Submitted:
18 October 2023
Posted:
18 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
Materials and Methods
Participations
2. Materials and Methods
2.1. Procedure
2.2. Intervention
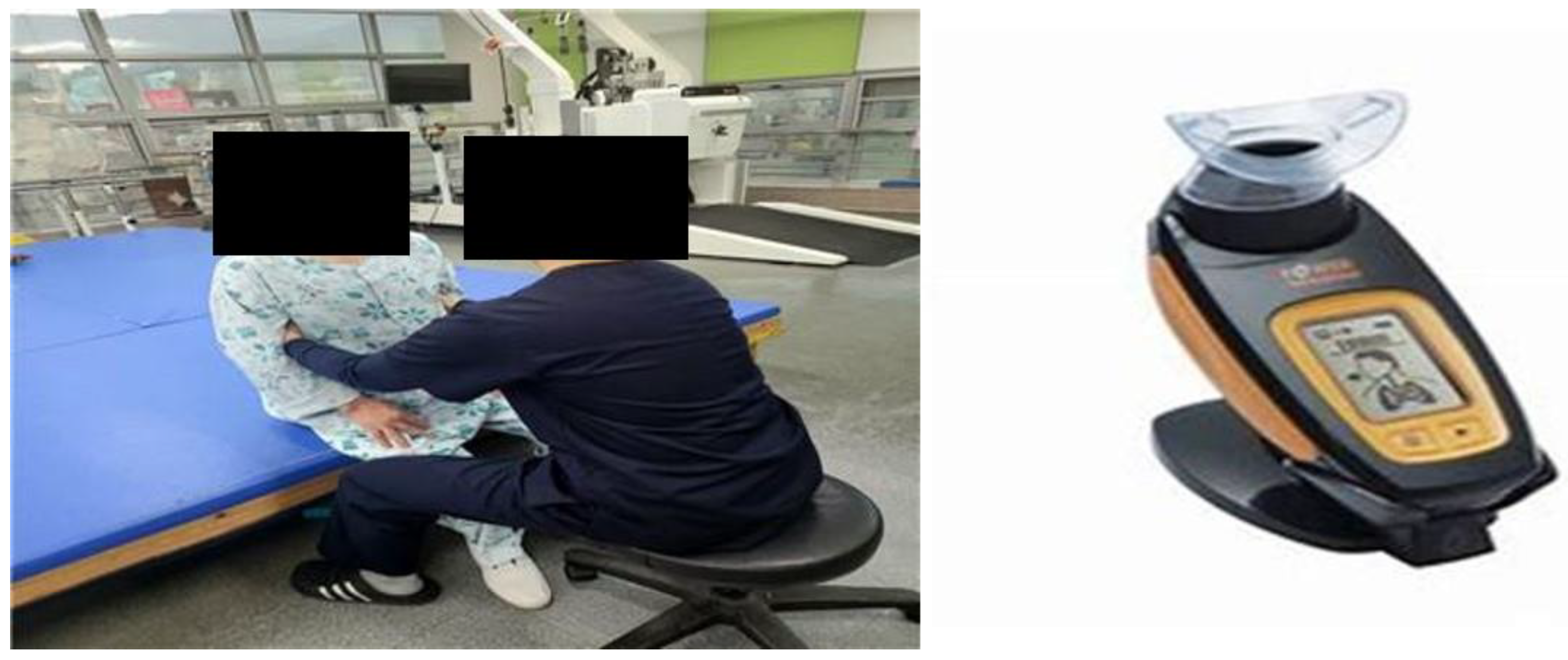
2.2.1. CMEBE Group
2.2.2. CPTBE Group
2.3. Evaluation
2.3.1. Respiratory Function Assessment
2.3.2. Trunk Stability Assessment
2.3.3. Endurance Assessment
2.4. Data Analysis
3. Results
3.1. General and Clinical Characteristics of the Patients
3.2. Changes in Respiratory Function before and after the Intervention
3.3. Changes in Trunk Stability before and after the Intervention
3.4. Changes in Endurance before and after the Intervention
4. Discussion
5. Conclutions
Conflicts of Interest
References
- Lee, S.W.; Yuh, W.T.; Yang, J.M.; Cho, Y.-S.; Yoo, I.K.; Koh, H.Y.; Marshall, D.; Oh, D.; Ha, E.K.; Han, M.Y.; et al. Nationwide Results of COVID-19 Contact Tracing in South Korea: Individual Participant Data From an Epidemiological Survey. Psychopharmacol. 2020, 8, e20992. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. COVID-19 outbreak in Korea () online: www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=361211; last accessed: 11.20. 20 November 2020.
- Lange, K.W. Food science and COVID-19. Food Sci. Hum. Wellness 2020, 10, 1–5. [Google Scholar] [CrossRef]
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Capan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.V.; George, M.G.; Hamdan, A.D.; Higashida, R.T.; Hoh, B.L. Janis, L.S; Kase, C.S., Kleindorfer, D.O., Lee, J.M., Moseley, M.E., Peterson, E.D., Turan, T.N., Valderrama, A.L., Eds.; Vinters, H.V. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013, 44(7), 2064–2089. [Google Scholar]
- National Statistical Office. Death cause statistics. 2020.
- McKenna, K.; Liddle, J.; Brown, A.; Lee, K.; Gustafsson, L. Comparison of time use, role participation and life satisfaction of older people after stroke with a sample without stroke. Aust. Occup. Ther. J. 2009, 56, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Seo, T.H. The effect of intensive Seraband exercise on balance and walking in chronic stroke patients. Journal of the Korea Entertainment Business Association Academic Conference. 2020, 5(4), 165–168. [Google Scholar]
- Kim, E.-K.; Lee, D.-K.; Kim, Y.-M. Effects of aquatic PNF lower extremity patterns on balance and ADL of stroke patients. J. Phys. Ther. Sci. 2015, 27, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J. Study on stroke effortful lung volume and respiratory efficiency improvement through recorder performance. Hum Behav Music Stud, 2007, 4(1), 31–46.
- De Almeida, I.C.; Clementino, A.C.; Rocha, E.H. Brandao D.C.; Andrade, A.D. Effects of hemiplegy on pulmonary function and diaphragmatic dome displacement. Respir Physiol Neurobiol, 2011, 178(2), 196–201. [CrossRef]
- Britto, R.R.; Rezende, N.R.; Marinho, K.C.; Torres, J.L.; Parreira, V.F.; Teixeira-Salmela, L.F. Inspiratory Muscular Training in Chronic Stroke Survivors: A Randomized Controlled Trial. Arch. Phys. Med. Rehabilitation 2011, 92, 184–190. [Google Scholar] [CrossRef]
- Sharp, S.A.; Brouwer, B.J. Isokinetic strength training of the hemiparetic knee: Effects on function and spasticity. Arch. Phys. Med. Rehabilitation 1997, 78, 1231–1236. [Google Scholar] [CrossRef]
- Patel, M.D.; Tilling, K.; Lawrence, E.; Rudd, A.G.; Wolfe, C.D.A.; McKevitt, C. Relationships between long-term stroke disability, handicap and health-related quality of life. J. Am. Geriatr. Soc. 2006, 35, 273–279. [Google Scholar] [CrossRef]
- Teixeira-Salmela, L.F.; Parreira, V.F.; Britto, R.R.; Brant, T.C.; Inácio. P.; Alcântara, T.O.; Carvalho, I.F. Respiratory Pressures and Thoracoabdominal Motion in Community-Dwelling Chronic Stroke Survivors. Arch. Phys. Med. Rehabilitation 2005, 86, 1974–1978. [Google Scholar] [CrossRef]
- Cohen, E.; Mier, A.; Heywood, P.; Murphy, K.; Boultbee, J.; Guz, A. Excursion-volume relation of the right hemidiaphragm measured by ultrasonography and respiratory airflow measurements. Thorax 1994, 49, 885–889. [Google Scholar] [CrossRef]
- Laroche, C.M.; Carroll, N.; Moxham, J.; Green, M. Clinical Significance of Severe Isolated Diaphragm Weakness. Am. Rev. Respir. Dis. 1988, 138, 862–866. [Google Scholar] [CrossRef] [PubMed]
- Annoni, J.-M.; Ackermann, D.; Kesselring, J. Respiratory function in chronic hemiplegia. Int. Disabil. Stud. 1990, 12, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.F.; Lien, I.N.; Wu, M.C. Respiratory function in patients with spinal cord injuries: effects of posture. Spinal Cord 1990, 28, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Dean, E. ; Frownfelter. Cardiovascular and pulmonary physical therapy. Evidence and practice. Fourth Edition. St. Louis: Mosby Elsevier, 2006.
- Fugl-Meyer, A.R.; Linderholm, H.; Wilson, A.F. Restrictive ventilatory dysfunction in stroke: its relation to locomotor function. Scand. J. Rehabil. Med. Suppl. 1983, 9, 118–24. [Google Scholar] [PubMed]
- Menezes, K.K.; Nascimento, L.R.; Ada, L.; Polese, J.C.; Avelino, P.R.; Teixeira-Salmela, L.F. Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. J. Physiother. 2016, 62, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Luo, M.; Wang, J.; Luo, H. Inspiratory muscle training for the recovery of function after stroke. Emergencias 2012, 2012, CD009360. [Google Scholar] [CrossRef]
- Cantuti-Castelvetri, L.; Ojha, R.; Pedro, L.D.; Djannatian, M.; Franz, J.; Kuivanen, S.; Simons, M. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science, 2020, 370(6518), 856–860.
- Verheyden, G.; Vereeck, L.; Truijen, S.; Troch, M.; Herregodts, I.; Lafosse, C.; Nieuwboer, A.; De Weerdt, W. Trunk performance after stroke and the relationship with balance, gait and functional ability. Clin. Rehabilitation 2006, 20, 451–458. [Google Scholar] [CrossRef]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age- and Gender-Related Test Performance in Community-Dwelling Elderly People: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and Gait Speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [CrossRef]
- Lanini, B.; Bianchi, R.; Romagnoli, I.; Coli, C.; Binazzi, B.; Gigliotti, F.; Pizzi, A.; Grippo, A.; Scano, G. Chest Wall Kinematics in Patients with Hemiplegia. Am. J. Respir. Crit. Care Med. 2003, 168, 109–113. [Google Scholar] [CrossRef]
- Kim, K.; Fell, D.W.; Lee, J.H. Feedback Respiratory Training to Enhance Chest Expansion and Pulmonary Function in Chronic Stroke: A Double-Blind, Randomized Controlled Study. J. Phys. Ther. Sci. 2011, 23, 75–79. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, D.H. Effects of PNF and respiratory muscle endurance training on lung function and physical activity in chronic stroke patients. PNF Mov, 2020, 18(2), 205- 214.
- Park, C.H. an informant. The effect of treadmill training on knee joints and elongation and speed of minutes in patients with paraplegia. J Korean Prof Phys Ther Soc, 2010, 8(1), 89–106.
- Park, S.-Y.; Son, W.-M.; Kwon, O.-S. Effects of whole body vibration training on body composition, skeletal muscle strength, and cardiovascular health. J. Exerc. Rehabilitation 2015, 11, 289–295. [Google Scholar] [CrossRef]
- Park, S.-J.; Lee, J.-H.; Min, K.-O. Comparison of the effects of core stabilization and chest mobilization exercises on lung function and chest wall expansion in stroke patients. J. Phys. Ther. Sci. 2017, 29, 1144–1147. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.-H.; Bang, H.-S. Effect of thoracic and cervical joint mobilization on pulmonary function in stroke patients. J. Phys. Ther. Sci. 2016, 28, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.; Shin, J.-H.; Lee, W.-H. Effect of Thoracic Joint Mobilization and Breathing Exercise on The Thickness of The Diaphragm, Expansion of The Chest, Respiratory Function, and Endurance in Chronic Stroke Patients. Phys. Ther. Rehabilitation Sci. 2023, 12, 278–292. [Google Scholar] [CrossRef]
- Petrovic, M.; Lahrmann, H.; Pohl, W.; Wanke, T. Idiopathic diaphragmatic paralysis—Satisfactory improvement of inspiratory muscle function by inspiratory muscle training. Respir. Physiol. Neurobiol. 2009, 165, 266–267. [Google Scholar] [CrossRef]
- Sutbeyaz, S.T.; Koseoglu, F.; Inan, L.; Coskun, O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: a randomized controlled trial. Clin. Rehabilitation 2010, 24, 240–250. [Google Scholar] [CrossRef]
| Parameters | CMEBE group (n = 15) | CPTBE group (n = 15) | t/x2 | p |
|---|---|---|---|---|
| Gender | ||||
| Male | 9 (60.0%) | 6 (40.0%) | 0.032 | 0.785 |
| Female | 6 (40.0%) | 9 (60.0%) | ||
| MAS | 0.826 | 0.421 | ||
| G0 | 6 (40.0%) | 6 (40.0%) | ||
| G1 | 5 (33.3%) | 6 (40.0%) | ||
| G1+ | 4 (26.7%) | 3 (20.0%) | ||
| Affected side | 0.248 | 0.211 | ||
| Right | 6 (40.0%) | 5 (33.3%) | ||
| Left | 9 (60.0%) | 10 (66.7%) | ||
| Diagnosis | 0.146 | 0.862 | ||
| Infarction | 7 (46.7%) | 4 (26.7%) | ||
| Haemorhage | 8 (53.3%) | 11 (73.3%) | ||
| Age (years) | 59.93 ± 12.48 | 55.21 ± 0.33 | 0.322 | 0.578 |
| Height (㎝) | 165.93 ± 7.48 | 162.13 ± 5.35 | 0.321 | 0.572 |
| Weight (kg) | 68.20 ± 6.88 | 60.93 ± 5.63 | 0.237 | 0.213 |
| MMSE-K | 27.13 ± 1.60 | 27.47 ± 1.46 | -0.851 | 0.251 |
| Parameters | CMEBE group (n = 15) | CPTBE group (n = 15) | t/x2 | p |
|---|---|---|---|---|
| Breathing function | ||||
| FVC ( ℓ ) | 1.88 ± 0.76 | 1.62 ± 0.51 | 0.652 | 0.416 |
| FEV1 ( ℓ ) | 2.94 ± 1.11 | 1.72 ± 0.39 | 1.231 | 0.122 |
| PEF ( ℓ ) | 2.56 ± 1.09 | 2.33 ± 0.91 | 0.326 | 0.562 |
| Trunk stability | ||||
| TIS (score) | 15.60 ± 3.32 | 16.02 ± 2.19 | -0.982 | 0.274 |
| Endurance | ||||
| 6-MWT (m) | 181.02 ± 20.89 | 179.00 ± 3.32 | -0.458 | 0.325 |
| Measures | CMEBE group (n = 15) | CPTBE group (n = 15) | t | p | ||||
|---|---|---|---|---|---|---|---|---|
| FVC (ℓ) | ||||||||
| pre | 1.88 | ± | 0.76 | 1.62 | ± | 0.51 | ||
| post | 2.64 | ± | 0.52 | 2.13 | ± | 0.66 | ||
| Change | 0.76 | ± | 0.24 | 0.51 | ± | 0.15 | 1.453 | 0.335 |
| t(p) | -3.172 (0.001**) | -2.518 (0.001**) | ||||||
| FEV1 (ℓ) | ||||||||
| pre | 2.94 | ± | 1.11 | 1.72 | ± | 0.39 | ||
| post | 3.24 | ± | 0.63 | 2.11 | ± | 0.32 | ||
| change | 1.11 | ± | 0.52 | 0.39 | ± | 0.07 | -0.521 | 0.042* |
| t (p) | -3.836 (0.001**) | -3.447(0.002**) | ||||||
| PEF (ℓ) | ||||||||
| pre | 2.56 | ± | 1.09 | 2.33 | ± | 0.91 | ||
| post | 3.65 | ± | 0.64 | 3.24 | ± | 0.76 | ||
| change | 1.09 | ± | 0.45 | 0.91 | ± | 0.15 | 1.325 | 0.219 |
| t (p) | -3.452 (0.002**) | -8.485 (0.001**) | ||||||
| Measures | CMEBE group (n = 15) | CPTBE group (n = 15) | t | p | ||||
|---|---|---|---|---|---|---|---|---|
| TIS (score) | ||||||||
| pre | 15.60 | ± | 3.32 | 16.02 | ± | 2.19 | ||
| post | 18.92 | ± | 2.31 | 18.21 | ± | 2.13 | ||
| Change | 3.32 | ± | 1.01 | 2.19 | ± | 0.06 | -2.414 | 0.017* |
| t (p) | -1.231 (0.013*) | -2.218 (0.011*) | ||||||
| Measures | CMEBE group (n = 15) | CPTBE group (n = 15) | t | p | ||||
|---|---|---|---|---|---|---|---|---|
| 6-MWT (m) | ||||||||
| pre | 181.02 | ± | 20.89 | 179.00 | ± | 3.32 | ||
| post | 202.00 | ± | 15.23 | 182.32 | ± | 2.12 | ||
| Change | 20.98 | ± | 5.66 | 3.32 | ± | 1.20 | 0.326 | 0.042* |
| t (p) | -7.536 (0.001**) | -9.018 (0.001**) | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





