1. Introduction
In the contemporary digital landscape, the convergence of technology and social behavior has led to a paradigm shift in the way individuals interact with information, ideas, and even their own self-perceptions [
1]. With the proliferation of social media platforms, the dynamics of self-image, dietary behaviors, and mental health have undergone profound transformations [
2], often with significant consequences [
3]. The pervasiveness of digital media has engendered a culture of constant comparison and idealized representations, fueling unrealistic standards of beauty and well-being [
4]. Instagram, as one of the most influential and visually oriented social platforms, has emerged as a prominent catalyst in shaping societal perceptions of body image and dietary norms [
5]. The ceaseless stream of meticulously curated content, portraying unattainable standards of physical perfection and dietary regimens, has been linked to the exacerbation of body dissatisfaction, fostering a climate conducive to the development of various eating disorders [
6].
Eating disorders represent a complex array of psychological conditions characterized by disturbances in individuals' eating behaviors and perceptions of body image [
7]. These disorders often manifest as a result of intricate interactions between genetic predispositions, environmental influences, societal pressures, and psychological factors [
8]. Beyond well-documented eating disorders, such as anorexia nervosa, bulimia nervosa and binge eating disorder, emerging concepts such as Orthorexia Nervosa have garnered increasing attention [
9]. Orthorexia Nervosa, while not formally recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), revolves around an obsession with consuming only foods perceived as healthy, pure, or "clean." This obsession often leads individuals to adhere to stringent dietary rules, culminating in severe nutritional deficiencies and social isolation due to the avoidance of situations that may compromise their dietary regimen [
10]. Moreover, the rigid dietary restrictions characteristic of Orthorexia Nervosa is often fueled by a profound desire for control, order, and a distorted sense of achievement associated with adhering to self-imposed dietary guidelines [
11]. The nuanced nature of Orthorexia Nervosa necessitates a comprehensive understanding of the underlying psychological and sociocultural factors driving to the development and perpetuation of this atypical eating disorder [
12].
The pervasive impact of eating disorders, such as orthorexia nervosa, extends beyond the realm of disordered eating behaviors, encompassing profound psychological distress often associated with co-occurring conditions such as depression, anxiety, and stress [
13]. Individuals grappling with these disorders commonly experience a profound sense of hopelessness, low self-worth, and persistent sadness, often resulting from the emotional turmoil arising from their distorted perceptions of body image and self-worth [
14]. The chronic cycle of stringent dietary regulations and obsessive thoughts about food quality in Orthorexia Nervosa further exacerbates the existing psychological vulnerabilities, contributing to heightened levels of anxiety and stress in response to perceived deviations from self-imposed dietary norms [
15]. This intricate interplay between disordered eating patterns and psychological distress underscores the critical need for a comprehensive examination of the multifaceted factors driving the development and perpetuation of these complex mental health conditions. Understanding the nuanced connections between eating disorders and co-occurring psychological challenges is paramount in developing systematic intervention strategies that address not only the behavioral aspects of disordered eating but also the underlying emotional and psychological vulnerabilities, fostering a more comprehensive approach to holistic well-being and recovery [
16].
In the face of the intricate web of psychological distress and disordered eating behaviours, the integration of mindfulness and mindful eating practices emerges as a compelling and systematic approach that amalgamates principles from psychology and nutrition [
17]. Mindful eating, characterised by a deliberate and nonjudgmental awareness of one's food choices and eating habits, fosters a more conscious and attuned relationship with food, emphasising the importance of savouring each bite and cultivating a deeper understanding of one's bodily cues and nutritional needs [
18]. By promoting a heightened sense of self-awareness and a non-reactive attitude toward food, mindful eating serves as a potential cornerstone for addressing the complex interplay between Orthorexia Nervosa, psychological distress, and the detrimental influences of Instagram use.
In the context of Orthorexia Nervosa, the incorporation of mindful eating practices could offer a transformative avenue for individuals to cultivate a more balanced and flexible approach to their dietary choices. By encouraging a non-restrictive and compassionate outlook towards food, mindful eating alleviates the rigid dietary rules and obsessive thoughts surrounding food quality, thereby mitigating the psychological distress and anxiety associated with deviating from self-imposed dietary norms [
19]. Furthermore, the cultivation of mindful eating habits could foster a profound sense of empowerment and autonomy, enabling individuals to embrace their dietary behaviours [
20] without succumbing to the pervasive pressures of social media and unrealistic beauty standards propagated by Instagram [
21].
The purpose of this research is to delve into a thorough examination of the complex interconnections among mindful eating, Instagram usage, and eating disorders, with a specific focus on the emerging concept of Orthorexia Nervosa, and its frequently understated yet crucial impact on depression, anxiety, and stress. The study seeks to unravel the intricate relationships between these variables, aiming to provide a comprehensive understanding of the underlying mechanisms shaping individuals' attitudes towards food, body image, and mental well-being. By elucidating the potential pathways through which mindful eating practices and Instagram use may influence the development and perpetuation of eating disorders, particularly Orthorexia Nervosa, the research endeavours to shed light on the often-unexplored role of psychological distress in the context of digital media consumption and dietary behaviours. Moreover, the study aims to highlight the significance of recognising the nuanced connections between mindful eating, Instagram usage, and psychological factors such as depression, anxiety, and stress, underscoring the need for holistic intervention strategies that address both the behavioural and emotional dimensions of disordered eating. Through a comprehensive analysis of these intricate associations, the study ultimately aspires to contribute to the formulation of targeted interventions and educational initiatives that promote healthier attitudes towards food, body image, and online engagement, fostering a more resilient and mindful approach to well-being in the digital era.
The hypothesis of our study suggests that, within a mindfulness-based approach, mindful eating may act as a mediator in the link between triggers for disordered eating behaviours such as depression, anxiety, and stress. Furthermore, these triggers influenced by contemporary society norms as portrayed on Instagram in the modern era, could be associated with Orthorexia.
2. Materials and Methods
2.1. Design and procedure
The study employed a cross-sectional design and utilized an online survey conducted in both Greek and English languages through the Sogolytics software platform [
22]. The first two survey questions were utilized as inclusion and exclusion criteria, ensuring participants' acknowledgment of the study's terms and conditions, and verifying their age within the range of 18 to 65 years. The survey was disseminated through direct messaging on various social media applications, with follow-up reminders to encourage participant engagement and provide a platform for addressing any inquiries or concerns related to the study. This hybrid method utilizes the advantages of both web and mailed questionnaires [
23].
To ensure the questionnaire's validity and reliability, a pilot study involving 50 participants was conducted [
24], revealing no issues with the survey. The data collected during the pilot study were seamlessly integrated into the final sample. Before initiating the data collection process, the study's purpose and hypotheses were clearly specified, providing a comprehensive framework for the research analysis and interpretation. The final sample consisted of 407 adults.
2.2. Ethics
This research adhered strictly to the established ethical guidelines and professional principles outlined in the Declaration of Helsinki. Participants were required to consent to the research's terms and conditions before their involvement. The study protocol, identified as application no. 17715 / 09.09.2021, received approval from the ethics and deontology committee at the University of the Aegean. The approval was granted based on the research's alignment with the university's Code of Ethics and Professional Conduct for Research, ensuring adherence to the appropriate ethical, professional, and legal standards.
2.3. Scales
2.3.1. Mindful Eating Scale-16
The MES-16 represents a condensed version of the 28-item Mindful Eating Scale (MES-28), initially introduced by Hulbert-Williams et al. [
25] to cater to the specific assessment needs within the domain of food behavior [
26]. Following the identification of certain deficient psychometric properties and sub-scale elements within the MES-28 by Hulbert-Williams et al. [
27], subsequent revisions were implemented to enhance its robustness. The refined MES-16 now comprises 16 components categorized into five distinct sub-scales: self-acceptance, awareness, non-reactivity, routine, and conscious action.
Utilizing a Likert scale [
28], the MES-16 prompts respondents to express their level of agreement with various statements related to mindful eating behaviors. A standard question within the MES-16 scale, for instance, involves assessing the degree of consciousness during eating habits, as indicated by the statement, "I eat something without really being aware of it." Respondents rate their agreement on a scale of 1 to 4, with the cumulative score ranging from 16 to 64. Higher scores on the MES-16 suggest a more pronounced tendency toward mindful eating practices [
27].
This particular scale was chosen due to its alignment with the fundamental principles of mindfulness, specifically as they pertain to dietary habits [
26]. The current study observed an acceptable internal consistency index (Cronbach's α) of 0.694 for the overall MES-16 scale.
2.3.2. Eating Disorder Examination Questionnaire Short (EDE-QS)
The Eating Disorder Examination Questionnaire (EDE-QS) is a 12-item validated self-report instrument used for the assessment of eating disorder symptoms, that derives from the 28-item Eating Disorder Examination (EDE-Q). The EDE-QS measures various facets of disordered eating behaviors such as dietary restraint, eating concerns, shape concerns, and weight concerns. Participants rate the frequency and severity of these behaviors over the preceding 7 days on a 4-point rating scale, with higher scores indicating a greater degree of pathology [
29]. Example question: "How dissatisfied have you been with your weight or shape?"
Widely recognized and extensively utilized, the EDE-QS serves as a critical instrument for identifying individuals at risk of eating disorders, facilitating early intervention and tailored treatment strategies. Its standardized scoring methodology and multidimensional assessment approach contribute to a comprehensive understanding of eating disorder pathology, guiding clinicians and researchers in the effective management and study of these complex conditions [
30]. In our study, this scale EDE-QS had a Cronbach’a internal consistency index of α=0.885.
2.3.3. Depression Anxiety Stress Scale (DASS-21)
The Depression Anxiety Stress Scale (DASS-21) is a well-established self-report measure used to assess the severity of symptoms related to depression, anxiety, and stress. Comprising 21 items, the scale is divided into three sub-scales, each focusing on specific psychological constructs: depression, anxiety, and stress. Participants rate the frequency and intensity of their experiences over the past week on a 4-point Likert scale, with higher scores indicating a greater degree of symptom severity [
31].
The DASS-21 employs a standardized scoring system that allows for the computation of individual sub-scale scores as well as a combined total score, providing a comprehensive evaluation of the participant's emotional well-being. It is widely recognized for its reliable and valid psychometric properties, making it an invaluable tool for both clinical and research purposes in the assessment and monitoring of mental health conditions [
32]. Example question: "Over the past week, how often have you felt downhearted and blue?" Participants select a response on the 4-point scale, ranging from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time).
Due to its robust assessment framework and sensitivity to changes in symptom severity, the DASS-21 serves as a critical instrument for identifying and evaluating individuals experiencing symptoms of depression, anxiety, and stress. Its systematic approach and comprehensive measurement contribute to a better understanding of psychological distress, facilitating targeted interventions and improved mental health outcomes [
33]. The DASS-21 had an excellent internal consistency index (Cronbach’s α), α=0.953
2.3.4. ORTO-R
ORTO-R represents a revised version of the original ORTO-15 questionnaire tailored to assess Orthorexia nervosa tendencies. Initially, the ORTO-15 consisted of 15 questions, each providing respondents with four Likert-scale response options (always, often, sometimes, and never), corresponding to scores ranging from 1 to 4. The original research publication introduced a diagnostic threshold of 35, obtained by summing individual item scores, to identify Orthorexia Nervosa (ON) [
34].
In its updated format, ORTO-R retains six questions from the original version, now offering respondents five response options (never, rarely, sometimes, frequently, and always) for each question. Scoring for the ORTO-R questionnaire ranges from 1 to 30, with individual question scores varying between 1 and 5, based on the selected response. Unlike the earlier iteration, ORTO-R does not propose a specific threshold for diagnosing ON. Instead, the cumulative score is interpreted on a scale, indicating different degrees of inclination towards Orthorexia Nervosa tendencies [
35]. The Cronbach’s α of ORTO-R in the current study was α=0.673.
2.3.5. Demographics, Somatometrics and Instagram use
Demographic questions such as age and gender, were included in the survey. To mitigate potential survey dropout rates [
36], somatometric inquiries were strategically positioned at the conclusion of the survey. Participants were prompted to furnish their height and weight, enabling the calculation of their Body Mass Index (BMI). While acknowledging the limitations of relying on self-reported data for height and weight, this approach remains accepted for BMI computations in adult populations, particularly across diverse socio-demographic cohorts [
37]. Following established protocols [
38], individuals' BMI values were classified into distinct subcategories, such as underweight, normal weight, overweight, and obesity.
Instagram use was evaluated through two specific questions in this study. The first question was employed to establish the presence of an active Instagram account among participants. The second question focused on quantifying the average daily time dedicated to the platform. The inclusion of these questions was intended to offer valuable insights into participants' Instagram usage patterns and their potential influence on psychological well-being and dietary behaviors [
39].
2.4. Statistical analysis
A comprehensive examination of the data was undertaken to detect potential omissions. Instances where participants abruptly discontinued the questionnaire (Missing Completely at Random) led to the exclusion of the corresponding data from the analysis [
40]. In cases of inadvertent oversights (Missing at Random), missing data points were substituted with the mean value derived from all respondents' answers.
The data were exported in a format compatible with import and processing in SPSS v28 and R-Statistics. Analysis and visualization of the data were conducted using the statistical analysis software SPSS v28 and R-Statistics. Before subjecting the data to statistical tests, a regularity check was performed to ensure its distribution met established criteria. The literature recommends conducting the regularity test before engaging in statistical analyses. To ensure the most accurate and reliable assessment of regularity, a combination of visual examination and the Shapiro-Wilk test was employed [
41]. Thorough regularity testing was applied to the primary research variables. The results in multinomial logistic regression analysis were adjusted for possible confounders such as age and gender. The statistical significance level was set at p<0.05.
3. Results
3.1. Subjects
The survey involved the participation of 548 individuals. Following the exclusion of 122 respondents who did not meet the survey's inclusion criteria and 19 cases with incomplete (answering less than 50% of total questions) or random responses (questions answered in less than 3 minutes), the final sample comprised 407 adults, with 68.3% being women. A predominant percentage of the participants (61.6%) fell within the age range of 18 to 29 years old. Women had statistically significant (p<0.05) lower scores of MES-16, and higher scores of DASS-21, EDE-QS, ORTO-R.
3.2. Correlations between MES-16, DASS-21, EDE-QS, and ORTO-R
To assess the correlation among MES-16, DASS-21, EDE-QS, and ORTO-R, Pearson’s correlation coefficients were computed. Statistical analysis revealed a significant negative correlation of MES-16 with DASS-21, EDE-QS, and ORTO-R scores, as well as a significant positive inter-correlation between DASS-21, EDE-QS and ORTO-R scores (
Table 1).
3.3. The association of depression, anxiety, and stress with mindful eating, and eating disorders
Pearson's correlation coefficients were used to further investigate the relationship between mindful eating, eating disorders and the various elements of the DASS-21 scale as reflected through its subcategories of depression, anxiety, and stress. MES-16 had a statistically significant negative correlation with depression, anxiety, and stress scores (
Table 2).
Eating disorders were significantly associated with depression, anxiety, stress (
Table 3). Among DASS-21 sub scales, stress had the strongest negative correlation with MES-16, and the strongest positive correlation with EDE-QS, followed by depression.
3.4. Mindful eating, eating disorders and Orthorexia nervosa
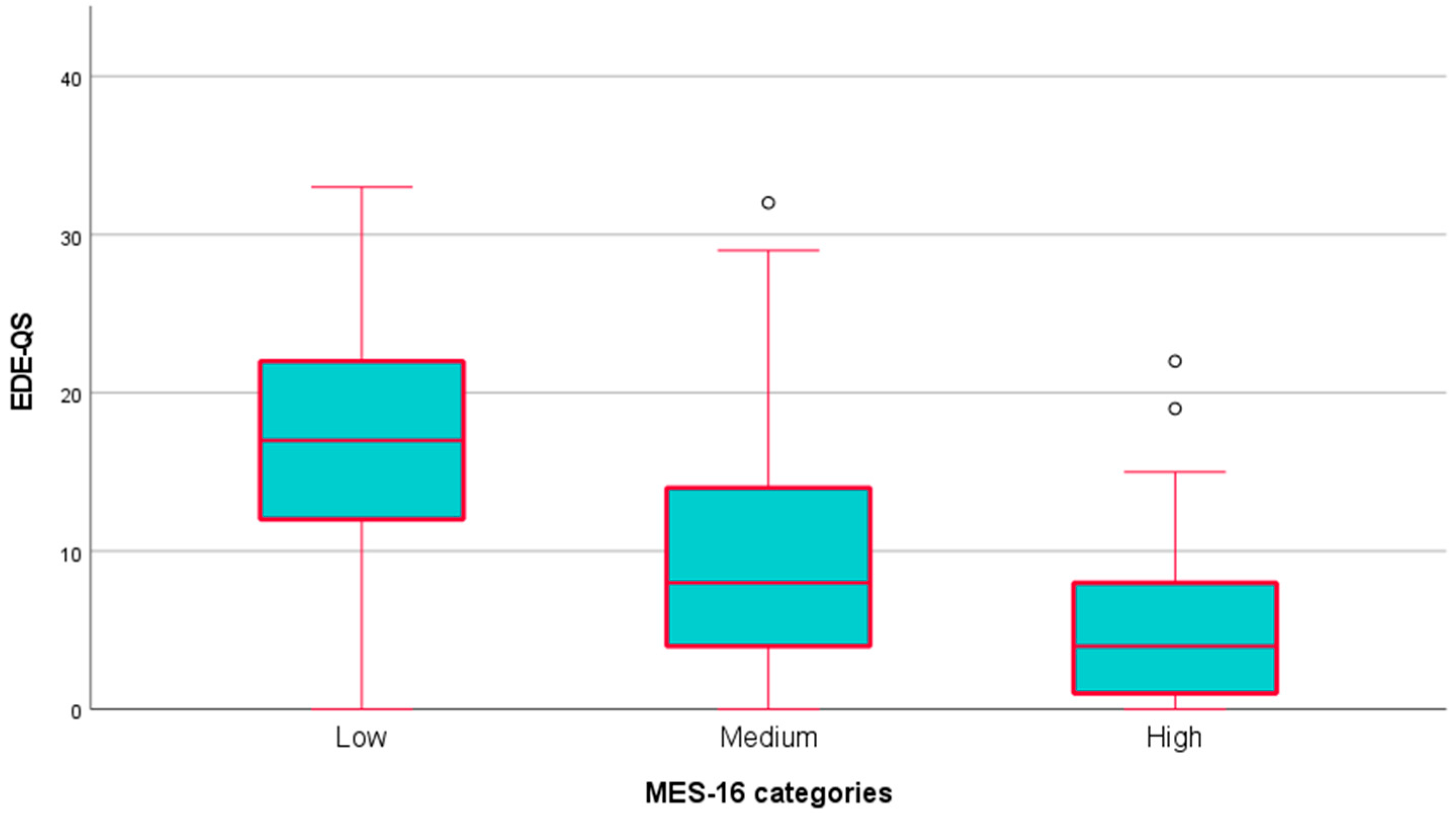
One-way ANOVA test indicated a statistically significant difference (p < 0.05) in the means of EDE-QS across different MES-16 categories (
Figure 1).
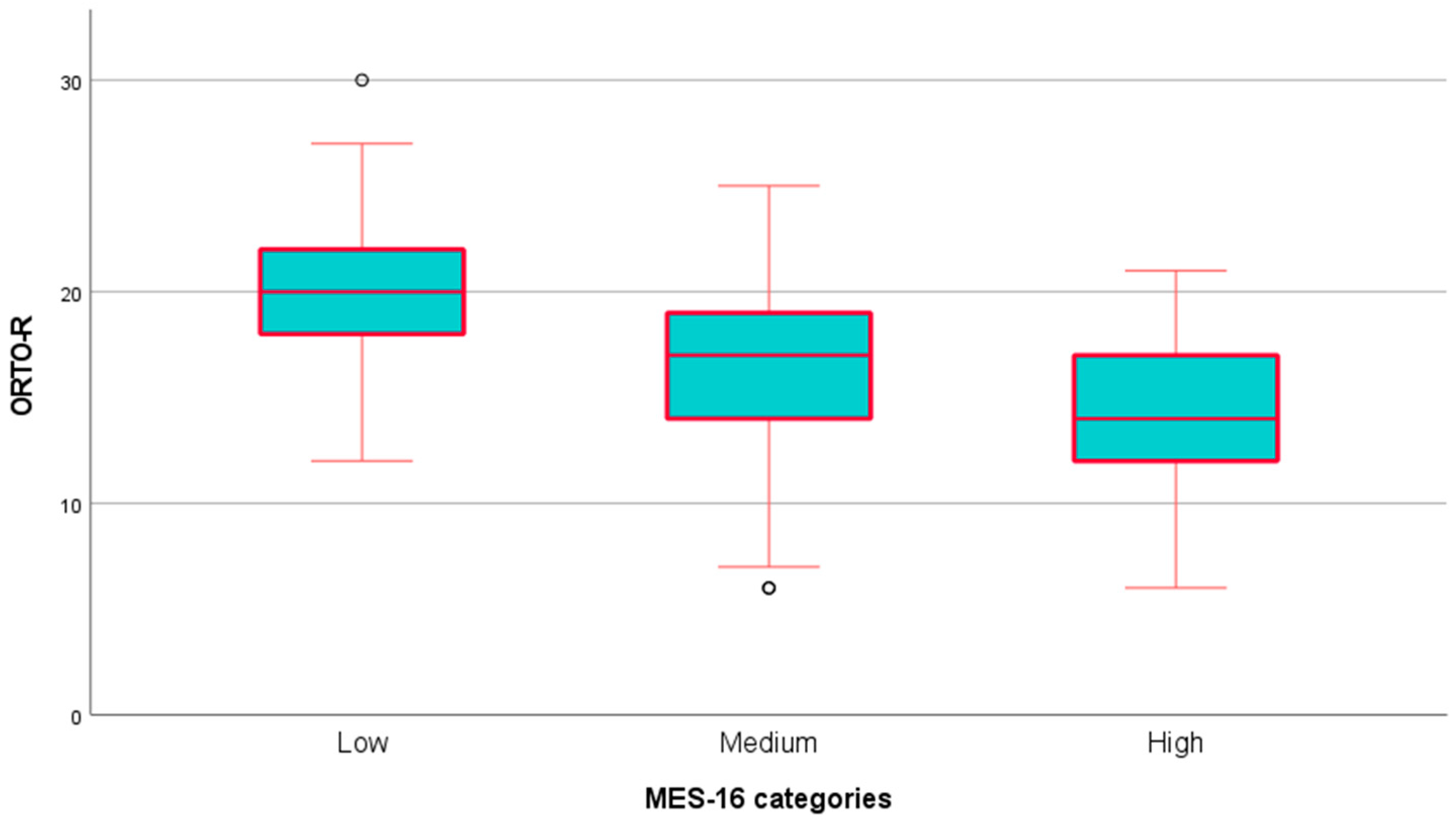
The same statistical test demonstrated a significant difference (p < 0.05) in the means of ORTO-R across various MES-16 categories (
Figure 2).
Multinomial logistic regression analysis identified MES-16 as a prognostic factor for having a low EDE-QS score (OR: 1.364, 95% CI: 1.263, 1.474, p < 0.001, compared to a high EDE-QS score) and having a low ORTO-R score (OR: 1.301, 95% CI: 1.208, 1.401, p < 0.001, compared to a high ORTO-R score).
3.5. Instagram engagement, depression, anxiety and stress
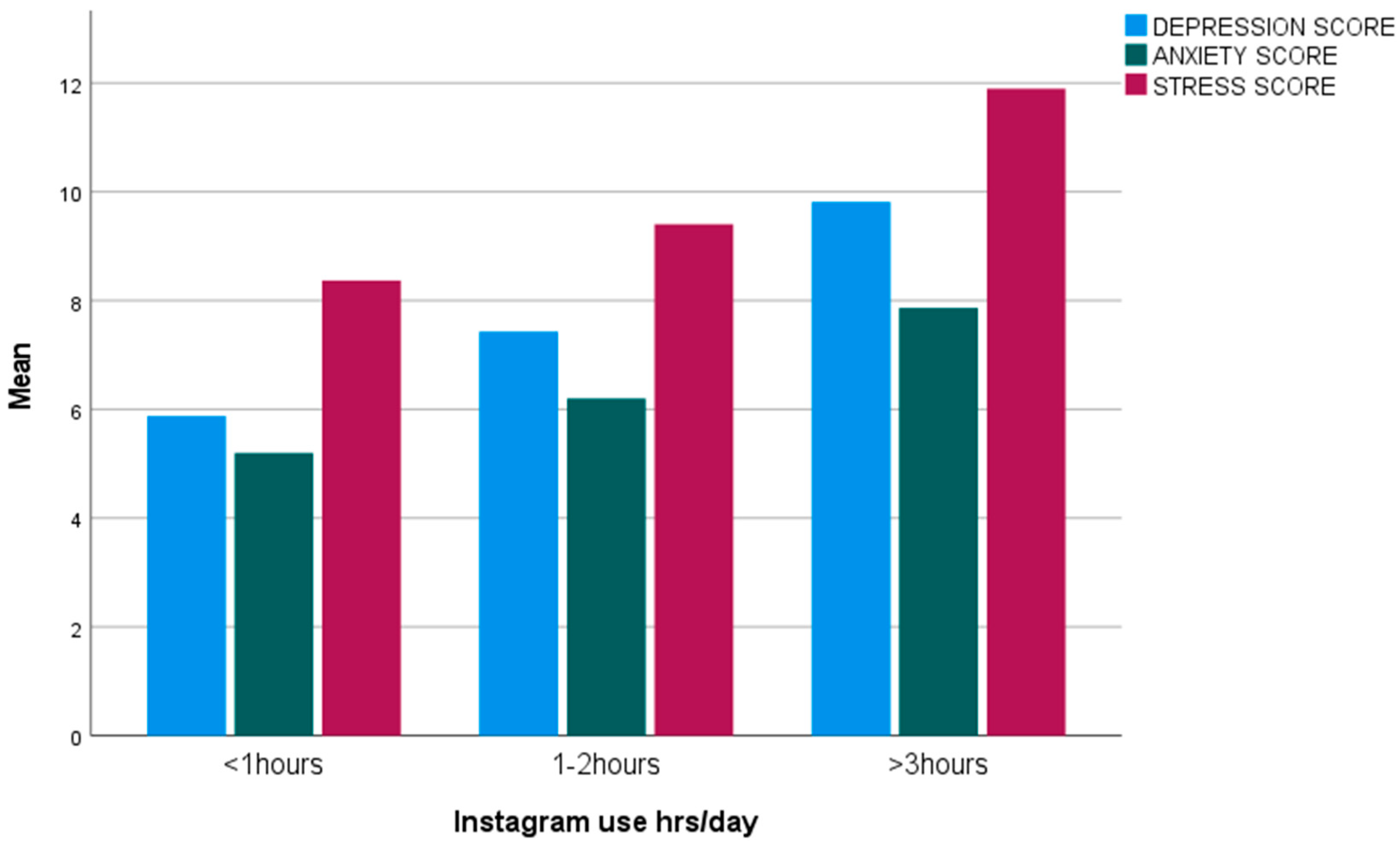
Instagram emerged as a widely favored social media platform among the study participants. Specifically, 46.5% of the participants dedicated more than 3 hours daily to Instagram, 35.2% allocated 1-3 hours daily, and a mere 15.5% spent less than 1 hour daily on the platform or were non-users of Instagram. There was a statistically significant difference between the means of depression (p=0.002), anxiety (p=0.016) and stress (p=0.002) scores in various Instagram engagement categories (
Figure 3).
3.6. Instagram engagement, eating disorders and anorexia nervosa
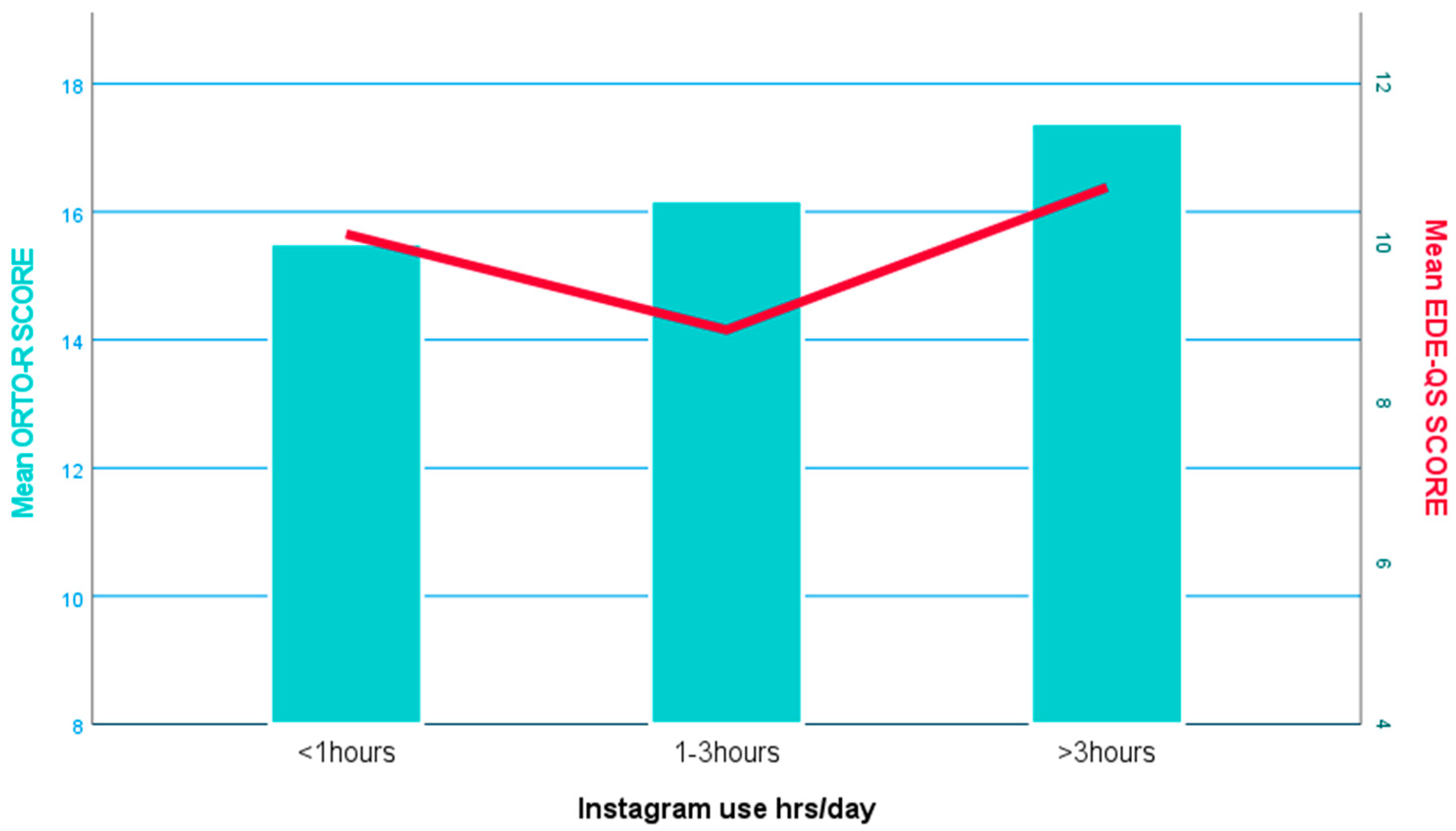
The daily utilization of this social media platform did not have any statistical significance in relation to EDE-QS scores. On the contrary, there was a significant difference (p<0.05) in the means of ORTO-R scores in different daily use of Instagram (
Figure 4).
Multinomial logistic regression analysis demonstrated that a one-unit increment in the ORTO-R score was associated with a 10% elevation in the odds of participants spending more than 3 hours per day on Instagram (OR: 1.100, 95% CI: 1.023, 1.183, p < 0.01) in comparison to individuals spending less than an hour per day on the platform. Moreover, women exhibited nearly three times higher odds than men of engaging in Instagram usage for more than 3 hours daily, after a one-point increase in the ORTO-R score (OR: 2.988, 95% CI: 1.628, 5.484, p < 0.001).
4. Discussion
This study represents the first known exploration of the intricate connections among mindful eating, Instagram usage, and eating disorders, with a specific focus on Orthorexia Nervosa, in the context of the Greek population. The significance of this research lies in its contribution to unraveling the complex web of psychological distress and disordered eating behaviors within the digital era, where the influence of social media, particularly Instagram, plays a pivotal role.
The study, involving 407 adults, sheds light on the intricate relationships between mindful eating (MES-16), psychological well-being (DASS-21), disordered eating (EDE-QS), and Orthorexia Nervosa tendencies (ORTO-R). Utilizing Pearson's correlation coefficients, the research quantitatively explores these connections.
Significantly, a negative correlation emerges between mindful eating and psychological well-being. This aligns with existing literature emphasizing the mental health benefits of mindfulness practices [
42], suggesting that mindful eating fosters a balanced and attuned relationship with eating, reducing psychological distress.
Furthermore, the negative correlation between mindful eating and eating disorders suggests a potential therapeutic role of mindful eating in mitigating disordered eating behaviors. Consistent with previous research [
43], this finding implies that mindful eating is associated with a lower likelihood of engaging in problematic eating behaviors linked to various eating disorders.
The negative correlation between mindful eating and Orthorexia nervosa is also notable, indicating that individuals practicing mindful eating are less likely to exhibit high Orthorexia Nervosa tendencies. This aligns with the conceptualization of mindful eating as fostering a nonrestrictive and compassionate approach to food, potentially mitigating the rigid dietary restrictions associated with Orthorexia Nervosa [
44].
Moreover, the study reveals a significant positive inter-correlation among psychological well-being, disordered eating, and Orthorexia nervosa, emphasizing the complex connections between psychological distress, disordered eating, and Orthorexia Nervosa tendencies. This aligns with existing literature highlighting the multifaceted nature of eating disorders and their co-occurrence with psychological challenges [
45]. The stringent dietary regulations seen in Orthorexia Nervosa contribute to heightened levels of depression, anxiety and stress [
46].
Pearson's correlation coefficients demonstrated a statistically significant negative association between mindful eating and depression, anxiety, and stress scores after categorizing DASS-21 [
47]. Notably, eating disorders are strongly linked to depression, anxiety, and stress [
48]. Stress emerges as a critical element, with a negative correlation with mindful eating and a positive correlation with eating disorders [
49].
These findings emphasize the crucial role of stress and depression in the manifestation of eating disorders [
50]. The strong negative correlation between stress and mindful eating suggests that mindful eating could serve as a potential mechanism to mitigate eating disorder symptoms [
51]. Mindful eating practices may address stress and depression, fostering a more balanced and attuned relationship with food and thereby contributing to the amelioration of disordered eating behaviors [
52]. This underscores the importance of incorporating mindfulness-based interventions in comprehensive strategies targeting eating disorders [
53].
The study participants overwhelmingly favored Instagram, with 46.5% spending more than 3 hours daily on the platform. This extensive engagement with Instagram was associated with depression, anxiety, and stress. These findings underscore the impact of Instagram on psychological well-being, aligning with existing literature that highlights the platform's role in influencing mental health outcomes [
54].
The study's focus on the relationship between Instagram engagement and eating disorders revealed intriguing results. While daily Instagram use did not show statistical significance concerning disordered eating, it did exhibit a noteworthy association with Orthorexia nervosa tendencies, as indicated by the significant difference in means of ORTO-R scores based on daily Instagram engagement. This finding supports the growing body of research that links social media use, particularly on visually oriented platforms like Instagram, to the development of Orthorexia nervosa [
55].
Multinomial logistic regression analysis further elucidated the connection between Instagram usage and Orthorexia Nervosa tendencies. A one-unit increment in the ORTO-R score was associated with a 10% increase in the odds of spending more than 3 hours per day on Instagram. Additionally, women showed nearly three times higher odds than men of engaging in extensive Instagram use if their ORTO-R score increased by one point. These results suggest a gender-specific association between Orthorexia Nervosa tendencies and increased Instagram usage, aligning with studies that emphasize the platform's role in shaping body image ideals and dietary norms, particularly for women [
56].
The presented findings underscore the need for awareness campaigns and educational initiatives addressing the impact of specific social media platforms, like Instagram, on mental health and dietary behaviors. The association between Instagram use and Orthorexia Nervosa tendencies highlights the platform's potential role in perpetuating unrealistic body image paradigms and promoting disordered eating behaviors. Recognizing these associations is crucial for developing targeted interventions that address the nuanced connections between online engagement, mental well-being, and the development of eating disorders.
Limitations
This study, while providing valuable insights, is not without limitations. The cross-sectional design limits the establishment of causality, and the reliance on self-reported data introduces potential biases. Future longitudinal studies and objective measures could enhance the robustness of findings. Additionally, the study's sample predominantly comprised young adults, potentially limiting the generalizability of results to other age groups.
5. Conclusions
The study's outcomes validate the hypothesized associations between mindful eating, Instagram engagement, and Orthorexia nervosa. Mindful eating demonstrates an inverse relationship with depression, anxiety, stress, and disordered eating, serving as a predictive factor for lower eating disorder and lower Orthorexia nervosa tendencies. Increased mindful eating levels correspond to diminished disordered eating and lower Orthorexia nervosa propensities. Moreover, the widespread use of Instagram in Greece, particularly high engagement rates, is associated with heightened depression, anxiety, and stress levels. Elevated Instagram engagement further aligns with increased Orthorexia nervosa tendencies, particularly in women. To substantiate these findings, randomized control trials are recommended, considering the study's cross-sectional design.
Author Contributions
Conceptualization, Efstratios Christodoulou and Antonios Koutelidakis; Data curation, Efstratios Christodoulou; Formal analysis, Efstratios Christodoulou; Investigation, Efstratios Christodoulou and Verra Markopoulou ; Methodology, Efstratios Christodoulou, Verra Markopoulou and Antonios Koutelidakis; Project administration, Antonios Koutelidakis; Resources, Efstratios Christodoulou and Verra Markopoulou ; Software, Efstratios Christodoulou; Supervision, Antonios Koutelidakis; Validation, Antonios Koutelidakis; Writing – original draft, Efstratios Christodoulou; Writing – review & editing, Antonios Koutelidakis.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the University of the Aegean's ethics and deontology committee (no. 17715/09.09.2021)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
No new data were created.
Acknowledgments
The authors thanks all the authors who participated to the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wright PJ, Raynor PA, Bowers D, et al. Leveraging digital technology for social connectedness among adults with chronic conditions: A systematic review. Digit Health. 2023;9:20552076231204746. Published 2023 Oct 3. [CrossRef]
- Vincente-Benito I, Ramírez-Durán MDV. Influence of Social Media Use on Body Image and Well-Being Among Adolescents and Young Adults: A Systematic Review [published online ahead of print, 2023 Jun 2]. J Psychosoc Nurs Ment Health Serv. 2023;1-8. [CrossRef]
- Karim F, Oyewande AA, Abdalla LF, Chaudhry Ehsanullah R, Khan S. Social Media Use and Its Connection to Mental Health: A Systematic Review. Cureus. 2020;12(6):e8627. Published 2020 Jun 15. [CrossRef]
- Jiotsa B, Naccache B, Duval M, Rocher B, Grall-Bronnec M. Social Media Use and Body Image Disorders: Association between Frequency of Comparing One's Own Physical Appearance to That of People Being Followed on Social Media and Body Dissatisfaction and Drive for Thinness. Int J Environ Res Public Health. 2021;18(6):2880. Published 2021 Mar 11. [CrossRef]
- Pedalino F, Camerini AL. Instagram Use and Body Dissatisfaction: The Mediating Role of Upward Social Comparison with Peers and Influencers among Young Females. Int J Environ Res Public Health. 2022;19(3):1543. Published 2022 Jan 29. [CrossRef]
- Aparicio-Martinez P, Perea-Moreno AJ, Martinez-Jimenez MP, Redel-Macías MD, Pagliari C, Vaquero-Abellan M. Social Media, Thin-Ideal, Body Dissatisfaction and Disordered Eating Attitudes: An Exploratory Analysis. Int J Environ Res Public Health. 2019;16(21):4177. Published 2019 Oct 29. [CrossRef]
- Budhiwianto S, Bennett CJ, Bristow CA, Dart J. Global Prevalence of Eating Disorders in Nutrition and Dietetic University Students: A Systematic Scoping Review. Nutrients. 2023; 15(10):2317. [CrossRef]
- Makri E, Michopoulos I, Gonidakis F. Investigation of Loneliness and Social Support in Patients with Eating Disorders: A Case-Control Study. Psychiatry International. 2022; 3(2):142-157. [CrossRef]
- Horovitz O, Argyrides M. Orthorexia and Orthorexia Nervosa: A Comprehensive Examination of Prevalence, Risk Factors, Diagnosis, and Treatment. Nutrients. 2023; 15(17):3851. [CrossRef]
- Gkiouleka M, Stavraki C, Sergentanis TN, Vassilakou T. Orthorexia Nervosa in Adolescents and Young Adults: A Literature Review. Children. 2022; 9(3):365. [CrossRef]
- Pontillo M, Zanna V, Demaria F, Averna R, Di Vincenzo C, De Biase M, Di Luzio M, Foti B, Tata MC, Vicari S. Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years. Journal of Clinical Medicine. 2022; 11(20):6134. [CrossRef]
- Horovitz O, Argyrides M. Orthorexia and Orthorexia Nervosa: A Comprehensive Examination of Prevalence, Risk Factors, Diagnosis, and Treatment. Nutrients. 2023; 15(17):3851. [CrossRef]
- Awad E, Salameh P, Sacre H, Malaeb D, Hallit S, Obeid S. Association between impulsivity and orthorexia nervosa / healthy orthorexia: any mediating effect of depression, anxiety, and stress?. BMC Psychiatry. 2021;21(1):604. Published 2021 Dec 3. [CrossRef]
- Costandache GI, Munteanu O, Salaru A, Oroian B, Cozmin M. An overview of the treatment of eating disorders in adults and adolescents: pharmacology and psychotherapy. Postep Psychiatr Neurol. 2023;32(1):40-48. [CrossRef]
- Scarff JR. Orthorexia Nervosa: An Obsession With Healthy Eating. Fed Pract. 2017;34(6):36-39.
- Strahler J, Hermann A, Walter B, Stark R. Orthorexia nervosa: A behavioral complex or a psychological condition?. J Behav Addict. 2018;7(4):1143-1156. doi:10.1556/2006.7.2018.129Mantzios M. Mindful eating: A conceptual critical review of the literature, measurement and intervention development. Nutr Health. 2023;29(3):435-441. [CrossRef]
- Mantzios M. Mindful eating: A conceptual critical review of the literature, measurement and intervention development. Nutr Health. 2023;29(3):435-441. [CrossRef]
- Nelson JB. Mindful Eating: The Art of Presence While You Eat. Diabetes Spectr. 2017;30(3):171-174. [CrossRef]
- Miley M, Egan H, Wallis D, Mantzios M. Orthorexia nervosa, mindful eating, and perfectionism: an exploratory investigation. Eat Weight Disord. 2022;27(7):2869-2878. [CrossRef]
- Kalika E, Egan H, Mantzios M. Exploring the role of mindful eating and self-compassion on eating behaviours and orthorexia in people following a vegan diet. Eat Weight Disord. 2022;27(7):2641-2651. [CrossRef]
- Kim D, Kim S. Social Media Affordances of Ephemerality and Permanence: Social Comparison, Self-Esteem, and Body Image Concerns. Social Sciences. 2023; 12(2):87. [CrossRef]
- Christodoulou E, Meca A, Koutelidakis AE. Herbal Infusions as a Part of the Mediterranean Diet and Their Association with Psychological Resilience: The Paradigm of Greek Mountain Tea. Nutraceuticals. 2023; 3(3):438-450. [CrossRef]
- Menon V, Muraleedharan A. Internet-based surveys: relevance, methodological considerations and troubleshooting strategies. Gen Psychiatr. 2020;33(5):e100264. Published 2020 Aug 1. [CrossRef]
- Christodoulou E, Deligiannidou G-E, Kontogiorgis C, Giaginis C, Koutelidakis AE. Natural Functional Foods as a Part of the Mediterranean Lifestyle and Their Association with Psychological Resilience and Other Health-Related Parameters. Applied Sciences. 2023; 13(7):4076. [CrossRef]
- Hulbert-Williams L, Nicholls W, Joy J, Hulbert-Williams N. Initial validation of the Mindful Eating Scale. Mindfulness, 2014;5(6):719–729. [CrossRef]
- Michail Mantzios. Development and initial validation of the Trait and State Mindful Eating Behaviour scales, 29 November 2022, PREPRINT (Version 1) available at Research Square. [CrossRef]
- Hulbert-Williams L, Nichols W, Flynn S, Hulbert-Williams N. Further development and validation of a novel measure of trait mindful eating (Poster). Retrieved from University of Chester website: https://www.chester.ac.uk/sites/files/chester/Mindful%20eating%20scale%20CFA%20poster.pdf.
- Arnold WE, McCroskey JC, Prichard SVO. The Likert-type scale. Today's Speech, 15/2: 31-33. Published 1967.
- Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, Serpell L. Development and Psychometric Validation of the EDE-QS, a 12 Item Short Form of the Eating Disorder Examination Questionnaire (EDE-Q) [published correction appears in PLoS One. 2018 Nov 5;13(11):e0207256]. PLoS One. 2016;11(5):e0152744. Published 2016 May 3. [CrossRef]
- Prnjak K, Mitchison D, Griffiths S, et al. Further development of the 12-item EDE-QS: identifying a cut-off for screening purposes. BMC Psychiatry. 2020;20(1):146. Published 2020 Apr 3. [CrossRef]
- Pezirkianidis C, Karakasidou E, Lakioti A, Stalikas A, Galanakis M. Psychometric Properties of the Depression, Anxiety, Stress Scales-21 (DASS-21) in a Greek Sample. Sci Res Publishing. 2018;9:2933-2950. [CrossRef]
- Oei TP, Sawang S, Goh YW, Mukhtar F. Using the Depression Anxiety Stress Scale 21 (DASS-21) across cultures. Int J Psychol. 2013;48(6):1018-1029. [CrossRef]
- Norton PJ. Depression Anxiety and Stress Scales (DASS-21): psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20(3):253-265. [CrossRef]
- Gonidakis F, Poulopoulou C, Michopoulos I, Varsou E. Validation of the Greek ORTO-15 questionnaire for the assessment of orthorexia nervosa and its relation to eating disorders symptomatology. Eat Weight Disord. 2021;26(8):2471-2479. [CrossRef]
- Gkiouras K, Grammatikopoulou MG, Tsaliki T, et al. Orthorexia nervosa: replication and validation of the ORTO questionnaires translated into Greek in a survey of 848 Greek individuals. Hormones (Athens). 2022;21(2):251-260. [CrossRef]
- Jones TL, Baxter MA, Khanduja V. A quick guide to survey research. Ann R Coll Surg Engl. 2013;95(1):5-7. [CrossRef]
- Hodge JM, Shah R, McCullough ML, Gapstur SM, Patel AV. Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLoS One. 2020;15(4):e0231229. Published 2020 Apr 13. [CrossRef]
- Nuttall FQ. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015;50(3):117-128. [CrossRef]
- Limniou M, Ascroft Y, McLean S. Differences between Facebook and Instagram Usage in Regard to Problematic Use and Well-Being. J Technol Behav Sci. 2022;7(2):141-150. [CrossRef]
- Kwak SK, Kim JH. Statistical data preparation: management of missing values and outliers. Korean J Anesthesiol. 2017;70(4):407-411. [CrossRef]
- Ghasemi A, Zahediasl S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab. 2012;10(2):486-489. [CrossRef]
- Christodoulou, E., Deligiannidou, G., Kontogiorgis, C., Giaginis, C., & Koutelidakis, A.Ε. (2023). Fostering Resilience and Wellness: The Synergy of Mindful Eating and the Mediterranean Lifestyle. Preprints. [CrossRef]
- Sala M, Shankar Ram S, Vanzhula IA, Levinson CA. Mindfulness and eating disorder psychopathology: A meta-analysis. Int J Eat Disord. 2020;53(6):834-851. [CrossRef]
- Kalika E, Hussain M, Egan H, Mantzios M. Exploring the moderating role of mindfulness, mindful eating, and self-compassion on the relationship between eating-disordered quality of life and orthorexia nervosa. Eat Weight Disord. 2023;28(1):18. Published 2023 Feb 20. [CrossRef]
- Duradoni M, Gursesli MC, Fiorenza M, Guazzini A. The Relationship between Orthorexia Nervosa and Obsessive Compulsive Disorder. Eur J Investig Health Psychol Educ. 2023;13(5):861-869. Published 2023 May 17. [CrossRef]
- Horovitz O, Argyrides M. Orthorexia and Orthorexia Nervosa: A Comprehensive Examination of Prevalence, Risk Factors, Diagnosis, and Treatment. Nutrients. 2023;15(17):3851. Published 2023 Sep 3. [CrossRef]
- Kotoulas AS, Karamanavis D, Lambrou GΙ, Karanikas P. A pilot study of the depression, anxiety and stress in Greek military personnel during the first year of the COVID-19 pandemic. BMJ Mil Health. 2023;169(4):297-301. [CrossRef]
- da Luz FQ, Mohsin M, Jana TA, Marinho LS, Santos Ed, Lobo I, Pascoareli L, Gaeta T, Ferrari S, Teixeira PC, et al. An Examination of the Relationships between Eating-Disorder Symptoms, Difficulties with Emotion Regulation, and Mental Health in People with Binge Eating Disorder. Behavioral Sciences. 2023; 13():234. [CrossRef]
- Sala M, Vanzhula I, Roos CR, Levinson CA. Mindfulness and Eating Disorders: A Network Analysis. Behav Ther. 2022;53(2):224-239. [CrossRef]
- Sander J, Moessner M, Bauer S. Depression, Anxiety and Eating Disorder-Related Impairment: Moderators in Female Adolescents and Young Adults. International Journal of Environmental Research and Public Health. 2021; 18(5):2779. [CrossRef]
- Giannopoulou I, Kotopoulea-Nikolaidi M, Daskou S, Martyn K, Patel A. Mindfulness in Eating Is Inversely Related to Binge Eating and Mood Disturbances in University Students in Health-Related Disciplines. Nutrients. 2020;12(2):396. Published 2020 Feb 2. [CrossRef]
- Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness Intervention for Stress Eating to Reduce Cortisol and Abdominal Fat among Overweight and Obese Women: An Exploratory Randomized Controlled Study. J Obes. 2011;2011:651936. [CrossRef]
- Sala L, Gorwood P, Vindreau C, Duriez P. Mindfulness-based cognitive therapy added to usual care improves eating behaviors in patients with bulimia nervosa and binge eating disorder by decreasing the cognitive load of words related to body shape, weight, and food. Eur Psychiatry. 2021;64(1):e67. Published 2021 Oct 28. [CrossRef]
- Ulvi O, Karamehic-Muratovic A, Baghbanzadeh M, Bashir A, Smith J, Haque U. Social Media Use and Mental Health: A Global Analysis. Epidemiologia (Basel). 2022;3(1):11-25. Published 2022 Jan 11. [CrossRef]
- Rozgonjuk D, Ignell J, Mech F, Rothermund E, Gündel H, Montag C. Smartphone and Instagram use, body dissatisfaction, and eating disorders: investigating the associations using self-report and tracked data. J Eat Disord. 2023;11(1):149. Published 2023 Sep 4. [CrossRef]
- Nelson SL, Harriger JA, Miller-Perrin C, Rouse SV. The effects of body-positive Instagram posts on body image in adult women. Body Image. 2022;42:338-346. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).