Submitted:
07 June 2024
Posted:
07 June 2024
You are already at the latest version
Abstract
Keywords:
Introduction
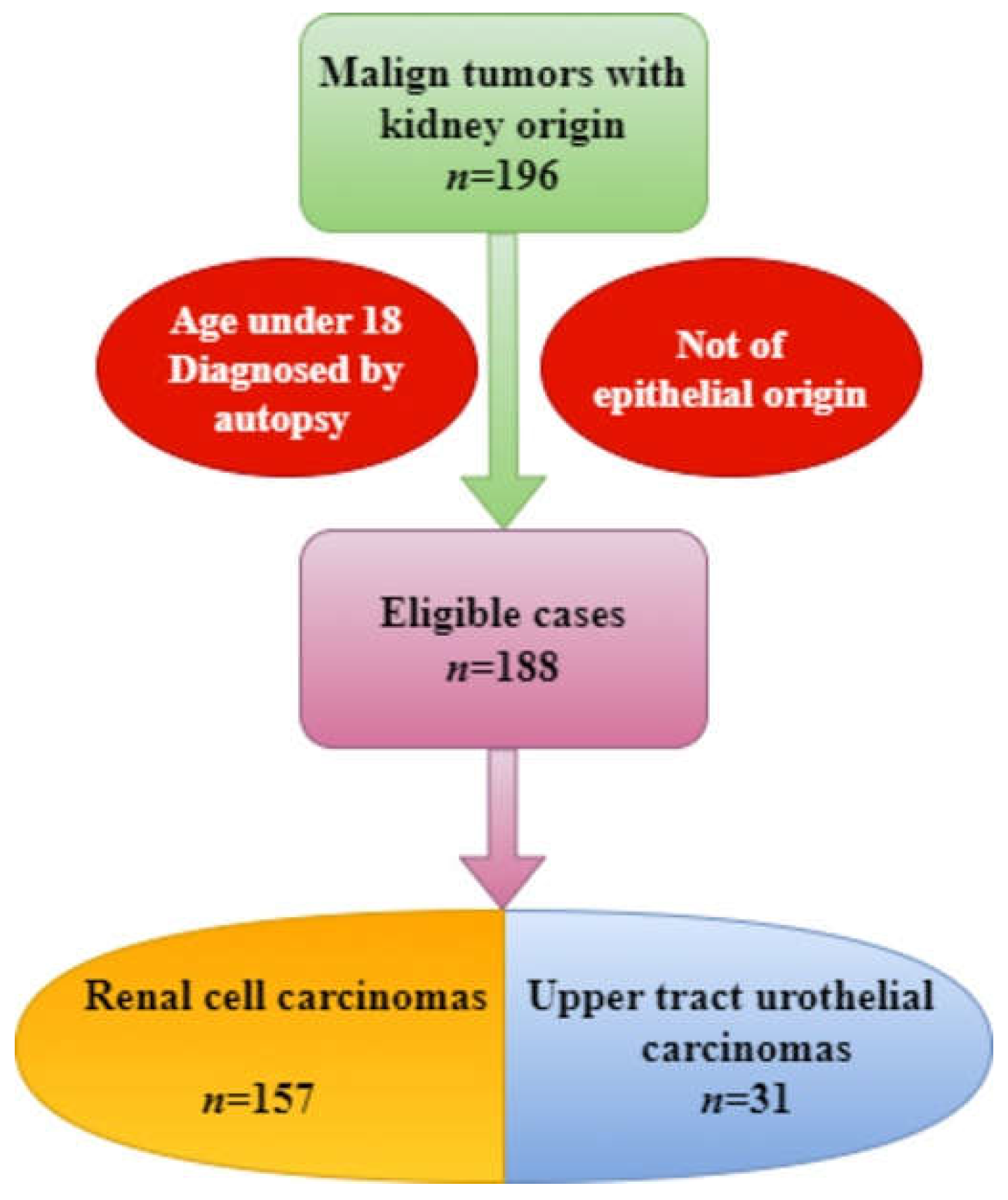
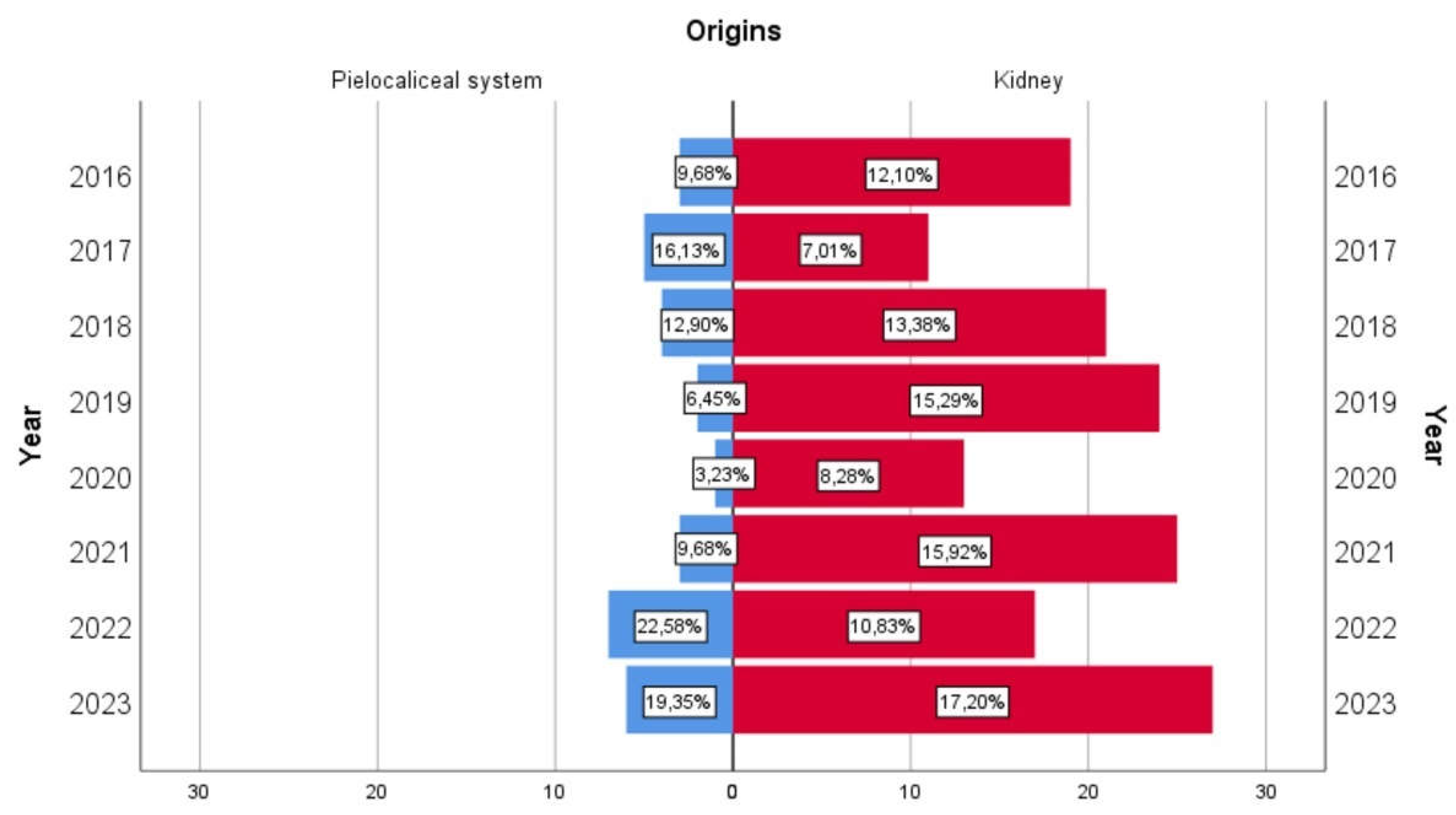
Materials and Methods
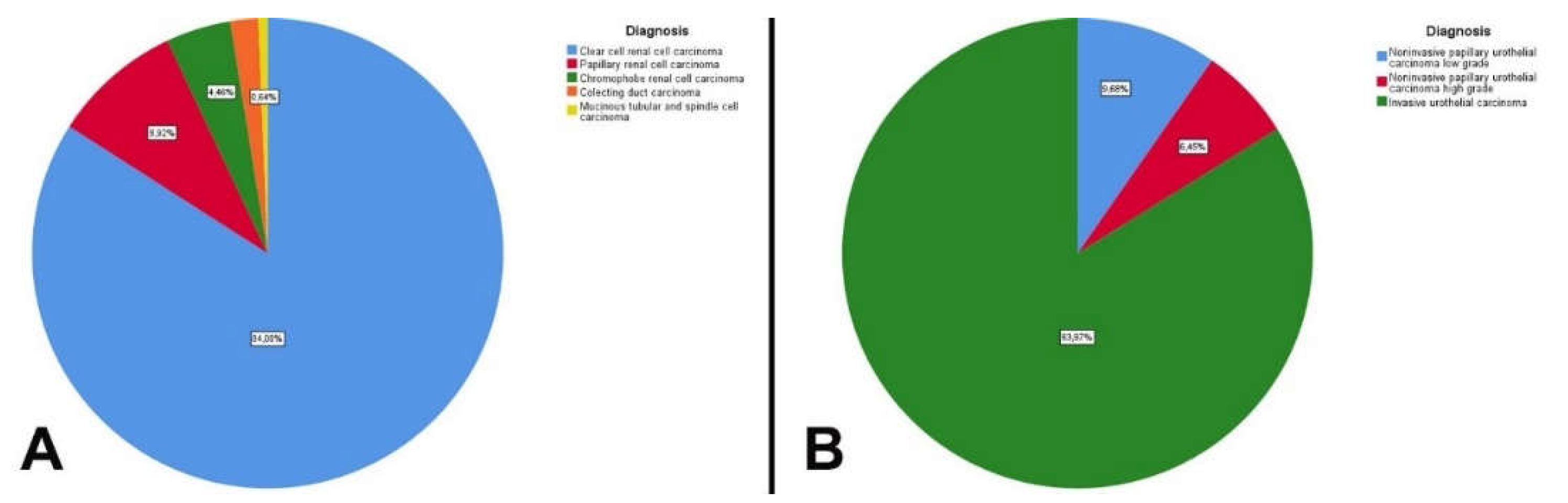
Results
Discussion
Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021 [published correction appears in CA Cancer J Clin. 2021 Jul;71(4):359]. CA Cancer J Clin. 2021;71(1):7-33. [CrossRef]
- Campbell SC, Clark PE, Chang SS, Karam JA, Souter L, Uzzo RG. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-Up: AUA Guideline: Part I. Journal of Urology. 2021;206(2):199-208. [CrossRef]
- Motzer RJ, Jonasch E, Agarwal N; et al. Kidney Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20(1):71-90. [CrossRef]
- Froemming A, Potretzke T, Takahashi N, Kim B. Upper tract urothelial cancer. Eur J Radiol. 2018;98:50-60. [CrossRef]
- Rouprêt M, Babjuk M, Burger M; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur Urol. 2021;79(1):62-79. [CrossRef]
- Padala SA, Barsouk A, Thandra KC; et al. Epidemiology of renal cell carcinoma. World Journal of Oncology. 2020;11(3):79-87. [CrossRef]
- Petros FG. Epidemiology, clinical presentation, and evaluation of upper-tract urothelial carcinoma. Translational Andrology and Urology. 2020;9(4):1794798-1791798. [CrossRef]
- Nuwatkrisin K, Itsaranujareankul T, Panumatrassamee K; et al. Long-term survival of upper tract urothelial carcinoma patients in a tertiary care hospital. Insight Urol 2022;43(1):25-32. [CrossRef]
- Capitanio U, Montorsi F. Renal cancer. The Lancet. 2016;387(10021):894-906. [CrossRef]
- Ljungberg B, Albiges L, Abu-Ghanem Y; et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Eur Urol. 2022;82(4):399-410. [CrossRef]
- Cassell A 3rd, Manobah B, Willie S. Diagnostic and Therapeutic Challenges of Rare Urogenital Cancers: Urothelial Carcinoma of the Renal Pelvis, Ureters and Urethra. World J Oncol. 2021;12(1):20-27. [CrossRef]
- Shao IH, Chang YH, Pang ST. Recent advances in upper tract urothelial carcinomas: From bench to clinics. Int J Urol. 2019;26(2):148-159. [CrossRef]
- Capitanio U, Bensalah K, Axel B; et al. Epidemiology of Renal Cell Carcinoma. European Urology. 2019; 74-84. [CrossRef]
- Bukavina L, Bensalah K, Bray F; et al. Epidemiology of Renal Cell Carcinoma: 2022 Update. Eur Urol. 2022;82(5):529-542. [CrossRef]
- Ali RM, Muhealdeen DN, Fakhralddin SS; et al. Prognostic factors in renal cell carcinoma: A single-center study. Mol Clin Oncol. 2023;19(3):66. [CrossRef]
- Volpe A, Patard JJ. Prognostic factors in renal cell carcinoma. World J Urol. 2010;28(3):319-327. [CrossRef]
- Collà Ruvolo C, Nocera L, Stolzenbach LF; et al. Incidence and Survival Rates of Contemporary Patients with Invasive Upper Tract Urothelial Carcinoma. Eur Urol Oncol. 2021;4(5):792-801. [CrossRef]
- Rouprêt M, Seisen T, Birtle AJ; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2023 Update. Eur Urol. 2023;84(1):49-64. [CrossRef]
- Medina-Rico M, Ramos HL, Lobo M, Romo J, Prada JG. Epidemiology of renal cancer in developing countries: Review of the literature. Can Urol Assoc J. 2018;12(3):E154-E162. [CrossRef]
- Rossi SH, Klatte T, Smith JU, Steward GD. Epidemiology and screening for renal cancer. WJU. 2018; 36:1341–1353. [CrossRef]
- Soualhi A, Rammant E, George G; et al. The incidence and prevalence of upper tract urothelial carcinoma: A systematic review. BMC Urology. 2021;21(1). [CrossRef]
- Perazella MA, Dreicer R, Rosner MH. Renal cell carcinoma for the nephrologist. Kidney International. 2018;94(3):471-483. [CrossRef]
- Barber N, Ali A. Urologic Cancers. Exon Publications. Brisbane, 2022, p. 63-67.
- Nabi S, Kessler ER, Bernard B, Flaig TW, Lam ET. Renal cell carcinoma: A review of biology and pathophysiology. F1000Res. 2018;7:307. [CrossRef]
- Miricescu D, Balan DG, Tulin A; et al. PI3K/AKT/mTOR signalling pathway involvement in renal cell carcinoma pathogenesis (Review). Exp Ther Med. 2021;21(5):540. [CrossRef]
- Kumar A, Kumari N, Gupta V, Prasad R. Renal Cell Carcinoma: Molecular Aspects. Indian J Clin Biochem. 2018;33(3):246-254. [CrossRef]
- Peired AJ, Antonelli G, Angelotti ML; et al. Acute kidney injury promotes development of papillary renal cell adenoma and carcinoma from renal progenitor cells. Sci Transl Med. 2020;12(536):eaaw6003. [CrossRef]
- Kang YC, Chen MH, Lin CY, Lin CY, Chen YT. Aristolochic acid-associated urinary tract cancers: An updated meta-analysis of risk and oncologic outcomes after surgery and systematic review of molecular alterations observed in human studies. Ther Adv Drug Saf. 2021;12:2042098621997727. [CrossRef]
- Singla, N.; Margulis, V. Differences between Upper Tract Urothelial Carcinoma and Bladder Cancer. AUA News. 2021;26(7):15-16.
- Aragon-Ching JB, Nizam A, Henson DE. Carcinomas of the Renal Pelvis, Ureters, and Urinary Bladder Share a Carcinogenic Field as Revealed in Epidemiological Analysis of Tumor Registry Data. Clinical Genitourinary Cancer. 2019;17(6):436-442. [CrossRef]
- Almås B, Halvorsen OJ, Johannesen TB, Beisland C. Higher than expected and significantly increasing incidence of upper tract urothelial carcinoma. A population based study. World J Urol. 2021;39(9):3385-3391. [CrossRef]
- Soualhi A, Rammant E, George G; et al. The incidence and prevalence of upper tract urothelial carcinoma: A systematic review. BMC Urol. 2021;21(1):Published 2021 Aug 17. [CrossRef]
- Okbah AA, Al-Shamahy HA, Al-Shamahi EH; et al. Renal lesions: Differentiation of malignant and benign tumors, sex and age distribution and variables associated with renal cell carcinoma in Sana’a City, Yemen. Universal Journal of Pharmaceutical Research. 2022;7(2):34-39. [CrossRef]
- Zaitsu M, Toyokawa S, Takeuchi T, Kobayashi Y, Kawachi I. Sex-specific analysis of renal cell carcinoma histology and survival in Japan: A population-based study 2004 to Health Sci Rep. 2019;3(1):ePublished 2019 Dec 20. [CrossRef]
- Huang CC, Su YL, Luo HL; et al. Gender Is a Significant Prognostic Factor for Upper Tract Urothelial Carcinoma: A Large Hospital-Based Cancer Registry Study in an Endemic Area. Front Oncol. 2019;9:Published 2019 Mar 21. [CrossRef]
- Deuker M, Rosiello G, Stolzenbach LF; et al. Sex- and Age-Related Differences in the Distribution of Metastases in Patients With Upper Urinary Tract Urothelial Carcinoma. J Natl Compr Canc Netw. 2021;19(5):534-Published 2021 Feb 11. [CrossRef]
- Escudier B, Porta C, Schmidinger M; et al. Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30(5):706-720. [CrossRef]
- Ko JJ, Xie W, Kroeger N; et al. The International Metastatic Renal Cell Carcinoma Database Consortium model as a prognostic tool in patients with metastatic renal cell carcinoma previously treated with first-line targeted therapy: A population-based study. Lancet Oncol. 2015;16(3):293-300. [CrossRef]
- Petros FG. Epidemiology, clinical presentation, and evaluation of upper-tract urothelial carcinoma. Transl Androl Urol. 2020;9(4):1794-1798. [CrossRef]
- Chou YH, Huang CH. Unusual clinical presentation of upper urothelial carcinoma in Taiwan. Cancer. 1999;85(6):1342-1344. [CrossRef]
- Ba Z, Xiao Y, He M; et al. Risk Factors for the Comorbidity of Hypertension and Renal Cell Carcinoma in the Cardio-Oncologic Era and Treatment for Tumor-Induced Hypertension. Front Cardiovasc Med. 2022;9:810262. [CrossRef]
- Seretis A, Cividini S, Markozannes G; et al. Association between blood pressure and risk of cancer development: A systematic review and meta-analysis of observational studies. Sci Rep. 2019;9(1):8565. [CrossRef]
- Kim CS, Han KD, Choi HS, Bae EH, Ma SK, Kim SW. Association of Hypertension and Blood Pressure With Kidney Cancer Risk: A Nationwide Population-Based Cohort Study. Hypertension. 2020;75(6):1439-1446. [CrossRef]
- Xie Y, Xu P, Wang M; et al. Antihypertensive medications are associated with the risk of kidney and bladder cancer: A systematic review and meta-analysis. Aging (Albany NY). 2020;12(2):1545-1562. [CrossRef]
- Lindsey N. Hypertension Linked to Worse Upper Tract Urothelial Cancer Outcomes. Oncology Times. 2023: 45(12): 14-15. [CrossRef]
- Lee M, Song SH, Kim H; et al. Effect of Body Mass Index and Hypertension on the Prognosis of Upper Tract Urothelial Carcinoma After Radical Nephroureterectomy. Korean J Urol Oncol. 2020;18(3):201-208. [CrossRef]
- Abudawood M. Diabetes and cancer: A comprehensive review. J Res Med Sci. 2019;24:94. [CrossRef]
- Ling X, Yi X, Xu Z; et al. Association of diabetes risk reduction diet with renal cancer risk in 101,755 participants: A prospective study. Journal of Translational Medicine. 2023;21(1). [CrossRef]
- Gao X, Zhou L, Ai J; et al. The Impact of Diabetes on the Prognosis of Upper Tract Urothelial Carcinoma After Radical Nephroureterectomy: A Systematic Review and Meta-Analysis. Front Oncol. 2021;11:Published 2021 Oct 18. [CrossRef]
- Liu X, Sun Q, Hou H; et al. The association between BMI and kidney cancer risk: An updated dose-response meta-analysis in accordance with PRISMA guideline. Medicine. 2018;97(44):e12860. [CrossRef]
- van de Pol JAA, George L, van den Brandt PA, Baldewijns MMLL, Schouten LJ. Etiologic heterogeneity of clear-cell and papillary renal cell carcinoma in the Netherlands Cohort Study. Int J Cancer. 2021;148(1):67-76. [CrossRef]
- Pan Y, Chen Z, Yang L; et al. Body Composition Parameters May Be Prognostic Factors in Upper Urinary Tract Urothelial Carcinoma Treated by Radical Nephroureterectomy [published correction appears in Front Oncol. 2021 Jul 23;11:740572]. Front Oncol. 2021;11:Published 2021 May 24. [CrossRef]
- Xu H, Tan P, Zheng X; et al. Metabolic syndrome and upper tract urothelial carcinoma: A retrospective analysis from a large Chinese cohort. Urol Oncol. 2019;37(4):291.e19-291.e28. [CrossRef]
- Kellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders HJ. Acute kidney injury. Nature Reviews Disease Primers. 2021;7(1). [CrossRef]
- Saly DL, Eswarappa MS, Street SE, Deshpande P. Renal Cell Cancer and Chronic Kidney Disease. Advances in Chronic Kidney Disease. 2021;28(5):460-468.e1. [CrossRef]
- Peired AJ, Lazzeri E, Guzzi F, Anders HJ, Romagnani P. From kidney injury to kidney cancer. Kidney Int. 2021;100(1):55-66. [CrossRef]
- Peired AJ, Antonelli G, Angelotti ML; et al. Acute kidney injury promotes development of papillary renal cell adenoma and carcinoma from renal progenitor cells. Sci Transl Med. 2020;12(536):eaaw6003. [CrossRef]
- Mori K, Janisch F, Mostafaei H; et al. Prognostic value of preoperative blood-based biomarkers in upper tract urothelial carcinoma treated with nephroureterectomy: A systematic review and meta-analysis. Urol Oncol. 2020;38(5):315-333. [CrossRef]
- Liu J, Lai S, Wu P; et al. Systematic oxidative stress indices predicts prognosis in patients with urothelial carcinoma of the upper urinary tract after radical nephroureterectomy. Eur J Med Res. 2023;28(1):Published 2023 Oct 28. [CrossRef]
- Kuroda K, Asakuma J, Horiguchi A; et al. Chronic kidney disease and positive surgical margins as prognosticators for upper urinary tract urothelial carcinoma patients undergoing radical nephroureterectomy. Mol Clin Oncol. 2019;10(5):547-554. [CrossRef]
- Xia L, Hu G, Guzzo TJ. Prognostic Significance of Preoperative Anemia in Patients Undergoing Surgery for Renal Cell Carcinoma: A Meta-analysis. Anticancer Res. 2017;37(6):3175-3181. [CrossRef]
- Fan Y, Li H, Ma X; et al. Prognostic Significance of Hypoxia-Inducible Factor Expression in Renal Cell Carcinoma: A PRISMA-compliant Systematic Review and Meta-Analysis. Medicine (Baltimore). 2015;94(38):e1646. [CrossRef]
- Warli SM, Andy A, Prapiska FF, Siregar GP, Sihombing B. Poor prognosis of urothelial carcinoma in patients presented with persistent paraneoplastic leukocytosis with anemia. Urol Ann. 2022;14(4):328-331. [CrossRef]
- Guan B, Weng M, Fan H; et al. Beijing Da Xue Xue Bao Yi Xue Ban. 2019;51(6):1056-1061. [CrossRef]
- Luo F, Wang YS, Su YH, Zhang ZH, Sun HH, Li J. Prognostic implications of preoperative anemia in urothelial carcinoma: A meta-analysis. PLoS ONE. 2017;12(2):ePublished 2017 Feb 9. [CrossRef]
- Chang Y, An H, Xu L; et al. Systemic inflammation score predicts postoperative prognosis of patients with clear-cell renal cell carcinoma. Br J Cancer. 2015;113(4):626-633. [CrossRef]
- Chen Z, Wang K, Lu H; et al. Systemic inflammation response index predicts prognosis in patients with clear cell renal cell carcinoma: A propensity score-matched analysis. Cancer Manag Res. 2019;11:909-Published 2019 Jan 18. [CrossRef]
- De Giorgi U, Procopio G, Giannarelli D; et al. Association of Systemic Inflammation Index and Body Mass Index with Survival in Patients with Renal Cell Cancer Treated with Nivolumab. Clin Cancer Res. 2019;25(13):3839-3846. [CrossRef]
- Jan HC, Yang WH, Ou CH. Combination of the Preoperative Systemic Immune-Inflammation Index and Monocyte-Lymphocyte Ratio as a Novel Prognostic Factor in Patients with Upper-Tract Urothelial Carcinoma. Ann Surg Oncol. 2019;26(2):669-684. [CrossRef]
- Mori K, Resch I, Miura N; et al. Prognostic role of the systemic immune-inflammation index in upper tract urothelial carcinoma treated with radical nephroureterectomy: Results from a large multicenter international collaboration. Cancer Immunol Immunother. 2021;70(9):2641-2650. [CrossRef]
- Jiang T, Wu YP, Chen SH, Ke ZB, Liang YC, Xu N. Prognosis and clinicopathological characteristics of renal cell carcinoma: Does bilateral occurrence influence overall and cancer-specific survival?. Transl Cancer Res. 2020;9(2):432-440. [CrossRef]
- Guo S, Yao K, He X; et al. Prognostic significance of laterality in renal cell carcinoma: A population-based study from the surveillance, epidemiology, and end results (SEER) database. Cancer Med. 2019;8(12):5629-5637. [CrossRef]
- Inamoto T, Matsuyama H, Komura K; et al. Tumor Location Based Segmentation in Upper-Tract Urothelial Carcinoma Impacts on the Urothelial Recurrence-Free Survival: A Multi-Institutional Database Study. Curr Urol. 2020;14(4):183-190. [CrossRef]
- Delahunt B, Eble JN, Samaratunga H, Thunders M, Yaxley JW, Egevad L. Staging of renal cell carcinoma: Current progress and potential advances. Pathology. 2021;53(1):120-128. [CrossRef]
- Cornejo KM, Rice-Stitt T, Wu CL. Updates in Staging and Reporting of Genitourinary Malignancies. Arch Pathol Lab Med. 2020;144(3):305-319. [CrossRef]
- Mohd AB, Ghannam RA, Mohd OB; et al. Etiologies, Gross Appearance, Histopathological Patterns, Prognosis, and Best Treatments for Subtypes of Renal Carcinoma: An Educational Review. Cureus. 2022;14(12):e32338. [CrossRef]
- Hsieh JJ, Purdue MP, Signoretti S; et al. Renal cell carcinoma. Nat Rev Dis Primers. 2017;3:17009. [CrossRef]
- Muglia VF, Prando A. Renal cell carcinoma: Histological classification and correlation with imaging findings. Radiologia Brasileira. 2015;48(3):166-174. [CrossRef]
- Eshghi M. Urothelial Malignancies of the Upper Urinary Tract. A Textbook of Step by Step Management. Springer. Phillapedhia. 2018, p. 107-112. [CrossRef]
- WHO Classification of Tumours Editorial Board. Urinary and male genital tumours. WHO classification of tumours series, 5th ed.; vol. Lyon, International Agency for Research on Cancer; 2022.
- Mori K, Janisch F, Parizi MK; et al. Prognostic Value of Variant Histology in Upper Tract Urothelial Carcinoma Treated with Nephroureterectomy: A Systematic Review and Meta-Analysis. J Urol. 2020;203(6):1075-1084. [CrossRef]
- Monda SM, Lui HT, Pratsinis MA, Chandrasekar T, Evans CP, Dall'Era MA. The Metastatic Risk of Renal Cell Carcinoma by Primary Tumor Size and Subtype. Eur Urol Open Sci. 2023;52:137-144. [CrossRef]
- Zganjar AJ, Thiel DD, Lyon TD. Diagnosis, workup, and risk stratification of upper tract urothelial carcinoma. Transl Androl Urol. 2023;12(9):1456-1468. [CrossRef]
- Foerster B, Abufaraj M, Mari A; et al. The Performance of Tumor Size as Risk Stratification Parameter in Upper Tract Urothelial Carcinoma (UTUC). Clin Genitourin Cancer. 2021;19(3):272.e1-272.e7. [CrossRef]
- Syed M, Loya A, Hameed M, Akhtar N, Mushtaq S, Hassan U. Prognostic Significance of Percentage Necrosis in Clear Cell Renal Cell Carcinoma. American Journal of Clinical Pathology. 2021;157(3):374-380. [CrossRef]
- Avulova S, Cheville JC, Lohse CM; et al. Grading Chromophobe Renal Cell Carcinoma: Evidence for a Four-tiered Classification Incorporating Coagulative Tumor Necrosis. Eur Urol. 2021;79(2):225-231. [CrossRef]
- Kuroe T, Watanabe R, Morisue R; et al. Dirty necrosis in renal cell carcinoma is associated with NETosis and systemic inflammation. Cancer Med. 2023;12(4):4557-4567. [CrossRef]
- Bitaraf M, Ghafoori Yazdi M, Amini E. Upper Tract Urothelial Carcinoma (UTUC) Diagnosis and Risk Stratification: A Comprehensive Review. Cancers (Basel). 2023;15(20):Published 2023 Oct 14. [CrossRef]
- Parmar K, Thummala Y, Kumar S, Kaundal P, Mandal S. Massive intratumoral bleed in renal cell cancer: An unusual life-threatening event. Ann R Coll Surg Engl. 2022;104(6):e168-e170. [CrossRef]
- Panaiyadiyan S, Singh P, Gurnani N, Nayak B. Upper Tract Urothelial Carcinoma with Intra-renal Haemorrhage. Indian J Surg Oncol. 2021;12(Suppl 2):367-370. [CrossRef]
- Xu W, Jiang X, Guan C, Gu M. The prognostic and predictive value of tumor infiltrating Macrophage and Neutrophil in patient with clear cell renal cell carcinoma: Tumor infiltrating lymphocytes in renal cell carcinoma. Medicine (Baltimore). 2020;99(46):e23181. [CrossRef]
- Zhang S, Zhang E, Long J; et al. Immune infiltration in renal cell carcinoma. Cancer Sci. 2019;110(5):1564-1572. [CrossRef]
- Cheng S, Zhong W, Xia K; et al. Prognostic role of stromal tumor-infiltrating lymphocytes in locally advanced upper tract urothelial carcinoma: A retrospective multicenter study (TSU-02 study). Oncoimmunology. 2021;10(1):Published 2021 Jan 4. [CrossRef]
- Taneja K, Williamson SR. Updates in Pathologic Staging and Histologic Grading of Renal Cell Carcinoma. Surg Pathol Clin. 2018;11(4):797-812. [CrossRef]
- Ali RM, Muhealdeen DN, Fakhralddin SS; et al. Prognostic factors in renal cell carcinoma: A single-center study. Mol Clin Oncol. 2023;19(3):Published 2023 Jul 14. [CrossRef]
- Dagher J, Delahunt B, Rioux-Leclercq N; et al. Clear cell renal cell carcinoma: Validation of World Health Organization/International Society of Urological Pathology grading. Histopathology. 2017;71(6):918-925. [CrossRef]
- Kryvenko ON. Tumor necrosis adds prognostically significant information to grade in clear cell renal cell carcinoma: A study of 842 consecutive cases from a single institution. Khor LY, Dhakal HP, Jia X, Reynolds JP, McKenney JK, Rini BI, Magi-Galluzzi C, Przybycin CG.Am J Surg Pathol. September 2016;40(9):1224-Urol Oncol. 2017;35(6):454-455. [CrossRef]
- Fojecki G, Magnusson A, Traxer O; et al. Consultation on UTUC, Stockholm 2018 aspects of diagnosis of upper tract urothelial carcinoma. World J Urol. 2019;37(11):2271-2278. [CrossRef]
- Kanwal R. Metastasis in renal cell carcinoma: Biology and treatment. Advances in Cancer Biology - Metastasis. 2023;7:100094. [CrossRef]
- Lemelin A, Takemura K, Yick D, Matthew Scott Ernst. Prognostic Models in Metastatic Renal Cell Carcinoma. Hematology/Oncology Clinics of North America. 2023;37(5):925-935. [CrossRef]
- Ku YH, Chen CM, Yu WL. Upper Tract Urothelial Carcinoma: Clinical Features and Management. SM J Urol. 2020; 6:11. [CrossRef]
- Lwin AA, Hsu CH, Chipollini J. Urothelial Carcinoma of the Renal Pelvis and Ureter: Does Location Make a Difference?. Clin Genitourin Cancer. 2020;18(1):45-49.e1. [CrossRef]
- Capek S, Krauss WE, Amrami KK, Parisi JE, Spinner RJ. Perineural Spread of Renal Cell Carcinoma: A Case Illustration with a Proposed Anatomic Mechanism and a Review of the Literature. World Neurosurgery. 2016;89:728.e11-728.e17. [CrossRef]
- Lin TW, Lee HY, Yang SF; et al. Perineural Invasion is a Powerful Prognostic Factor for Upper Tract Urothelial Carcinoma Following Radical Nephroureterectomy. Ann Surg Oncol. 2022;29(5):3306-3317. [CrossRef]
- Niu S, Liang P, Lin MY; et al. Predominant global glomerulosclerosis in patients of upper urinary tract urothelial carcinoma with pre-existing renal function impairment is a predictor of poor renal outcomes. BMC Cancer. 2019;19(1). [CrossRef]
- Roupret M, Gontero P, Birtle A; et al. EAU Guidelines on Upper Tract Urothelial Carcinoma. European Association of Urology. Milan, 2023, p. 13-14.
- Kohada Y, Hayashi T, Goto K; et al. Preoperative risk classification using neutrophil-lymphocyte ratio and hydronephrosis for upper tract urothelial carcinoma. Jpn J Clin Oncol. 2018;48(9):841-850. [CrossRef]
- Hsieh JJ, Purdue MP, Signoretti S; et al. Renal cell carcinoma. Nat Rev Dis Primers. 2017;3:17009. [CrossRef]
- Chandrasekar T, Boorjian SA, Capitanio U, Gershman B, Mir MC, Kutikov A. Collaborative Review: Factors Influencing Treatment Decisions for Patients with a Localized Solid Renal Mass. Eur Urol. 2021;80(5):575-588. [CrossRef]
- Bahadoram S, Davoodi M, Hassanzadeh S, Bahadoram M, Barahman M, Mafakher L. Renal cell carcinoma: An overview of the epidemiology, diagnosis, and treatment. G Ital Nefrol. 2022;39(3):2022-volPublished 2022 Jun 20.
- Kim SP, Campbell SC, Gill IS; et al. Collaborative Review of Risk Benefit Trade-offs Between Partial and Radical Nephrectomy in the Management of Anatomically Complex Renal Masses. 2017;72(1):64-75. [CrossRef]
- Rouprêt M, Babjuk M, Burger M; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur Urol. 2021;79(1):62-79. [CrossRef]
- Verges DP, Lallas CD, Hubosky SG, Bagley DH Jr. Endoscopic Treatment of Upper Tract Urothelial Carcinoma. Curr Urol Rep. 2017;18(4):31. [CrossRef]
- Leow JJ, Liu Z, Tan TW, Lee YM, Yeo EK, Chong YL. Optimal Management of Upper Tract Urothelial Carcinoma: Current Perspectives. Onco Targets Ther. 2020;13:1-Published 2020 Jan 6. [CrossRef]
- Azizi M, Cheriyan SK, Peyton CC, Foerster B, Shariat SF, Spiess PE. Optimal Management of Upper Tract Urothelial Carcinoma: An Unmet Need. Curr Treat Options Oncol. 2019;20(5):Published 2019 Apr 1. [CrossRef]
- Unadkat P, Olumi AF, Gershman B. The Role of Lymphadenectomy in Patients with Advanced Renal Cell Carcinoma. Urologic Clinics of North America. 2020;47(3):371-377. [CrossRef]
- Chan VW, Wong CHM, Yuan Y, Teoh JY. Lymph node dissection for upper tract urothelial carcinoma: A systematic review. Arab J Urol. 2020;19(1):37-Published 2020 Jul 27. [CrossRef]
- Karmali RJ, Suami H, Wood CG, Karam JA. Lymphatic drainage in renal cell carcinoma: Back to the basics. BJU Int. 2014;114(6):806-817. [CrossRef]
- Carlson P, McGary CT. Educational Case: Renal Cell and Urothelial Carcinoma. Acad Pathol. 2020;7:2374289520956363. [CrossRef]
- Singla N, Hutchinson R, Menegaz C; et al. Comparing Changes in Renal Function After Radical Surgery for Upper Tract Urothelial Carcinoma and Renal Cell Carcinoma. Urology. 2016;96:44-53. [CrossRef]
| Renal cell carcinomas | Upper tract urothelial carcinomas | p-Value | |
|---|---|---|---|
| Age (years) Median (Percentiles 25-75) Min-max |
64 (56-70) 28-81 |
73 (63-81) 45-87 |
<0.001 |
| Decade (n, %) | 7, 38.85% | 9, 32.26% | <0.001 |
| Gender Female Male |
42.68% 57.32% |
38.71% 61.29% |
0.842 |
| Environment Rural Urban |
47.13% 52.87% |
32.26% 67.74% |
0.167 |
| Deaths | 24.85% | 45.16% | 0.029 |
| Renal cell carcinomas | Upper tract urothelial carcinomas | p-Value | |
| Hematuria Absence Microscopic Macroscopic |
22.29% 36.94% 40.77% |
3.23% 25.81% 70.97% |
0.004 |
| Flank pain | 71.34% | 48.39% | 0.020 |
| Oligoanuria | 11.46% | 25.81% | 0.046 |
| Dysuria | 47.77% | 32.26% | 0.120 |
| High blood pressure | 59.23% | 70.97% | 0.313 |
| Diabetes mellitus | 24.84% | 25.81% | 0.910 |
| Obesity | 17.83% | 25.81% | 0.321 |
| Acute kidney injury | 27.39% | 64.52% | <0.001 |
| Serum creatinine (mg/dL) Median (Percentiles 25-75) Min-Max |
0.88 (0.73-1.26) 0.29-12.62 |
1.34 (1.02-1.72) 0.69-26.16 |
<0.001 |
| Anemia Mild Moderate Severe |
26.75% 52.38% 33.33% 14.29% |
70.97% 40.91% 40.91% 18.18% |
<0.001 0.721 |
| Systemic inflammatory syndrome | 57.96% | 64.52% | 0.553 |
| Renal cell carcinomas | Upper tract urothelial carcinomas | p-Value | |
| Weight (g) Median (Percentiles 25-75) Min-Max |
339 (250-468) 120-1665 |
310 (230-350) 145-547 |
0.065 |
| Length (cm) Median (Percentiles 25-75) Min-Max |
12 (11-14) 7.5-21 |
12 (11-13.50) 8.5-18 |
0.069 |
| Kidney Left Right |
51.59% 48.41% |
54.84% 45.16% |
0.845 |
| Localization Superior Middle third/pelvis Inferior All |
40.13% 28.66% 28.03% 3.18% |
25.81% 45.16% 19.35% 9.68% |
0.065 |
| Renal cell carcinomas | Upper tract urothelial carcinomas | p-Value | |
|---|---|---|---|
| Pseudoencapsulation Cystic spaces |
91.08% 52.87% |
0% 6.45% |
<0.001 <0.001 |
| Infiltrative appearance Exceeding the renal capsule Invasion of the pielocaliceal system |
24.20% 17.19% 14.65% |
87.10% 6.45% - |
<0.001 0.176 - |
| Maximum tumor diameter (cm) Median (Percentiles 25-75) Min-Max |
5.5 (3.95-7.5) 0.9-19 |
4.5 (3.5-5.8) 0.7-8 |
0.025 |
| Renal cell carcinomas | Upper tract urothelial carcinomas | p-Value | |
| Tumor necrosis | 56.69% | 61.29% | 0.694 |
| Hemorrhagic infiltrate | 72.61% | 38.71% | 0.001 |
| Intratumoral inflammatory infiltrate Acute Mixed Chronic |
2.55% 8.92% 88.53% |
0% 16.13% 83.87% |
0.410 |
| Angiolymphatic invasion | 22.92% | 48.39% | 0.007 |
| Perineural invasion | 7.64% | 29.03% | 0.002 |
| Histological grade Low grade (1 and 2) High grade (3 and 4) |
ISUP 2 – 41.40 % 55.41% 44.59% |
38.71% 61.29% |
- 0.115 |
| pT | 3a – 31.21% | 3 – 64.52% | - |
| Metastasis (n) | 2 – lung | 2 - bone | - |
| Complete resection | 98.73% | 87.10% | 0.007 |
| Adjacent renal parenchyma Chronic pyelonephritis Normal Interstitial nephritis Hydronephrosis |
35.67% 31.85% 25.48% 1.27% |
70.97% 3.23% 19.35% 6.45% |
0.001 |
| Univariate analysis | Multivariate analysis | |||||
| Parameter | Hazard risk | p-Value | CI95% | Hazard risk | p-Value | CI95% |
| Age | 1.073 | 0.002 | 1.027-1.121 | 1.084 | 0.002 | 1.031-1.139 |
| Exceeding the renal capsule | 2.504 | 0.040 | 1.045-6.003 | 1.255 | 0.693 | 0.407-3.871 |
| The lesion throughout the kidney | 10.000 | 0.046 | 1.045-95.683 | 5.110 | 0.238 | 0.341-76.590 |
| ILV | 2.444 | 0.029 | 1.096-5.448 | 1.635 | 0.344 | 0.591-4.519 |
| High grade | 2.172 | 0.039 | 1.039-4.537 | 2.242 | 0.076 | 0.919-5.469 |
| Acute kidney injury | 2.734 | 0.010 | 1.268-5.895 | 2.023 | 0.126 | 0.820-4.990 |
| Anemia | 2.875 | 0.007 | 1.329-6.219 | 2.838 | 0.028 | 1.122-7.179 |
| Univariate analysis | Multivariate analysis | |||||
| Parameter | Hazard risk | p-Value | CI95% | Hazard risk | p-Value | CI95% |
| Perineural invasion | 7.500 | 0.029 | 1.228-45.807 | 10.513 | 0.066 | 0.859-128.708 |
| Acute kidney injury | 6.750 | 0.035 | 1.145-39.796 | 1.701 | 0.682 | 0.134-21.600 |
| Anemia | 11.556 | 0.033 | 1.223-109.185 | 9.812 | 0.129 | 0.513-187.778 |
| Hematuria | 10.448 | 0.038 | 1.138-95.926 | 18.271 | 0.067 | 0.814-410.233 |
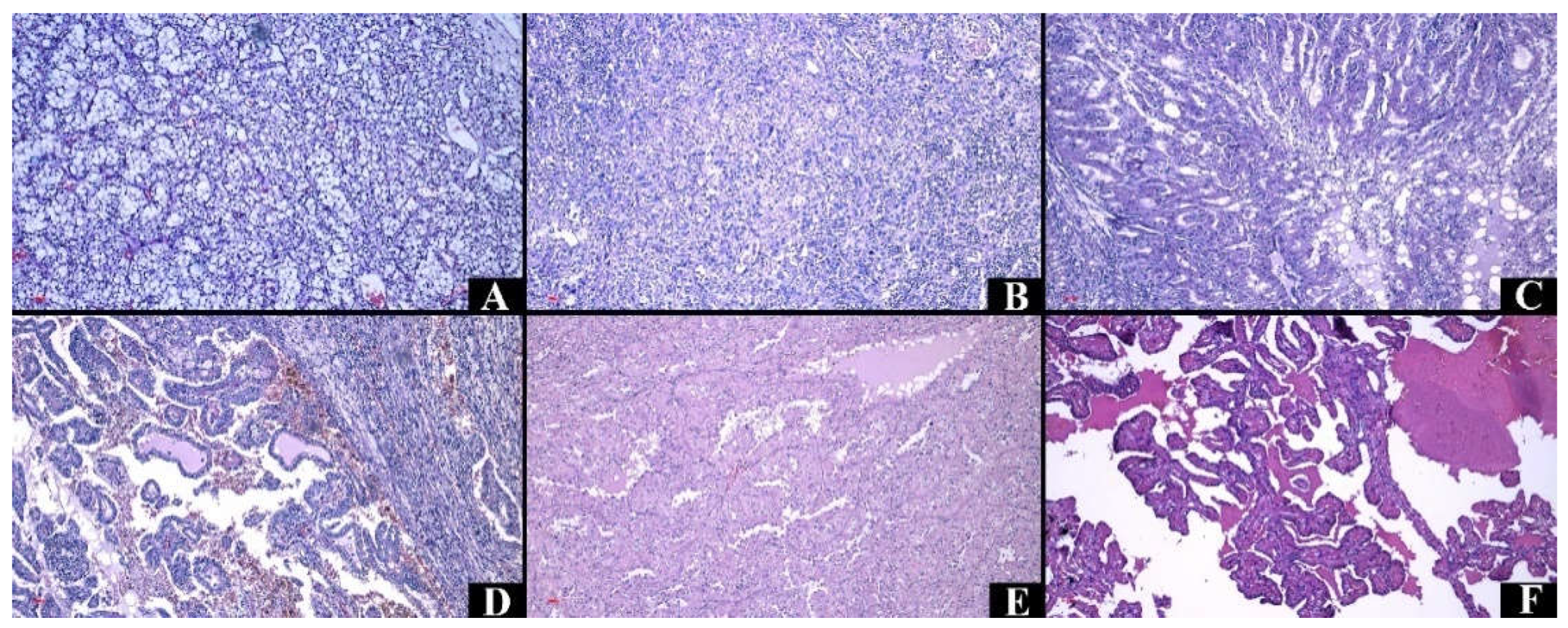
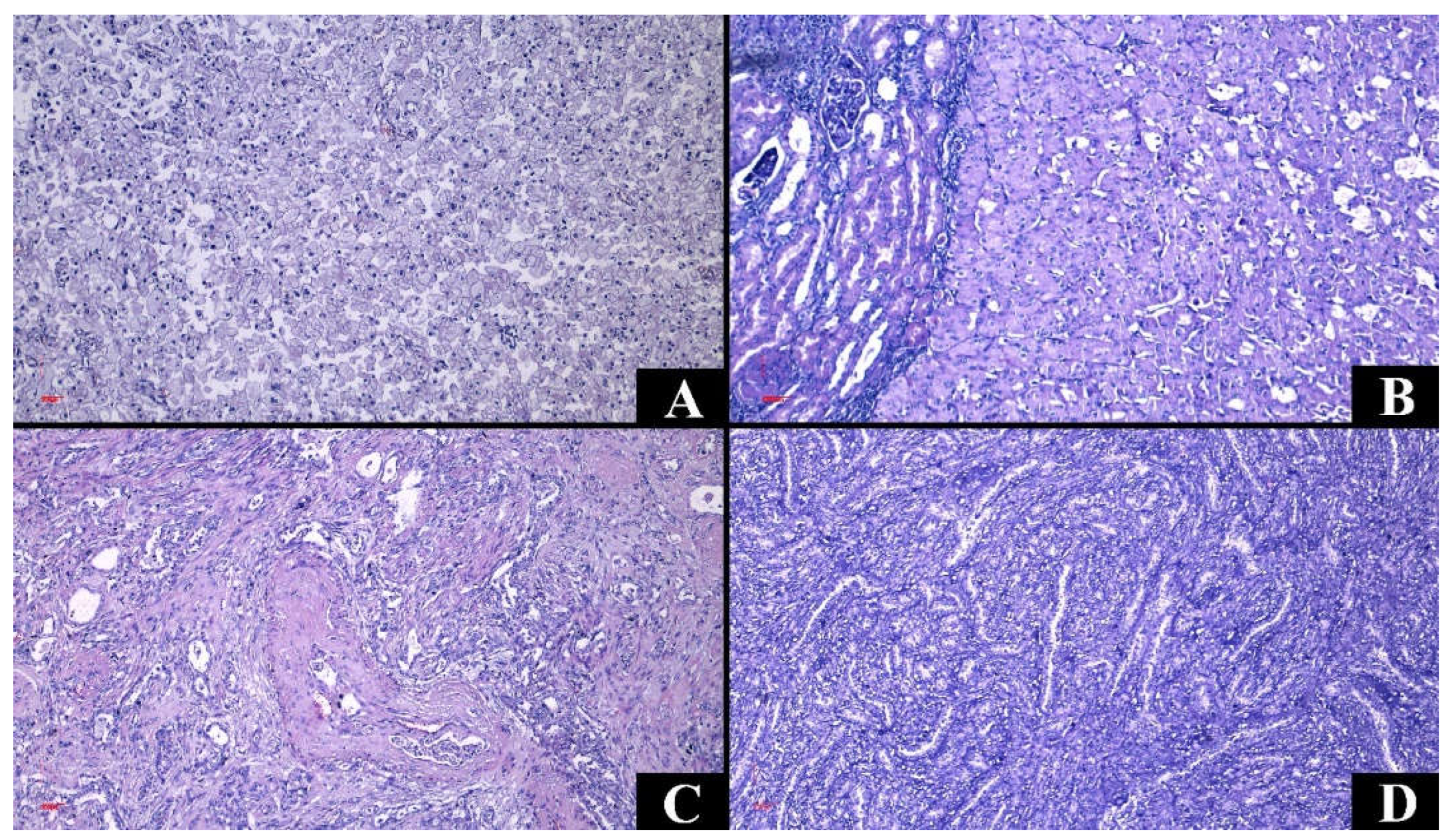
| Tumor type | Variants | Gross aspect | Origin | Histologic features |
| Clear cell renal cell carcinoma |
|
Pseudo-encapsulated, Golden yellow, Necrosis, Hemorrhage |
Tubular epithelium, Proximal nephron |
Nests and sheets of cells with clear cytoplasm. |
| Papillary renal cell carcinoma |
|
Often pseudo encapsulated Solid or cystic Whitish Necrosis, Hemorrhage |
Tubular epithelium, Distal nephron |
Thin or thick papillae lined by uni- or pseudostratified cuboidal epithelium, foamy macrophages, and psammomatous bodies. |
| Chromophobe renal cell carcinoma |
|
Well defined Gray to tan-brown, Central scar |
Intercalated cells of the distal tubules, Distal nephron |
Cells with prominent membrane and pale/eosinophilic cytoplasm. |
| Carcinoma of collecting ducts | Partially cystic Grayish-white |
Collector tubes | Tubulopapillary architecture, hobnail cells, mucinous material, desmoplastic stroma. |
|
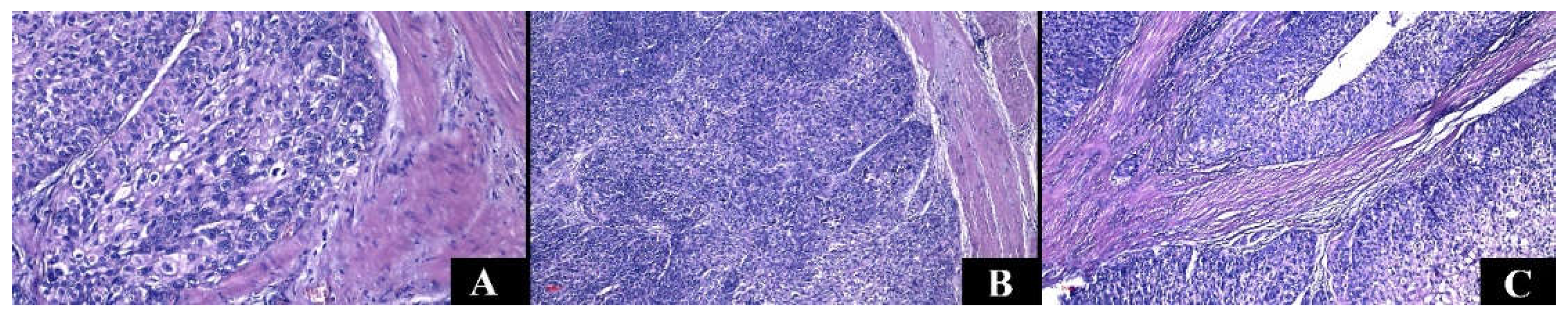
| Non-invasive urothelial carcinoma |
|
Flat or exophytic lesion | Urothelium | Varying degrees of cytoarchitectural atypia (fusion of papillae, disorganized tumor cells); cells with moderate or increased pleomorphism, mitotic activity. |
| Invasive urothelial carcinoma |
|
Sessile, polypoid, nodular, or ulcerative lesion | Urothelium | Urothelial cells with high-grade atypia can associate divergent differentiation. Various architectures: papillary, micropapillary, nested, or tubular. |
| Therapeutic management | Recommendations | Risks | |
| Active surveillance |
|
|
|
| Ablative techniques |
|
|
|
| Surgical techniques |
|
|
|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





