities to address this issue. These products integrate multiple sensors and feedback mechanisms to monitor and analyze patients' rehabilitation status in real time, thereby providing personalized rehabilitation plans. Mathew et al.[
17] combined upper limb rehabilitation robots with artificial intelligence to collect real-time data, resulting in more scientifically based rehabilitation treatments. Guo et al.[
18] believe that intelligent technology and assistive devices are among the future trends, as they can significantly reduce the burden of home care. However, for the elderly, the gap between their weakened physical functions and digital technology becomes a major constraint on innovation. Researchers need to focus on the ethics of aging suitability, ensuring that product designs align with the cognitive and usage habits of elderly users.
2. Materials and Methods
2.1. Multimodal Theory
The human sensory system, comprising the five primary senses and their associated neural networks, forms an integrated perception system that allows us to understand and interact with the world in various ways. This complex sensory mechanism enables multifaceted interactions and interpretations of our environment. Currently, most intelligent products primarily rely on voice and screen interactions, which limit the enhancement of natural interaction experiences[
19]. Voice commands and screen displays cannot comprehensively cover the diversity and complexity of the human sensory system, especially in scenarios requiring delicate and intuitive feedback[
20]. In this context, touch, as a crucial means of human cognition, becomes particularly significant. It is not merely simple physical contact but includes various sensory information such as pressure, vibration, and temperature, which are transmitted to the brain via the nervous system to help us understand and respond to the external environment[
21]. Integrating multimodal tactile information with non-tactile sensory strategies opens up new possibilities for enhancing tactile experiences in the realm of intelligent products[
22].
For elderly smart interactions, the "compensation of the five senses" becomes a method. By utilizing a multi-sensory compensation mechanism, it effectively enhances the sensory capabilities of the elderly in smart interactions[
23], addressing the common sensory function challenges they face. In the context of multimodal perspectives, the collection and analysis of physiological data become key in designing age-appropriate products, providing precise data support for rehabilitation plans, and promoting more natural and profound interactions between intelligent products and users[
24]. The core lies in organically combining various sensory feedbacks such as visual, auditory, and tactile, forming an integrated rehabilitation experience[
25].Marques et al.[
26] explored the benefits of outdoor intelligent therapeutic and rehabilitation spaces combining mobile medical technology and sensors for elderly health. They collected biometric data from the elderly in outdoor spaces and transmitted the data through intelligent interaction platforms, effectively enhancing both physical and psychological health. When designing multimodal rehabilitation products, it is essential to consider the ethics of aging suitability, ensuring that product designs align with the cognitive and usage habits of elderly users. Adhering to principles of simplicity and ease of use, and providing clear voice prompts and visual guidance is crucial[
27].
2.2. Market Research
The needs of the elderly consumer group span various aspects of life. However, as they age, they inevitably face the harsh reality of declining physical functions[
28,
29]. Currently, the rehabilitation medical industry in our country is not yet fully developed and is mainly divided into two categories: rehabilitation hospital treatment and home recuperation. Given the uneven quality of professional service personnel and the high costs, many elderly people tend to opt for home recuperation. To improve this situation, it is imperative to strengthen the construction of the rehabilitation medical system and enhance the quality of rehabilitation products available for the elderly on the market. As shown in
Table 1, there are five categories of commonly used rehabilitation products for the elderly.
2.3. User Research
Zhang et al.[
32] proposed a comprehensive assisted product design model based on user preferences (PAPDM), which captures the preference factors of the elderly to design auxiliary products that better meet their needs, thereby reducing abandonment rates and promoting active aging. Bai et al.[
33] studied the determinants of comfort in intelligent mattress design from the perspective of user needs, emphasizing that the angle range of the bed board should be optimized based on individual differences and needs to adjust sleeping posture and balance pressure distribution, thereby improving sleep comfort.
This study focuses on the needs analysis of elderly users, exploring the potential opportunities for introducing multimodal interactions in the rehabilitation process. The research aims to understand the cognition, experiences, and expectations of elderly people regarding intelligent rehabilitation devices, thereby identifying service opportunities and design positioning. The researcher visited local rehabilitation centers, elderly activity centers, and residents' homes to conduct on-site interviews with five elderly individuals who are capable of self-care (see
Figure 1). Through face-to-face interviews with target users, the study provides a deeper understanding of their experiences, needs, and the motivations behind their product choices. The entire interview process was audio-recorded and transcribed for subsequent information sorting and analysis.
From the interviews, it was found that each elderly individual has specific health conditions. The interviewers have summarized and distilled the core information, which is presented in tabular form, as shown in
Table 2.
The study found that the surveyed users primarily suffer from common geriatric and chronic diseases. Many individuals entering old age still maintain good physical function, and thus, those with mild conditions often rely on self-healing methods. However, this approach can pose significant health risks. Those with more severe conditions tend to seek medical examinations and treatment in hospitals, following doctors' orders for home recovery.Currently, the prevalence of rehabilitation products is relatively low, with limited exposure to relevant products, which are often difficult to operate and generally not very effective. Through interviews, it was discovered that elderly individuals are not averse to intelligent rehabilitation products, but they may feel averse to complicated operations. Function prompts should emphasize key information, ensuring that modules are clear and easy to understand, and leaning towards simplicity and straightforwardness in product design.
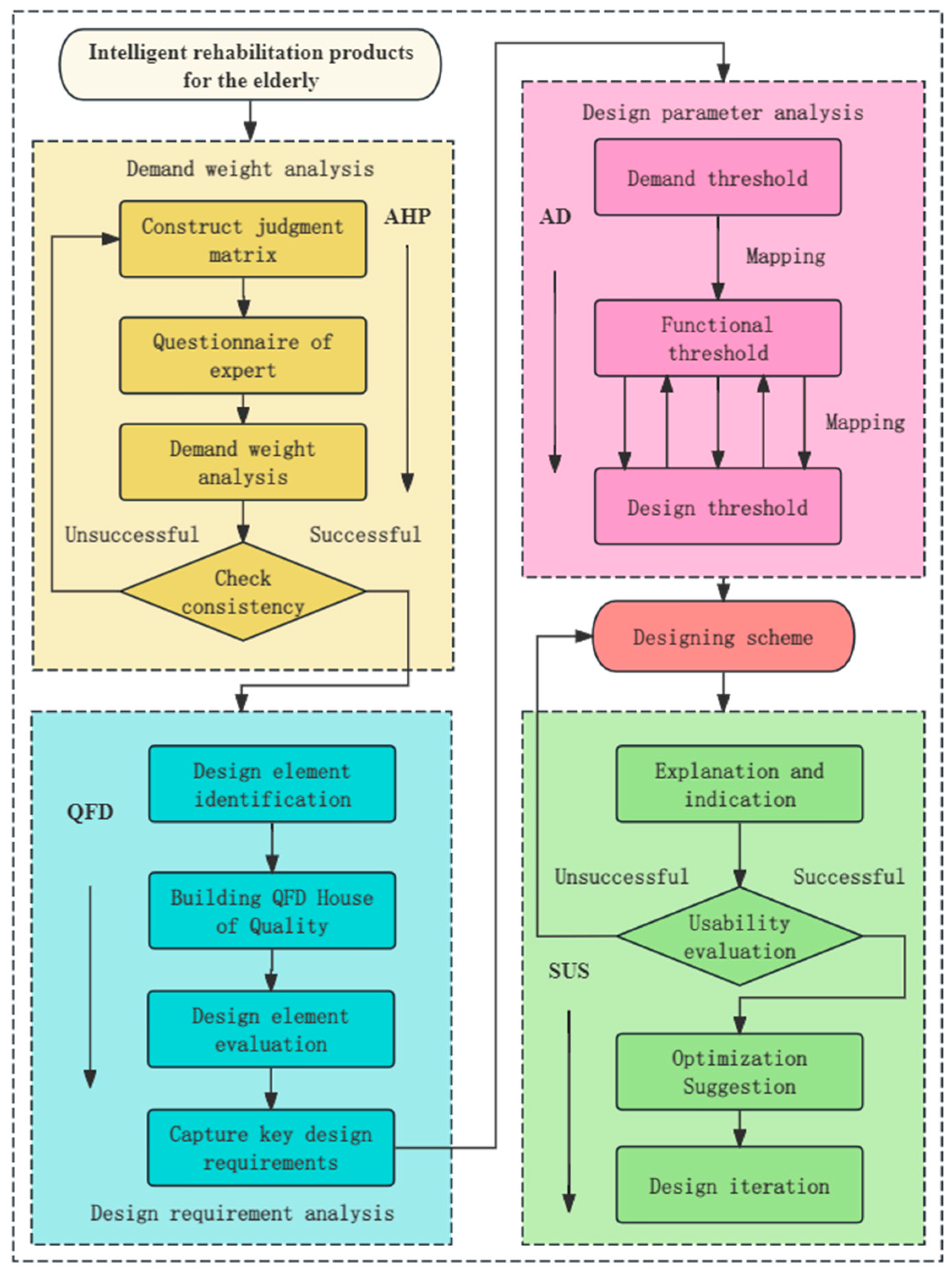
2.4. Design Process Based on AHP-QFD-AD
The Analytic Hierarchy Process (AHP) is an effective decision-making tool that constructs an analytical decision model by considering various factors influencing the design of elderly rehabilitation products and determining their relative importance. These determined weights can provide a basis for design decisions, thereby guiding the design of intelligent rehabilitation products for the elderly[
34]. Quality Function Deployment (QFD) translates user needs into specific product characteristics and technical specifications, accurately understanding the needs of elderly users and converting them into specific technical specifications and functional characteristics, which helps create products that align with user needs[
35]. Axiomatic Design (AD) helps designers optimize rehabilitation product designs by mapping user needs to relevant domains, completing the transformation from "needs" to "functions" to "design," obtaining specific design parameters, and constructing the optimal solution[
36].
This comprehensive evaluation method allows for a better understanding of user needs and the design of more attractive products. It effectively avoids the limitations of a single model by scientifically converting user needs into specific technical specifications and design parameters. Additionally, it systematically evaluates and quantifies the priorities of various needs, ensuring the rigor and logic of the design process[
37]. Thus, the designed intelligent rehabilitation products for the elderly not only meet the actual needs of elderly users but also stand out in the competitive market, as shown in
Figure 2.
According to age brackets, the elderly population is subdivided into several stages: 60-64 years (active health period), 65-74 years (self-sufficient period), 75-84 years (slow movement period), and 85 years and above (stage needing care and attention)[
30]. This classification reflects that a significant proportion of elderly individuals can maintain relatively independent living abilities during these stages, demonstrating a trend of autonomous living among the elderly population[
31]. The mainstream rehabilitation products for the elderly primarily target geriatric diseases, assisting them in achieving autonomous movement at various stages. In the future, more intelligent and personalized rehabilitation products will become key market drivers, aiming to fully meet the rehabilitation and living needs of the elderly at different stages.
3. Results
3.1. Analytic Hierarchy Process
3.1.1. Determine User Needs
The initially summarized user needs were subjective and lacked emphasis. To precisely determine the design requirements in QFD, the AHP quantitative analysis method was introduced to objectively filter user needs. To obtain the weights of each criterion, this study invited five teachers and designers from the field of rehabilitation products to serve as expert representatives. As shown in
Table 4, the relative importance weights and rankings of each evaluation criterion are presented. The calculated consistency ratio is 0.029, which does not exceed the threshold value of 0.1, thus confirming that this weight distribution meets the consistency standard. Based on the weight values, user needs were filtered to derive the key user needs for intelligent rehabilitation products for the elderly, aiding the accuracy of subsequent QFD research.
3.1.2. Determine User Needs
The initially summarized user needs were subjective and lacked emphasis. To precisely determine the design requirements in QFD, the AHP quantitative analysis method was introduced to objectively filter user needs. To obtain the weights of each criterion, this study invited five teachers and designers from the field of rehabilitation products to serve as expert representatives. As shown in
Table 4, the relative importance weights and rankings of each evaluation criterion are presented. The calculated consistency ratio is 0.029, which does not exceed the threshold value of 0.1, thus confirming that this weight distribution meets the consistency standard. Based on the weight values, user needs were filtered to derive the key user needs for intelligent rehabilitation products for the elderly, aiding the accuracy of subsequent QFD research.
3.2. Quality Function Deployment
In the Quality Function Deployment (QFD) method, the constructed House of Quality uses an intuitive matrix layout and graphical representation to guide the final design in a quantitative manner. The specific content is shown in
Table 5.
3.2.1. Design Requirement Analysis
Based on the comprehensive expert evaluations, a series of design recommendations for intelligent rehabilitation products for the elderly were obtained. Elderly individuals tend to be conservative and prefer products that are durable, safe, and of high quality. Since they have established fixed living habits and usage patterns, the design should prioritize user habits[
38]. After discussions with the expert panel, it was unanimously decided to use an intelligent rehabilitation bed as the main design subject for this study. A comprehensive analysis of the related design requirements for this intelligent rehabilitation bed was conducted, resulting in the specific design scheme shown in
Table 6.
3.2.2. Quality House Construction
To determine the weights among the design elements of intelligent rehabilitation products for the elderly, it is necessary to clarify the correlation between user needs and design requirements. Our research team invited three senior designers of medical rehabilitation products to form an expert panel. They conducted pairwise comparisons for each combination to establish the House of Quality for elderly intelligent rehabilitation products. The study used a scoring system from 1, 3, 5, to 9, representing weak to strong correlations, respectively. The results are shown in
Table 7.
3.3. Axiomatic Design
3.3.1. Demand Mapping
From the QFD analysis, the six highest-weighted factors are: sturdy structure (18.7%), wear and pressure resistance (18.2%), ergonomics (13.7%), unified control adjustment (10.2%), visual Auditory Tactile feedback (8.6%), and monitoring system (8.3%). These factors will serve as the basis for the design practice of this device. Following the core principles of Axiomatic Design (AD) theory ensures precise mapping between functional requirements and design parameters. Based on the expert team's recommendations, the design parameters for intelligent rehabilitation products that meet the needs of elderly users are established, as shown in
Table 8.
3.3.2. Independence Test
Mapping the functional requirements (FR) to the specific design parameters (DP) of intelligent rehabilitation products for the elderly, we obtain the design matrix G:
From this analysis, the constructed matrix is a diagonal matrix, achieving an uncoupled state where each element is independent. This follows the principle of the independence axiom, indicating that parameters FR1 to FR6 are viable. The design parameters involved in this scheme are reasonable and can provide theoretical support for subsequent designs.
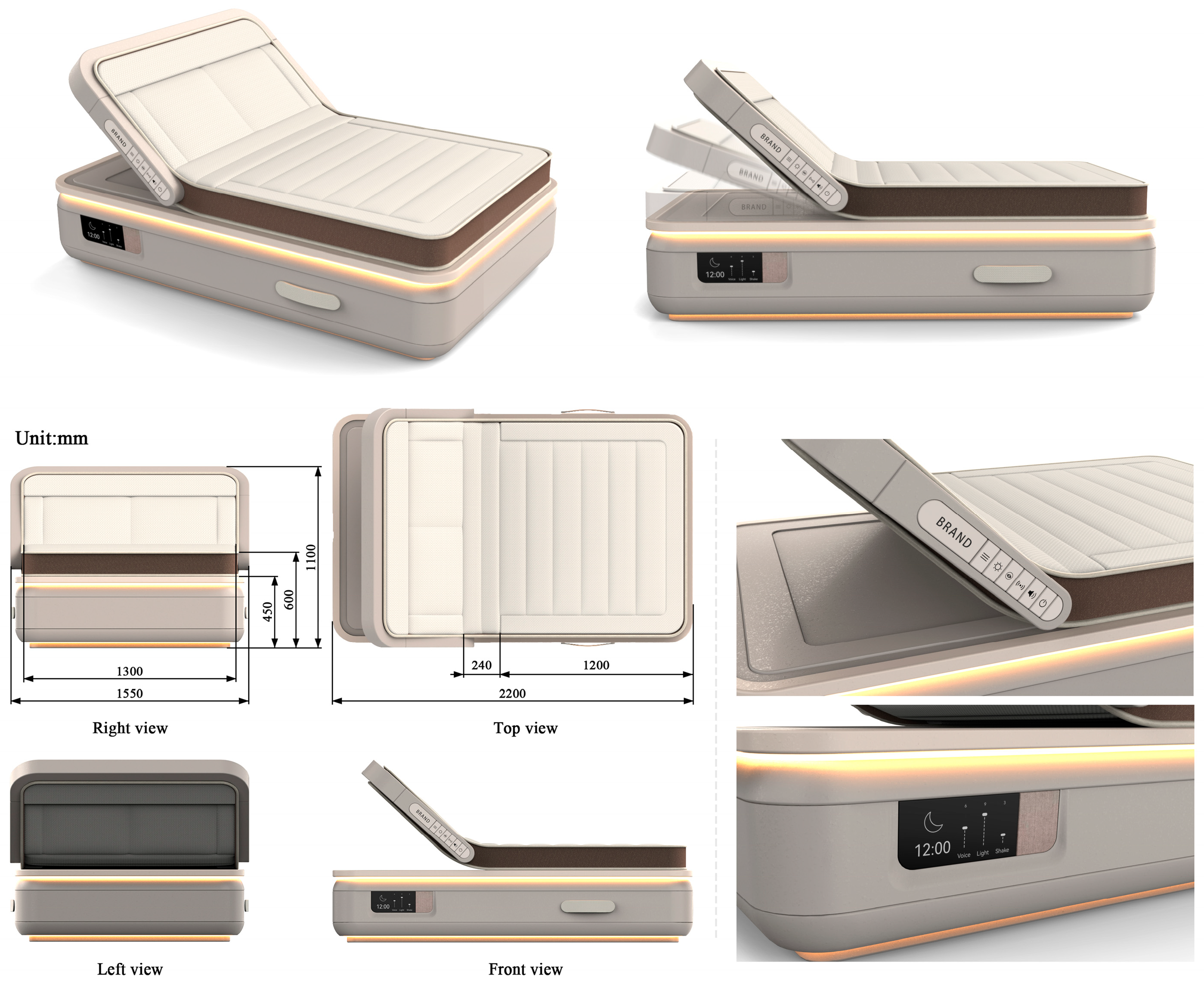
4. Discussion
Applying the preliminary research results of this paper to design practice, a comprehensive evaluation method combining AHP-QFD-AD was used. Based on the key functional requirements (FR1-FR6) and their detailed design parameters (DP1-DP6), an exploratory design study of intelligent rehabilitation products for the elderly based on multimodal theory was conducted. The specific design scheme for an intelligent rehabilitation bed was completed, and the final product renderings are shown in
Figure 3.
This intelligent rehabilitation bed is designed based on multimodal sensory experiences, providing comprehensive rehabilitation support and health monitoring for the elderly. The bed features an enhanced reinforced support structure and a high-strength alloy steel frame, ensuring excellent wear and pressure resistance. Designed with ergonomics in mind, the bed can adjust its angle and dimensions without exposing sharp edges, providing optimal comfort and safety to meet the individual needs of different elderly users. The bed integrates voice and button control systems to simplify operation steps and offers personalized functional modes such as head elevation, massage functions, and intelligent awakening. Digital intelligent technology plays a crucial role in the intelligent rehabilitation bed, with built-in bio-radar sensors for intelligent vital sign monitoring. These sensors monitor heart rate, respiration, blood pressure, and other vital signs in real-time. The monitoring data is transmitted to the cloud for centralized management, and in case of abnormalities, an alert is sent to medical staff to ensure timely medical intervention and data feedback. The bed eliminates the complex operation interfaces of conventional smart products, providing familiar button operations for the elderly and incorporating an intelligent voice rehabilitation assistant. This allows elderly users to conveniently access health reports and reminders, enhancing scientific rigor and user experience while significantly reducing the learning curve. This approach highlights innovative thinking and humanistic care in elderly care, ensuring the intelligent rehabilitation bed's outstanding performance as an age-friendly product.
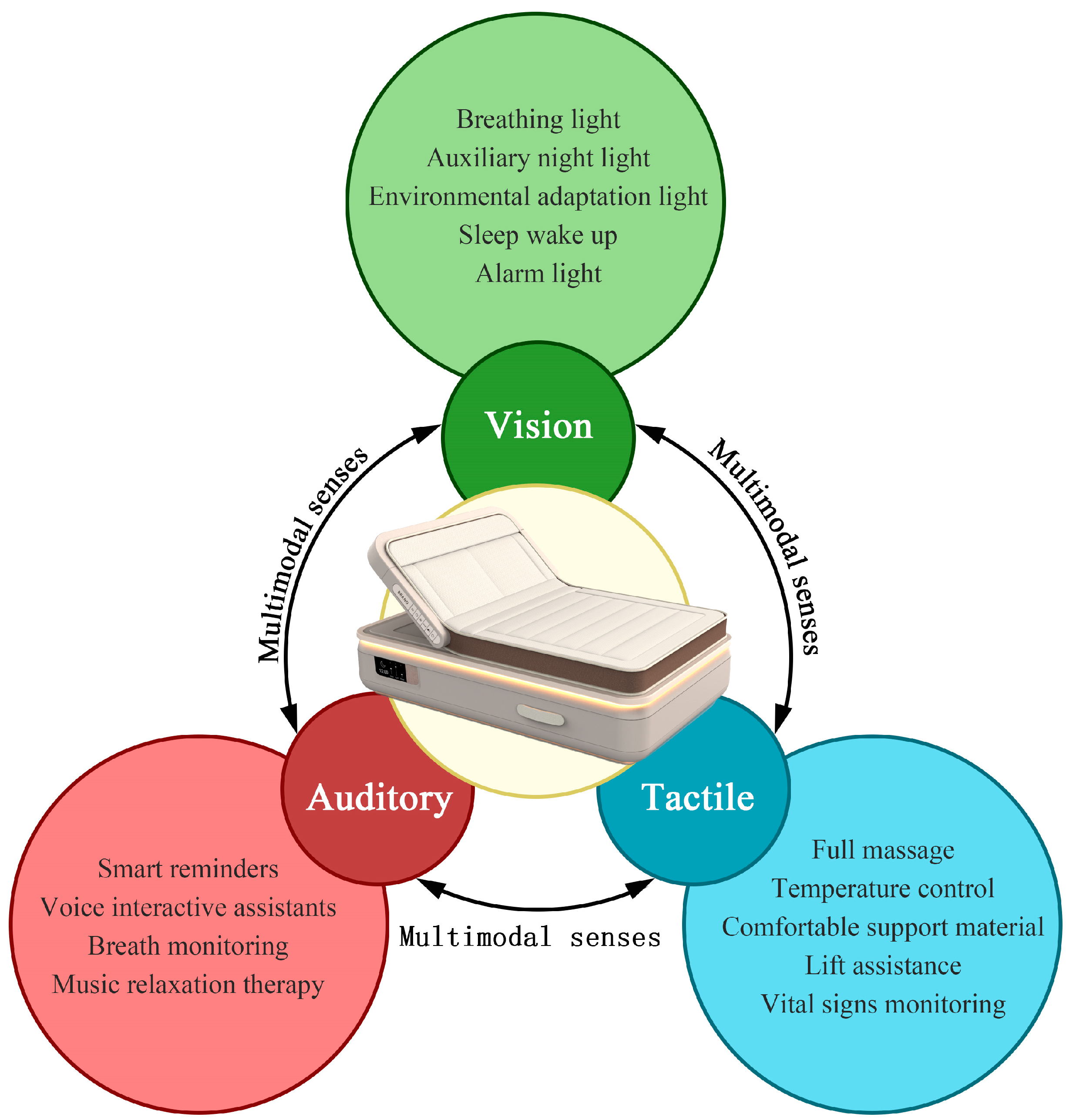
The multimodal sensory regulation function combines visual, auditory, and tactile feedback to further enhance the user experience, as shown in
Figure 4. Visually, the intelligent integrated LED lights simulate the transition between day and night through gradual light changes, helping elderly users adjust their biological clocks. Auditorily, the sound relaxation system, equipped with white noise and meditation music, helps elderly users achieve deep rest. Tactilely, the precision massage device embedded in the mattress promotes blood circulation through various tactile stimuli, providing targeted rehabilitation massages.
To verify the user satisfaction with the design scheme of the intelligent rehabilitation bed for the elderly, after outputting the design scheme, a System Usability Scale (SUS) was created. This scale provides an assessment measure of overall usability and consists of 10 questions, with odd-numbered items being positive statements and even-numbered items being negative statements[
39].The five elderly participants who were involved in the initial user research were invited again to evaluate the design scheme of the intelligent rehabilitation bed. The evaluation was conducted using images and functional explanations. The statistical results are shown in
Table 9.
The results show that the design scheme of the intelligent rehabilitation bed for the elderly has an average score of 90.5, rated as A. The product demonstrates high usability and integration. However, items 2, 7, and 9 show higher deviations, indicating that there are still some deficiencies in ease of use, learnability, and self-confidence. These areas can be optimized and improved in subsequent iterations to better meet the needs of elderly users.
5. Conclusions
The results of this study indicate that applying the AHP-QFD-AD methodology to design intelligent rehabilitation products for the elderly is effective and beneficial. The research team used the highest-weighted design parameters—enhanced reinforced support structure (4.07), high-strength alloy steel (3.96), angle adjustable and angular-free design (2.98), integrated voice and key control system (2.21), multisensory personalized regulation (1.87), and contact physiological parameter sensor (1.8)—as important bases for developing the intelligent rehabilitation bed. It integrates multimodal sensory feedback, providing comprehensive health monitoring and personalized rehabilitation plans. The combination of visual, auditory, and tactile feedback significantly improves user satisfaction and engagement, enhancing the physical and mental health of elderly users.
This methodology offers a viable framework for creating user-centered rehabilitation products that meet the comprehensive needs of elderly users, demonstrating high usability and acceptance among them. It can translate user needs into specific design requirements, ensuring that the developed products are not only functional but also user-friendly and accessible. Designers and manufacturers aiming to create effective rehabilitation solutions for the elderly should adopt this approach.
Although the current research has shown promising results, future studies should involve larger and more diverse samples of elderly users to further validate and refine the design. Additionally, continuous feedback and iteration based on user experience are crucial for improving the usability and effectiveness of rehabilitation products. By maintaining a focus on simplicity and ease of use while integrating advanced features, these products can remain accessible and beneficial to elderly users, enhancing their quality of life through effective and engaging rehabilitation solutions.
Author Contributions
Conceptualization, D.X. and X.L.; methodology, D.X. and X.L.; software, P.P.; validation, D.X. and X.L.; writing—original draft preparation, D.X.; writing—review and editing, X.L.; visualization, L.H. and D.X.; supervision, X.L.; project administration, X.L.; funding acquisition, X.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministry of Education industry-university cooperative education project, grant number 23081924595; Fujian Province Education science 14th Five-Year Plan 2023 annual topic, grant number FJJKBK23-11.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All analytical data presented in this study can be obtained by contacting the authors upon reasonable request.
Acknowledgments
The authors thank all the participants who participated in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nocera, A.; Senigagliesi, L.; Ciattaglia, G.; Raimondi, M.; Gambi, E. ML-Based Edge Node for Monitoring Peoples’ Frailty Status. Sensors 2024, 24, 4386. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Bajaj, V.; Fitzpatrick, T.; Watts, J.; Khojandi, A.; Ramdhani, R.A. Differential Responses to Low- and High-Frequency Subthalamic Nucleus Deep Brain Stimulation on Sensor-Measured Components of Bradykinesia in Parkinson’s Disease. Sensors 2024, 24, 4296. [Google Scholar] [CrossRef] [PubMed]
- Magi, C.E.; Bambi, S.; Rasero, L.; Longobucco, Y.; El Aoufy, K.; Amato, C.; Vellone, E.; Bonaccorsi, G.; Lorini, C.; Iovino, P. Health Literacy and Self-Care in Patients with Chronic Illness: A Systematic Review and Meta-Analysis Protocol. Healthcare 2024, 12, 762. [Google Scholar] [CrossRef] [PubMed]
- Kerari, A.; Bahari, G.; Alharbi, K.; Alenazi, L. The Effectiveness of the Chronic Disease Self-Management Program in Improving Patients’ Self-Efficacy and Health-Related Behaviors: A Quasi-Experimental Study. Healthcare 2024, 12, 778. [Google Scholar] [CrossRef] [PubMed]
- Nakao-Kato, M.; Izumi, S.-I.; Nishioka, S.; Momosaki, R.; Wakabayashi, H. The Relationship between Low Skeletal Muscle Mass and Subsequent Oral Intake Ability among the Aged Population. Healthcare 2023, 11, 729. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, A.; Petrica, J. The Quiet Epidemic: An Overview of Emerging Qualitative Research Trends on Sedentary Behavior in Aging Populations. Healthcare 2023, 11, 2215. [Google Scholar] [CrossRef]
- Lixandru, C.I.; Maniu, I.; Cernușcă-Mițariu, M.M.; Făgețan, M.I.; Cernușcă-Mițariu, I.S.; Domnariu, H.P.; Lixandru, G.A.; Domnariu, C.D. A Post-Implanto-Prosthetic Rehabilitation Study Regarding the Degree of Improvement in Patients’ Quality of Life: A Before–After Study. Healthcare 2024, 12, 1378. [Google Scholar] [CrossRef] [PubMed]
- Montoya-Murillo, G., Ibarretxe-Bilbao, N., Peña, J., & Ojeda, N. Effects of cognitive rehabilitation on cognition, apathy, quality of life, and subjective complaints in the elderly: a randomized controlled trial. The American Journal of Geriatric Psychiatry 2020, 28, 518-529. [CrossRef]
- Bordne, S., Rietz, C., Schulz, R. J., & Zank, S. Behavioral and emotional quality of life of patients undergoing inpatient geriatric rehabilitation. Rehabilitation Psychology 2020, 65, 299. [CrossRef]
- Franco-Urbano, M.S.; Rodríguez-Martínez, M.d.C.; García-Pérez, P. The Impact of Depression on the Functional Outcome of the Elderly Stroke Victim from a Gender Perspective: A Systematic Review. Healthcare 2022, 10, 2110. [Google Scholar] [CrossRef]
- Elsadek, M., Shao, Y., & Liu, B. Benefits of indirect contact with nature on the physiopsychological well-being of elderly people. HERD: Health Environments Research & Design Journal 2021, 14, 227-241. [CrossRef]
- Vitacca, M.; Paneroni, M.; Saleri, M.; Beccaluva, C.G. Insights into Digital MedicRehApp Maintenance Model for Pulmonary Telerehabilitation: Observational Study. Healthcare 2024, 12, 1372. [Google Scholar] [CrossRef]
- Park, E.; Lee, J.S.; Park, H.Y.; Yang, J.D.; Jung, T.-D. Effect of Serial Home-Based Exercise Immediately after Latissimus Dorsi Reconstruction in Patients with Breast Cancer. Healthcare 2022, 10, 1760. [Google Scholar] [CrossRef]
- Ju, F.; Wang, Y.; Xie, B.; Mi, Y.; Zhao, M.; Cao, J. The Use of Sports Rehabilitation Robotics to Assist in the Recovery of Physical Abilities in Elderly Patients with Degenerative Diseases: A Literature Review. Healthcare 2023, 11, 326. [Google Scholar] [CrossRef]
- McDonagh, S. T., Dalal, H., Moore, S., Clark, C. E., Dean, S. G., Jolly, K., ... & Taylor, R. S. Home-based versus centre-based cardiac rehabilitation. Cochrane database of systematic reviews 2023, (10). [CrossRef]
- Politi, L., Salerni, L., Bubbico, L., Ferretti, F., Carucci, M., Rubegni, G., & Mandalà, M. Risk of falls, vestibular multimodal processing, and multisensory integration decline in the elderly–Predictive role of the functional head impulse test. Frontiers in neurology 2022, 13, 964017. [CrossRef]
- Mathew, M., Thomas, M. J., Navaneeth, M. G., Sulaiman, S., Amudhan, A. N., & Sudheer, A. P. A systematic review of technological advancements in signal sensing, actuation, control and training methods in robotic exoskeletons for rehabilitation. Industrial Robot: the international journal of robotics research and application 2022, 50, 432-455. [CrossRef]
- Jia, G., Zhang, G., Yuan, X., Gu, X., Liu, H., Fan, Z., & Bu, L. A synthetical development approach for rehabilitation assistive smart product–service systems: A case study. Advanced Engineering Informatics 2021, 48, 101310. [CrossRef]
- Seaborn, K., Miyake, N. P., Pennefather, P., & Otake-Matsuura, M. Voice in human–agent interaction: A survey. ACM Computing Surveys (CSUR) 2021, 54(4), 1-43. [CrossRef]
- Rhee, C. E., & Choi, J. Effects of personalization and social role in voice shop**: An experimental study on product recommendation by a conversational voice agent. Computers in Human Behavior 2020, 109, 106359. [CrossRef]
- Pyo, S., Lee, J., Bae, K., Sim, S., & Kim, J. Recent progress in flexible tactile sensors for human-interactive systems: from sensors to advanced applications. Advanced Materials 2021, 33(47), 2005902. [CrossRef]
- Amoli, V., Kim, J. S., Kim, S. Y., Koo, J., Chung, Y. S., Choi, H., & Kim, D. H. Ionic tactile sensors for emerging human-interactive technologies: a review of recent progress. Advanced Functional Materials 2020, 30(20), 1904532. [CrossRef]
- Lluva-Plaza, S.; Jiménez-Martín, A.; Gualda-Gómez, D.; Villadangos-Carrizo, J.M.; García-Domínguez, J.J. Multisensory System for Long-Term Activity Monitoring to Facilitate Aging-in-Place. Sensors 2023, 23, 8646. [Google Scholar] [CrossRef]
- Yuan, J.; Zhang, L.; Kim, C.-S. Multimodal Interaction Evaluation and Optimization Design of Smart Landscape Devices for Elderly People in Seaside Parks. Electronics 2023, 12, 3822. [Google Scholar] [CrossRef]
- Bartolome, J.I.; Cho, G.; Cho, J.-D. Multi-Sensory Color Expression with Sound and Temperature in Visual Arts Appreciation for People with Visual Impairment. Electronics 2021, 10, 1336. [Google Scholar] [CrossRef]
- Marques, B.; McIntosh, J.; Valera, A.; Gaddam, A. Innovative and Assistive eHealth Technologies for Smart Therapeutic and Rehabilitation Outdoor Spaces for the Elderly Demographic. Multimodal Technol. Interact 2020, 4, 76. [Google Scholar] [CrossRef]
- Özsungur, F. A research on the effects of successful aging on the acceptance and use of technology of the elderly. Assistive Technology 2022, 34, 77–90. [Google Scholar] [CrossRef]
- Wang, J., Wang, Y., Cai, H., Zhang, J., Pan, B., Bao, G., & Guo, T. Analysis of the status quo of the Elderly’s demands of medical and elderly care combination in the underdeveloped regions of Western China and its influencing factors: a case study of Lanzhou. BMC geriatrics 2020, 20, 1-17. [CrossRef]
- Sturm, N.; Stolz, R.; Schalhorn, F.; Valentini, J.; Krisam, J.; Frick, E.; Mächler, R.; Szecsenyi, J.; Straßner, C. Self-Efficacy, Social Activity, and Spirituality in the Care of Elderly Patients with Polypharmacy in Germany—A Multicentric Cross-Sectional Study within the HoPES3 Trial. Healthcare 2021, 9, 1312. [Google Scholar] [CrossRef]
- Wu, H., Wei, Y., Miao, X., Li, X., Feng, Y., Yuan, Z., ... & **a, Q. Characteristics of balance performance in the Chinese elderly by age and gender. BMC geriatrics 2021, 21, 1-11. [CrossRef]
- Podgorica, N., Flatscher-Thöni, M., Deufert, D., Siebert, U., & Ganner, M. A systematic review of ethical and legal issues in elder care. Nursing Ethics 2021, 28, 895-910. [CrossRef]
- Hong, S.; Kim, J.-S.; Choi, Y.-A. Predictive Validity of the Johns Hopkins Fall Risk Assessment Tool for Older Patients in Stroke Rehabilitation. Healthcare 2024, 12, 791. [Google Scholar] [CrossRef]
- Bai, X.; Liu, Y.; Dai, Z.; Chen, Y.; Fang, P.; Ma, J. Determinants of Perceived Comfort: Multi-Dimensional Thinking in Smart Bedding Design. Sensors 2024, 24, 4058. [Google Scholar] [CrossRef]
- Yue, H., Zhu, T. L., Zhou, Z. J., & Zhou, T. Improvement of evaluation method of elderly family medical product design based on AHP. Mathematical Problems in Engineering 2022, 4036030. [CrossRef]
- Fang, M.; Yang, W.; Li, H.; Pan, Y. Enhancing User Experience through Optimization Design Method for Elderly Medication Reminder Mobile Applications: A QFD-Based Research Approach. Electronics 2023, 12, 2860. [Google Scholar] [CrossRef]
- Fazeli, H. R., & Peng, Q. Generation and evaluation of product concepts by integrating extended axiomatic design, quality function deployment and design structure matrix. Advanced Engineering Informatics 2022, 54, 101716. [CrossRef]
- Li, X., & Li, H. Age-appropriate design of domestic intelligent medical products: An example of smart blood glucose detector for the elderly with AHP-QFD Joint KE. Heliyon 2024, 10(5). [CrossRef]
- Briede-Westermeyer, J.C.; Pacheco-Blanco, B.; Luzardo-Briceño, M.; Pérez-Villalobos, C. Mobile Phone Use by the Elderly: Relationship between Usability, Social Activity, and the Environment. Sustainability 2020, 12, 2690. [Google Scholar] [CrossRef]
- Ureña, R.; Chiclana, F.; Gonzalez-Alvarez, A.; Herrera-Viedma, E.; Moral-Munoz, J.A. m-SFT: A Novel Mobile Health System to Assess the Elderly Physical Condition. Sensors 2020, 20, 1462. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).