Submitted:
11 July 2024
Posted:
12 July 2024
Read the latest preprint version here
Abstract
Keywords:
Introduction
- A.
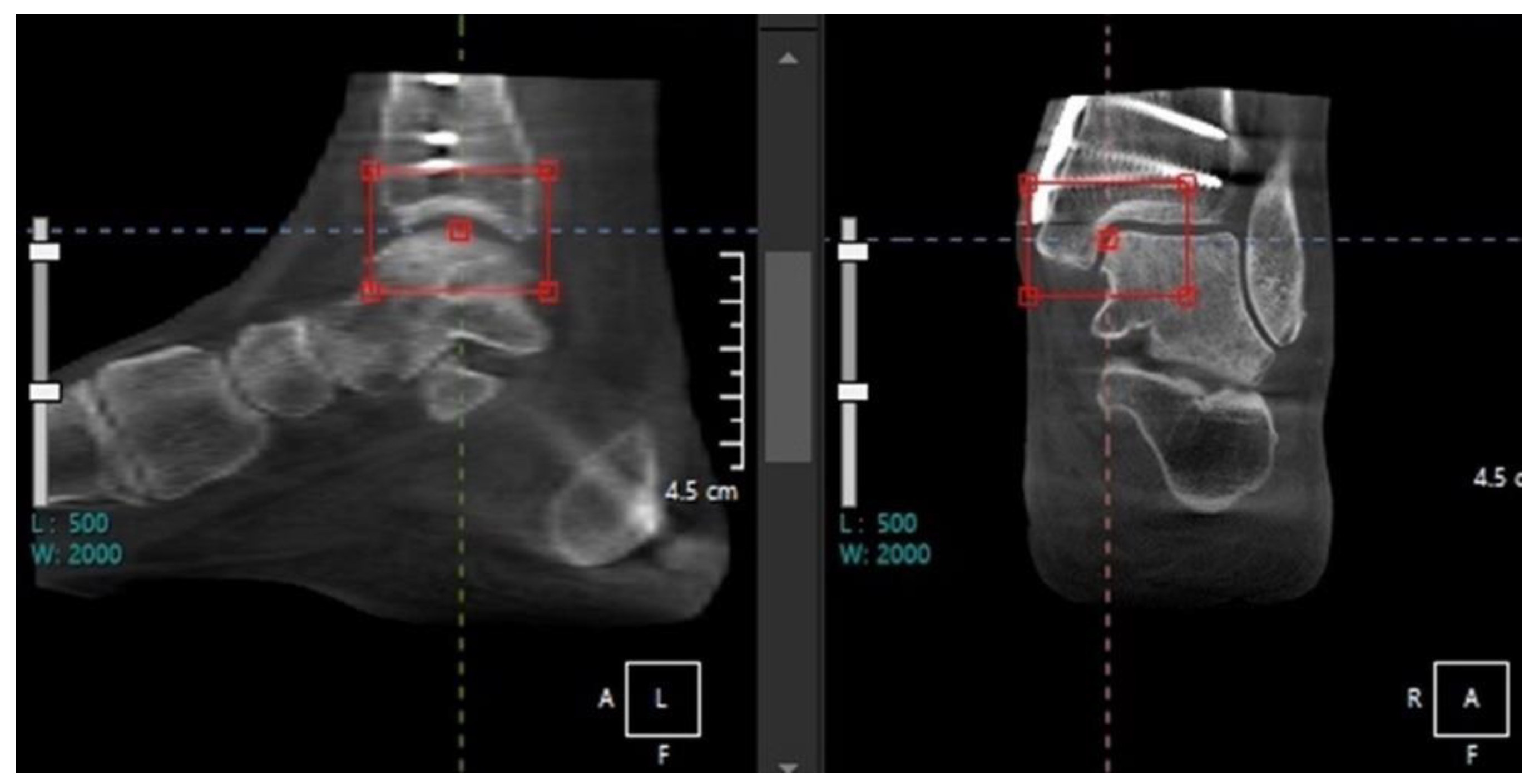
- Normal anatomy
- B.
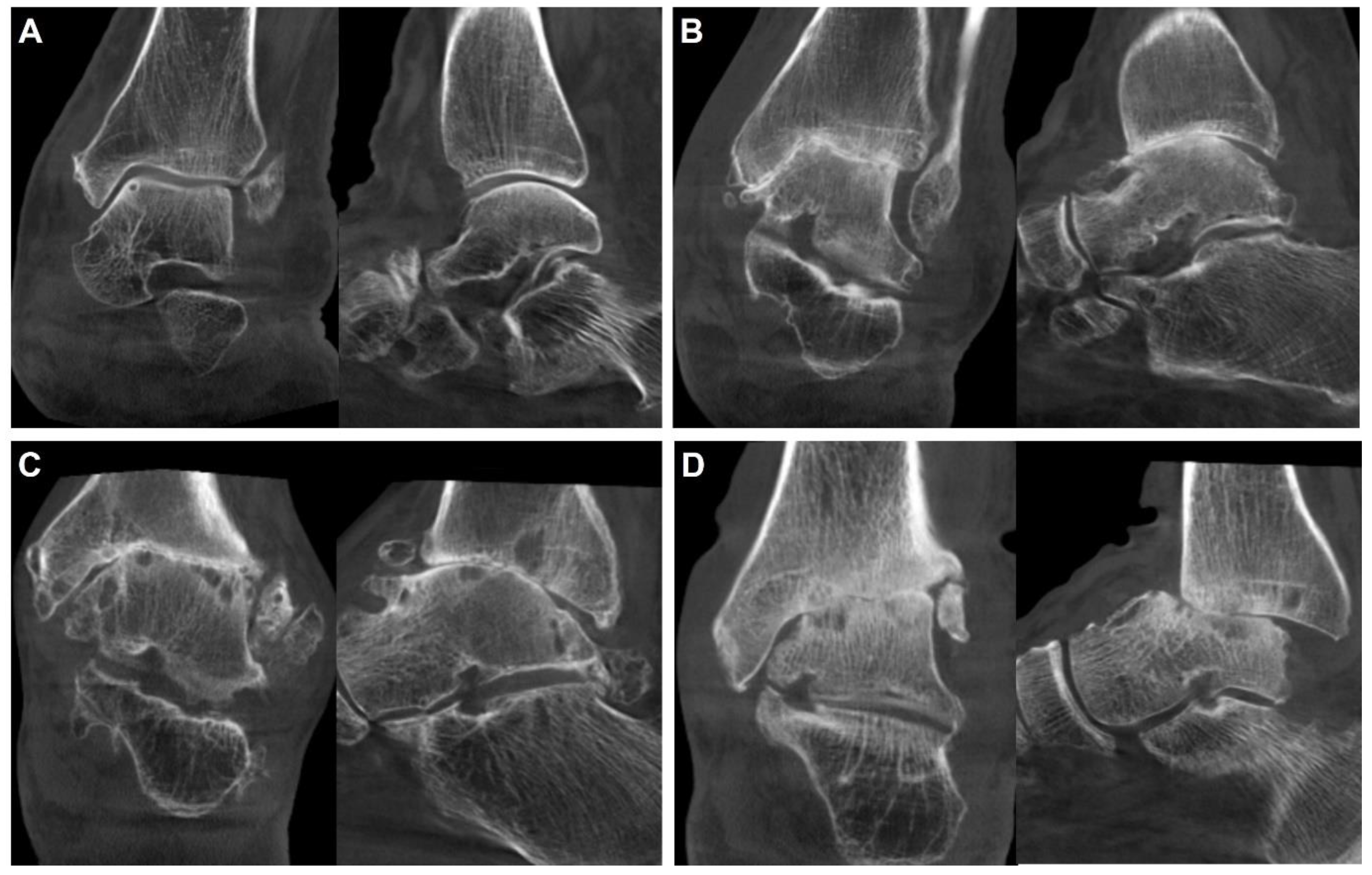
- Ankle Osteoarthritis
Diagnosis
Classification
Treatment
- a)
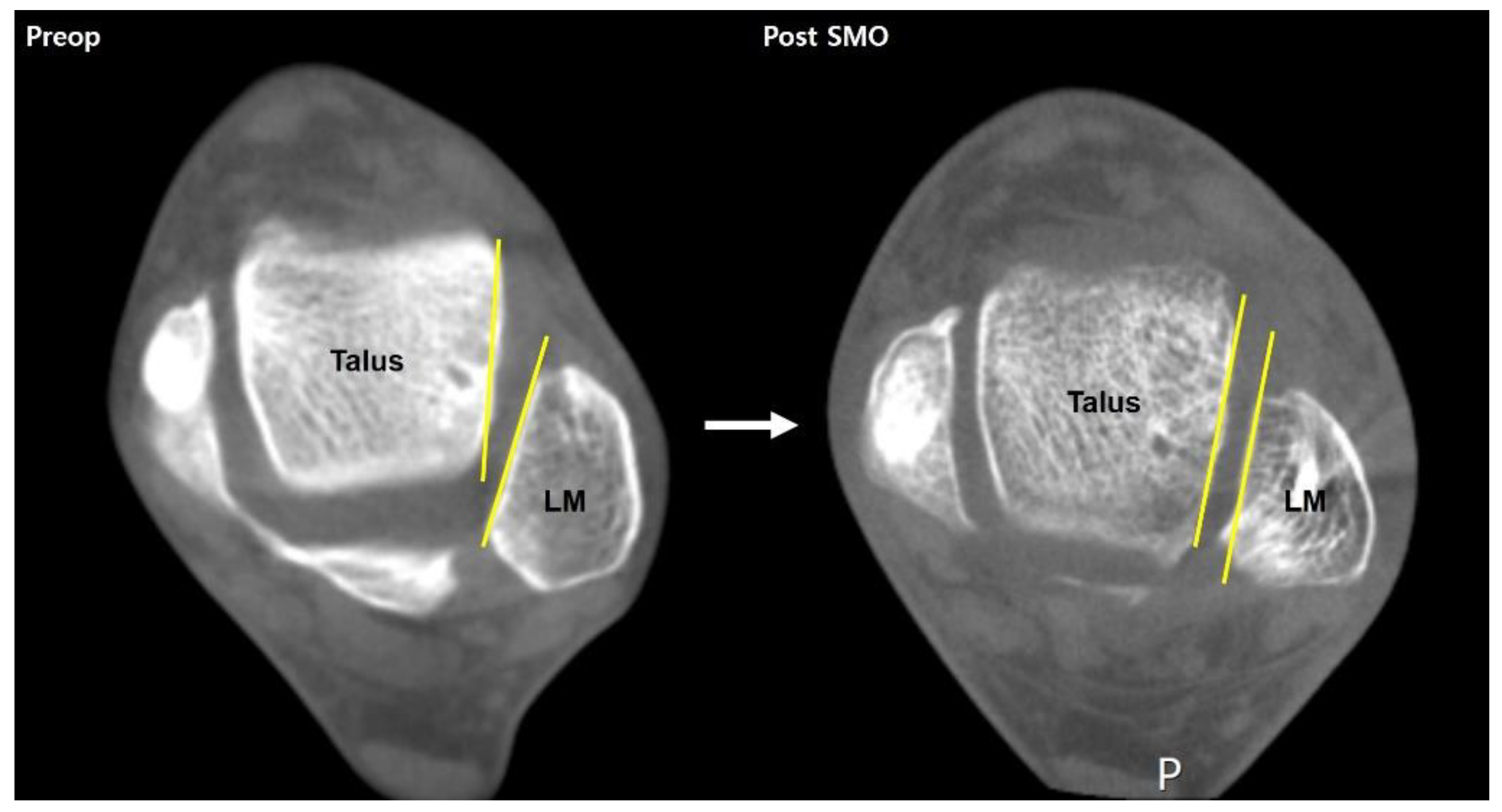
- Deformity correction surgery
- b)
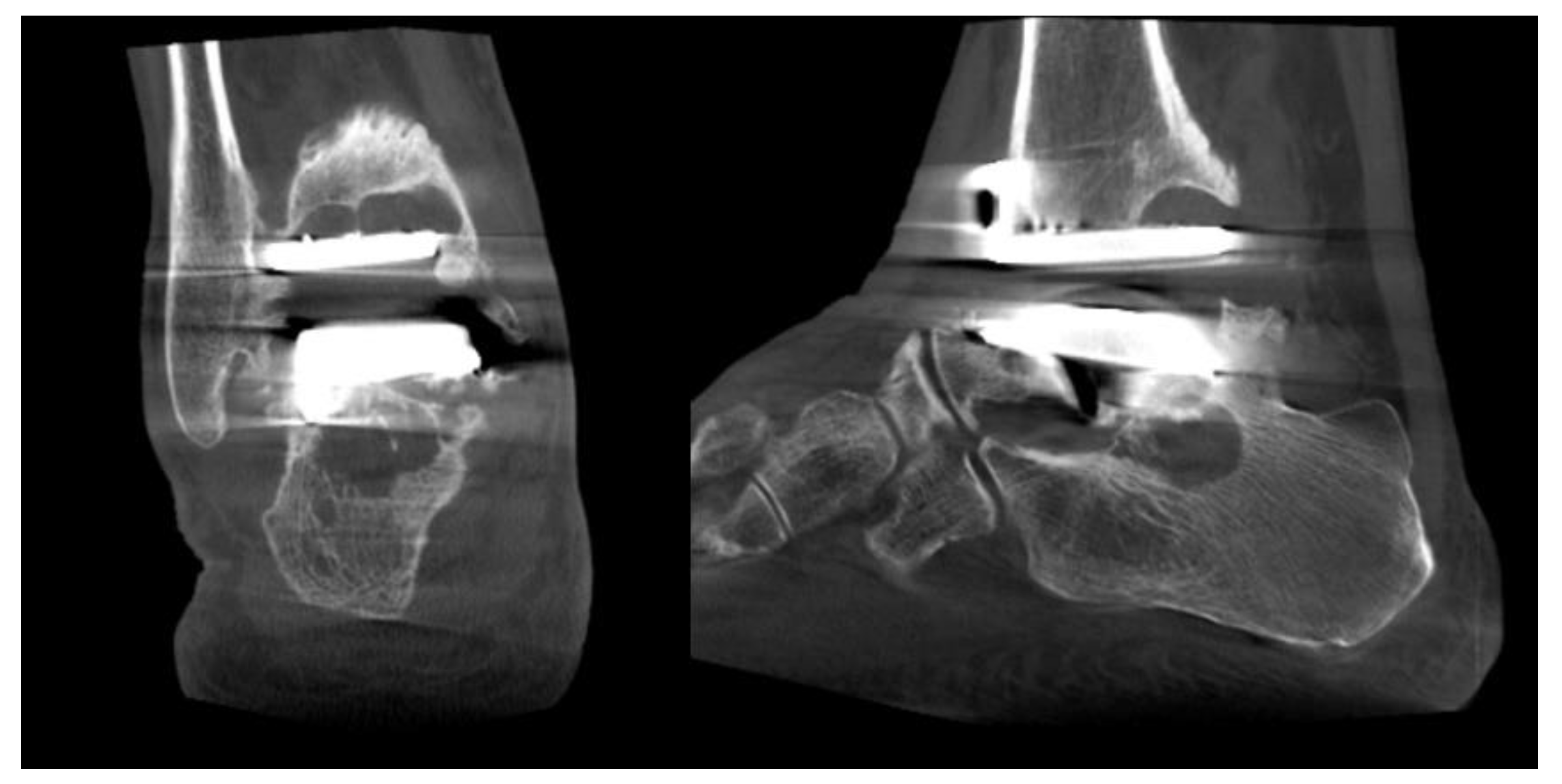
- Ankle replacement surgery
- A.
- Syndesmosis injury
- B.
- Osteochondral lesion of talus
- C.
- Chronic ankle instability
- D.
- Acute ankle sprain
Conclusion
References
- Barg, A.; Bailey, T.; Richter, M.; de Cesar Netto, C.; Lintz, F.; Burssens, A.; Phisitkul, P.; Hanrahan, C.J.; Saltzman, C.L. Weightbearing Computed Tomography of the Foot and Ankle: Emerging Technology Topical Review. Foot Ankle Int 2018, 39, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Lintz, F.; de Cesar Netto, C.; Barg, A.; Burssens, A.; Richter, M. Weight-bearing cone beam CT scans in the foot and ankle. EFORT Open Rev 2018, 3, 278–286. [Google Scholar] [CrossRef]
- Kang, D.H.; Kang, C.; Hwang, D.S.; Song, J.H.; Song, S.H. The value of axial loading three dimensional (3D) CT as a substitute for full weightbearing (standing) 3D CT: Comparison of reproducibility according to degree of load. Foot Ankle Surg 2019, 25, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Kang, C.; Kim, T.G.; Lee, G.S.; Lee, J.K.; Ahn, K.J.; Kim, D.H.; Lee, S.W. Perioperative axial loading computed tomography findings in varus ankle osteoarthritis: Effect of supramalleolar osteotomy on abnormal internal rotation of the talus. Foot Ankle Surg 2021, 27, 217–223. [Google Scholar] [CrossRef]
- Richter, M.; Lintz, F.; de Cesar Netto, C.; Barg, A.; Burssens, A. Results of more than 11,000 scans with weightbearing CT - Impact on costs, radiation exposure, and procedure time. Foot Ankle Surg 2020, 26, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Lepojärvi, S.; Niinimäki, J.; Pakarinen, H.; Koskela, L.; Leskelä, H.V. Rotational Dynamics of the Talus in a Normal Tibiotalar Joint as Shown by Weight-Bearing Computed Tomography. J Bone Joint Surg Am 2016, 98, 568–575. [Google Scholar] [CrossRef]
- Colin, F.; Horn Lang, T.; Zwicky, L.; Hintermann, B.; Knupp, M. Subtalar joint configuration on weightbearing CT scan. Foot Ankle Int 2014, 35, 1057–1062. [Google Scholar] [CrossRef]
- Richter, M.; Lintz, F.; Zech, S.; Meissner, S.A. Combination of PedCAT Weightbearing CT With Pedography Assessment of the Relationship Between Anatomy-Based Foot Center and Force/Pressure-Based Center of Gravity. Foot Ankle Int 2018, 39, 361–368. [Google Scholar] [CrossRef]
- Tazegul, T.E.; Anderson, D.D.; Barbachan Mansur, N.S.; Kajimura Chinelati, R.M.; Iehl, C.; VandeLune, C.; Ahrenholz, S.; Lalevee, M.; de Cesar Netto, C. An Objective Computational Method to Quantify Ankle Osteoarthritis From Low-Dose Weightbearing Computed Tomography. Foot Ankle Orthop 2022, 7, 24730114221116805. [Google Scholar] [CrossRef]
- Kim, J.B.; Yi, Y.; Kim, J.Y.; Cho, J.H.; Kwon, M.S.; Choi, S.H.; Lee, W.C. Weight-bearing computed tomography findings in varus ankle osteoarthritis: abnormal internal rotation of the talus in the axial plane. Skeletal Radiol 2017, 46, 1071–1080. [Google Scholar] [CrossRef]
- Willey, M.C.; Compton, J.T.; Marsh, J.L.; Kleweno, C.P.; Agel, J.; Scott, E.J.; Bui, G.; Davison, J.; Anderson, D.D. Weight-Bearing CT Scan After Tibial Pilon Fracture Demonstrates Significant Early Joint-Space Narrowing. J Bone Joint Surg Am 2020, 102, 796–803. [Google Scholar] [CrossRef]
- Turmezei, T.D.; Malhotra, K.; MacKay, J.W.; Gee, A.H.; Treece, G.M.; Poole, K.E.S.; Welck, M.J. 3-D joint space mapping at the ankle from weight-bearing CT: reproducibility, repeatability, and challenges for standardisation. Eur Radiol 2023, 33, 8333–8342. [Google Scholar] [CrossRef]
- Barg, A.; Amendola, R.L.; Henninger, H.B.; Kapron, A.L.; Saltzman, C.L.; Anderson, A.E. Influence of Ankle Position and Radiographic Projection Angle on Measurement of Supramalleolar Alignment on the Anteroposterior and Hindfoot Alignment Views. Foot Ankle Int 2015, 36, 1352–1361. [Google Scholar] [CrossRef]
- Bernasconi, A.; Cooper, L.; Lyle, S.; Patel, S.; Cullen, N.; Singh, D.; Welck, M. Intraobserver and interobserver reliability of cone beam weightbearing semi-automatic three-dimensional measurements in symptomatic pes cavovarus. Foot Ankle Surg 2020, 26, 564–572. [Google Scholar] [CrossRef]
- Krähenbühl, N.; Tschuck, M.; Bolliger, L.; Hintermann, B.; Knupp, M. Orientation of the Subtalar Joint: Measurement and Reliability Using Weightbearing CT Scans. Foot Ankle Int 2016, 37, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.W.; Kim, D.Y.; Park, G.Y.; Lee, D.O.; Lee, D.Y. Coronal plane Calcaneal-Talar Orientation in Varus Ankle Osteoarthritis. Foot Ankle Int 2022, 43, 928–936. [Google Scholar] [CrossRef]
- TAKAKURA, Y. The Treatment for Osteoarthritis of Ankle Joint. Japanese Journal of Rheumatism and Joint Surgery 1986, 5, 347–352. [Google Scholar]
- Kim, J.B.; Park, C.H.; Ahn, J.Y.; Kim, J.; Lee, W.C. Characteristics of medial gutter arthritis on weightbearing CT and plain radiograph. Skeletal Radiol 2021, 50, 1575–1583. [Google Scholar] [CrossRef] [PubMed]
- Holzer, N.; Salvo, D.; Marijnissen, A.C.; Vincken, K.L.; Ahmad, A.C.; Serra, E.; Hoffmeyer, P.; Stern, R.; Lübbeke, A.; Assal, M. Radiographic evaluation of posttraumatic osteoarthritis of the ankle: the Kellgren-Lawrence scale is reliable and correlates with clinical symptoms. Osteoarthritis Cartilage 2015, 23, 363–369. [Google Scholar] [CrossRef]
- Krause, F.G.; Di Silvestro, M.; Penner, M.J.; Wing, K.J.; Glazebrook, M.A.; Daniels, T.R.; Lau, J.T.; Stothers, K.; Younger, A.S. Inter- and intraobserver reliability of the COFAS end-stage ankle arthritis classification system. Foot Ankle Int 2010, 31, 103–108. [Google Scholar] [CrossRef]
- Richter, M.; de Cesar Netto, C.; Lintz, F.; Barg, A.; Burssens, A.; Ellis, S. The Assessment of Ankle Osteoarthritis with Weight-Bearing Computed Tomography. Foot Ankle Clin 2022, 27, 13–36. [Google Scholar] [CrossRef] [PubMed]
- Hintermann, B.; Knupp, M.; Barg, A. Supramalleolar Osteotomies for the Treatment of Ankle Arthritis. J Am Acad Orthop Surg 2016, 24, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.J.; Azam, M.T.; Weiss, M.B.; Kennedy, J.G.; Walls, R.J. Supramalleolar osteotomy for the treatment of ankle osteoarthritis leads to favourable outcomes and low complication rates at mid-term follow-up: a systematic review. Knee Surg Sports Traumatol Arthrosc 2023, 31, 701–715. [Google Scholar] [CrossRef] [PubMed]
- Knupp, M.; Stufkens, S.A.; van Bergen, C.J.; Blankevoort, L.; Bolliger, L.; van Dijk, C.N.; Hintermann, B. Effect of supramalleolar varus and valgus deformities on the tibiotalar joint: a cadaveric study. Foot Ankle Int 2011, 32, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Burssens, A.; Susdorf, R.; Krähenbühl, N.; Peterhans, U.; Ruiz, R.; Barg, A.; Hintermann, B. Supramalleolar Osteotomy for Ankle Varus Deformity Alters Subtalar Joint Alignment. Foot Ankle Int 2022, 43, 1194–1203. [Google Scholar] [CrossRef]
- Faict, S.; Burssens, A.; Van Oevelen, A.; Maeckelbergh, L.; Mertens, P.; Buedts, K. Correction of ankle varus deformity using patient-specific dome-shaped osteotomy guides designed on weight-bearing CT: a pilot study. Arch Orthop Trauma Surg 2023, 143, 791–799. [Google Scholar] [CrossRef]
- Lee, G.W.; Wang, S.H.; Lee, K.B. Comparison of Intermediate to Long-Term Outcomes of Total Ankle Arthroplasty in Ankles with Preoperative Varus, Valgus, and Neutral Alignment. J Bone Joint Surg Am 2018, 100, 835–842. [Google Scholar] [CrossRef]
- Pugely, A.J.; Lu, X.; Amendola, A.; Callaghan, J.J.; Martin, C.T.; Cram, P. Trends in the use of total ankle replacement and ankle arthrodesis in the United States Medicare population. Foot Ankle Int 2014, 35, 207–215. [Google Scholar] [CrossRef]
- Yasutomi, M.; An, V.V.G.; Xu, J.; Wines, A.; Sivakumar, B.S.; Symes, M.J. Trends in the use of ankle arthrodesis and total ankle replacements in Australia over the past 20 years. Eur J Orthop Surg Traumatol 2024, 34, 1997–2001. [Google Scholar] [CrossRef]
- Tapaninaho, K.; Ponkilainen, V.T.; Haapasalo, H.; Mattila, V.M.; Huttunen, T.T.; Repo, J.P. Incidence of ankle arthrodesis and total ankle replacement between 1997 and 2018: A nationwide registry study in Finland. Foot Ankle Surg 2023, 29, 288–292. [Google Scholar] [CrossRef]
- Tucker, W.A.; Barnds, B.L.; Morris, B.L.; Tarakemeh, A.; Mullen, S.; Schroeppel, J.P.; Vopat, B.G. Nationwide Analysis of Total Ankle Replacement and Ankle Arthrodesis in Medicare Patients: Trends, Complications, and Cost. Foot Ankle Spec 2022, 15, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.H.; Daniels, T.R. Ankle arthritis. J Bone Joint Surg Am 2003, 85, 923–936. [Google Scholar] [CrossRef] [PubMed]
- Cody, E.A.; Scott, D.J.; Easley, M.E. Total Ankle Arthroplasty: A Critical Analysis Review. JBJS Rev 2018, 6, e8. [Google Scholar] [CrossRef] [PubMed]
- SooHoo, N.F.; Zingmond, D.S.; Ko, C.Y. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg Am 2007, 89, 2143–2149. [Google Scholar] [CrossRef]
- Goldberg, A.J.; Chowdhury, K.; Bordea, E.; Hauptmannova, I.; Blackstone, J.; Brooking, D.; Deane, E.L.; Bendall, S.; Bing, A.; Blundell, C.; et al. Total Ankle Replacement Versus Arthrodesis for End-Stage Ankle Osteoarthritis: A Randomized Controlled Trial. Ann Intern Med 2022, 175, 1648–1657. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Merchan, E.C.; Moracia-Ochagavia, I. Results of Total Ankle Arthroplasty Versus Ankle Arthrodesis. Foot Ankle Clin 2024, 29, 27–52. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.J.; Consul, D.; Umbel, B.D.; Berlet, G.C. Accuracy of Weightbearing CT Scans for Patient-Specific Instrumentation in Total Ankle Arthroplasty. Foot Ankle Orthop 2021, 6, 24730114211061493. [Google Scholar] [CrossRef] [PubMed]
- Zeitlin, J.; Henry, J.; Ellis, S. Preoperative Guidance With Weight-Bearing Computed Tomography and Patient-Specific Instrumentation in Foot and Ankle Surgery. Hss j 2021, 17, 326–332. [Google Scholar] [CrossRef]
- de Cesar Netto, C.; Day, J.; Godoy-Santos, A.L.; Roney, A.; Barbachan Mansur, N.S.; Lintz, F.; Ellis, S.J.; Demetracopoulos, C.A. The use of three-dimensional biometric Foot and Ankle Offset to predict additional realignment procedures in total ankle replacement. Foot Ankle Surg 2022, 28, 1029–1034. [Google Scholar] [CrossRef]
- Vale, C.; Almeida, J.F.; Pereira, B.; Andrade, R.; Espregueira-Mendes, J.; Gomes, T.M.; Oliva, X.M. Complications after total ankle arthroplasty- A systematic review. Foot Ankle Surg 2023, 29, 32–38. [Google Scholar] [CrossRef]
- Glazebrook, M.A.; Arsenault, K.; Dunbar, M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int 2009, 30, 945–949. [Google Scholar] [CrossRef]
- Lawton, C.D.; Prescott, A.; Butler, B.A.; Awender, J.F.; Selley, R.S.; Dekker Ii, R.G.; Balderama, E.S.; Kadakia, A.R. Modern total ankle arthroplasty versus ankle arthrodesis: A systematic review and meta-analysis. Orthop Rev (Pavia) 2020, 12, 8279. [Google Scholar] [CrossRef] [PubMed]
- Lintz, F.; Mast, J.; Bernasconi, A.; Mehdi, N.; de Cesar Netto, C.; Fernando, C.; Buedts, K. 3D, Weightbearing Topographical Study of Periprosthetic Cysts and Alignment in Total Ankle Replacement. Foot Ankle Int 2020, 41, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chun, D.I.; Kim, J.; Kim, Y.S.; Cho, J.H.; Won, S.H.; Park, S.Y.; Yi, Y. Relationship between fracture morphology of lateral malleolus and syndesmotic stability after supination-external rotation type ankle fractures. Injury 2019, 50, 1382–1387. [Google Scholar] [CrossRef] [PubMed]
- Dikos, G.D.; Heisler, J.; Choplin, R.H.; Weber, T.G. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma 2012, 26, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, J.H.; Kwon, H.W.; Lee, M.; Kim, D.; Choi, Y.J.; Park, K.R.; Lee, S.; Cho, J. Normal Distal Tibiofibular Syndesmosis Assessment Using Postmortem Computed Tomography (PMCT). Diagnostics (Basel) 2023, 14. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Fang, M.; Van Oevelen, A.; Peiffer, M.; Audenaert, E.; Burssens, A. Diagnostic applications and benefits of weightbearing CT in the foot and ankle: A systematic review of clinical studies. Foot Ankle Surg 2024, 30, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Hagemeijer, N.C.; Chang, S.H.; Abdelaziz, M.E.; Casey, J.C.; Waryasz, G.R.; Guss, D.; DiGiovanni, C.W. Range of Normal and Abnormal Syndesmotic Measurements Using Weightbearing CT. Foot Ankle Int 2019, 40, 1430–1437. [Google Scholar] [CrossRef] [PubMed]
- Krähenbühl, N.; Bailey, T.L.; Weinberg, M.W.; Davidson, N.P.; Hintermann, B.; Presson, A.P.; Allen, C.M.; Henninger, H.B.; Saltzman, C.L.; Barg, A. Is load application necessary when using computed tomography scans to diagnose syndesmotic injuries? A cadaver study. Foot Ankle Surg 2020, 26, 198–204. [Google Scholar] [CrossRef]
- Krähenbühl, N.; Bailey, T.L.; Weinberg, M.W.; Davidson, N.P.; Hintermann, B.; Presson, A.P.; Allen, C.M.; Henninger, H.B.; Saltzman, C.L.; Barg, A. Impact of Torque on Assessment of Syndesmotic Injuries Using Weightbearing Computed Tomography Scans. Foot Ankle Int 2019, 40, 710–719. [Google Scholar] [CrossRef]
- Shamrock, A.; Den Hartog, T.J.; Dowley, K.; Day, J.; Barbachan Mansur, N.S.; Carvalho, K.A.M.; de Cesar Netto, C.; O'Malley, M. Normal Values for Distal Tibiofibular Syndesmotic Space With and Without Subject-Driven External Rotation Stress. Foot Ankle Int 2024, 45, 80–85. [Google Scholar] [CrossRef]
- Bhimani, R.; Ashkani-Esfahani, S.; Lubberts, B.; Guss, D.; Hagemeijer, N.C.; Waryasz, G.; DiGiovanni, C.W. Utility of Volumetric Measurement via Weight-Bearing Computed Tomography Scan to Diagnose Syndesmotic Instability. Foot Ankle Int 2020, 41, 859–865. [Google Scholar] [CrossRef] [PubMed]
- Walley, K.C.; Gonzalez, T.A.; Callahan, R.; Fairfull, A.; Roush, E.; Saloky, K.L.; Juliano, P.J.; Lewis, G.S.; Aynardi, M.C. The Role of 3D Reconstruction True-Volume Analysis in Osteochondral Lesions of the Talus: A Case Series. Foot Ankle Int 2018, 39, 1113–1119. [Google Scholar] [CrossRef]
- Yasui, Y.; Hannon, C.P.; Fraser, E.J.; Ackermann, J.; Boakye, L.; Ross, K.A.; Duke, G.L.; Shimozono, Y.; Kennedy, J.G. Lesion Size Measured on MRI Does Not Accurately Reflect Arthroscopic Measurement in Talar Osteochondral Lesions. Orthop J Sports Med 2019, 7, 2325967118825261. [Google Scholar] [CrossRef]
- Siegler, S.; Konow, T.; Belvedere, C.; Ensini, A.; Kulkarni, R.; Leardini, A. Analysis of surface-to-surface distance mapping during three-dimensional motion at the ankle and subtalar joints. J Biomech 2018, 76, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Dibbern, K.N.; Li, S.; Vivtcharenko, V.; Auch, E.; Lintz, F.; Ellis, S.J.; Femino, J.E.; de Cesar Netto, C. Three-Dimensional Distance and Coverage Maps in the Assessment of Peritalar Subluxation in Progressive Collapsing Foot Deformity. Foot Ankle Int 2021, 42, 757–767. [Google Scholar] [CrossRef]
- Efrima, B.; Dahmen, J.; Barbero, A.; Benady, A.; Maccario, C.; Indino, C.; Kerkhoffs, G.; Usuelli, F.G. Enhancing precision in osteochondral lesions of the talus measurements and improving agreement in surgical decision-making using weight-bearing computed tomography and distance mapping. Knee Surg Sports Traumatol Arthrosc 2024. [Google Scholar] [CrossRef]
- Van Bergeyk, A.B.; Younger, A.; Carson, B. CT analysis of hindfoot alignment in chronic lateral ankle instability. Foot Ankle Int 2002, 23, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Lintz, F.; Bernasconi, A.; Baschet, L.; Fernando, C.; Mehdi, N.; de Cesar Netto, C. Relationship Between Chronic Lateral Ankle Instability and Hindfoot Varus Using Weight-Bearing Cone Beam Computed Tomography. Foot Ankle Int 2019, 40, 1175–1181. [Google Scholar] [CrossRef]
- Lintz, F.; Bernasconi, A.; Ferkel, E.I. Can Weight-Bearing Computed Tomography Be a Game-Changer in the Assessment of Ankle Sprain and Ankle Instability? Foot Ankle Clin 2023, 28, 283–295. [Google Scholar] [CrossRef]
- Fuller, R.M.; Kim, J.; An, T.W.; Rajan, L.; Cororaton, A.D.; Kumar, P.; Deland, J.T.; Ellis, S.J. Assessment of Flatfoot Deformity Using Digitally Reconstructed Radiographs: Reliability and Comparison to Conventional Radiographs. Foot Ankle Int 2022, 43, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Jacques, T.; Morel, V.; Dartus, J.; Badr, S.; Demondion, X.; Cotten, A. Impact of introducing extremity cone-beam CT in an emergency radiology department: A population-based study. Orthop Traumatol Surg Res 2021, 107, 102834. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Schilke, R.; Duerr, F.; Zech, S.; Andreas Meissner, S.; Naef, I. Automatic software-based 3D-angular measurement for Weight-Bearing CT (WBCT) provides different angles than measurement by hand. Foot Ankle Surg 2022, 28, 863–871. [Google Scholar] [CrossRef]
- Richter, M.; Zech, S.; Naef, I.; Duerr, F.; Schilke, R. Automatic software-based 3D-angular measurement for weight-bearing CT (WBCT) is valid. Foot Ankle Surg 2024. [Google Scholar] [CrossRef]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




