Submitted:
29 December 2023
Posted:
29 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
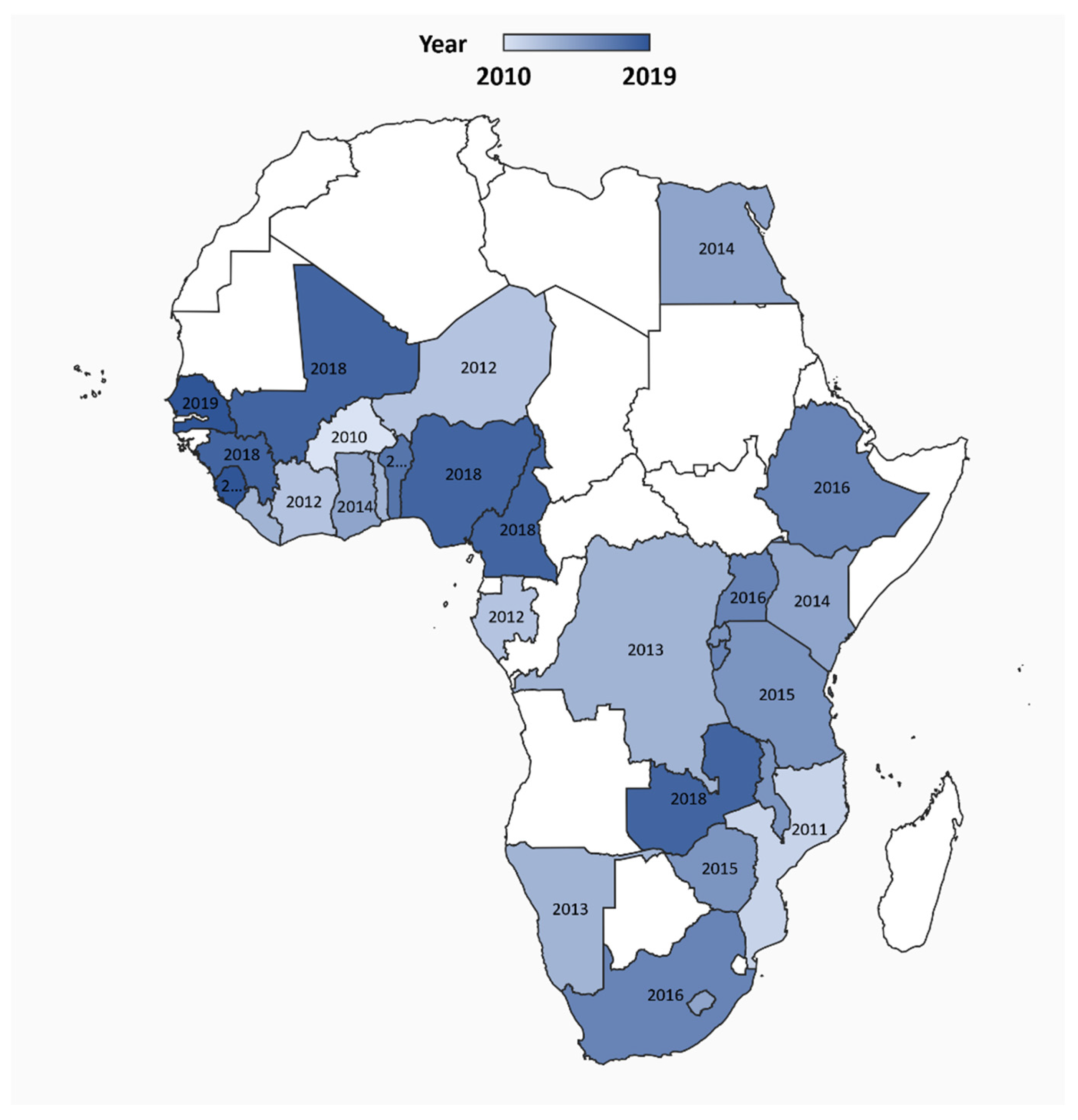
2.1. Design and setting
2.2. Country-level COVID-19 data source
2.3. Country-level health system data source, measures
2.4. Country-level social determinants of health data source, measures
2.5. Data Processing
2.6. Statistical Analysis
3. Results
3.1. Characteristics of study countries
3.2. Multivariate analysis of correlates for COVID-19 case and death rates in the 28 study countries
4. Discussion
5. Limitations
6. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Health System Measures per 10,000 population and COVID-19 Outcomes
| Country | Health System Measures per 10,000 population | COVID-19 Outcomes per 10,000 population | ||||
| Doctors | Ventilators | Hospital Beds | Cases | Deaths | ||
| Algeria | 16.86 | 0.06 | 19.0 | 8.96 | 0.31 | |
| Angola | 2.01 | 0.07 | 8.0 | 0.59 | 0.03 | |
| Benin | 0.77 | ~ | 5.0 | 1.75 | 0.03 | |
| Botswana | 4.94 | 0.65 | 18.0 | 5.27 | 0.01 | |
| Burkina Faso | 0.80 | 0.01 | 4.0 | 0.61 | 0.03 | |
| Burundi | 0.94 | 0.02 | 7.9 | 0.36 | 0.00 | |
| Cabo Verde | 7.46 | 0.91 | 21.0 | 57.52 | 0.62 | |
| Cameroon | 0.71 | 0.02 | 15.0 | 7.00 | 0.15 | |
| CAR | 0.68 | 0.01 | 10.0 | 9.80 | 0.13 | |
| Chad | 0.41 | 0.01 | 4.0 | 0.60 | 0.05 | |
| Comoros | 2.54 | ~ | 21.6 | 4.69 | 0.08 | |
| Congo | 1.34 | ~ | 16.0 | 7.12 | 0.14 | |
| Côte d'Ivoire | 2.04 | 0.03 | 4.0 | 6.61 | 0.04 | |
| Djibouti | 2.06 | 0 | 14.0 | 55.13 | 0.61 | |
| DRC | 0.67 | 0.01 | 8.0 | 1.11 | 0.03 | |
| Egypt | 4.43 | 0.04 | 14.3 | 9.60 | 0.51 | |
| Equatorial Guinea | 3.74 | 0.15 | 21.0 | 35.55 | 0.61 | |
| Eritrea | 0.61 | 0 | 7.0 | 0.81 | 0.00 | |
| Eswatini | 3.19 | 0.14 | 21 | 32.62 | 0.60 | |
| Ethiopia | 0.75 | 0.05 | 3.3 | 2.58 | 0.05 | |
| Gabon | 6.48 | 0.46 | 13.0 | 37.86 | 0.23 | |
| Gambia | 0.91 | 0.02 | 11.0 | 7.19 | 0.23 | |
| Ghana | 1.30 | 0.07 | 9.0 | 13.88 | 0.08 | |
| Guinea | 0.76 | 0.02 | 3.0 | 6.47 | 0.04 | |
| Guinea-Bissau | 1.18 | 0.00 | 10.0 | 11.02 | 0.17 | |
| Kenya | 1.53 | 0.06 | 14.0 | 5.73 | 0.09 | |
| Lesotho | 0.65 | ~ | 13.0 | 4.45 | 0.14 | |
| Liberia | 0.34 | 0.01 | 8.0 | 2.55 | 0.17 | |
| Libya | 20.30 | 0.36 | 32.0 | 11.42 | 0.21 | |
| Madagascar | 1.59 | 0.01 | 2.0 | 5.13 | 0.06 | |
| Malawi | 0.35 | 0.01 | 13.0 | 2.70 | 0.08 | |
| Mali | 1.25 | 0.03 | 1.0 | 1.33 | 0.06 | |
| Mauritania | 1.81 | 0.00 | 4.0 | 14.70 | 0.35 | |
| Mauritius | 25.36 | ~ | 34.0 | 2.72 | 0.08 | |
| Morocco | 7.13 | 0.45 | 10.0 | 11.25 | 0.17 | |
| Mozambique | 0.81 | 0.01 | 7.0 | 0.94 | 0.01 | |
| Namibia | 4.10 | 1.25 | 27.0 | 15.66 | 0.14 | |
| Niger | 0.39 | 0.01 | 3.9 | 0.50 | 0.03 | |
| Nigeria | 3.71 | 0.02 | 5.0 | 2.43 | 0.05 | |
| Rwanda | 1.31 | 0.04 | 16.0 | 1.86 | 0.01 | |
| Sao Tome/ Principe | 0.51 | ~ | 29.0 | 41.15 | 0.70 | |
| Senegal | 0.65 | 0.02 | 3.0 | 7.38 | 0.15 | |
| Seychelles | 20.79 | ~ | 36.0 | 13.01 | 0.00 | |
| Sierra Leone | 0.21 | 0.02 | 4.0 | 2.50 | 0.09 | |
| Somalia | 0.2 | 0.01 | 8.7 | 2.10 | 0.06 | |
| South Africa | 8.81 | 0.55 | 23.0 | 99.67 | 1.99 | |
| South Sudan | ~ | 0 | ~ | 2.25 | 0.04 | |
| Sudan | 2.5 | 0.07 | 7.4 | 2.88 | 0.19 | |
| Tanzania | 0.13 | ~ | 7.0 | 0.09 | 0.00 | |
| Togo | 0.76 | 0.02 | 7.0 | 1.40 | 0.03 | |
| Tunisia | 12.73 | 0.21 | 21.8 | 1.73 | 0.05 | |
| Uganda | 1.56 | 0.02 | 5.0 | 0.32 | 0.00 | |
| Zambia | 11.53 | 0.06 | 20.0 | 5.23 | 0.15 | |
| Zimbabwe | 2.07 | 0.02 | 17.0 | 3.53 | 0.09 | |
| Africa Mean | 3.79 | 0.13 | 12.58 | 10.95 | 0.18 | |
| Note: ~ denotes countries without data. CAR= Central African Republic. DRC= Democratic Republic of Congo. The most recently completed Standard DHS was used for every country except for Senegal for which Continuous DHS was used. | ||||||
References
- Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) 2020 [Available from: https://coronavirus.jhu.edu/map.html.
- Sherrard-Smith E, Hogan AB, Hamlet A, Watson OJ, Whittaker C, Winskill P, et al. The potential public health consequences of COVID-19 on malaria in Africa. Nature Medicine 2020, 26, 1411–1416. [Google Scholar] [CrossRef] [PubMed]
- Haider N, Yavlinsky A, Simons D, Osman AY, Ntoumi F, Zumla A, et al. Passengers' destinations from China: low risk of Novel Coronavirus (2019-nCoV) transmission into Africa and South America. Epidemiol Infect. 2020, 148, e41. [Google Scholar] [CrossRef] [PubMed]
- Nkengasong JN, Mankoula W. Looming threat of COVID-19 infection in Africa: act collectively, and fast. Lancet (London, England). 2020, 395, 841–842. [Google Scholar] [CrossRef]
- El-Sadr WM, Justman J. Africa in the Path of Covid-19. New England Journal of Medicine. 2020, 383, e11. [Google Scholar]
- Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boëlle PY, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020, 395, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Wallace DJ, Angus DC, Seymour CW, Barnato AE, Kahn JM. Critical care bed growth in the United States. A comparison of regional and national trends. Am J Respir Crit Care Med. 2015, 191, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020, 69, 382–386. [CrossRef] [PubMed]
- Wunsch, H. Is there a Starling curve for intensive care? Chest. 2012, 141, 1393–1399. [Google Scholar] [CrossRef] [PubMed]
- Wunsch H, Angus DC, Harrison DA, Linde-Zwirble WT, Rowan KM. Comparison of medical admissions to intensive care units in the United States and United Kingdom. Am J Respir Crit Care Med. 2011, 183, 1666–1673. [Google Scholar] [CrossRef] [PubMed]
- Moise IK, Verity JF, Kangmennaang J. Identifying youth-friendly service practices associated with adolescents' use of reproductive healthcare services in post-conflict Burundi: a cross-sectional study. Int J Health Geogr. 2017, 16, 2. [Google Scholar] [CrossRef]
- Onovo AA, Kalaiwo A, Obanubi C, Odezugo G, Estill J, Keiser O. Estimates of the COVID-19 Infection Fatality Rate for 48 African Countries: A Model-Based Analysis. BioMed [Internet]. 2021, 1, 63–79. [Google Scholar]
- Cabore JW, Karamagi HC, Kipruto HK, Mungatu JK, Asamani JA, Droti B, et al. COVID-19 in the 47 countries of the WHO African region: a modelling analysis of past trends and future patterns. Lancet Glob Health. 2022, 10, e1099–e114. [Google Scholar] [CrossRef] [PubMed]
- Wamai RG, Hirsch JL, Van Damme W, Alnwick D, Bailey RC, Hodgins S, et al. What Could Explain the Lower COVID-19 Burden in Africa despite Considerable Circulation of the SARS-CoV-2 Virus? Int J Environ Res Public Health. 2021, 18, 8638. [Google Scholar] [CrossRef] [PubMed]
- 15. Pearson CA, Van Schalkwyk C, Foss AM, O'Reilly KM, Pulliam JR. Projected early spread of COVID-19 in Africa through 1 June 2020. Euro Surveill. 1 June.
- Bradshaw D, Dorrington R, Moultrie T, Groenewald P, Moultrie H. Underestimated COVID-19 mortality in WHO African region. Lancet Glob Health. 2022, 10, e1559. [Google Scholar] [CrossRef] [PubMed]
- Ihekweazu C, Agogo E. Africa’s response to COVID-19. BMC Medicine. 2020, 18, 151. [Google Scholar]
- Ghosh J, Moise IK, Kalipeni E. Regional integration and relationship with different forms of foreign direct investments in Southern Africa. In: Munoz JM, editor. Advances in Geoeconomics. London: Routledge; 2017. p. 151-9.
- Singu S, Acharya A, Challagundla K, Byrareddy SN. Impact of Social Determinants of Health on the Emerging COVID-19 Pandemic in the United States. Frontiers in Public Health. 2020, 8, 406. [Google Scholar] [CrossRef] [PubMed]
- Moise, I. Variation in Risk of COVID-19 Infection and Predictors of Social Determinants of Health in Miami–Dade County, Florida. Preventin Chronic Diseases. 2020, 17. [Google Scholar] [CrossRef]
- 21. Rojas D, Melo A, Moise IK, Saavedra J, Szapocznik J. The Association Between the Social Determinants of Health and HIV Control in Miami-Dade County ZIP Codes, 2017. J Racial Ethn Health Disparities. 2020.
- Mwisongo A, Nabyonga-Orem J. Global health initiatives in Africa – governance, priorities, harmonisation and alignment. BMC Health Services Research. 2016, 16, 212. [Google Scholar]
- 23. Dzinamarira T, Dzobo M, Chitungo I. COVID-19: A perspective on Africa's capacity and response. J Med Virol. 2020.
- Nuwagira E, Muzoora C. Is Sub-Saharan Africa prepared for COVID-19? Trop Med Health. 2020, 48, 18. [Google Scholar] [CrossRef] [PubMed]
- Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Leach M, MacGregor H, Akello G, Babawo L, Baluku M, Desclaux A, et al. Vaccine anxieties, vaccine preparedness: Perspectives from Africa in a Covid-19 era. Soc Sci Med. 2022, 298, 114826. [Google Scholar] [CrossRef] [PubMed]
- Msellati P, Sow K, Desclaux A, Cottrell G, Diallo M, Le Hesran JY, et al. Reconsidering the COVID-19 vaccine strategy in West and Central Africa. Lancet. 2022, 400, 1304. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh MM, Erondu NA, Tomori O, Dzau VJ, Okiro EA, Maleche A, et al. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet. 2020, 395, 1735–1738. [Google Scholar] [CrossRef] [PubMed]
- MEASURE DHS. MEASURE DHS: Demographic and Health Surveys. DHS Survey Types. Calverton, MD: ICF Macro.
- Moise IK, Kangmennaang J, Halwiindi H, Grigsby-Toussaint DS, Fuller DO. Increase in Obesity Among Women of Reproductive Age in Zambia, 2002-2014. J Womens Health (Larchmt). 2019, 28, 1679–1687. [Google Scholar] [CrossRef]
- Ozodiegwu ID, Ambrose M, Battle KE, Bever C, Diallo O, Galatas B, et al. Beyond national indicators: adapting the Demographic and Health Surveys’ sampling strategies and questions to better inform subnational malaria intervention policy. Malaria Journal. 2021, 20, 122. [Google Scholar] [CrossRef] [PubMed]
- (US) NRC, (US) IoM. U.S. Health in International Perspective: Shorter Lives, Poorer Health. 2013.
- 33. Houreld K, Lewis D, McNeill R, Granados S. Virus exposes gaping holes in Africa’s health systems. Reuters Graphics, 2020.
- Maclean R, Marks S, et al. 10 African Countries Have No Ventilators. That’s Only Part of the Problem. New York Times. 2020 [Available from: https://www.nytimes.com/2020/04/18/world/africa/africa-coronavirus-ventilators.html.
- Islam, S. The human development index and per capita GDP. Applied Economics Letters. 1995, 2, 166–167. [Google Scholar] [CrossRef]
- Ghosh J, Moise IK, Kalipeni E. The role of regional integration in foreign direct investment in Southern Africa. Advances in Geoeconomics: Routledge; 2017. p. 151-9.
- Moise, IK. Geographic gender differences in traumatic unintentional injury hospitalization and youth drinking. Drug and Alcohol Dependence. 2019, 205, 107701. [Google Scholar] [CrossRef]
- Kolak M, Bhatt J, Park YH, Padrón NA, Molefe A. Quantification of Neighborhood-Level Social Determinants of Health in the Continental United States. JAMA Netw Open. 2020, 3, e1919928. [Google Scholar] [CrossRef] [PubMed]
- Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. The Lancet Public health. 2020, 5, e186–e7.
- The DHS Program. Demographic and Health Surveys: The DHS Program,; 2017 [Available from: https://dhsprogram.com/.
- Belmin C, Hoffmann R, Elkasabi M, Pichler P-P. LivWell: a sub-national Dataset on the Living Conditions of Women and their Well-being for 52 Countries. Scientific Data. 2022, 9, 719. [Google Scholar] [CrossRef] [PubMed]
- Smits J, Permanyer I. The Subnational Human Development Database. Sci Data. 2019, 6, 190038.
- Kummu M, Taka M, Guillaume JHA. Gridded global datasets for Gross Domestic Product and Human Development Index over 1990–2015. Scientific Data. 2018, 5, 180004. [Google Scholar] [CrossRef] [PubMed]
- DHS Program. Description of the Demographic and Health Surveys Individual Recode Data File. DHS II; 2008.
- The World Bank pcMsm-li, text-indent:-31.5pt, lfo1 m-lll, border:none, 31.0pt m-p-appp, mso-border-shadow:yes">. Population, total [Available from: https://data.worldbank.org/indicator/SP.POP.TOTL.
- ESRI Inc. ArcGIS Desktop: Release 10. Redlands, California: Environmental Systems Research Institute; 2010.
- IBM SPSS Statistics for Windows, Version 22.0. [Internet]. IBM Corp. 2013.
- Soko ND, Dlamini S, Ntsekhe M, Dandara C. The COVID-19 Pandemic and Explaining Outcomes in Africa: Could Genomic Variation Add to the Debate? OMICS: A Journal of Integrative Biology. 2022, 26, 594–607. [Google Scholar] [CrossRef] [PubMed]
- Rice BL, Annapragada A, Baker RE, Bruijning M, Dotse-Gborgbortsi W, Mensah K, et al. Variation in SARS-CoV-2 outbreaks across sub-Saharan Africa. Nature Medicine. 2021, 27, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Singini GC, Manda SOM. Inter-Country COVID-19 Contagiousness Variation in Eight African Countries. Front Public Health. 2022, 10, 796501. [Google Scholar] [CrossRef] [PubMed]
- Dalal J, Triulzi I, James A, Nguimbis B, Dri GG, Venkatasubramanian A, et al. COVID-19 mortality in women and men in sub-Saharan Africa: a cross-sectional study. BMJ Global Health. 2021, 6, e007225. [Google Scholar] [CrossRef] [PubMed]
- Moon Z, Zuchowski M, Moss-Morris R, Hunter MS, Norton S, Hughes LD. Disparities in access to mobile devices and e-health literacy among breast cancer survivors. Supportive Care in Cancer. 2022, 30, 117–126. [Google Scholar] [CrossRef]
- Ferrell KW, Woodard LM, Woodard TJ. Role of medication therapy management in preexposure prophylaxis therapy for HIV prevention. J Pharm Pract. 2015, 28, 10–12. [Google Scholar] [CrossRef] [PubMed]
- Friedman RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, et al. A telecommunications system for monitoring and counseling patients with hypertension. Impact on medication adherence and blood pressure control. Am J Hypertens. 1996, 9, 285–292. [Google Scholar] [CrossRef]
- Pintye J, Rogers Z, Kinuthia J, Mugwanya KK, Abuna F, Lagat H, et al. Two-Way Short Message Service (SMS) Communication May Increase Pre-Exposure Prophylaxis Continuation and Adherence Among Pregnant and Postpartum Women in Kenya. Global health, science and practice. 2020, 8, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Zhuang Z, Cao P, Zhao S, Han L, He D, Yang L. The shortage of hospital beds for COVID-19 and non-COVID-19 patients during the lockdown of Wuhan, China. Ann Transl Med. 2021, 9, 200. [Google Scholar] [CrossRef] [PubMed]
- Alavinejad M, Mellado B, Asgary A, Mbada M, Mathaha T, Lieberman B, et al. Management of hospital beds and ventilators in the Gauteng province, South Africa, during the COVID-19 pandemic. PLOS Global Public Health. 2022, 2, e0001113.
- Naidoo R, Naidoo K. Prioritising ‘already-scarce’ intensive care unit resources in the midst of COVID-19: a call for regional triage committees in South Africa. BMC Medical Ethics. 2021, 22, 28. [Google Scholar]
- Rispel LC, Marshall C, Matiwane B, Tenza IS. Innovations, contestations and fragilities of the health system response to COVID-19 in the Gauteng Province of South Africa. PLoS One. 2021, 16, e0261339. [Google Scholar]
- McQuoid-Mason, DJ. COVID-19: May hospitals in one province of South Africa reserve empty beds for patients from their province and turn down emergency requests from other provinces? S Afr Med J. 2021, 111, 304–306. [Google Scholar] [CrossRef] [PubMed]
- Moise IK, Kalipeni E, Jusrut P, Iwelunmor JI. Assessing the reduction in infant mortality rates in Malawi over the 1990–2010 decades. Global Public Health. 2017, 12, 757–779. [Google Scholar] [CrossRef] [PubMed]
- Bicego GT, Boerma JT. Maternal education and child survival: a comparative study of survey data from 17 countries. Social science & medicine. 1993, 36, 1207–1227. [Google Scholar]
- Dallolio L, Di Gregori V, Lenzi J, Franchino G, Calugi S, Domenighetti G, et al. Socio-economic factors associated with infant mortality in Italy: an ecological study. Int J Equity Health. 2012, 11, 45. [Google Scholar] [CrossRef]
- Kalipeni, E. Determinants of infant mortality in Malawi: a spatial perspective. Soc Sci Med. 1993, 37, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Flor LS, Friedman J, Spencer CN, Cagney J, Arrieta A, Herbert ME, et al. Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: a comprehensive review of data from March, 2020, to September, 2021. Lancet. 2022, 399, 2381–2397. [Google Scholar] [CrossRef] [PubMed]
- 66. Heo MH, Kwon YD, Cheon J, Kim KB, Noh JW. Association between the Human Development Index and Confirmed COVID-19 Cases by Country. Healthcare (Basel). 2020; 10.
- Faramarzi A, Javan-Noughabi J, Mousavi SA, Bahrami Asl F, Shabanikiya H. Socioeconomic status and COVID-19-related cases and fatalities in the world: A cross-sectional ecological study. Health Science Reports. 2022, 5, e628.
- Desmon, S. COVID-19 Prevention When There’s No Soap and Water 2020 [Available from: https://ccp.jhu.edu/2020/04/13/handwashing-covid-19-no-soap-water/.
- Amegah, AK. Improving handwashing habits and household air quality in Africa after COVID-19. Lancet Glob Health. 2020, 8, e1110–e1. [Google Scholar] [CrossRef] [PubMed]
- Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004, 15, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Cole SR, Platt RW, Schisterman EF, Chu H, Westreich D, Richardson D, et al. Illustrating bias due to conditioning on a collider. International Journal of Epidemiology. 2009, 39, 417–420. [Google Scholar]

| Social Determinants of Health Measures | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Residency (% households) | Wealth Index (% households) | Educational Status (% head of households) | Sanitation (% households) | Overcrowding (% households) | ||||||
| n | Rural | Urban | Poor | Average | No education | Primary | Secondary or higher | Place to wash hands | Soap or detergent present | >3 people per sleeping room | |
| Benin | 14423 | 55 | 45 | 36.9 | 18.9 | 51.8 | 22.2 | 24.5 | 55.5 | 20.4 | 22.5 |
| Burkina Faso | 14156 | 69.4 | 30.6 | 37.3 | 19.3 | 76.1 | 13 | 10.9 | 80.9 | 17.4 | 18.6 |
| Burundi | 15977 | 81.2 | 18.8 | 41.3 | 18.1 | 47.2 | 39.7 | 13.1 | 98.5 | 7.5 | 13.7 |
| Cameroon | 17223 | 44.8 | 55.2 | 33.2 | 22.5 | 19.4 | 32.9 | 46 | 95.2 | 46.4 | 15.7 |
| Côte d’Ivoire | 4466 | 58.6 | 41.4 | 42.6 | 21.8 | 57.4 | 20.3 | 22.1 | 84.8 | 28.7 | 24.1 |
| DR Congo | 18171 | 70.1 | 29.9 | 49.3 | 19.6 | 14.7 | 32.5 | 52.8 | 92.6 | 37.3 | 28.2 |
| Egypt | 28175 | 50.4 | 49.6 | 34.4 | 16.7 | 25.3 | 15.6 | 59.1 | 97 | 90.8 | 8.4 |
| Ethiopia | 16650 | 68.6 | 31.4 | 42.2 | 12.4 | 52.1 | 28 | 19.6 | 54.3 | 24.3 | 45.6 |
| Gambia | 11835 | 50.2 | 49.8 | 45.7 | 15.1 | 67.1 | 7.4 | 25.3 | 98.9 | 66.9 | 21.3 |
| Ghana | 6215 | 49.8 | 50.2 | 41.7 | 21.8 | 28.3 | 14.1 | 57.6 | 90.2 | 40.2 | 20.2 |
| Guinea | 7912 | 65.9 | 34.1 | 42.2 | 18.8 | 68.4 | 9.8 | 21.3 | 70.2 | 34 | 21.2 |
| Kenya | 36430 | 61.8 | 38.2 | 44.2 | 18.8 | 20.9 | 45.6 | 33.5 | 62.4 | 44.5 | 28.2 |
| Lesotho | 9333 | 70.2 | 29.8 | 42.6 | 19.9 | 17.3 | 53.1 | 27.8 | 7.5 | 47.2 | 15.5 |
| Liberia | 9402 | 63 | 37 | 58.4 | 19.7 | 38.3 | 21.3 | 40.4 | 26.3 | 38.3 | 25.6 |
| Malawi | 9510 | 81.1 | 18.9 | 39 | 19.1 | 15.8 | 56.1 | 27.5 | 84.2 | 14.7 | 19.4 |
| Mali | 26361 | 69 | 31 | 38.3 | 19.6 | 69.4 | 12.8 | 17 | 74 | 24.9 | 21.2 |
| Mozambique | 13919 | 63.4 | 36.6 | 33.7 | 20.2 | 29.6 | 50.9 | 17.5 | 98.6 | 39.1 | 18.9 |
| Namibia | 9840 | 51.6 | 48.4 | 37 | 20.4 | 17.6 | 28.3 | 53.7 | 94.6 | 60.1 | 13 |
| Nigeria | 40427 | 58.5 | 41.5 | 37.4 | 22.1 | 30.7 | 21.2 | 48 | 79.3 | 36.4 | 20.8 |
| Rwanda | 12699 | 77.2 | 22.8 | 42.5 | 18.4 | 25.5 | 60.9 | 13.6 | 76.6 | 54.1 | 11.4 |
| Senegal | 12598 | 62.1 | 37.9 | 52 | 20.1 | 70.6 | 14.2 | 13.4 | 39 | 56.4 | 20.2 |
| Sierra Leone | 4592 | 63.8 | 36.2 | 39.7 | 18.3 | 66 | 9.4 | 24.5 | 89 | 35.8 | 23.7 |
| South Africa | 9548 | 40.8 | 59.2 | 42.8 | 21.3 | 13.4 | 21.1 | 64 | 87.2 | 48.9 | 8.7 |
| Tanzania | 12561 | 71.1 | 28.9 | 34.1 | 20.4 | 20.8 | 60.4 | 18.7 | 77.2 | 59.5 | 17.6 |
| Togo | 19588 | 61.9 | 38.1 | 37.1 | 22.4 | 35.4 | 27.8 | 36.8 | 80.4 | 63.5 | 21.9 |
| Uganda | 11083 | 77.2 | 22.8 | 43.3 | 18.4 | 16.3 | 52 | 30.5 | 57.6 | 45.8 | 26.6 |
| Zambia | 12831 | 63.3 | 36.7 | 44.6 | 20.4 | 9.7 | 42.7 | 45.7 | 52.4 | 40.5 | 25.1 |
| Zimbabwe | 10534 | 58.8 | 41.2 | 32.9 | 16.8 | 6.6 | 31.4 | 61.1 | 97.4 | 45.6 | 15.4 |
| Coefficient | Std. Error | P-value | Odds Ratio 95% Wald CI |
|
|---|---|---|---|---|
| Social Determinants of Health (SDoH) measures | ||||
| Geography | ||||
| Population living in urban areas (%) | -0.042 | 0.048 | 0.384 | 0.959 (0.874 - 1.053) |
| Wealth | ||||
| Human Development Index | -2.387 | 6.525 | 0.715 | 0.092 (0.000 - 32,925.611) |
| Education | ||||
| Women education (%) | 0.089 | 0.054 | 0.102 | 1.093 (0.982 - 1.215) |
| Sanitation | ||||
| Households, quality water access, %) | 0.143 | 0.055 | 0.009 | 1.153 (1.036 - 1.284) |
| Employment | ||||
| Women currently working (%) | -0.041 | 0.046 | 0.379 | 0.96 (0.877 - 1.051) |
| Healthcare access | ||||
| Not having health insurance (%), | 0.232 | 0.059 | 0.001 | 1.262 (1.124 - 1.417) |
| Crowding | ||||
| Average number of householders (> than 3) | -1.735 | 1.069 | 0.105 | 0.176 (0.022 - 1.433) |
| Access to Information | ||||
| Women, mobile phone (%) | 0.089 | 0.046 | 0.053 | 1.093 (0.999 - 1.195) |
| Women listening to the radio at least once a week (%) | 0.061 | 0.057 | 0.284 | 1.063 (0.951 - 1.188) |
| Healthcare System Measures | 0.462 | |||
| Doctor rates per 10,000 population | 1.792 | 4.732 | 0.000 | 5.999 (2.427 - 14.832) |
| Ventilator rates per 10,000 population | 9.086 | 0.314 | 0.055 | 8,826.966 (0.827 - 941,768) |
| Hospital bed rates per 10,000 population | 0.072 | 0.048 | 0.820 | 1.074 (0.58 - 1.988) |
| Coefficient | Std. Error | P-value | Odds Ratio 95% Wald CI |
|
|---|---|---|---|---|
| Social Determinants of Health (SDoH) measures | ||||
| Geography | ||||
| Population living in urban areas (%) | -0.001 | 0.0010 | 0.166 | 0.999 (0.997 – 1.001 |
| Wealth | ||||
| Human Development Index | -0.182 | 0.1309 | 0.165 | 0.834 (0.645 – 1.078) |
| Education | ||||
| Women education (%) | 0.003 | 0.0011 | 0.014 | 1.003 (1.001 – 1.005) |
| Sanitation | ||||
| Households with high quality water access, %) | 0.004 | 0.0011 | 0.001 | 1.004 (1.002 – 1.006) |
| Employment | ||||
| Women currently working (%) | -0.001 | 0.0009 | 0.247 | 0.999 (0.997 – 1.001) |
| Healthcare Access | ||||
| Insurance coverage (%), | 0.001 | 0.0012 | 0.370 | 1.001 (0.999 – 1.003) |
| Crowding | ||||
| Average number of householders (> than 3) | -0.042 | 0.0214 | 0.051 | 0.959 (0.920 – 1.000) |
| Access to Information | ||||
| Women owning a mobile phone (%) | 0.001 | 0.0009 | 0.181 | 1.001 (0.999 – 1.003) |
| Women listening to the radio at least once a week (%) | 0.002 | 0.0011 | 0.058 | 1.002 (1.000 – 1.004) |
| Healthcare System Measures | ||||
| Doctor rates per 10,000 population | 0.025 | 0.0093 | 0.007 | 1.025 (1.007 – 1.004) |
| Ventilator rates per 10,000 population | -0.107 | 0.0949 | 0.258 | 0.898 (0.746 – 1.082) |
| Hospital bed rates per 10,000 population | 0.013 | 0.0063 | 0.044 | 1.013 (1.000 – 1.025) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





