Submitted:
19 July 2024
Posted:
22 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
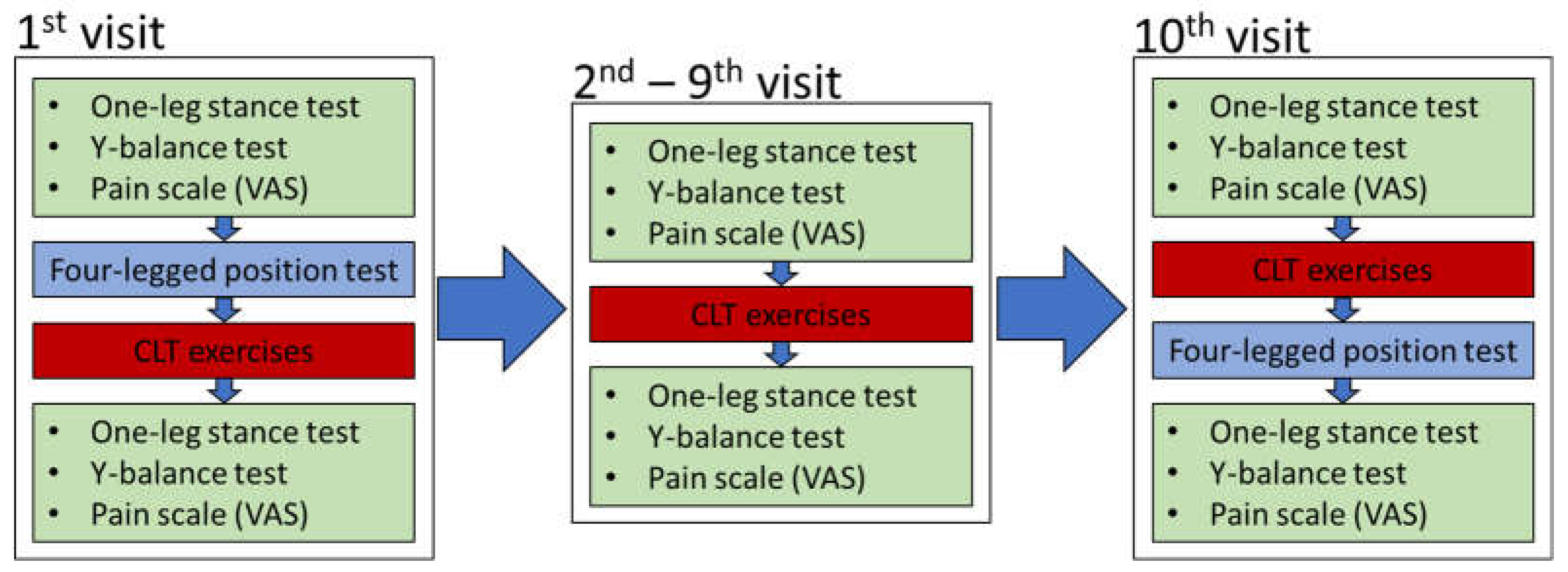
2. Materials and Methods
2.1. Test Subjects
2.2. Coordinative Locomotor Training (CLT) Exercises
2.3. Modified One-Leg Stance Test
2.4. Y-Balance Test
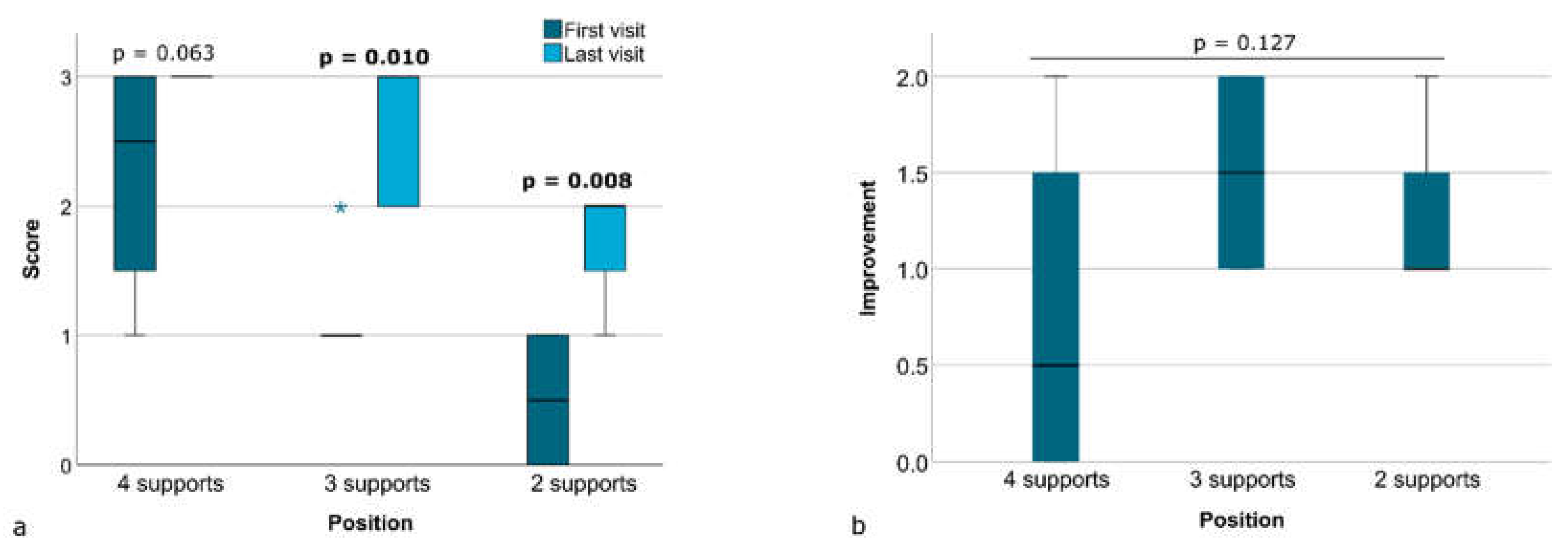
2.5. Four-Legged Position Test
2.6. Visual-Analog Scale (VAS) for Pain Evaluation
2.7. Statistical Analysis
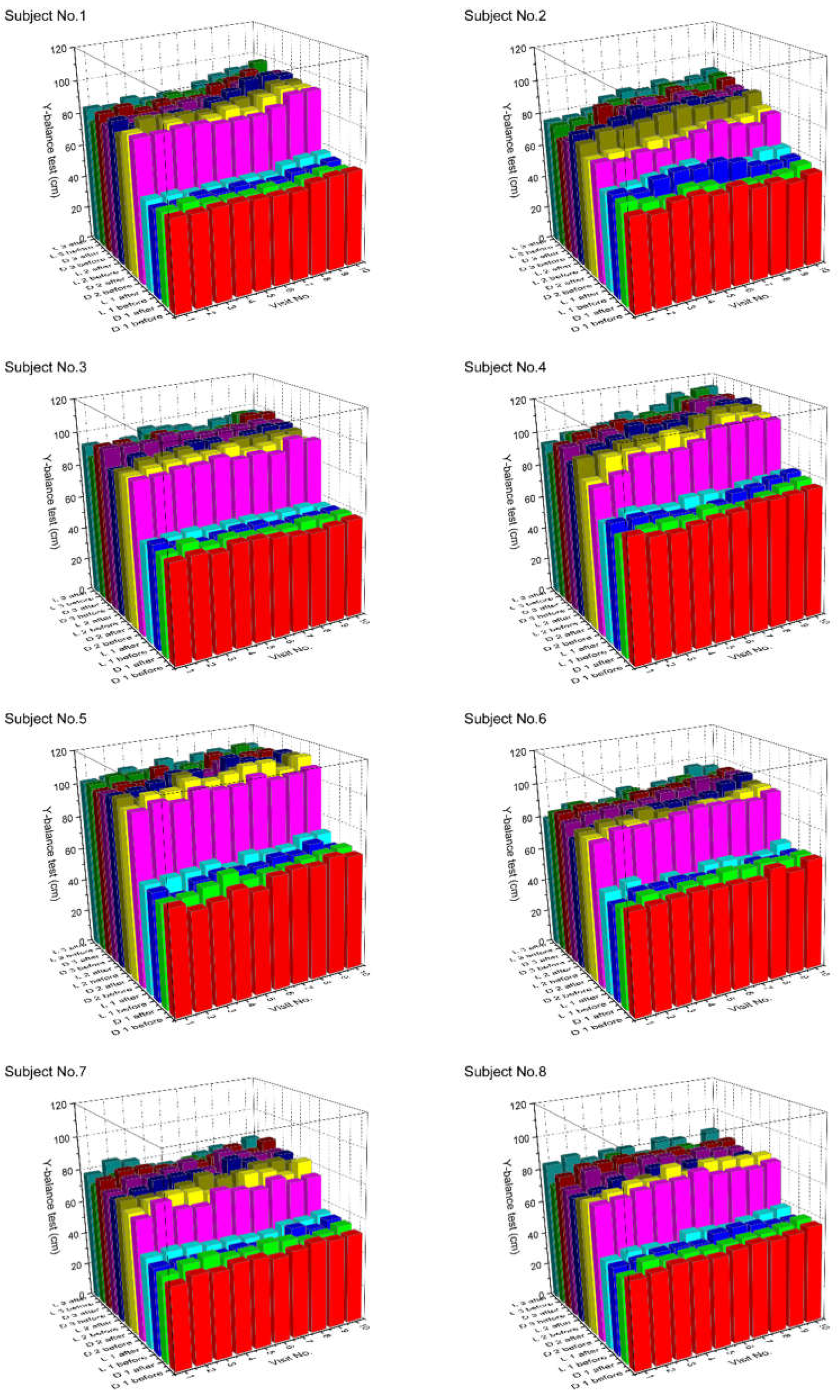
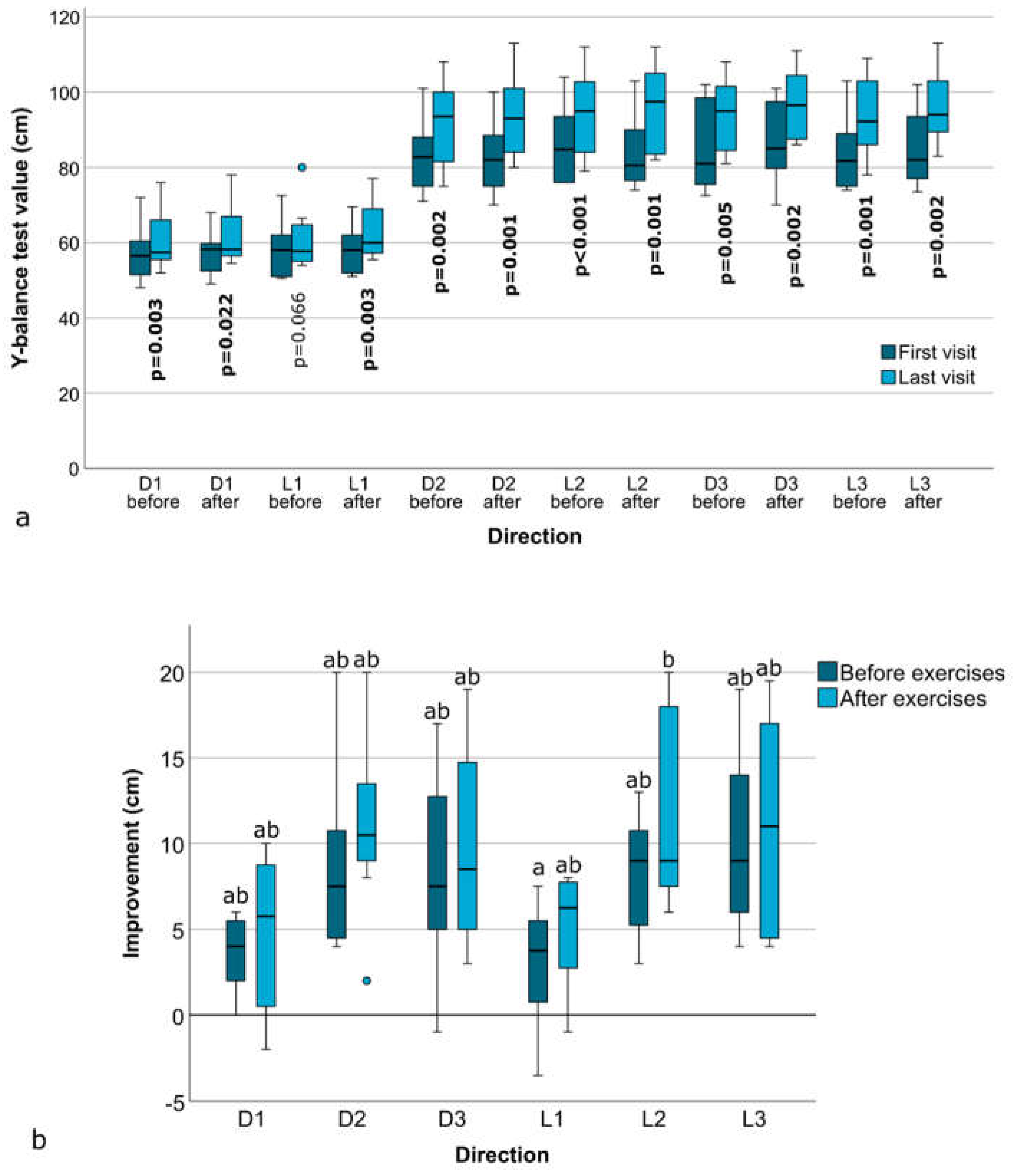
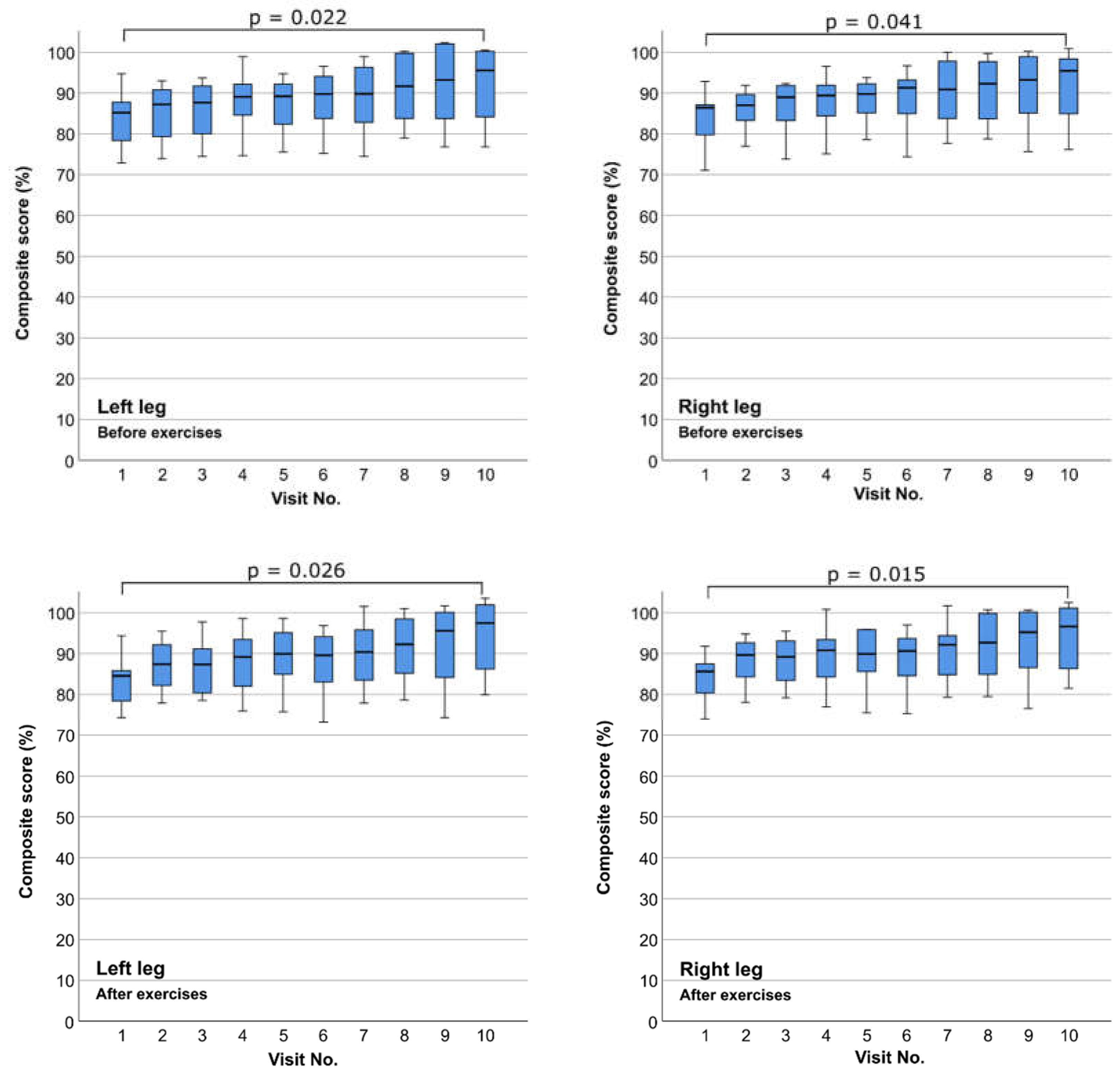
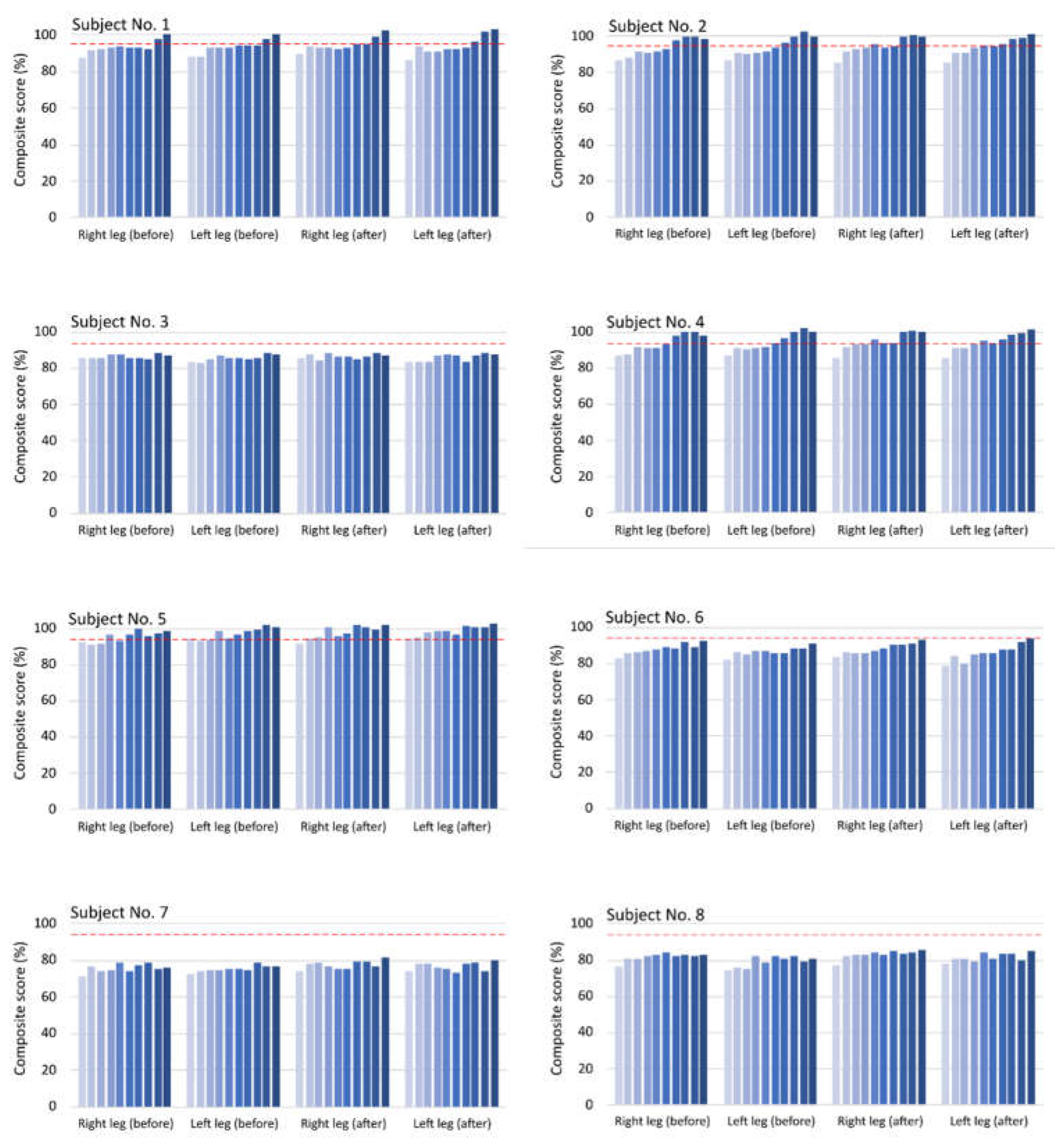
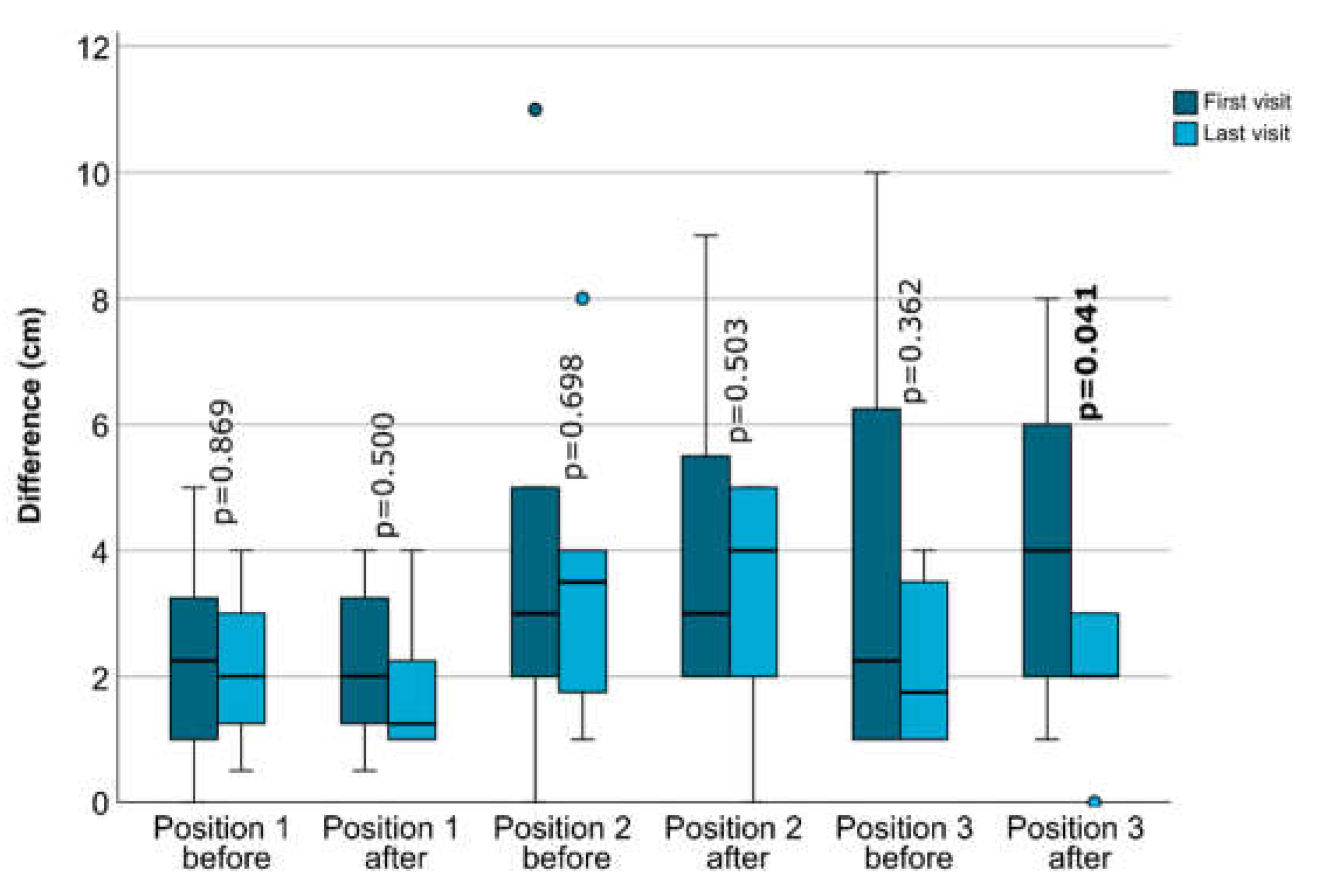
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dietz, B. PNF in Lokomotion; Springer Berlin Heidelberg: Berlin, Heidelberg, 2018; ISBN 978-3-642-27665-1.
- Jochim-Lauth, B.; Ritter, K. Komplexe Patternaddition–Coordinative Locomotor Training by Britta Dietz. Physiopraxis 2023, 21, 42–43. [CrossRef]
- Lee, H. The Effects of Coordinative Locomotor Training Using Elastic Band on Dynamic Balance and Grip Strength in Elementary School Baseball Player. Phys. Ther. Rehabil. Sci. 2021, 10, 414–420. [CrossRef]
- Kim, T.; Kim, S. The Effects of a Coordinative Locomotor Training Program on the Functional Movement Screen Scores of Badminton Players. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2016, 14, 23–32. [CrossRef]
- Kim, J. The Effect of Balance Exercise on Postural Control and Shooting Record in Archers. Korean J. Sport Biomech. 2008, 18, 65–74. [CrossRef]
- Lee, K.; Kim, S. The Effects of Combined Training on the Physical Fitness of Male Short Distance Athletes-A Case Study. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2019, 17, 177–187. [CrossRef]
- Kim, T.-Y. The Effect of Strengthening Exercise Using the Sprinter/Skater Patterns. J. Korean Proprioceptive Neuromuscul. Facil. Assoc. 2006, 4, 71–79.
- Jeong, W.-S.; Jeong, J.-Y.; Kim, C.-K.; Jung, D.-I.; Kim, K.-Y. Effect of Lower Limb Muscle Activity on Balancing through Sprinter Patterns of PNF. J. Korea Contents Assoc. 2011, 11, 281–292. [CrossRef]
- Ann, Y.D.; Jong, H.P. The Effects of PNF Combined Patterns Training on Balance Ability and Functional Ability of Hockey Players. J. Digit. Converg. 2013, 11, 521–528.
- Jeon, J.-K. The Effects of Combination Patterns Exercise of Proprioceptive Neuromuscular Facilitation on Balance in Chronic Low Back Pain Elderly Patients. J. Digit. Converg. 2013, 11, 361–368.
- Lim, J.-H.; Lee, M.-K.; Kim, T.-Y.; Ko, H.-E. The Combination of PNF Patterns for Coordinative Locomotor Training. J. Korean Proprioceptive Neuromuscul. Facil. Assoc. 2013, 11, 17–25.
- Cho, H.-S.; Shin, H.-S.; Bang, D.-H. The Effects of Upper and Lower Limb Coordinated Exercise of PNF for Balance in Elderly Woman. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2015, 13, 189–196.
- Cho, H.-S.; Cha, H.-G.; Shin, H.-S. The Effects of PNF Upper- and Lower Limb Coordinated Exercise on the Balancing and Walking-Abilities in Stroke Patients. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2017, 15, 27–33. [CrossRef]
- Choi, J.-W.; Hwang, S.-P. A Comparison between Integrated Patterns of PNF and Bowling Exercises. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2015, 13, 89–93. [CrossRef]
- Choi, W.; Seo, T. The Effects of PNF Skater Pattern on the Balance in Stroke Patients. J. Korea Entertain. Ind. Assoc. 2015, 9, 289–298. [CrossRef]
- Kim, J.; Choi, W.; Seo, T. Effect of Proprioceptive Neuromuscular Facilitation Integration Pattern and Swiss Ball Training on Pain and Balance in Elderly Patients with Chronic Back Pain. J. Phys. Ther. Sci. 2015, 27, 3237–3240. [CrossRef]
- Hwang, S.; Maeng, G.; Kim, J.; Jung, C. The Effects of Coordinative Locomotion Training Using the PNF Pattern on Walking in Patients with Spinal Cord Injury. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2016, 14, 67–74. [CrossRef]
- Kim, Y.; Lee, H. Effects of Skater and Sprinter Combined Pattern in PNF on Muscle Contraction Onset Time and Muscle Activation of Trunk Muscle. Arch. Orthop. Sports Phys. Ther. 2018, 14, 55–64. [CrossRef]
- Pyo, A.; Kim, S.; Kim, T.; Na, E.; Eom, M.; Jeon, Y.; Jo, E.; Jo, H.; Kim, J. Changes of Dynamic Balance and Flexibility after Skater and Sprinter Pattern. J. Korean Clin. Health Sci. 2016, 4, 644–651. [CrossRef]
- Kim, H.; Choi, J.; Cho, Y. The Effect of Upper and Lower Extremity Coordination Training with Elastic Band on Balance and Functional Ability for Chronic Stroke Patients. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2019, 17, 119–127. [CrossRef]
- Park, M.; Lee, D.; Jeong, M. The Effect of Coordinative Locomotor Training on Physical Factors for Falls in the Elderly with Mild Cognitive Impairment. Korean Soc. Phys. Med. 2020, 15, 65–73. [CrossRef]
- Cho, W.; Park, S.; Choi, A. The Effect of Coordinative Locomotor Training with Elastic Band on Balance and Flexibility in Elementary School Baseball Players. J. Korea Converg. Soc. 2019, 10, 261–266.
- Ko, H.; Song, H.; Jeon, B. Effects of Functional Taping and CLT Program on the Fall Efficacy and Balance of Stroke Patients with Knee Pain on the Non-Affected Side. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2016, 14, 203–208. [CrossRef]
- Hwang, J.; Park, J.; Lim, J. Effects of Coordinative Locomotor Training Program on Low Extremity Strength, Balance and Quality of Life in Patients with Cancer: Single-Subject Design. J. Korean Soc. Phys. Med. 2017, 12, 47–59. [CrossRef]
- Kim, J.; Lim, J. The Effects of Coordinative Locomotor Training on Coordination and Gait in Chronic Stroke Patients: A Randomized Controlled Pilot Trial. J. Exerc. Rehabil. 2018, 14, 1010–1016. [CrossRef]
- Lim, J.; Jang, H.; Cho, W.; Park, S. The Effects of Coordinative Locomotor Training Combined with Climbing on the Trunk Muscles in Adults. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2018, 16, 397–404. [CrossRef]
- Kim, J.; Kim, T.; Lee, J. Effect of Coordinative Locomotor Training on Balance and Plantar Foot Pressure in Scoliosis Patients -A Single Subject Study. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2017, 15, 227–236. [CrossRef]
- Lim, J.; Park, S. The Effects of Coordinative Locomotor Training on Balance in Patients with Chronic Stroke: Meta-Analysis of Studies in Korea. J. Korean Phys. Ther. Sci. 2020, 27, 36–47. [CrossRef]
- Lee, S.; Bae, S.; Kim, K. The Effect of Pressure Belt during PNF Sprinter Pattern Training Using Thera-Band on Leg Muscle Strength and Gait in Stroke Patients: One-Group Pretest-Post Test Design. J. Korean Acad. Orthop. Man. Phys. Ther. 2021, 27, 63–73.
- Kim, J.; Lee, M.; Lee, J.; Ko, H. The Effect of Coordinative Locomotor Training on Walking in a Chronic Stroke Patient-A Single Subject Design. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2018, 16, 7–17. [CrossRef]
- Kim, K.; Lee, D.; Jung, S. Effect of Coordination Movement Using the PNF Pattern Underwater on the Balance and Gait of Stroke Patients. J. Phys. Ther. Sci. 2015, 27, 3699–3701. [CrossRef]
- Kim, J.; Oh, E. Effect of Coordinative Locomotor Training on Spine Appearance and Quality of Life in Patients with Idiopathic Scoliosis: Single Subject Study. Korean Soc. Phys. Med. 2021, 16, 89–97. [CrossRef]
- Lee, S.; Kim, H.; Jung, J.; Lee, S. Immediate Effects of Sprinter-Pattern Exercise on the Lordotic Curve and Abdominal Muscle Activity in Individuals with Hyperlordosis. Medicina (Mex.) 2023, 59, 2177. [CrossRef]
- Noh, H.; Kim, S. Comparative Study on the Effects of Proprioceptive Neuromuscular Facilitation and Elastic Band Exercise on the Physical Function and Blood Lipid Levels of Obese Elderly Women. Phys. Ther. Korea 2015, 22, 79–92. [CrossRef]
- Lee, J.; Kim, J. Effect of Coordinative Locomotor Training on Postural Imbalance and Gait in Children: A Single Subject Design. J. Korean Soc. Phys. Med. 2019, 14, 63–71. [CrossRef]
- Lim, J.; Kuk, E.; Kim, J. Change of Foot Pressure Distributions on Stance Leg during Coordinative Locomotor Training in Healthy Adults. Korean Soc. Phys. Med. 2023, 18, 59–66. [CrossRef]
- Kim, G.; Yi, D.; Yim, J. Effect of Sprinter Pattern Bridging Exercise Using Theraband on Activation of Lower Extremity and Abdominal Muscle. Phys. Ther. Rehabil. Sci. 2021, 10, 244–250. [CrossRef]
- Lee, H. The Effect of Coordinative Locomotor Training Using Elastic Band on Pain, Muscle Strength, Dynamic Balance and Muscle Activity of Female College Students with Patellofemoral Pain Syndrome. J. Korean Phys. Ther. Sci. 2023, 30, 59–71. [CrossRef]
- Springer, B.A.; Marin, R.; Cyhan, T.; Roberts, H.; Gill, N.W. Normative Values for the Unipedal Stance Test with Eyes Open and Closed. J. Geriatr. Phys. Ther. 2007, 30, 8–15. [CrossRef]
- Michikawa, T.; Nishiwaki, Y.; Takebayashi, T.; Toyama, Y. One-Leg Standing Test for Elderly Populations. J. Orthop. Sci. 2009, 14, 675–685. [CrossRef]
- Fratti Neves, L.; Quadros de Suoza, C.; Martins Picasso, C. The Y Balance Test – How and Why to Do It? Int. Phys. Med. Rehabil. J. 2017, 2. [CrossRef]
- Hébert-Losier, K. Clinical Implications of Hand Position and Lower Limb Length Measurement Method on Y-Balance Test Scores and Interpretations. J. Athl. Train. 2017, 52, 910–917. [CrossRef]
- Park, S.; Park, C.; Kim, Y. The Effects of Coordinative Locomotor Training with Elastic Bands on the Body Alignment of Elementary School Baseball Players. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2019, 17, 411–419. [CrossRef]
- Ko, H.; Jeon, B.; Song, H. Effects of Coordinative Locomotor Training Program on Balance and Gait of Stroke Patients. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2017, 15, 247–252. [CrossRef]
- Alnahdi, A.H.; Alderaa, A.A.; Aldali, A.Z.; Alsobayel, H. Reference Values for the Y Balance Test and the Lower Extremity Functional Scale in Young Healthy Adults. J. Phys. Ther. Sci. 2015, 27, 3917–3921. [CrossRef]
- Plisky, P.J.; Gorman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The Reliability of an Instrumented Device for Measuring Components of the Star Excursion Balance Test. North Am. J. Sports Phys. Ther. NAJSPT 2009, 4, 92–99.
- Choi, J.; Kim, Y.; Lee, S. The Effects of the Combined Patterns of Proprioceptive Neuromuscular Facilitation on Static Balance. J. Korea Proprioceptive Neuromuscul. Facil. Assoc. 2008, 6, 1–2.
- Kim, S.; Yu, S.; Park, S. Effect of CLT and Sling Exercise Combined Program on Knee Pain in Patellofemoral Pain Patient: A Single-Subject Study. J. Korean Acad. Orthop. Man. Phys. Ther. 2019, 25, 73–81.
- Jeong, M. The Effect of Coordinative Locomotor Training Using Elastic Bands on the Flexibility and Body Alignment of Elementary School Right-Handed Baseball Players. J. Korean Phys. Ther. 2021, 33, 217–223.
- Lee, J.; Kim, J. The Coordinative Locomotor Training Intervention Strategy Using the Icf Tool to Improve the Standing Posture in Scoliosis: A Case Report. J. Korean Phys. Ther. 2021, 33, 7–15. [CrossRef]
| Visit No. / Approach |
Position | Pattern | Activity level |
|---|---|---|---|
|
1 Hands on |
Four-legged position 4 contact points* Four-legged position 3 contact points* Four-legged position 2 contact points* Supine |
Sprinter/skater Sprinter/skater Sprinter/skater Sprinter/skater |
Securing Linking Linking Securing/linking |
|
2 Hands on |
Sitting High sitting |
Sprinter/skater Sprinter/skater |
Securing/linking Securing/linking |
|
3 Hands on |
Bear stand 4 contact points Bear stand 3 contact points Bear stand 2 contact points |
Sprinter/skater Sprinter/skater Sprinter/skater |
Securing Securing/linking Securing/linking |
|
4 Hands on |
Hook lying Bridging Supine |
Chopping Chopping Lifting |
Securing/linking Securing Securing/linking |
|
5 Hands on |
Supine Hook lying One-leg bridging |
Chopping Sprinter/skater+ Sprinter/skater+ |
Securing/linking Securing/linking+ Securing/linking+ |
|
6 Hands on |
Half-edge seat Standing position with arm support on the table |
Chopping Sprinter/skater |
Securing/linking Securing/linking |
|
7 Hands on |
Four-legged position 4 contact points Four-legged position 3 contact points Four-legged position 2 contact points (head leaning on the wall) Side lying |
Sprinter/skater Sprinter/skater Sprinter/skater Sprinter/skater |
Securing Linking Linking Linking |
|
8 Hands on |
Hook lying One-leg bridging |
Sprinter/skater+ Sprinter/skater+ Sprinter/skater+ |
Linking+ Linking+ Controlling+ |
|
9 Hands off |
Standing | Sprinter/skater Sprinter/skater/chopping Sprinter/skater CLT dance |
Securing Linking Controlling Integration |
|
10 Hands off |
Standing Four-legged position 4 contact points* Four-legged position 3 contact points* Four-legged position 2 contact points* |
Sprinter/skater+ Sprinter/skater/chopping+ Sprinter/skater+ CLT dance+ Sprinter/skater Sprinter/skater Sprinter/skater |
Securing+ Linking+ Controlling+ Integration+ Securing Linking Linking |
| Position No. | Position consists of four-legged stance with: | Scoring criteria (for each position) The subject is able to hold the position against resistance on the scapula and ischial tuberosity: |
Score |
|---|---|---|---|
| 1 | Four supports |
|
3 |
| 2 | Three supports with arm or leg movement in sprinter/skater pattern |
|
2 |
| 3 | Two supports with arm and leg movement in sprinter/skater pattern |
|
1 |
|
0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




