Submitted:
29 November 2023
Posted:
30 November 2023
You are already at the latest version
Abstract
Keywords:
INTRODUCTION
METHODS
Study population
Echocardiography and cardiac staging
TAVI procedure and ECG assessment
Statistical analysis
RESULTS
Baseline characteristics of the study population
Staging and ECG outcomes after TAVI
Predictors of PPMI and in-hospital mortality
DISCUSSION
Cardiac damage and post-TAVI conduction disorders
Limitations
Conclusion
Conflicts of Interest
References
- Rosseel, L.; Mylotte, D.; Cosyns, B.; Vanhaverbeke, M.; Zweiker, D.; Teles, R.C.; Angerås, O.; Neylon, A.; Rudolph, T.K.; Wykrzykowska, J.J.; et al. Contemporary European practice in transcatheter aortic valve implantation: results from the 2022 European TAVI Pathway Registry. Front. Cardiovasc. Med. 2023, 10, 1227217. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2021, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Karyofillis, P.; Kostopoulou, A.; Thomopoulou, S.; Habibi, M.; Livanis, E.; Karavolias, G.; Voudris, V. Conduction abnormalities after transcatheter aortic valve implantation. J. Geriatr. Cardiol. 2018, 15, 105–112. [Google Scholar] [CrossRef]
- Auffret, V.; Puri, R.; Urena, M.; Chamandi, C.; Rodriguez-Gabella, T.; Philippon, F.; Rodés-Cabau, J. Conduction Disturbances After Transcatheter Aortic Valve Replacement. Circ. 2017, 136, 1049–1069. [Google Scholar] [CrossRef]
- Mangieri, A.; Montalto, C.; Pagnesi, M.; Lanzillo, G.; Demir, O.; Testa, L.; Colombo, A.; Latib, A. TAVI and Post Procedural Cardiac Conduction Abnormalities. Front. Cardiovasc. Med. 2018, 5, 85. [Google Scholar] [CrossRef] [PubMed]
- Scarsini, R.; De Maria, G.L.; Joseph, J.; Fan, L.; Cahill, T.J.; Kotronias, R.A.; Burzotta, F.; Newton, J.D.; Kharbanda, R.; Prendergast, B.; et al. Impact of Complications During Transfemoral Transcatheter Aortic Valve Replacement: How Can They Be Avoided and Managed? J. Am. Hear. Assoc. 2019, 8, e013801. [Google Scholar] [CrossRef] [PubMed]
- Sammour, Y.; Krishnaswamy, A.; Kumar, A.; Puri, R.; Tarakji, K.G.; Bazarbashi, N.; Harb, S.; Griffin, B.; Svensson, L.; Wazni, O.; et al. Incidence, Predictors, and Implications of Permanent Pacemaker Requirement After Transcatheter Aortic Valve Replacement. JACC: Cardiovasc. Interv. 2021, 14, 115–134. [Google Scholar] [CrossRef]
- Auffret, V.; Webb, J.G.; Eltchaninoff, H.; Muñoz-García, A.J.; Himbert, D.; Tamburino, C.; Nombela-Franco, L.; Nietlispach, F.; Morís, C.; Ruel, M.; et al. Clinical Impact of Baseline Right Bundle Branch Block in Patients Undergoing Transcatheter Aortic Valve Replacement. JACC: Cardiovasc. Interv. 2017, 10, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- van Rosendael, P.J.; Delgado, V.; Bax, J.J. Pacemaker implantation rate after transcatheter aortic valve implantation with early and new-generation devices: a systematic review. Eur. Hear. J. 2018, 39, 2003–2013. [Google Scholar] [CrossRef]
- Lenders, G.D.; Collas, V.; Hernandez, J.M.; Legrand, V.; Danenberg, H.D.; Heijer, P.D.; Rodrigus, I.E.; Paelinck, B.P.; Vrints, C.J.; Bosmans, J.M. Depth of valve implantation, conduction disturbances and pacemaker implantation with CoreValve and CoreValve Accutrak system for Transcatheter Aortic Valve Implantation, a multi-center study. Int. J. Cardiol. 2014, 176, 771–775. [Google Scholar] [CrossRef]
- Prihadi, E.A.; Leung, M.; Vollema, E.M.; Ng, A.C.; Marsan, N.A.; Bax, J.J.; Delgado, V. Prevalence and Prognostic Relevance of Ventricular Conduction Disturbances in Patients With Aortic Stenosis. Am. J. Cardiol. 2017, 120, 2226–2232. [Google Scholar] [CrossRef] [PubMed]
- Sebag, F.A.; Lellouche, N.; Chaachoui, N.; Dubois-Rande, J.; Gueret, P.; Monin, J. Prevalence and clinical impact of QRS duration in patients with low-flow/low-gradient aortic stenosis due to left ventricular systolic dysfunction. Eur. J. Hear. Fail. 2014, 16, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, R.C.; Amat-Y-Leon, F.; Pietras, R.J.; Wyndham, C.; Deedwania, P.C.; Wu, D.; Denes, P.; Rosen, K.M. Sites of Conduction Disease in Aortic Stenosis. Ann. Intern. Med. 1977, 87, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Généreux, P.; Pibarot, P.; Redfors, B.; Mack, M.J.; Makkar, R.R.; A Jaber, W.; Svensson, L.G.; Kapadia, S.; Tuzcu, E.M.; Thourani, V.H.; et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur. Hear. J. 2017, 38, 3351–3358. [Google Scholar] [CrossRef] [PubMed]
- Tastet, L.; Tribouilloy, C.; Maréchaux, S.; Vollema, E.M.; Delgado, V.; Salaun, E.; Shen, M.; Capoulade, R.; Clavel, M.-A.; Arsenault, M.; et al. Staging Cardiac Damage in Patients With Asymptomatic Aortic Valve Stenosis. J. Am. Coll. Cardiol. 2019, 74, 550–563. [Google Scholar] [CrossRef]
- Viva, T.; Postolache, A.; Trung, M.-L.N.; Danthine, P.; Petitjean, H.; Bruno, V.D.; Martinez, C.; Lempereur, M.; Guazzi, M.; Aghezzaf, S.; et al. A new integrative approach combining right heart catheterization and echocardiography to stage aortic stenosis-related cardiac damage. Front. Cardiovasc. Med. 2023, 10, 1184308. [Google Scholar] [CrossRef] [PubMed]
- Faroux, L.; Chen, S.; Muntané-Carol, G.; Regueiro, A.; Philippon, F.; Sondergaard, L.; Jørgensen, T.H.; Lopez-Aguilera, J.; Kodali, S.; Leon, M.; et al. Clinical impact of conduction disturbances in transcatheter aortic valve replacement recipients: a systematic review and meta-analysis. Eur. Hear. J. 2020, 41, 2771–2781. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Ko, Y.-G.; Shim, C.Y.; Ryu, J.; Lee, Y.-J.; Seo, J.; Lee, S.-J.; Cho, I.; Hong, S.-J.; Ahn, C.-M.; et al. Impact of New-Onset Persistent Left Bundle Branch Block on Reverse Cardiac Remodeling and Clinical Outcomes After Transcatheter Aortic Valve Replacement. Front. Cardiovasc. Med. 2022, 9, 893878. [Google Scholar] [CrossRef]
- Jørgensen, T.H.; De Backer, O.; Gerds, T.A.; Bieliauskas, G.; Svendsen, J.H.; Søndergaard, L. Mortality and Heart Failure Hospitalization in Patients With Conduction Abnormalities After Transcatheter Aortic Valve Replacement. JACC: Cardiovasc. Interv. 2019, 12, 52–61. [Google Scholar] [CrossRef]
- Wang, B.; Mei, Z.; Ge, X.; Li, Y.; Zhou, Q.; Meng, X.; An, G. Comparison of outcomes of self-expanding versus balloon-expandable valves for transcatheter aortic valve replacement: a meta-analysis of randomized and propensity-matched studies. BMC Cardiovasc. Disord. 2023, 23, 1–18. [Google Scholar] [CrossRef]
- Smith, C.R.; Leon, M.B.; Mack, M.J.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. N. Engl. J. Med. 2011, 364, 2187–2198. [Google Scholar] [CrossRef] [PubMed]
- Aladham, A.; Gada, H.; Wang, Y.; Mumtaz, M.; Sultan, I.; Mulukutla, S.; Vora, A.N. Incidence of Permanent Pacemaker Implantation Using the Cusp Overlap Technique. JACC: Cardiovasc. Interv. 2022, 15, 1006–1008. [Google Scholar] [CrossRef] [PubMed]
- Szotek, M.; Drużbicki; Sabatowski, K.; Amoroso, G.R.; De Schouwer, K.; Matusik, P.T. Transcatheter Aortic Valve Implantation and Cardiac Conduction Abnormalities: Prevalence, Risk Factors and Management. J. Clin. Med. 2023, 12, 6056. [Google Scholar] [CrossRef] [PubMed]
- Regueiro, A.; Altisent, O.A.-J.; Del Trigo, M.; Campelo-Parada, F.; Puri, R.; Urena, M.; Philippon, F.; Rodés-Cabau, J. Impact of New-Onset Left Bundle Branch Block and Periprocedural Permanent Pacemaker Implantation on Clinical Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement. Circ. Cardiovasc. Interv. 2016, 9, e003635. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, S.; Han, X.; Chen, Y.; Chen, H.; Wan, Z.; Song, B. Prognostic Outcome of New-Onset Left Bundle Branch Block After Transcatheter Aortic Valve Replacement in Patients With Aortic Stenosis: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 842929. [Google Scholar] [CrossRef] [PubMed]
- Chamandi, C.; Barbanti, M.; Munoz-Garcia, A.; Latib, A.; Nombela-Franco, L.; Gutiérrez-Ibanez, E.; Veiga-Fernandez, G.; Cheema, A.N.; Cruz-Gonzalez, I.; Serra, V.; et al. Long-Term Outcomes in Patients With New-Onset Persistent Left Bundle Branch Block Following TAVR. JACC: Cardiovasc. Interv. 2019, 12, 1175–1184. [Google Scholar] [CrossRef] [PubMed]
- Avvedimento, M.; Franzone, A.; Leone, A.; Piccolo, R.; Castiello, D.S.; Ilardi, F.; Mariani, A.; Esposito, R.; Iapicca, C.; Angellotti, D.; et al. Extent of Cardiac Damage and Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation. J. Clin. Med. 2021, 10, 4563. [Google Scholar] [CrossRef]
- Mills, R.W.; Wright, A.T.; Narayan, S.M.; McCulloch, A.D. The effects of wall stretch on ventricular conduction and refractoriness in the whole heart. In Cardiac Mechano-Electric Coupling and Arrhythmias; Kohl, P., Sachs, F., Franz, M.R., Eds.; Oxford University Press: Oxford, UK, 2011; p. 0. [Google Scholar] [CrossRef]
| Total | Group 1 | Group 2 | Group 3 | p-value | |
|---|---|---|---|---|---|
| Clinical characteristics | |||||
| Number of patients (%) | 119 (100%) | 16 (13.5%) | 70 (58.8%) | 33 (27.7%) | |
| Age (years) | 84 (79 - 86) | 78 (73,5 – 84,5) | 83,5 (79 – 87) | 85 (81 – 87) | 0.017 |
| Male, (%) | 64 (53.78) | 9 (56.3) | 37 (52.9) | 18 (54.6) | 0.97 |
| Body mass index, Kg/m2 | 25.51 (23.2 – 29.6) | 27.1 (23.3-29.5) | 26.4 (23.1-30.1) | 24.9 (23.5-26.9) | 0.58 |
| Current smoker (%) | 45 (37.8) | 8 (50) | 26 (37.1) | 11 (33.3) | 0.30 |
| Hypertension n (%) | 106 (89.1) | 14 (87.5) | 62 (88.6) | 30 (90.9) | 0.82 |
| Diabetes (%) | 35 (29.4) | 6 (37.5) | 20 (28.6) | 9 (27.3) | 0.52 |
| Dyslipidemia (%) | 96 (80.7) | 14 (87.5) | 55 (78.6) | 27 (81.8) | 0.86 |
| Atrial fibrillation (%) | 48 (40.3) | 3 (18.8) | 25 (35.7) | 20 (60.6) | 0.003 |
| Stroke (%) | 22 (18.5) | 0 (0) | 15 (21.4) | 7 (21.2) | 0.19 |
| Prior peripheral vascular disease (%) | 59 (49.6) | 7 (43.8) | 37 (52.9) | 15 (45.5) | 0.90 |
| Coronary artery disease (%) | 53 (44.5) | 8 (50) | 29 (41.4) | 16 (48.5) | 0.89 |
| Chronic kidney diseases (eGFR <45 mL/min) | 50 (42.0) | 5 (31.3) | 29 (41.4) | 16 (48.5) | 0.25 |
| Medical therapy | |||||
| Beta-blockers (%) | 84 (70.6) | 9 (56.3) | 49 (70) | 26 (78.8) | 0.11 |
| Calcium antagonists (%) | 28 (23.5) | 4 (25) | 16 (22.9) | 8 (24.2) | 1.00 |
| Amiodarone (%) | 21 (17.7) | 2 (12.5) | 12 (17.1) | 7 (21.2) | 0.57 |
| Procedure | |||||
| Euroscore II (%) | 3.98 (2.51 – 6.02) | 3.92 (2.8-4.9) | 3.64 (2.35-6.06) | 4.8 (2.8-11.27) | 0.24 |
| Calcium score | 2471.45 (1652 - 3768) | 1582 (869-3197) | 2990 (1853-4111) | 2211 (1855-3117) | 0.10 |
| Pre-dilatation (%) | 38 (31.9) | 3 (18.8) | 23 (32.9) | 12 (36.4) | 0.28 |
| Post-dilatation (%) | 15 (12.6) | 1 (6.3) | 12 (17.1) | 2 (6.1) | 0.66 |
| Prosthesis size | 0.55 | ||||
| 23 mm (%) | 8 (6.72) | 0 (0) | 4 (5.7) | 4 (12.1) | |
| 26 mm (%) | 33 (27.7) | 5 (31.3) | 19 (27.1) | 9 (27.3) | |
| 29 mm (%) | 45 (37.8) | 7 (43.8) | 27 (38.6) | 11 (33.3) | |
| 34 mm (%) | 33 (27.7) | 4 (25) | 20 (28.6) | 9 (27.3) | |
| Approach (%) | 0.32 | ||||
| Femoral | 103 (86.6) | 14 (87.5) | 60 (85.7) | (87.9) | |
| Trans-Axillary | 15 (12.6) | 2 (12.5) | 10 (14.3) | (9.1) | |
| Carotid | 1 (0.84) | 0 (0) | 0 (0) | 1 (3) | |
| General anesthesia (%) | 0.42 | ||||
| General | 80 (67.2) | 7 (43.8) | 52 (74.3) | 21 (63.6) | |
| Local anesthesia + sedation | 39 (32.8) | 9 (56.3) | 18 (25.7) | 12 (36.4) | |
| Procedure time(min) | 122 (101 - 140) | 123.5 (102.5-132.5) | 123 (102-140) | 115 (99-147) | 0.84 |
| Electrocardiogram | |||||
| Heart rate (bpm) | 71 (62 – 81) | 73.5 (65-85) | 69 (60-80) | 72 (62-81) | 0.59 |
| Rhythm | < 0.0001 | ||||
| Sinus (%) | 94 (78.99) | 16 (100) | 61 (87.1) | 17 (51.5) | |
| Atrial fibrillation (%) | 25 (21.01) | 0 (0) | 9 (12.9) | 16 (48.5) | |
| PR interval (ms) | 180 (164 – 204) | 165 (161-177) | 180 (164-204) | 202 (180-214) | 0.020 |
| < 200 ms (%) | 63 (67.0) | 15 (93.8) | 40 (57.1) | 8 (24.2) | |
| 200-239 ms (%) | 20 (21.3) | 1 (6.3) | 13 (18.6) | (18.2) | |
| ≥ 240 ms (%) | 11 (11.70) | 0 (0) | 8 (11.4) | 3 (9.1) | |
| QRS (ms) | 96 (84 – 112) | 89 (78-98) | 96 (86-119) | 94 (84-110) | 0.13 |
| < 120 ms (%) | 96 (80.7) | 14 (87.5) | 54 (77.1) | 28 (84.9) | |
| 120-149 ms (%) | 17 (14.3) | 2 (12.5) | 10 (14.3) | (15.1) | |
| ≥ 150 ms (%) | 6 (5.04) | 0 (0) | 6 (8.6) | 0 (0) | |
| Prior bundle branch block | 0.47 | ||||
| Left (%) | 10 (8.4) | 1 (6.3) | 7 (10) | 2 (6.1) | |
| Right (%) | 6 (5.04) | 1 (6.3) | 5 (7.1) | 0 (0) |
| Total | Group 1 N=16 (13.5%) |
Group 2 N=70 (58.8%) |
Group 3 N=33 (27.7%) |
p value | |
|---|---|---|---|---|---|
| Electrocardiogram | |||||
| Heart rate (bpm) | 73 (65 – 86) | 72 (61-95) | 72 (65-81) | 79 (67.5-88.5) | 0.41 |
| Rhythm | |||||
| Atrial fibrillation (%) | 25 (21.7) | 0 (0) | 9 (12.9) | 16 (48.5) | < 0.0001 |
| PR interval (ms) | 190 (166 – 214) | 170 (162-194) | 192 (172-215) | 214 (168-226) | 0.052 |
| < 200 ms (%) | 55 (63.2) | 13 (81.3) | 36 (51.4) | (18.2) | |
| 200-239 ms (%) | 19 (21.8) | 2 (12.5) | 11 (15.7) | (18.2) | |
| ≥ 240 ms (%) | 13 (14.9) | 1 (6.3) | 9 (12.9) | 3 (9.1) | |
| Delta PR | 8 (-6 - 20) | 4 (-3 – 23)* | 8 (-6 – 18)* | 2 (-22 – 26) | 0.71 |
| QRS (ms) | 122 (96 – 140) | 101 (88-129) | 122 (94- 140) | 124.5 (103-142) | 0.13 |
| < 120 ms (%) | 54 (47.4) | 10 (62.5) | 30 (42.9) | 14 (42.4) | |
| 120-149 ms (%) | 42 (36.8) | 6 (37.5) | 23 (32.9) | 13 (39.4) | |
| ≥ 150 ms (%) | 18 (15.8) | 0 (0) | 13 (18.6) | 5 (15.2) | |
| Delta QRS | 8 (2-36) | 11 (6 – 24)* | 5 (0 – 33)* | 19 (4 – 54)* | 0.082 |
| New bundle branch block | 0.17 | ||||
| Left (%) | 41 (34.5) | 4 (25) | 24 (34.3) | (39.4) | |
| Right (%) | 3 (2.52) | 0 (0) | 1 (1.4) | 2 (6.1) | |
| Complications | |||||
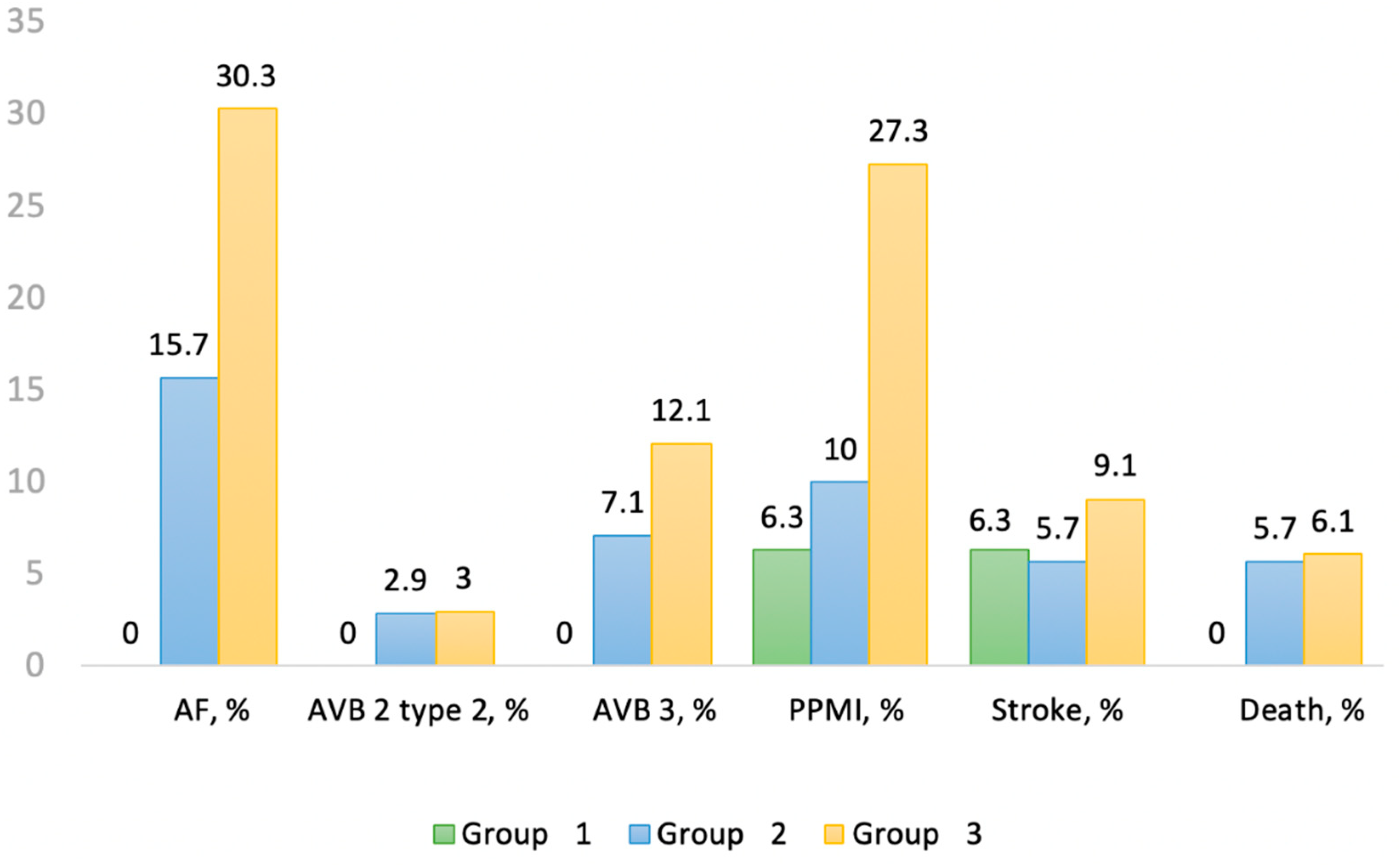
| Paroxysmal atrial fibrillation (%) | 21 (17.7) | 0 (0) | 11 (15.7) | 10 (30.3) | 0.012 |
| High degree AV block (%) | 12 (10) | 0 (0) | 7 (10) | 5 (15) | 0.38 |
| Permanent pacemaker implantation (%) | 17 (14.3) | 1 (6.3) | 7 (10) | 9 (27.3) | 0.022 |
| Stroke (%) | 8 (6.7) | 1 (6.3) | 4 (5.7) | 3 (9.1) | 0.32 |
| Death (%) | 6 (5) | 0 (0) | 4 (5.7) | 2 (6.1) | 0.52 |
| Variables | HR (LCL – UCL) | p-value | Units |
|---|---|---|---|
| Local vs general anesthesia | 2.77 (1.11 – 6.89) | 0.028 | |
| Heart rate ECG pre-TAVI | 0.96 (0.93 – 1) | 0.047 | 1 beat |
| Duration QRS ECG pre-TAVI | 1.16 (1 – 1.34) | 0.051 | 10 ms |
| PR pre-TAVI 200-239 ms vs < 200 ms | 3.35 (0.97 – 11.59) | 0.056 | |
| Per-procedure: AV block 2 type 2 vs No AV block | 142.6 (8.71 – 2333.5) | 0.0005 | |
| Per-procedure: AV block 3 vs No AV block | 6.2 (2.19 – 17.54) | 0.0006 | |
| Prosthesis size 34 vs 29 | 5.27 (1.45 – 19.17) | 0.012 | |
| Atrial fibrillation | 2.95 (1.16 – 7.51) | 0.023 | |
| Heart rate ECG post-TAVI | 0.97 (0.94 – 1) | 0.082 | 1 beat |
| Interval PR ECG post-TAVI | 1.20 (1.06 – 1.36) | 0.004 | 10 ms |
| Delta PR | 1.02 (1 – 1.04) | 0.11 | 1 ms |
| Duration QRS ECG post-TAVI | 1.55 (1.26 – 1.91) | <0.0001 | 10 ms |
| Delta QRS | 1.03 (1.01 – 1.05) | 0.001 | 1 ms |
| ECG post-TAVI: left bundle-branch block vs No bundle-branch block | 5.76 (1.62 – 20.44) | 0.007 | |
| ECG post-TAVI: right bundle-branch block vs No bundle-branch block | 7.15 (1.44 – 35.49) | 0.016 | |
| PR post-TAVI < 200 ms vs ≥ 240 ms | 0.13 (0.02 – 0.79) | 0.027 | |
| PR post-TAVI 200-239 ms vs < 200 ms | 6.59 (1.2 – 35.99) | 0.030 | |
| QRS post-TAVI ≥ 150 ms vs < 120 ms | 16.97 (4.55 – 63.29) | <0.0001 | |
| QRS post-TAVI 120-149 ms vs ≥ 150 ms | 0.17 (0.06 – 0.48) | 0.0009 | |
| Post-TAVI: AV block 3 vs No AV block | 9.95 (3.67 – 26.92) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





