1. Introduction
Despite important advancements in diagnostic, methods of treatment and follow-up [4-6], coronary artery disease represents a multifaceted pathology that requires the understanding of multiple physio-pathological mechanisms for which no standardized treatment exists [
8]. Coronary angiography represents the golden standard for evaluation of atherosclerotic disease representing the diagnostic standard in indicating the need for revascularization. However, it presents numerous drawbacks and quantifying the severity of an atherosclerotic lesion by invasive coronary angiography may be subjective and operator dependent. Also, moderate stenoses may be in fact hemodynamically significant. The same applies for apparently severe angiographic stenoses that can prove to be in fact without hemodynamic significance.
The need for additional tools has emerged as a need for the cardiologist to have a better understanding of which coronary lesions should be treated conservatory and which should be treated by revascularization (interventional or surgical) [
9]. Unfortunately, both imaging Optical Coherence Tomography (OCT) and hemodynamic Fractional Flow Reserve (FFR) methods for assessing the severity of coronary artery disease present numerous drawbacks- OCT requires multiple administrations of contrast media increasing the risk of contrast nephropathy and prolongs the time of the procedure with a higher radiation exposure of both the medical personnel and the patient while FFR requires administration of adenosine (intravenous or intracoronary).
Several studies have investigated the correlation between minimal luminal area (MLA) measured by OCT and FFR in patients with coronary artery disease for patients with chronic coronary syndromes [10-12] . The aim of the studies was to establish a relationship between the anatomical and physiological assessments of coronary lesions in patients with acute myocardial infarction. Positive correlations between MLA and FFR suggest that lesions with a smaller luminal area on OCT may indeed be functionally significant.
Understanding the correlation between OCT-derived minimal luminal area and FFR has important clinical and interventional implications. Combining anatomical information from OCT with physiological data from FFR can enhance the accuracy of lesion assessment. This integrated approach assists the interventional cardiologist in making informed decisions regarding the need for revascularization procedures, optimizing patient care and outcomes.
Despite the potential benefits, challenges exist in establishing a universally applicable correlation between OCT-derived MLA and FFR. Variability in image interpretation, operator dependence, and the dynamic nature of coronary physiology are factors that need to be considered. Future research should focus on refining these correlations and exploring additional parameters that may improve the accuracy of non-invasive assessments.
The present analysis studies a population consisting of patients with acute myocardial infarction, evaluating the capability of OCT to differentiate the hemodynamic significance of intermediate lesions, with the possibility of complete revascularization during the index hospitalization, without the need for performing FFR assessment. A clear OCT parameter cut-off for each vessel may translate into a shorter hospitalization, reduction of costs and better outcomes for the patient.
2. Materials and Methods
2.1. Study Population
All patient presented with acute ST-elevation myocardial infarction or non-ST elevation myocardial infarction and were treated according to the latest European guidelines [
7,
9,
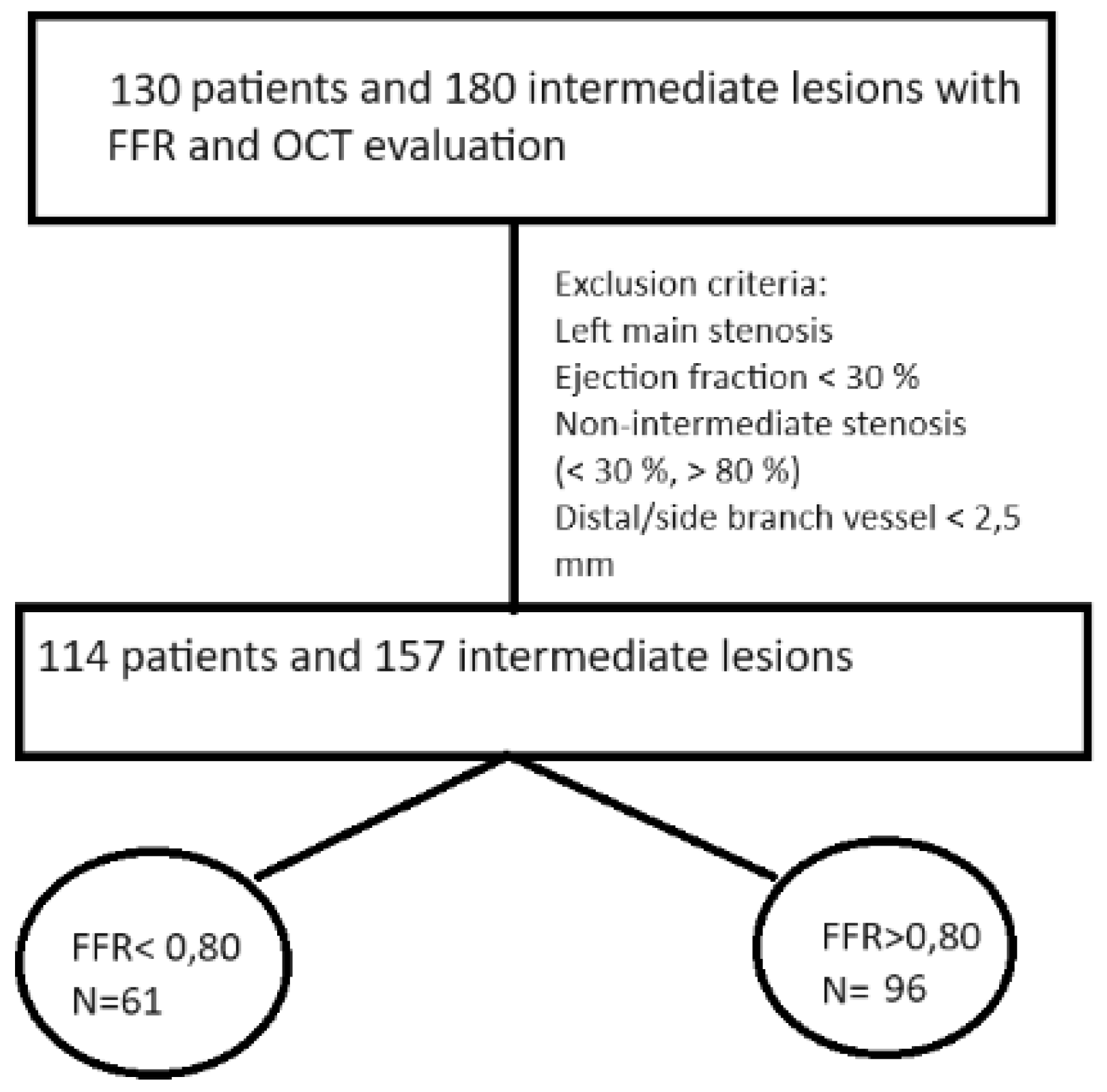
13]. In the index procedure the culprit vessel was treated and the patients who had intermediate stenoses of non-culprit vessels were included in the study. The patients who satisfied the following criteria were included: recent acute myocardial infarction, intermediate coronary lesion on the non-culprit vessel defined as 30-80 % stenosis on angiography (visual or QCA), no left main or distal/small side branch lesions, ejection fraction grater than 30 %. Clinical patient characteristics were collected from medical charts and all patients signed the written informed consent before the first and second coronary catheterizations. 114 patients and 157 lesions were selected for analysis (
Figure 1).
2.2. Coronary Angiography Protocol
After the diagnostic of ST- segment elevation myocardial infarction or non-ST elevation myocardial infarction coronary angiography was performed. For patients with non-ST elevation myocardial infarction at very high risk coronary angiography was performed within 2 hours after presentation and for patients with non-ST elevation myocardial infarction at high risk coronary angiography was performed in the first 24 hours.
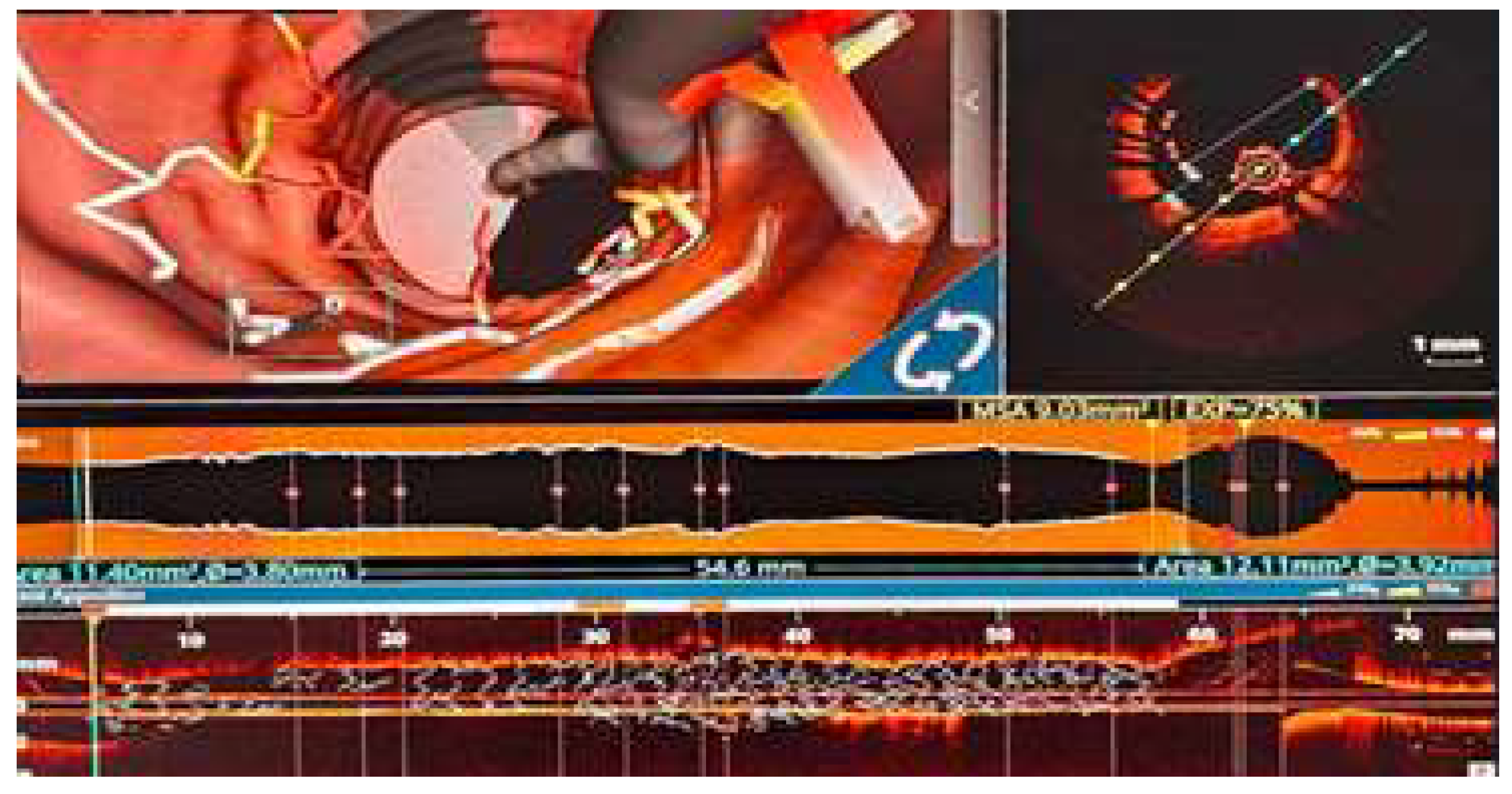
The culprit lesion was treated at operator’s discretion and patients with intermediate stenoses on non-culprit vessels were selected for inclusion in the study. The second coronary angiography was performed between days 3-5 of the index hospitalization. OCT was performed on the culprit lesion with extensive images acquisitions starting from 20 mm proximal the implanted stent up to 20 mm distal to the stent. Expansion of the stent, areas of malposition (image 1), proximal or distal dissection areas, plaque protrusion and thrombotic masses were assessed by OCT. Supplementary post dilatation was performed when considered necessary by the operator when severe under expansion and malposition were present[
14], with final OCT reevaluation being performed.
The non-culprit vessel/vessels with intermediate stenoses (estimated visually or by QCA) were assessed by FFR with intracoronary administration of adenosine in different quantities with the aim of obtaining an EKG response or a clear separation of the Pd/Pa curves. Regardless of the FFR result, OCT was performed, with multiple measurements being carried at the level of the atherosclerotic plaque. In case of FFR under 0,80 myocardial revascularization by implantation of one or multiple stent was performed at this level, followed by OCT and FFR reevaluation. Additional post dilatation or stent implantation was performed based on the OCT imaging at operator’s discretion. After each post dilatation/stent implantation OCT was considered a mandatory step in order to ensure an optimal final result. The final OCT targets were pursued: malposition of less than 400 µm, expansion > 90 % of the distal reference lumen area, no proximal or distal edge dissections.
Image 1.
OCT with 3D reconstruction. Severe malposition of the stent requiring 1:1 noncompliant balloon post dilatation.
Image 1.
OCT with 3D reconstruction. Severe malposition of the stent requiring 1:1 noncompliant balloon post dilatation.
2.3. Fractional Flow Reserve (FFR) as a Physiological Index:
For the FFR analysis we utilized the Pressure Wire X guidewire from Abbott. After engaging the ostium of the coronary artery avoiding aggressive cannulation, the FFR guidewire is advanced in the vessel (proximal to the lesion),zeroed and the pressure equalized, followed by advancement of the pressure wire distal to the lesion. FFR was performed by intracoronary infusion of adenosine in different quantities (50/100/150/200/250/300 ug) depending on the interrogated vessel, aiming either an ECG response or a clear separation of the Pd/Pa curves. The cutoff value for the FFR was 0,80.
2.4. Optical Coherence Tomography Analysis
Optical Coherence Tomography was performed in all patients using the St Jude OCT console system and the DragonFly Optis kit catheter from Abbott Cardiovascular. The non-culprit vessel with intermediate lesions were analyzed after the FFR assessment and numerous OCT data were introduced in a complex database. For the current analysis we extracted the minimal luminal area (MLA), the length of the atherosclerotic plaque, proximal and distal reference luminal area and minimal diameter. MLA was defined as the cross-section with the smallest area[
8]. The proximal and distal luminal area were defined as the cross-sections where the plaque begins/ends, measurement being carried where OCT showed normal or near normal aspect of the coronary wall[
8]. The reference luminal area (RA) was calculated by adding proximal and distal luminal area and dividing the result by two[
8]. Percent luminal area stenosis (PAS) was calculated using the reference luminal area (RA) minus minimal luminal area (MLA), divided by RA.
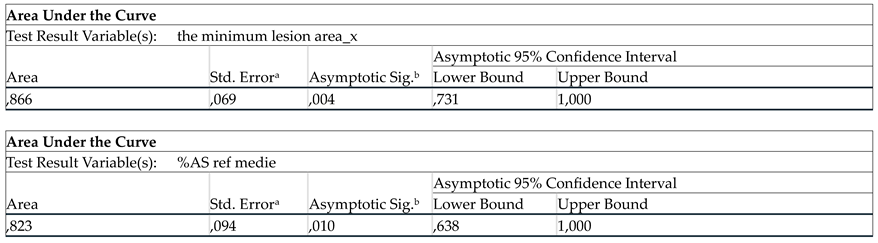
2.5. Statistical Analysis
Statistical analysis was performed using SPSS (version 26.0, SPSS Inc., Chicago, IL, USA). Data analysis was performed on per-lesion basis. To determine the cut-off value for MLA and PAS in predicting FFR value ≤0,8 we used the Youden method based on the receiver operating curves (ROCs) representation. Area under the ROC curve (AUC) values and the 95% confidence intervals were calculated. The sensitivity, specificity, and accuracy were calculated using the determined cut-off values for MLA and PAS.
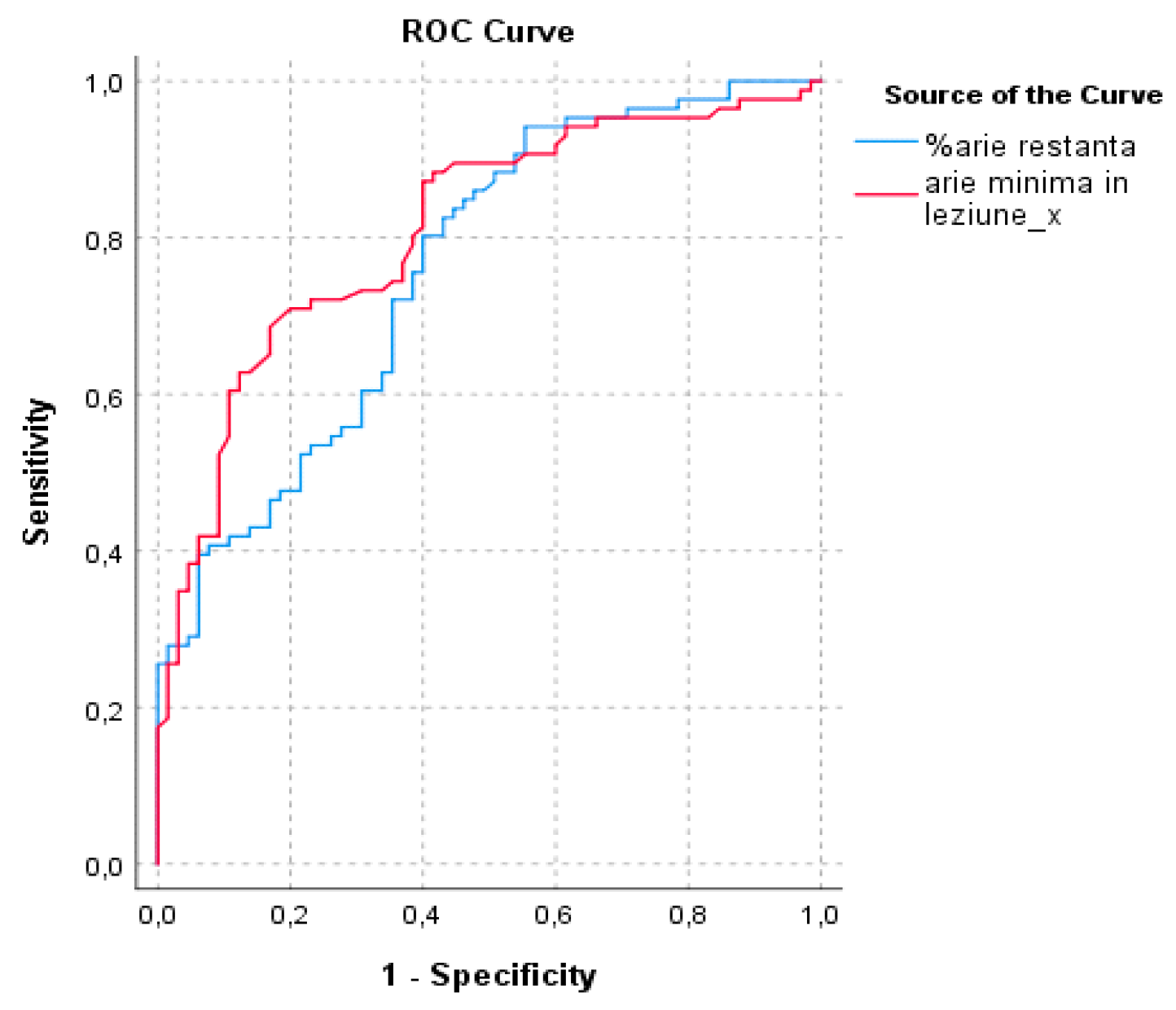
In order to be able to compare the statistical significance of PSA compared to MLA, a surrogate parameter was used - the remaining area (RMA) which is represented by the difference of reference area (RA) and minimal luminal area (MLA).
3. Results
Data analysis was performed in a structured way. Firstly, analysis for the correlation of minimal luminal area and fractional flow reserve was done.
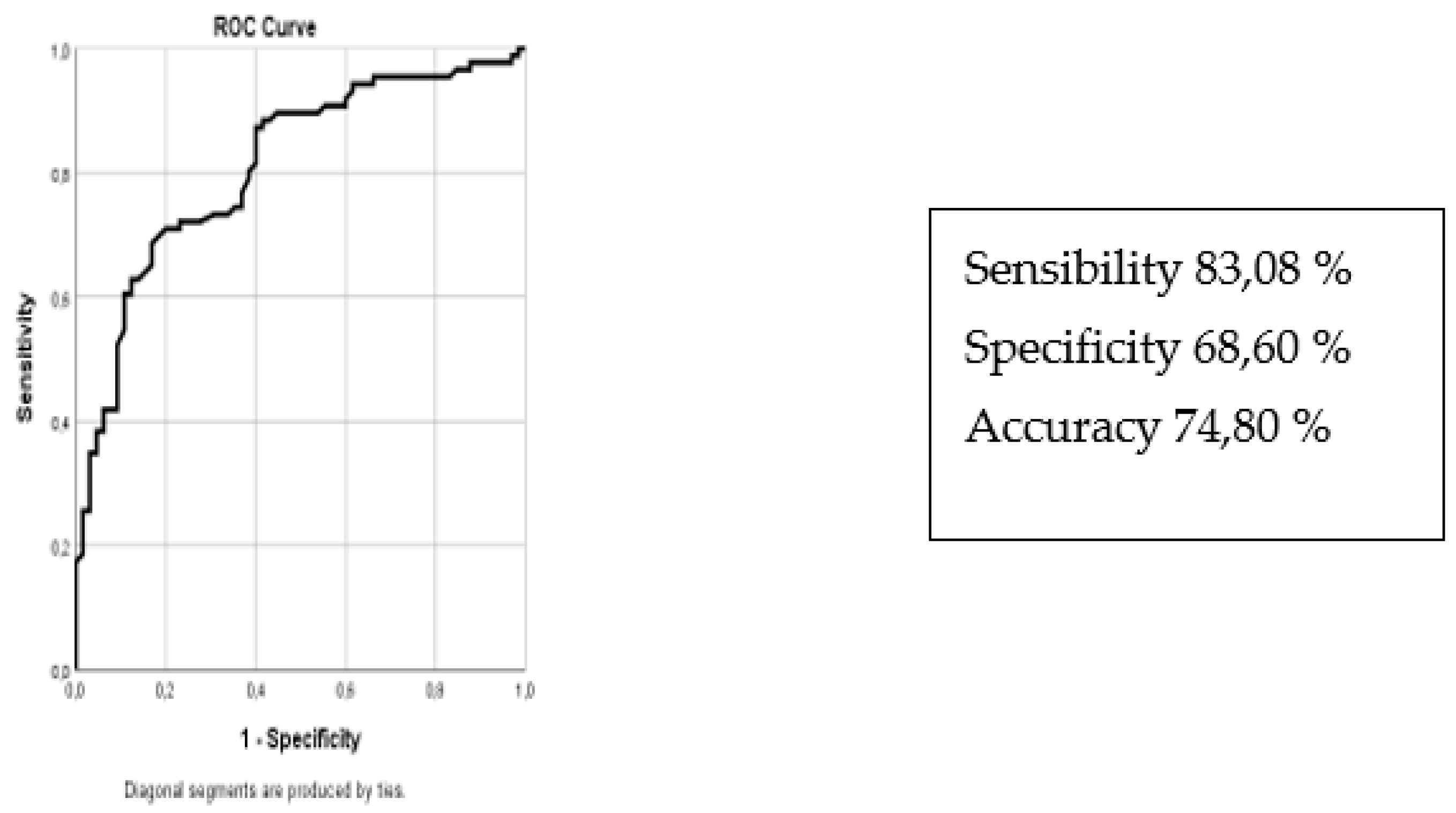
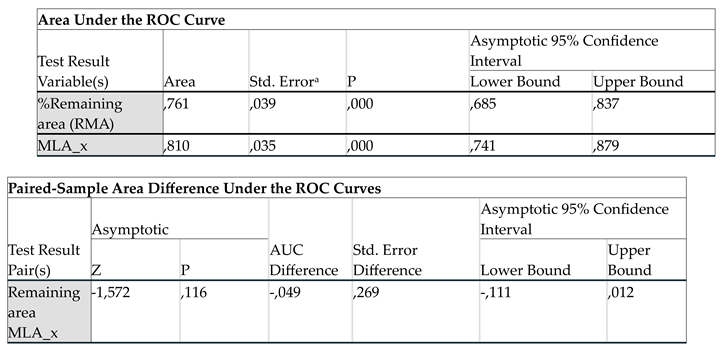
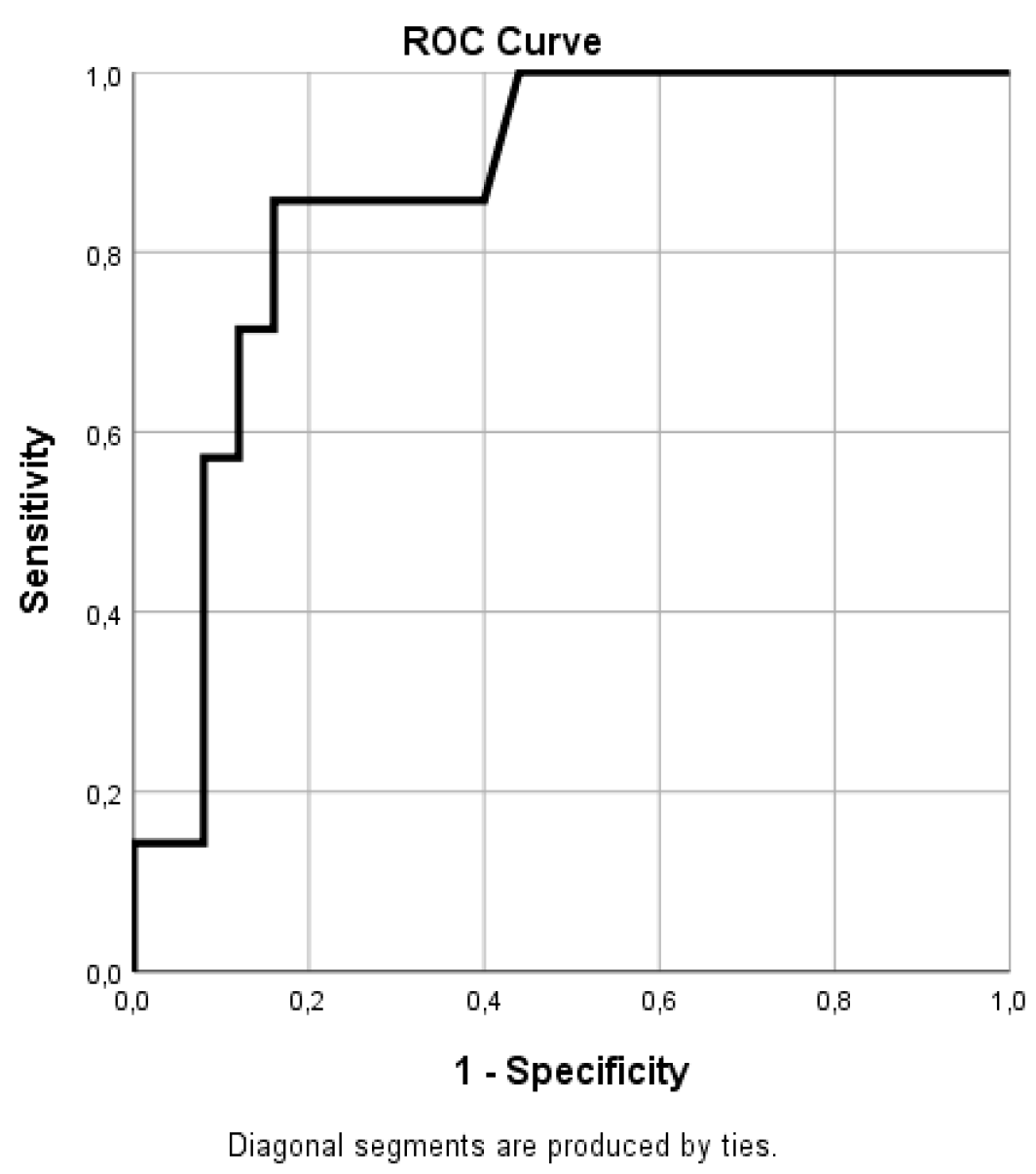
Figure 2 shows the ROC curve for OCT derived MLA to predict FFR< 0,80.
Figure 2.
ROC curve for OCT derived MLA to predict fractional flow reserve (FFR) <0,8.
Figure 2.
ROC curve for OCT derived MLA to predict fractional flow reserve (FFR) <0,8.

Area under the curve (AUC) analysis shows an important correlation between the MLA value and the proportion of positive FFR. A value of AUC of 0,810 (CI 95 % 0,741-0,879) shows a good discriminatory capacity. Based on the ROC Curve the best cut-off value for the minimal lumen area obtained is of 2,08 mm2 with a sensibility of 83,08 %, specificity 68,60 %, accuracy 74,80 % (figure 2).
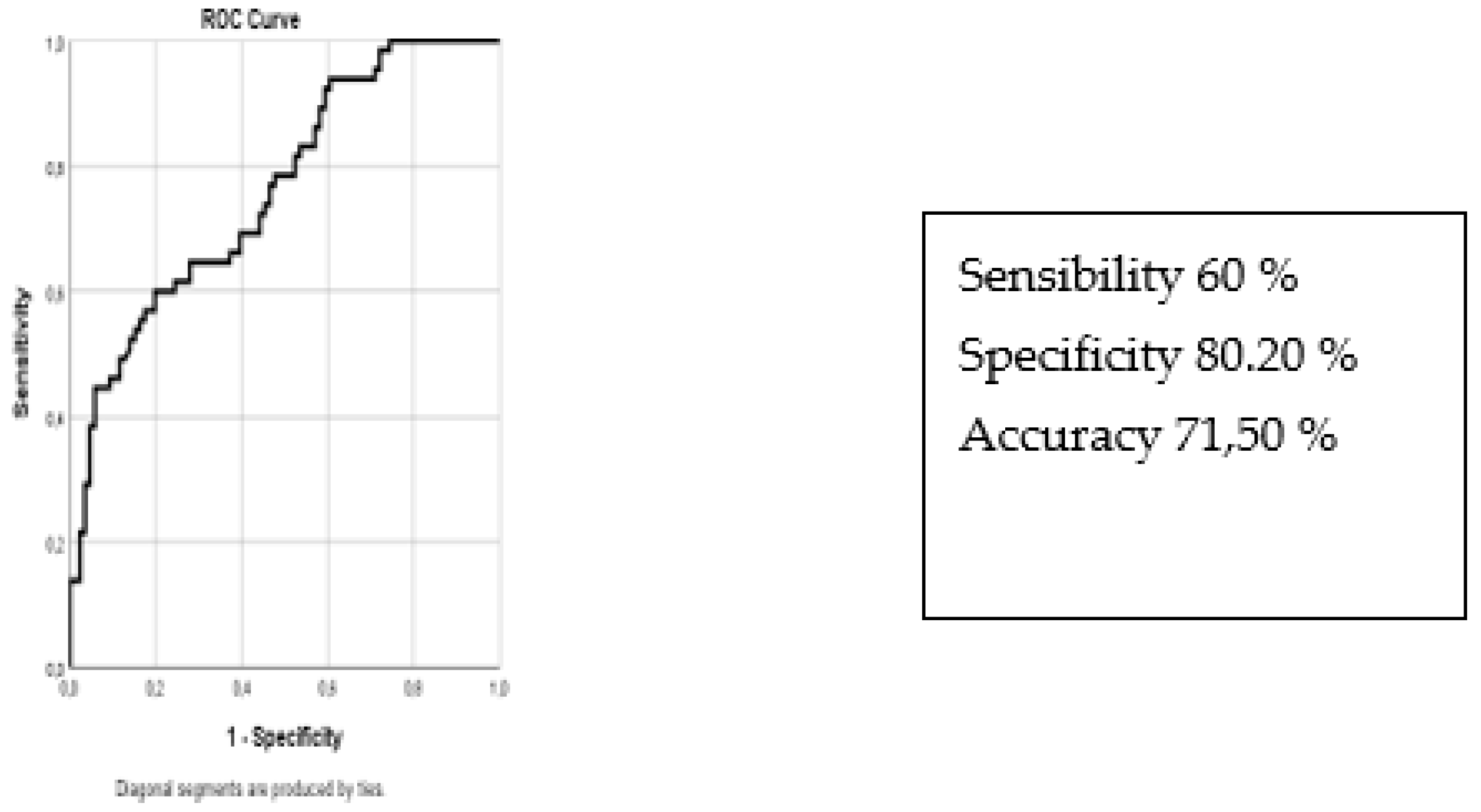
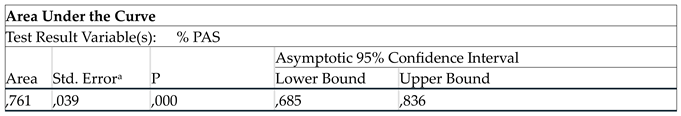
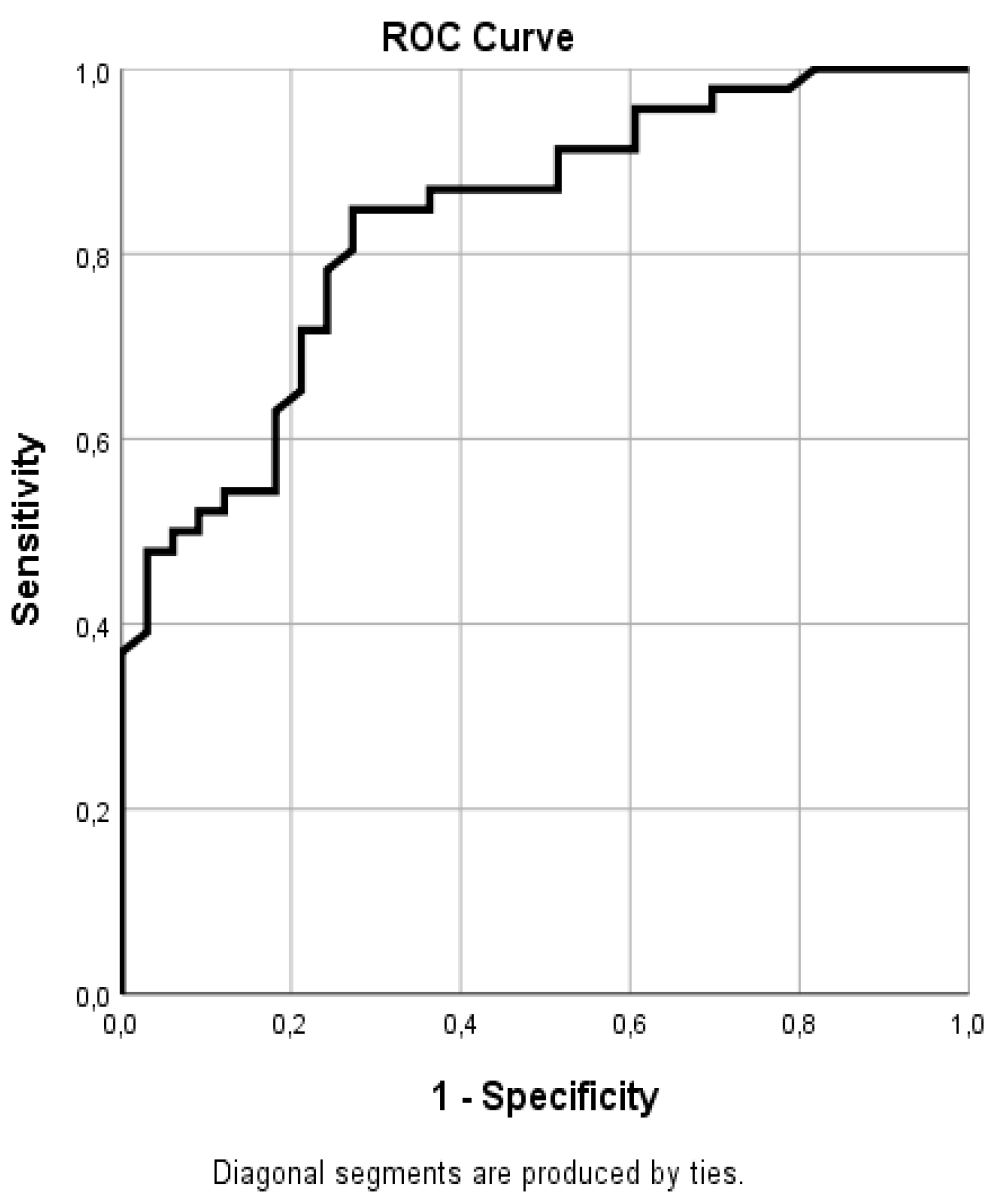
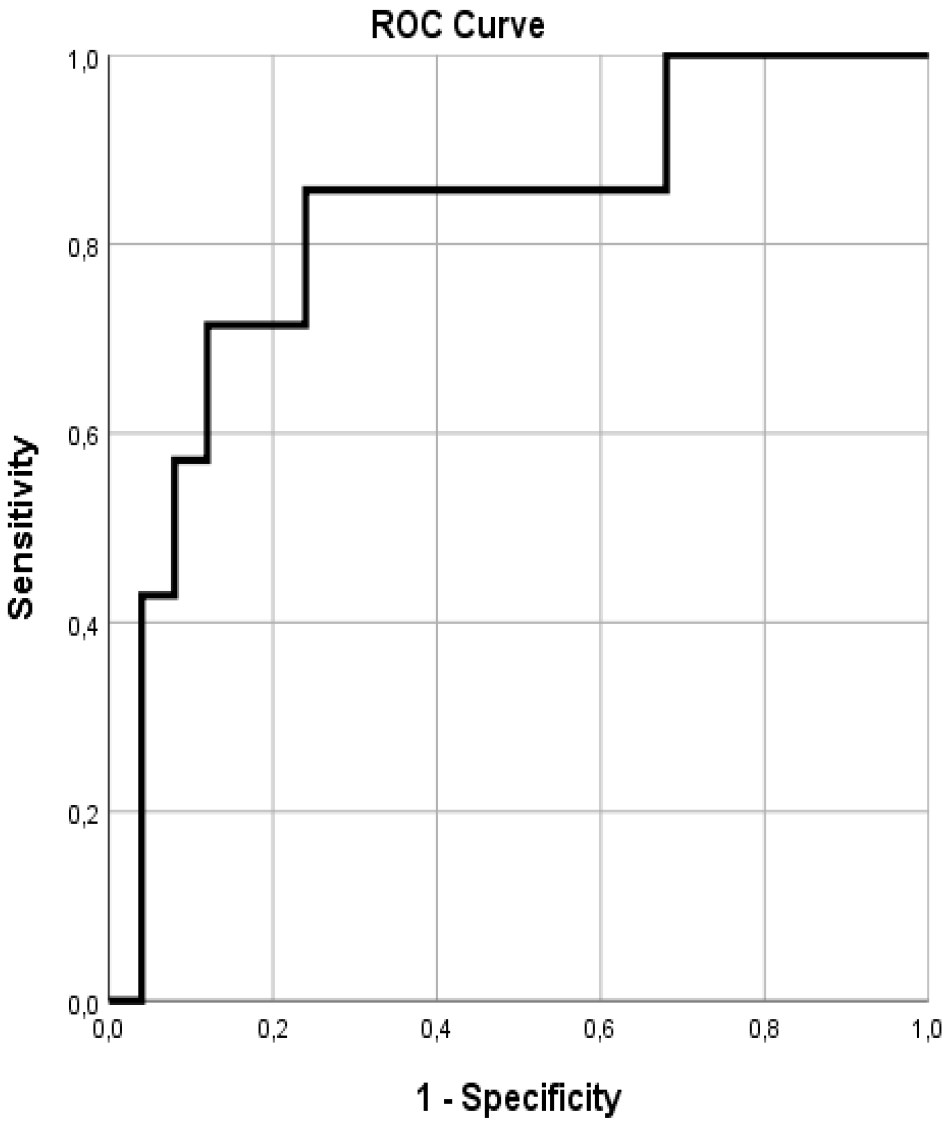
A similar analysis (
Figure 3) of the percent luminal stenosis area (PSA) shows a good correlation with the fractional flow reserve area (FFR). There is a good correlation of percent PAS and FFR value with a cut-off value of 76,85% which corresponds to a diametrical stenosis of 50%.
Figure 3.
ROC curve for percent luminal area stenosis (PAS) to predict FFR <0,80.
Figure 3.
ROC curve for percent luminal area stenosis (PAS) to predict FFR <0,80.
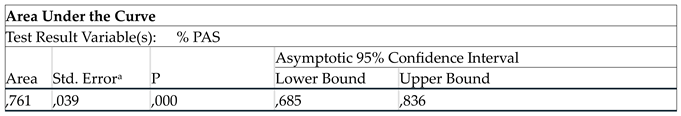
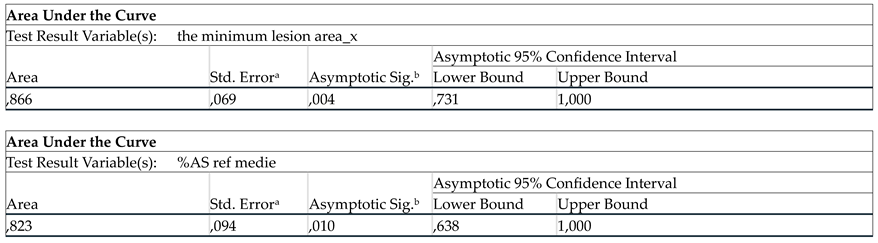
It was performed a comparative analysis of PSA and MLA to predict an ischemic threshold for FFR (
Figure 4). Comparing the two methods, there are no significantly differences between the MLA and PSA to predict an FFR under 0,80 (p>0,05).
Figure 4.
shows comparative analysis of remaining area (RMA) and minimal luminal area (MLA).
Figure 4.
shows comparative analysis of remaining area (RMA) and minimal luminal area (MLA).
The Results of the Analysis on Each Individual Coronary Artery
A very important part of the analysis was represented by the correlation of OCT derived parameters and FFR values for each separate coronary territory in order to depict whether there are significant differences. Out of the 157 lesion included in the analysis, 80 lesions were located on the left anterior descending artery (LAD), 33 lesions on the circumflex artery (CX) and 44 on the right coronary artery (RCA).
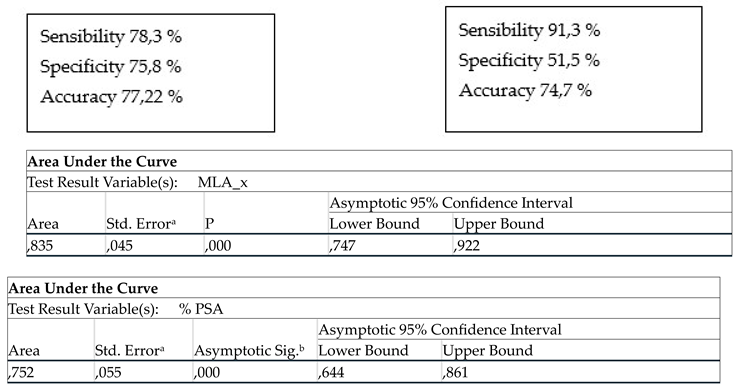
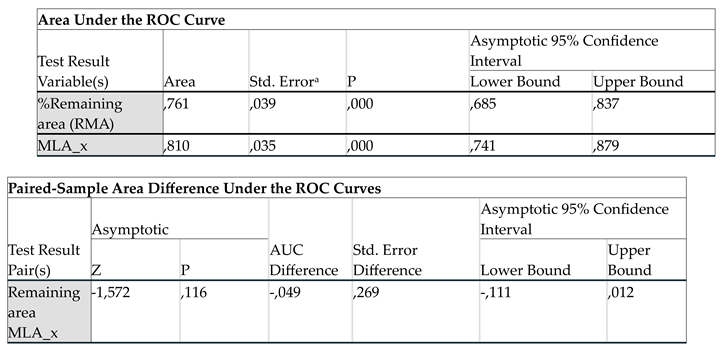
For the
left anterior descending artery (
Figure 5 and
Figure 6) a cut-off point for the MLA of 2,23 mm
2 and for the PSA of 65,3 % were obtained.
Figure 5.
ROC curve for MLA in LAD.
Figure 5.
ROC curve for MLA in LAD.
Figure 6.
ROC curve for PSA in LAD.
Figure 6.
ROC curve for PSA in LAD.
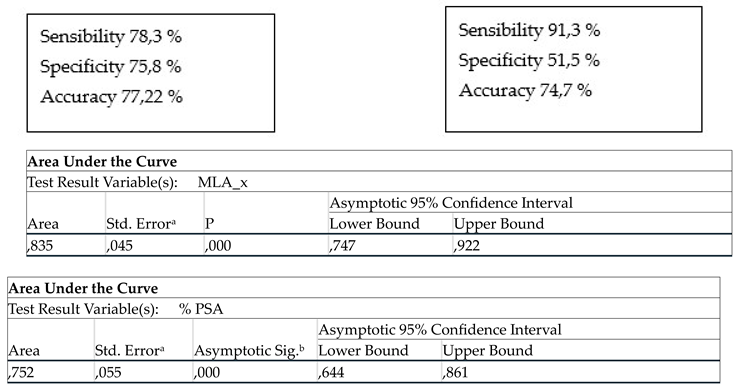
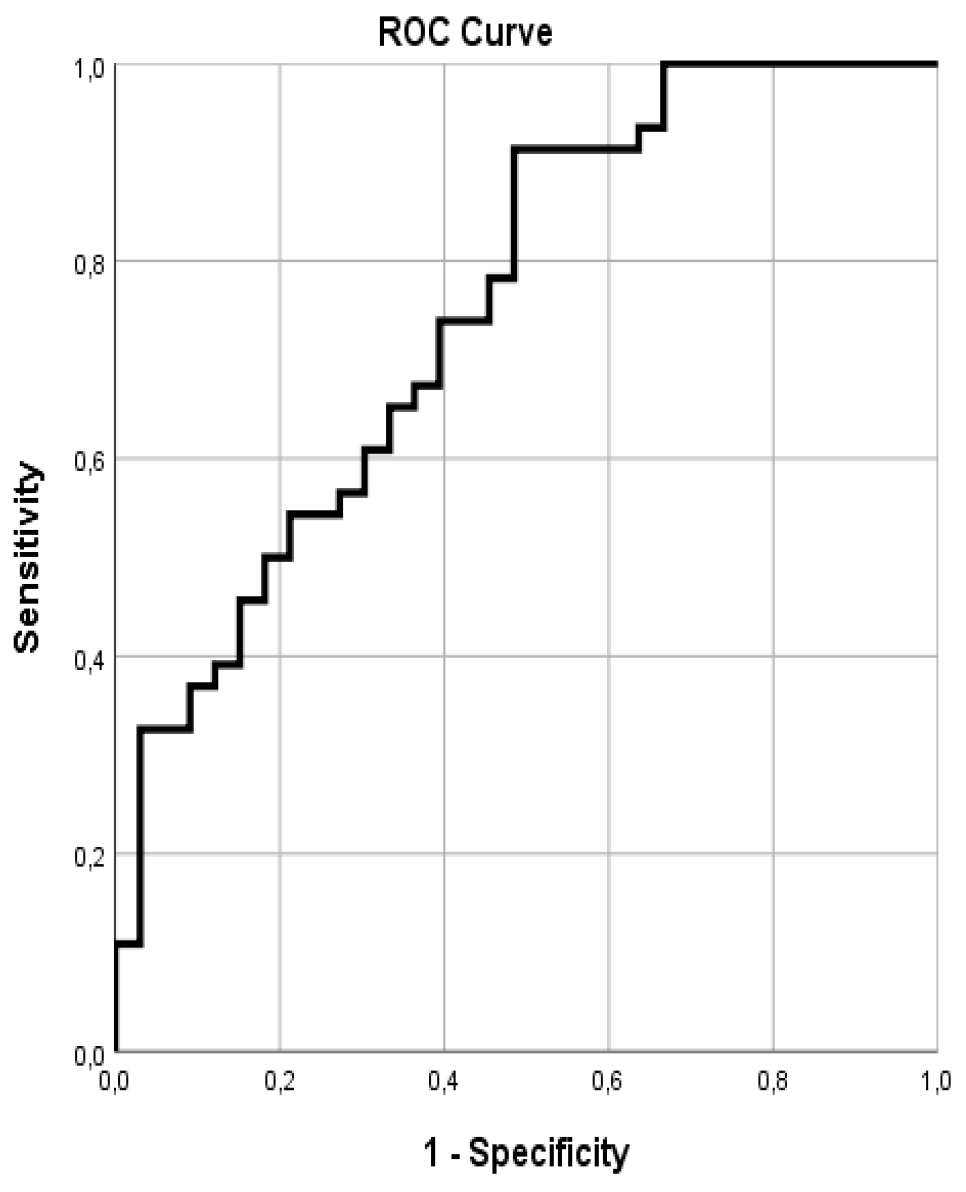
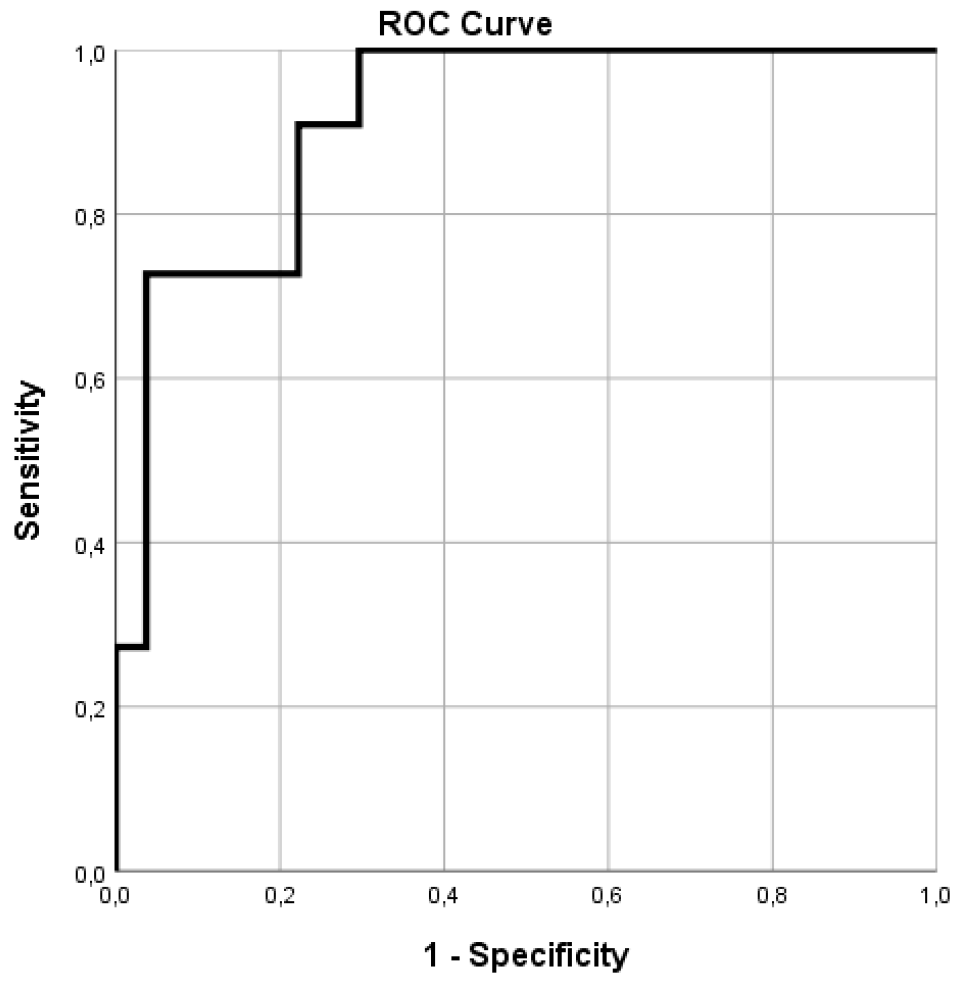
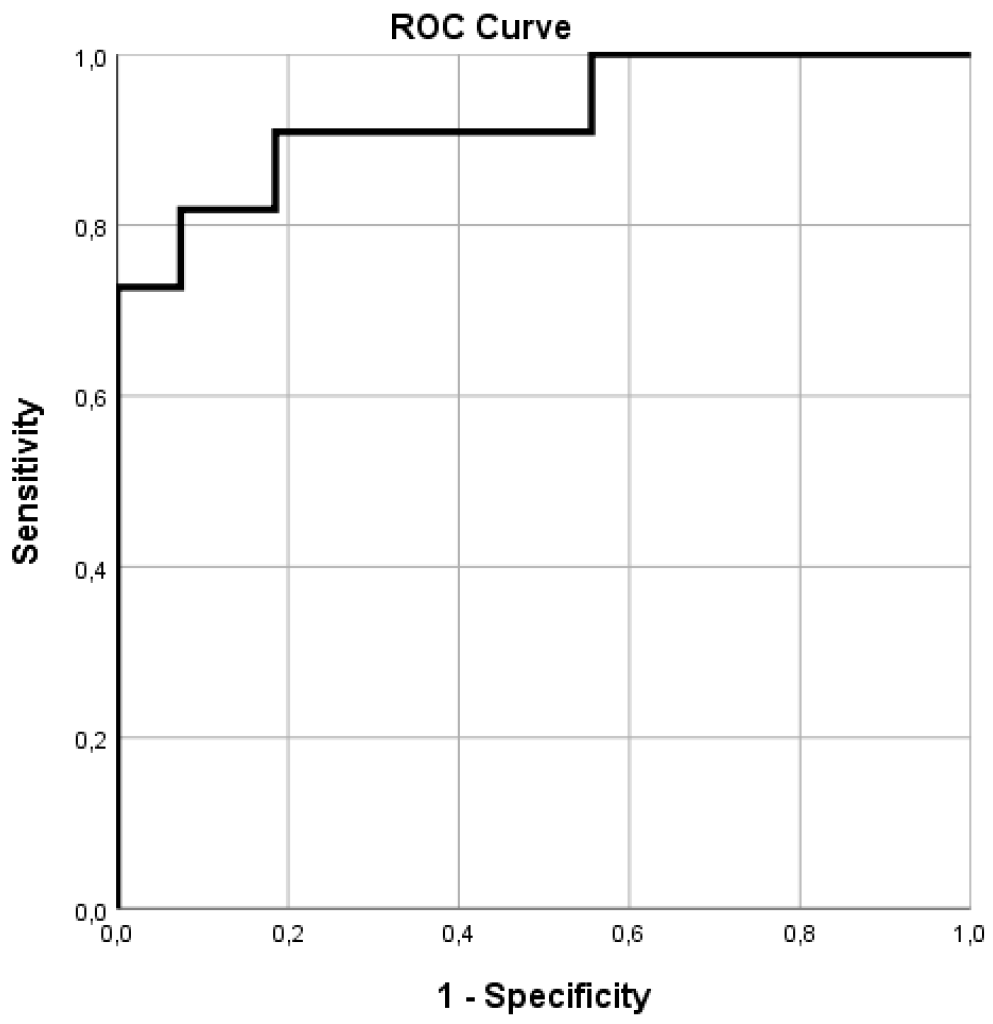
For the
right coronary artery the cut-off value for the MLA was 2,28 mm
2, with a better area under the curve (AUC) than that observed in the case of the left descending artery (
Figure 7). For the PAS (
Figure 8) the cut-off was 78,5 %, with a very low specificity (33,3%) and accuracy (52,6%).
Figure 7.
ROC curve for the MLA in RCA.
Figure 7.
ROC curve for the MLA in RCA.
Figure 8.
ROC curve for the PSA in RCA.
Figure 8.
ROC curve for the PSA in RCA.
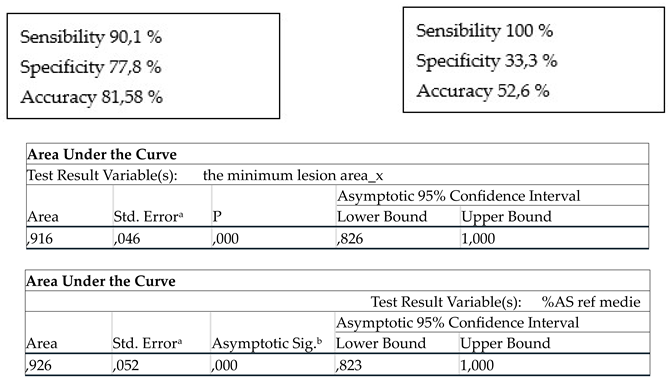
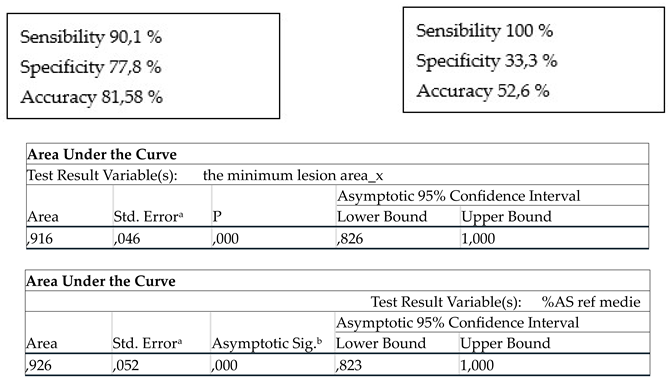
For the
circumflex artery a MLA of 1,16 mm
2 was obtained, with a very good sensibility (100 %) but with a very low specificity (48%) and accuracy (59,4%) (
Figure 8). A cut-off value of 76,2 % was obtained for the PAS (
Figure 9).
Figure 8.
ROC curve for the MLA in CX.
Figure 8.
ROC curve for the MLA in CX.
Figure 9.
ROC curve for the PSA in CX.
Figure 9.
ROC curve for the PSA in CX.
4. Discussion
The therapeutic management of non-critical (intermediate) coronary lesions still represents a challenge. Fractional flow reserve remains the gold standard in the assessment of severity of the coronary stenosis.
Although, multiple studies have addressed the possible correlation between OCT and FFR, there are insufficient data to obtain a standardized value which can be universally applied to the heterogenous population from daily practice. All the patients from our study presented a acute myocardial infarction. The present analysis has numerous findings which are in line with previous reported data.
There is a wide range of OCT parameters values which can have a strong correlation with hemodynamic significance of a coronary lesion, but this values depend on the cut-off chosen for the differentiation of ischemic and non-ischemic lesions[
11,
15,
17]. While for a cut-off value of 0,75 a much lower threshold for MLA was obtained in other studies[
11], for the present analysis the FFR cut-off was chosen to be 0,80 for the purpose of being in line with the majority of studies addressing the same parameters. According to our results, a MLA derived from OCT has a good correlation with a FFR value under 0,80.
In our research the cut-off was established to 2,08 mm
2 which is slightly above the range of cut-offs published until the present day, ranging between 1.55 and 2.05 mm
2 for the same value of the fractional flow reserve. Studies using a cut-off for the FFR of less than 0,75 have reported values for the minimal luminal area between 1.39 mm
2 and 1.91 mm
2[
12,
15]. Also, the PSA has proved a valuable parameter with a good correlation with the FFR value. This is a parameter rarely addressed in similar studies. It is important to mention that our data shows that PSA has no additive value to that of MLA to predict a FFR under 0,80.
Detailed analysis for each coronary artery shows moderate correlation of OCT derived parameters and FFR values. Although for the LAD a cut-off of 2,23 mm2 was obtained for the MLA, this value comes with a relatively low sensibility and specificity. Also, the value for the PSA in the LAD territory has a very good sensibility but a rather low specificity. In the case of RCA, the MLA is a better predictor for ischemic FFR than in the case of the LAD, with good specificity, sensibility and accuracy. For the CX artery the OCT parameters have a rather weak correlation with the FFR values.
To our knowledge, the analysis of imaging and hemodynamic data was never performed in a population of patients with acute myocardial infarction. However, the results should not be impacted by the clinical setting considering the fact that all lesions included in the analysis were performed on non culprit lesions and there are no literature data to show that FFR may be modified by acute myocardial infarction[1-3, 17-19].
5. Conclusions
The correlation between minimal luminal diameter measured by OCT and FFR in patients with acute myocardial infarction represents a significant step forward in the comprehensive evaluation of coronary artery disease in the acute setting. Integrating anatomical and physiological information provides a more holistic understanding of the severity and functional significance of coronary lesions. As technology continues to advance, refining these correlations will contribute to further improvements in CAD assessment, guiding clinicians in delivering personalized and effective patient care.
The synergy between OCT and FFR holds promise in enhancing our ability to assess and manage coronary artery disease, including patients with acute myocardial infarction, marking a pivotal advancement in the field of interventional cardiology. In conclusion, our study has showed that the use of OCT parameters can identify non-critical lesions potentially causing ischemia.
6. Study limitations
The study presents some limitations. The number of patients and lesions included in the analysis is small, so larger multicenter studies are needed. For this reason, the statistical analysis was difficult, especially since we tried to find out the significance of the OCT parameters on each coronary. The study population presented with acute myocardial infarction, therefore the results may not apply on other types of populations.
Author Contributions
Conceptualization: V.P., L.C., A.S.U. Data curation: L.C., V.P., M.B. Formal analysis: L.C., V.P., D.T.,B.A., D.A. Investigation: V.P., L.C., C.M., B.D., M.M., A.C., T.B., A.S.U. Methodology: V.P., L.C., A.S.U. Project administration: L.C., A.S.U. Resources: A.S.U. Software: D.T., A.S.U. Validation: V.P., L.C. Visualization: L.C., V.P., B.D., C.M. Writing – original draft: V.P., L.C., A.S.U. Writing – review & editing: V.P., L.C., N.P.F., D.S., A.S.U. The research leading to these results has received funding from the EEA Grants 2014-2021, under Project contract no. 33/2021
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Clinical Emergency Hospital Bucharest no. 9013/28.09.2018.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Van Nunen LX, Zimmermann FM, Tonino PAL, et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. The Lancet. 2015;386(10006):1853-1860. [CrossRef]
- De Bruyne B, Kalesan B, Barbato E, et al. Fractional Flow Reserve–Guided PCI versus Medical Therapy in Stable Coronary Disease. The New England Journal of Medicine. 2012;367(11):991-1001. [CrossRef]
- Byrne RA, Rosselló X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. European Heart Journal. 2023;44(38):3720-3826. [CrossRef]
- Shimamura K, Kubo T, Akasaka T. Evaluation of coronary plaques and atherosclerosis using optical coherence tomography. Expert Review of Cardiovascular Therapy. 2021;19(5):379-386. [CrossRef]
- Volleberg RHJA, Mol JQ, Van Der Heijden D, et al. Optical coherence tomography and coronary revascularization: from indication to procedural optimization. Trends in Cardiovascular Medicine. 2023;33(2):92-106. [CrossRef]
- Pawłowski T, Prati F, Kulawik T, Ficarra E, Bil J, Gil R. Optical coherence tomography criteria for defining functional severity of intermediate lesions: a comparative study with FFR. The International Journal of Cardiovascular Imaging. 2013;29(8):1685-1691. [CrossRef]
- Prati F, Regar E, Mintz GS, et al. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. European Heart Journal. 2009;31(4):401-415. [CrossRef]
- Tearney GJ, Regar E, Akasaka T, et al. Consensus Standards for acquisition, measurement, and reporting of intravascular Optical coherence tomography studies. Journal of the American College of Cardiology. 2012;59(12):1058-1072. [CrossRef]
- 2014 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal. 2014;35(37):2541-2619. [CrossRef]
- Ibáñez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal. 2017;39(2):119-177. [CrossRef]
- Usui E, Yonetsu T, Kanaji Y, et al. Relationship between optical coherence tomography-derived morphological criteria and functional relevance as determined by fractional flow reserve. Journal of Cardiology. 2018;71(4):359-366. [CrossRef]
- Zafar H, Ullah I, Dinneen K, et al. Evaluation of hemodynamically severe coronary stenosis as determined by fractional flow reserve with frequency domain optical coherence tomography measured anatomical parameters. Journal of Cardiology. 2014;64(1):19-24. [CrossRef]
- Paiva L, Providência R, Barra S, Dinis P, Faustino A, Gonçalves L. Universal Definition of Myocardial Infarction: Clinical insights. Cardiology. 2015;131(1):13-21. [CrossRef]
- Hachinohe D, Mitomo S, Candilio L, Latib A. A Practical Approach to Assessing Stent Results with IVUS or OCT. Methodist DeBakey Cardiovascular Journal. 2018;14(1):32. [CrossRef]
- Shiono Y, Kitabata H, Kubo T, et al. Optical coherence Tomography-Derived anatomical criteria for functionally significant coronary stenosis assessed by fractional flow reserve. Circulation Journal. 2012;76(9):2218-2225. [CrossRef]
- Ploscaru V, Popa-Fotea NM, Câlmâc L, et al. Artificial intelligence and cloud based platform for fully automated PCI guidance from coronary angiography-study protocol. PLOS ONE. 2022;17(9):e0274296. [CrossRef]
- Reith S, Battermann S, Hellmich M, Marx N, Burgmaier M. Correlation between optical coherence tomography-derived intraluminal parameters and fractional flow reserve measurements in intermediate grade coronary lesions: a comparison between diabetic and non-diabetic patients. Clinical Research in Cardiology. 2014;104(1):59-70. [CrossRef]
- Shah R. Accuracy of fractional flow reserve during acute myocardial infarction. European Heart Journal. 2020;41(27):2597. [CrossRef]
- Shah N, Al-Lamee R, Davies JE. Fractional flow reserve in acute coronary syndromes: A review. IJC Heart & Vasculature. 2014;5:20-25. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).