1. Introduction
An epiphrenic diverticulum is caused by the inability of lower esophageal sphincter (LES) to relax, which leads to an elevation of intraluminal pressure like that observed in achalasia [
1]. The laparoscopic approach for epiphrenic diverticulum is a common procedure, but there are apprehensions due to the perioperative complications associated with diverticulectomy [
2,
3]. Here we report a successfully treated case of esophageal achalasia combined with an epiphrenic diverticulum by a simultaneous laparoscopic procedure.
2. Detailed Case Description
2.1. Case Presentation
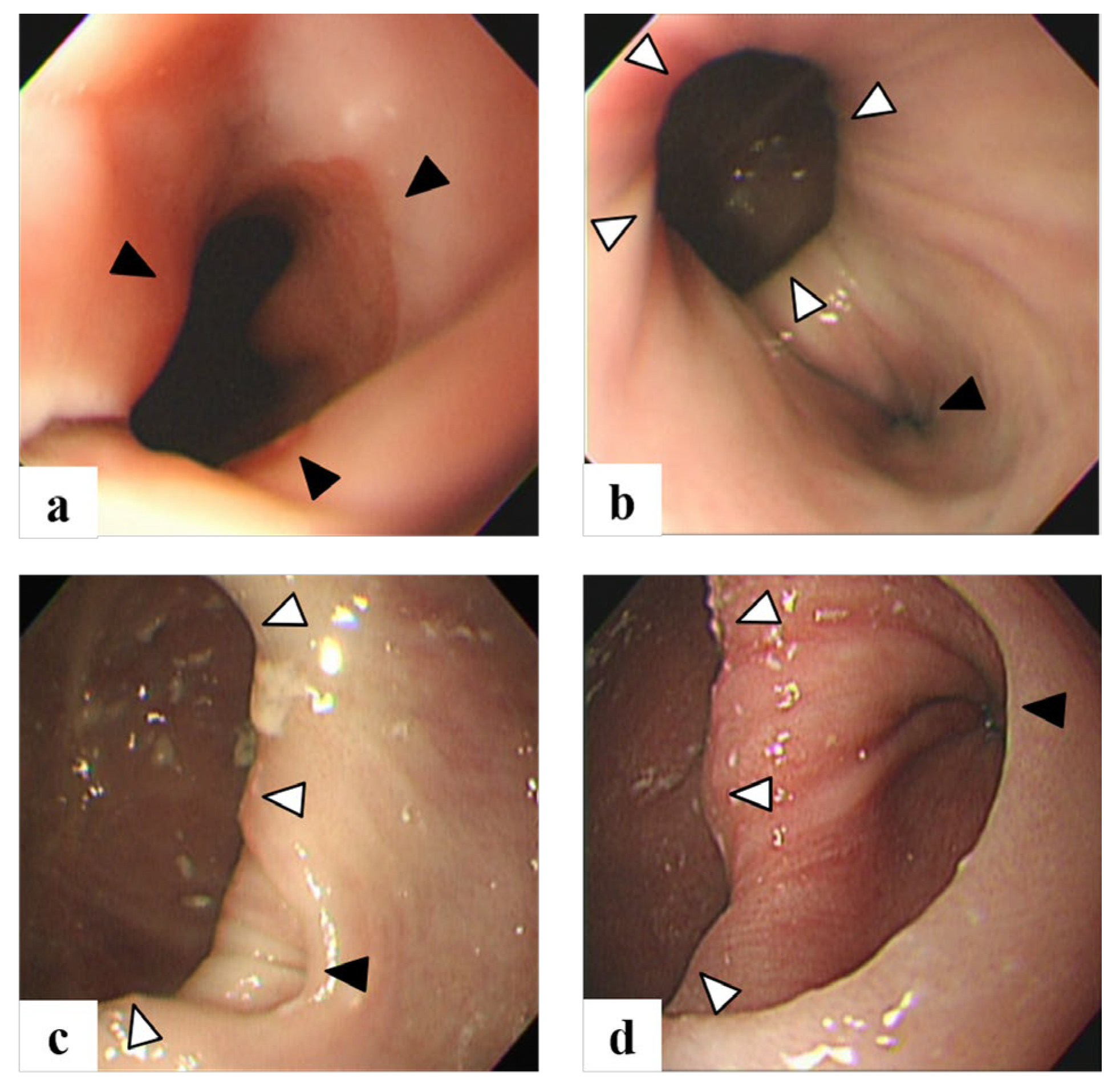
A 74-year-old man with past history of rheumatoid arthritis and cerebellar infarction was referred to our hospital with a complaint of ongoing chest discomfort while eating, since past 5 years. An esophagogastroduodenoscopy (EGD) performed 3 years back had indicated no abnormal esophageal findings. However, an EGD performed one year later, led to the diagnosis of an epiphrenic diverticulum in the lower esophagus. The changes in appearance of the diverticulum in these 3 years were shown in
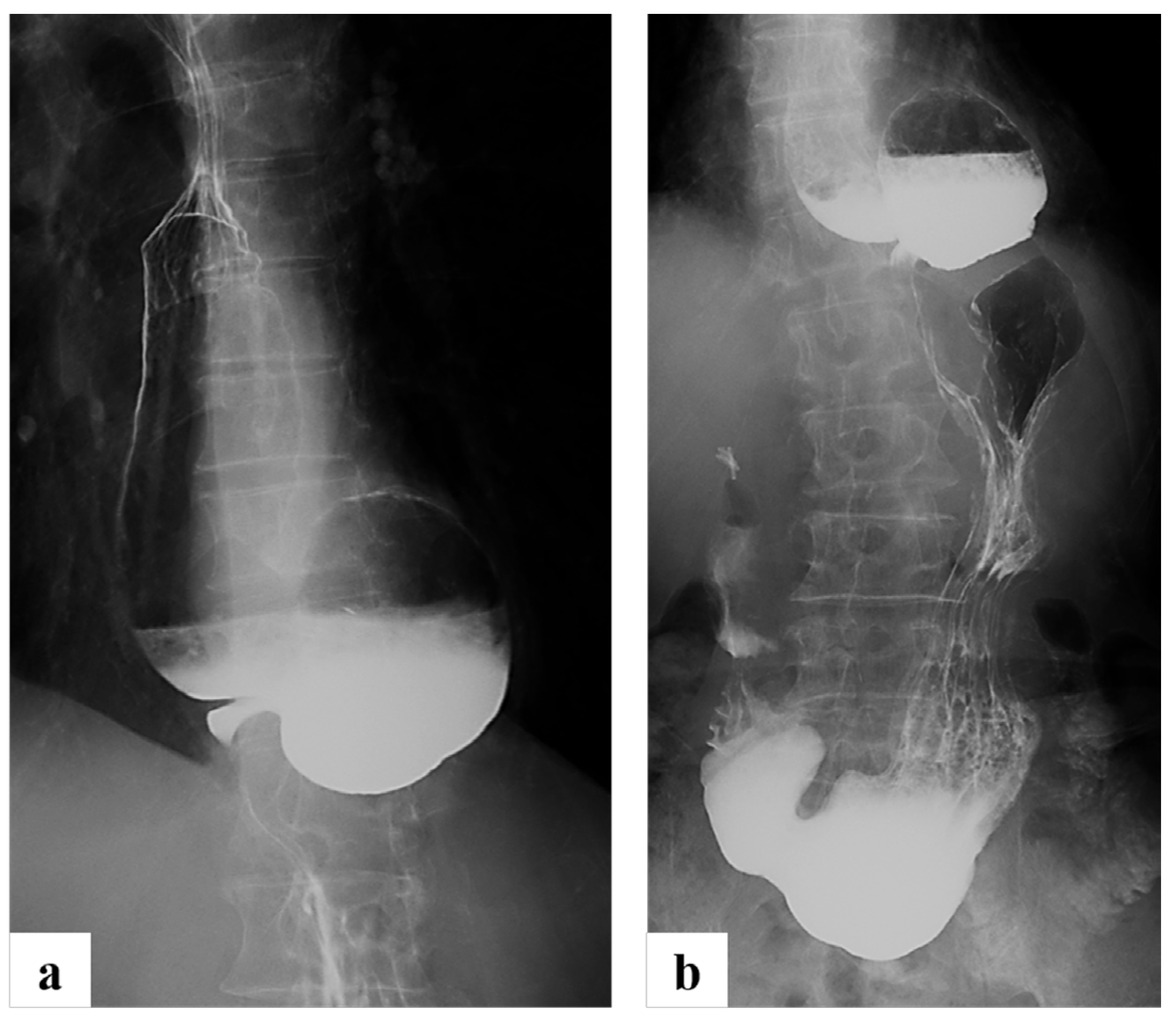
Figure 1. Further examination revealed a chronologically enlarged epiphrenic diverticulum at the left wall of the lower esophagus in the EGD. He was also suspected to have esophageal achalasia based on of L-shaped meandering of the esophagus as observed on barium esophagography (
Figure 2a). The lumen of the esophagus was narrowed due to the compression by the diverticulum at esophagogastric junction (EGJ) (
Figure 2b).
(a) Mild esophageal dilatation with narrowing at the EGJ was observed three years ago (black arrowhead). However, there was no abnormal findings which was suspected to be epiphrenic diverticulum. (b) EGD at one year ago revealed the occurrence of an epiphrenic diverticulum at the left wall of the lower esophagus (white arrowhead) with narrowing lumen at EGJ (black arrowhead). (c) EGD in five months before operation revealed the enlargement of diverticulum and the true lumen of esophagus was narrowed due to the compression by the diverticulum (black arrowhead). (d) Two months before operation, EGD revealed the further enlargement of diverticulum (white arrowhead).
2.2. Surgical Procedure
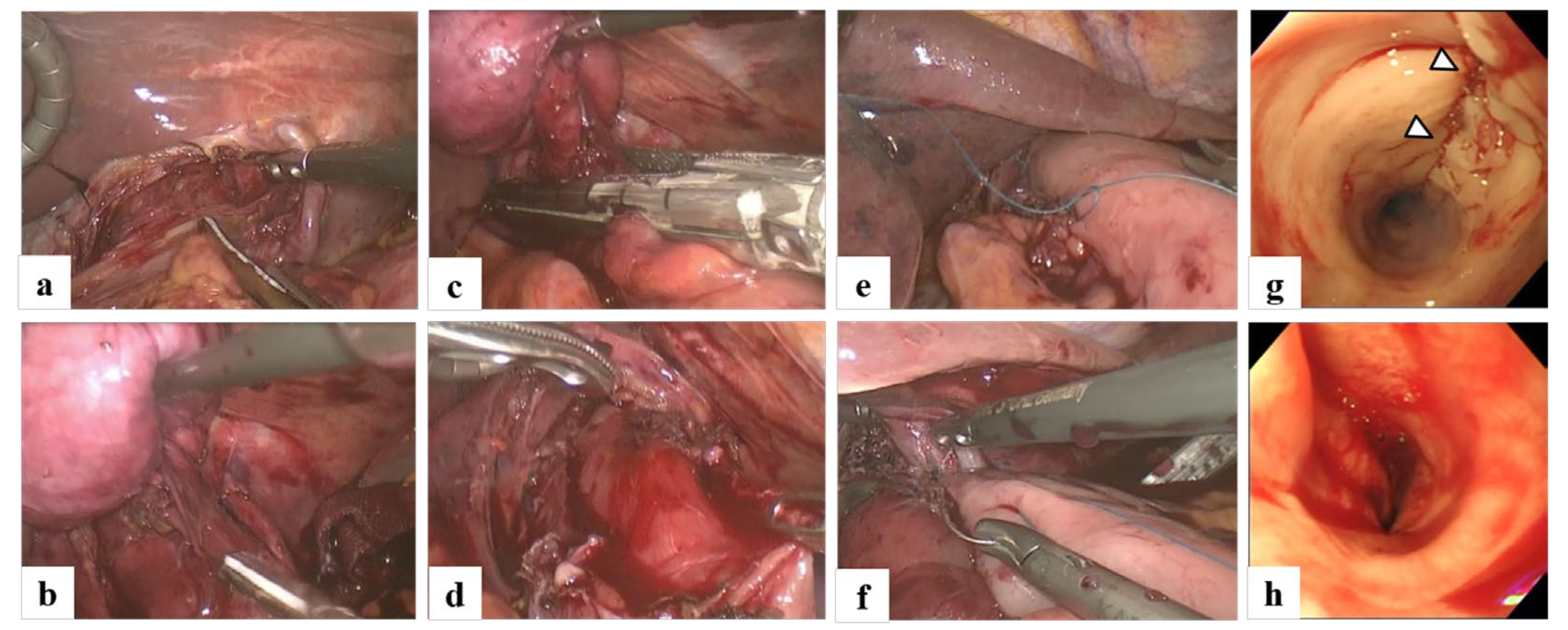
He was diagnosed with a combination of esophageal achalasia (advanced sigmoid type, Grade I) and an epiphrenic diverticulum; and a simultaneous laparoscopic surgery was performed. The surgery was performed in a lithotomy position in which the surgeon assumed the French position. The intraoperative surgical views were shown in
Figure 3. Five trocars were inserted into abdominal cavity: (1) periumbilical 12 mm camera port, (2) 12 mm left hypochondrial right-hand working port, (3) 5 mm right hypochondrial left-hand working port, (4) 5 mm left anterior axillary retraction port and (5) 5 mm subxiphoid liver retractor port. The round ligament of the liver was fixed to the abdominal wall with a piercing ligation using a 3-0 prolene needle suture, in order to keep the operative field broad. The liver branch of the vagal nerve was preserved. After exposure of the abdominal esophagus, the diaphragm was cut at the anterior part of esophageal hiatus (
Figure 3a), and the diverticular wall was separated from the surrounding organs using a combination of sharp and blunt dissection (
Figure 3b). A Penrose drain was passed behind the abdominal esophagus in order to prevent direct grasping of the stomach and esophagus, and to pull the stomach into the abdominal cavity for retraction, thereby, avoiding injury to both stomach and esophagus. The diverticular wall was then properly excised using two linear staplers, taking care to avoid the esophageal wall injury (
Figure 3c). The most critical part is pinching the diverticular wall by a suture device horizontally along the esophagus, and cutting it with several suture devices in a planned manner. After the resection of diverticulum, a craniocaudal incision was made in the esophageal muscle layer around the suture line after diverticulectomy (
Figure 3d), and both incisional line of the muscle layer and the suture line were wrapped by the fornix of stomach (
Figure 3e,f). After the resection of diverticulum, the absence of anastomotic leakage or intraluminal stenosis was confirmed by endoscopic intraluminal observation (
Figure 3g). Heller’s myotomy and Dor’s fundoplication were then performed to recreate the antireflux valve. Intraoperative EGD after Dor’s fundoplication revealed the enlargement of EGJ and the easiness of the scope passage (
Figure 3h). The surgery required 276 minutes and the intraoperative blood loss was 50 g.
2.3. Clinical Follow-Up
He started taking oral intake on the next operative day and was discharged on the twelfth postoperative day without any postoperative complications. Postoperative esophagography at five days after operation revealed no evidence of interference in the passage at the lower esophagus and no apparent regurgitation. The preoperative complaints of passage disorder rapidly improved after surgery and have not relapsed until the follow-up review at 70 months.
3. Discussion
The co-existence of an epiphrenic diverticulum and achalasia has been observed in only 2.2%–10% cases of achalasia [
2]. Thoracoscopic or laparoscopic diverticulectomy is necessary after treating abnormal esophageal motility dysfunction [
2,
3]. Achalasia is defined as an esophageal motor dysfunction characterized by LES relaxation failure and esophageal motility functional disorder [
4]. In cases with severe symptoms such as dysphagia, regurgitation to the oral cavity, chest pain, and body weight loss caused by achalasia or diffuse esophageal spasm (DES), endoscopic intervention or surgical procedure is often chosen [
4,
5]. Peroral endoscopic myotomy (POEM) is one of the non-surgical endoscopic procedures for the treatment of achalasia and DES, and is the emerging treatment of choice in Japan and worldwide [
5]. However, in cases where achalasia and epiphrenic diverticulum are the joint illnesses, POEM is not sufficient. In recent years, diverticular peroral endoscopic myotomy (D-POEM), which is a septotomy of the diverticulum using the POEM technique, has also been reported to be an effective endoscopic intervention for the treatment of epiphrenic diverticulum [
6,
7]. However, in the recent years, there have been some instances in which the occurrence of reflux symptoms and persistence of passage disorder have been observed after POEM [
5].
Generally, a Heller-Dor’s operation including the myotomy of lower esophagus and fundoplication has been performed as the surgical procedure for achalasia and epiphrenic diverticulum combination, and the success rate has been around 90% [
8]. Moreover, many institutions prefer laparoscopic procedure due to its widespread applications and superiority [
9]. There have been several reports of laparoscopic surgery for esophageal achalasia with epiphrenic diverticula, because of its minimally invasive nature [
8]. However, it should be noted that this procedure is not necessarily safe due to suture leakage and associated complications. Melman et al. and Achim et al. have reported that the suture leakage after the diverticulectomy occurs in approximately 18%–23% of all cases [
2,
3]. It has previously been reported that the diverticulectomy is commonly reinforced with layered sutures, and Heller-Dor’s procedure is performed at the contralateral wall of the esophagus [
10]. However, considering the occurrence of suture leakage at the site, it is theoretically considered logical and effective to reinforce this vulnerable site with Dor’s fundoplication.
In our study, there was some limitations. Firstly, the diagnosis of esophageal achalasia was not confirmed by manometry. Secondly, the functional improvement of LES, the esophageal motility, and the degree of postoperative gastro esophageal reflux were examined by manometry, or 24h pH monitoring. The most important point of our procedure is that the incisional line of the muscle layer as well as suturing line of diverticulectomy were wrapped by the fornix of the stomach to make up for the wall strength. The result of this procedure has been satisfactory without any complications. Depending on the location and size of the epiphrenic diverticulum and the degree of achalasia, further adjustments may be required for each case.
4. Conclusions
We focused on approaches and surgical details while performing Heller-Dor’s simultaneous laparoscopic surgery for treating patient suffering from esophageal achalasia with an epiphrenic diverticulum.
Author Contributions
Conceptualization, K.O. and I.N.; resources, J.K. and H.S.; writing—original draft preparation, K.O.; writing—review and editing, N.I.; supervision, H.T.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
All data generated during this report are included in this published article. Further enquiries can be directed to the corresponding author.
Acknowledgments
The Authors thank Enago (
www.enago.jp) for editing a draft of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
List of abbreviations: LES, lower esophageal sphincter; EGD, esophagogastroduodenoscopy; EGJ, esophagogastric junction; DES, diffuse esophageal spasm; POEM, peroral endoscopic myotomy; D-POEM, diverticular peroral endoscopic myotomy
References
- Nehra, D.; Lord, R.V.: DeMeester, T.R.; Theisen, J.; Peters, J.H.; Crookes, P.F.; Bremner, C.G. Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg 2002, 235(3), 346-354. [CrossRef]
- Nadaleto, B.F.; Herbella, F.A.M.; Patti, M.G. Treatment of achalasia and epiphrenic diverticulum. World J Surg 2022, 46(7), 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Achim, V.; Aye, R.W.; Farivar, A.S.; Vallières, E.; Louie, B.E. A combined thoracoscopic and laparoscopic approach for high epiphrenic diverticula and the importance of complete myotomy. Surg Endosc 2017, 31(2), 788–794. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, S.N.; Friedel, D.; Modayil, R.; Parkman, H.P. Diagnosis and management of esophageal achalasia. BMJ 2016, 354:i2785. [CrossRef]
- Shiwaku, H.; Inoue, H.; Yamashita, K.; Ohmiya, T.; Beppu, R.; Nakashima, R.; Takeno, S.; Sasaki, T.; Nimura, S.; Yamashita, Y. Peroral endoscopic myotomy for esophageal achalasia: Outcomes of the first over 100 patients with short-term follow-up. Surg Endosc 2016, 30(11), 4817–4826. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zeng, X.; Yuan, X.; Chang, K.; Sanaei, O.; Fayad, L.; Kumbhari, V.; Singh, V.; Kalloo, A.N.; Hu, B.; Khashab, M.A. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: The first multicenter D-POEM experience. Endoscopy 2019, 51(4), 346–349. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Takeuchi, M.; Hashimoto, S.; Mizuno, K.; Furukawa, K.; Sato, A.; Yokoyama, J.; Terai, S. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol 2019, 25(12), 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Melman, L.; Quinlan, J.; Robertson, B.; Brunt, L.M.; Halpin, V.J.; Eagon, J.C.; Frisella, M.M.; Matthews, B.D. Esophageal manometric characteristics and outcomes for laparoscopic esophageal diverticulectomy, myotomy, and partial fundoplication for epiphrenic diverticula. Surg Endosc 2009, 23(6), 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Katada, N.; Sakuramoto, S.; Yamashita, K.; Shibata, T.; Moriya, H.; Kikuchi, S.; Watanabe, M. Recent trends in the management of achalasia. Ann Thorac Cardiovasc Surg. 2012, 18(5), 420–428. [Google Scholar] [CrossRef]
- Hirano, Y.; Takeuchi, H.; Oyama, T.; Saikawa, Y.; Niihara, M.; Sako, H.; Omagari, K.; Nishi, T.; Suzuki, K.; Hibi, J.; Kitagawa, Y. Minimally invasive surgery for esophageal epiphrenic diverticulum: The results of 133 patients in 25 published series and our experience. Surg Today 2013, 43(1), 1–7. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).