Introduction
Impaired kidney function in CLL patients can significantly impact overall health and survival. Common factors contributing to renal dysfunction in CLL include sepsis, dehydration, tumor lysis syndrome, compression of the ureter by enlarged lymph nodes, and side effects of cancer therapy. Renal involvement in CLL is rare, affecting approximately 7.5% of diagnosed patients according to a study conducted at the Mayo Clinic [
2]. These patients tended to be older, male, and have advanced CLL. They were also less likely to receive certain treatments and more likely to receive others. During follow-up, about 16% of patients experienced acute kidney injury, associated with age, gender, and specific CLL characteristics. Another study from the Mayo Clinic found that kidney disease in CLL patients was associated with poorer outcomes, including lower overall survival rates [
1]. However, due to the indolent nature of CLL and its prevalence among elderly individuals who often have pre-existing renal issues, kidney biopsies are rarely performed. In fact, only about 1.2% of CLL patients in the study by Strati et al. underwent a kidney biopsy [
1]. The lack of biopsy data makes it challenging to fully understand the underlying causes of renal dysfunction in CLL patients.
Case Presentation
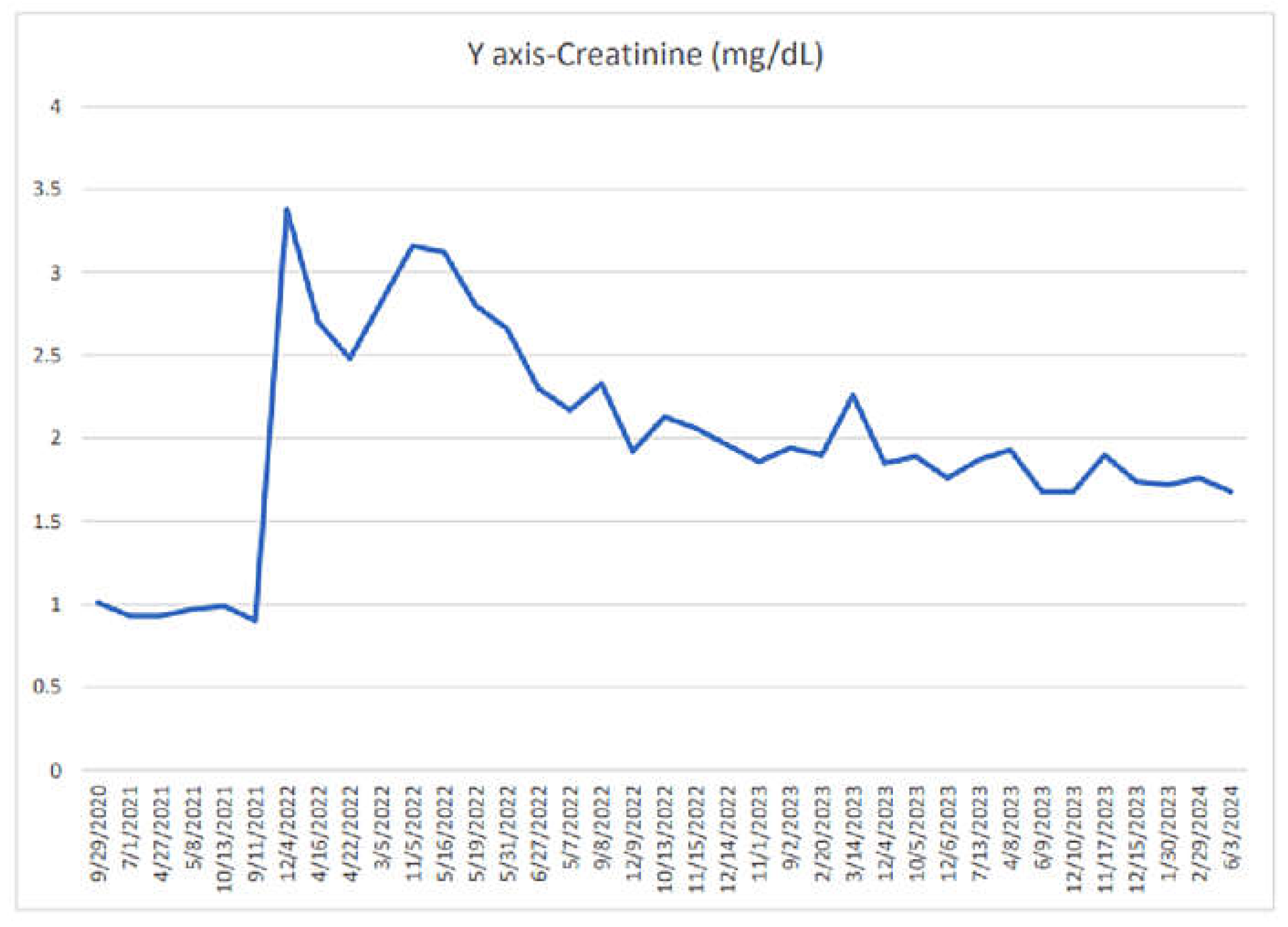
A 67-year-old female with a history of Chronic Lymphocytic Leukemia (CLL) was diagnosed in 2012. CLL is characterized by Trisomy 12, unmutated IGVH, and positive markers including Zap 70 and CD38. The patient was asymptomatic on diagnosis, was under surveillance until 2019. In April 2019 as she started experiencing fatigue, rapid lymphocyte doubling time, and thrombocytopenia, treatment with Ibrutinib and Rituximab was given until April 2022. However, in April 2022, she developed acute kidney injury, with a peak creatinine level of 3.5. Preliminary work-up including tumor lysis labs which were negative and CT scan of the Abdomen and Pelvis was unremarkable with no extrinsic or intrinsic obstruction noted on the renal drainage system. Renal biopsy was pursued as a further investigative step revealing extensive diffuse lymphoid infiltration of the kidney by monoclonal B cells consistent with CLL and 2nd review of pathology was done at the Mayo Clinic, confirming the Renal infiltration of the CLL.
Subsequently, the treatment regimen was switched to Venetoclax and Obinutuzumab in June 2022. She completed six cycles of Obinutuzumab by November 2022, and continued Venetoclax with good tolerance until August 2023, with significant recovery of the renal function to creatinine of 1.6. The patient remains asymptomatic currently, prompting surveillance by Hematology and Nephrology being off Venetoclax per current guidelines [
3]. Laboratory monitoring with CBC, CMP monthly, the Flow cytometry quarterly. With careful avoidance of nephrotoxic medications and encouraging adequate hydration. If renal function worsens post-Venetoclax discontinuation, resumption of therapy is being considered.
Figure 1.
Discussion
Renal involvement in CLL is uncommon, occurring in less than 5% of cases, and typically presents with nonspecific symptoms such as fatigue and renal dysfunction. Diagnosis often requires a renal biopsy, revealing lymphoid infiltration like ours. CLL is an indolent disease, not all patients need to be treated.
Figure 2 defines various indications of treatment in patients with CLL, Renal failure when noted in a patient with CLL should be thoroughly evaluated to rule out differentials like Sepsis. dehydration, nephrotoxic medication use, tumor lysis syndrome, with the help of a thorough history, exam, medication review, complete blood count, and comprehensive metabolic panel to check for electrolytes. If the preliminary work-up is unrevealing, further investigation with imaging is necessary and
Nephrology consultation is also required as many of the cancer therapies have a comprehensive list of side effects which need a multidisciplinary approach. CLL renal infiltration is very rare. Accurate incidence is ill-defined, as the number of patients who 2 of 4 received renal biopsies as part of the CLL workup is low historically(2), as it is very difficult to discern the etiology of renal dysfunction in CLL in the elderly given baseline CKD. Hence it should be considered in the list of differentials and an appropriate workup with renal biopsy is required to make the diagnosis. Once proven that renal failure is secondary to CLL, appropriate treatment must be initiated.
Before treatment initiation FISH profiling of the tumor is necessary for risk stratification. Based on the presence or absence of del (17p)/TP53 mutation stratify the agents of choice used for the treatment of CLL. Our case was negative for (17p)/TP53 mutation upon the FISH testing [
1,
4].
Figure 2 lists the first-line treatment choices for low and intermediate risk. This list is constantly evolving as there is a tremendous amount of research that’s ongoing on patients with CLL. When our patient got started on the treatment Ibrutinib + Rituximab [
5] was the preferred combination of choice, but down the lane, as she got diagnosed with renal infiltration of the CLL, Venetoclax + Obinutuzumab mab [
6] became a category 1 combination. Management of CLL in patients with renal dysfunction can be of challenge, given the high risk for TLS and the requiring dose reductions of the cancer therapy [
7], frequent monitoring of CMP, uric acid, and aggressive support from nephrology colleagues and along with the use of prophylactic Allopurinol. A meticulous medication review with the help of a pharmacist is required to avoid drug interactions. [8]. Although most CLL medications aren’t known to harm the kidneys, some like Venetoclax and ibrutinib were the most linked to acute kidney injury (AKI). However, newer-generation Bruton Tyrosine Kinase Inhibitors (BTKi) have fewer kidney-related side effects compared to Ibrutinib. The precise reasons behind AKI and other kidney issues with these drugs aren’t entirely clear, but there have been reports of acute interstitial nephritis with ibrutinib, as well as a notable association between ibrutinib and hypertension, which can persist despite treatment. Adhering to strict dosing protocols and promptly addressing any side effects is crucial for ensuring safe and effective treatment outcomes.
Conclusions
In CLL, renal failure can be a consequence of tumor infiltration, glomerular diseases, electrolyte imbalances, and treatment-related toxicities. With the advent of more targeted therapies for CLL, the risk of TLS (tumor lysis syndrome) becomes a crucial consideration, requiring proactive preventive measures. In clinical practice, both hematologists and nephrologists must be well-versed with various differentials leading to suboptimal renal function in patients with CLL. However, uncommon renal infiltration of CLL is worth working up for in cases of inconclusive non-interventional workup as it might indicate disease recurrence/progression prompting the treatment change or resumption. With the advent of advanced cancer therapies it can be reversible if caught early and treated cautiously.
References
- Hallek, M. Chronic lymphocytic leukemia: 2020 update on diagnosis, risk stratification and treatment. Am J Hematol. 2019, 94, 1266–1287. [Google Scholar] [CrossRef]
- Strati, P.; Nasr, S.H.; Leung, N. Renal complications in chronic lymphocytic leukemia and monoclonal B-cell lymphocytosis: the Mayo Clinic experience. haematologica. Ferrata-Storti Foundation 2015, 100, 1180–1188. [Google Scholar] [CrossRef] [PubMed]
- NCCN Guidelines 2024. CLL [Internet]. [Cited. (20242011478). Available online: https://www.nccn.org/professionals/physician_gls/pdf/cll.pdf.
- Strati, P.; Shanafelt, T.D. Monoclonal B-cell lymphocytosis and early-stage chronic lymphocytic leukemia: diagnosis, natural history, and risk stratification. Blood. 2015, 126, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Burger, J.A.; Tedeschi, A.; Barr, P.M.; et al. : Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015, 373, 2425–2437. [Google Scholar] [CrossRef]
- Levey, A.S.; Becker, C.; Inker, L.A. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015, 313, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Wanchoo, R.; Bernabe Ramirez, C.; Barrientos, J.; Jhaveri, K.D. Renal involvement in chronic lymphocytic leukemia. ClinKidney J. 2018, 11, 670–680, 10.1093%2Fckj%2Fsfy026 8. U.S Food and Drug Administration. Full prescribing information for Venetoclax [Internet] . Cited. 202420. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).