Submitted:
13 October 2023
Posted:
16 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Aspects
2.3. Description of the Questionnaire
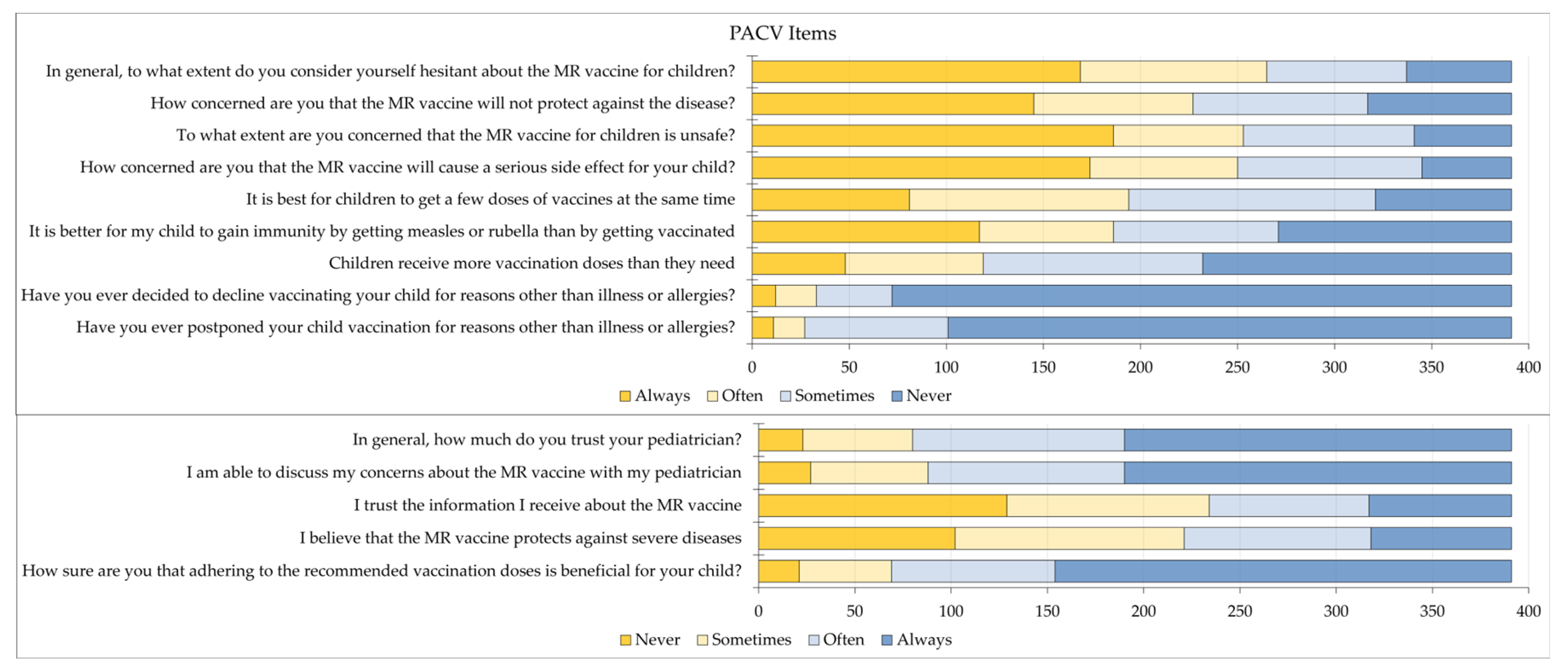
2.4. PACV Items
2.5. Data Analysis
3. Results
3.1. Study Sample
3.2. Parental MR Vaccination Hesitancy and its Associated Factors
3.3. Factors Associated with PACV Constructs
| Variable | Category | Behavior construct | Confidence in safety and efficacy construct | Trust construct | |||
|---|---|---|---|---|---|---|---|
| Mean±SD 3 | p | Mean±SD | p | Mean±SD | p | ||
| Age | < 40 years | 7.8±1.6 | .472 | 9.9±4.9 | .219 | 5.8±2.1 | .342 |
| ≥ 40 years | 7.6±1.8 | 9.3±4.8 | 5.6±2.2 | ||||
| Sex | Male | 7.7±1.8 | .718 | 10.1±5 | .203 | 5.7±2.2 | .879 |
| Female | 7.7±1.6 | 9.4±4.8 | 5.8±2.1 | ||||
| Offspring | 1 or 2 | 7.7±1.8 | .993 | 10.3±5.2 | .021 | 5.9±2.2 | .196 |
| 3 or more | 7.8±1.6 | 9.1±4.5 | 5.6±2.1 | ||||
| Educational level | High school or less | 7.7±1.8 | .014 | 9±4.8 | .343 | 5.7±2.1 | .690 |
| Undergraduate | 7.8±1.5 | 9.9±5 | 5.8±2.2 | ||||
| Postgraduate | 7.1±1.9 | 9.4±4.3 | 5.6±2.0 | ||||
| Governorate | Center | 7.9±1.6 | .066 | 9.8±4.9 | .534 | 5.9±2.1 | .005 |
| North | 7.5±1.8 | 9.5±4.8 | 5.2±2.0 | ||||
| South | 7.4±1.9 | 8.7±5.2 | 5.5±2.4 | ||||
| Occupation | Employed (HCW 1) | 7.9±1.5 | .647 | 10.3±5.0 | .481 | 5.7±2.0 | .490 |
| Employed (non-HCW) | 7.6±1.8 | 9.6±4.9 | 5.6±2.1 | ||||
| Unemployed | 7.8±1.6 | 9.4±4.8 | 5.8±2.2 | ||||
| History of chronic disease | Yes/not sure | 8.1±1.5 | .001 | 9.2±4.8 | .257 | 6.0±2.0 | .159 |
| No | 7.6±1.7 | 9.8±4.9 | 5.6±2.2 | ||||
| Health insurance | Yes | 7.7±1.7 | .079 | 9.9±4.8 | .041 | 5.6±2.1 | .045 |
| No | 8.0±1.5 | 8.6±4.9 | 6.2±2.1 | ||||
| Monthly income of household | ≤ 1000 JOD 2 | 7.8±1.6 | .150 | 9.5±4.9 | .485 | 5.8±2.2 | .206 |
| > 1000 JOD | 7.5±1.8 | 9.9±4.6 | 5.5±1.9 | ||||
| Previous parent vaccination history score | < 3 | 7.8±1.5 | .631 | 9.3±4.6 | .286 | 5.7±2.0 | .299 |
| ≥ 3 | 7.6±1.8 | 10.0±5.2 | 5.8±2.2 | ||||
| Previous child vaccination history score | < 4 | 7.8±1.8 | .059 | 9.4±4.9 | .271 | 5.9±2.1 | .162 |
| ≥ 4 | 7.7±1.5 | 9.9±4.9 | 5.6±2.2 | ||||
4. Discussion
4.1. Study Limitations
4.2. Recommendations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| aOR | Adjusted odds ratio |
| CI | Confidence interval |
| CNS | Central nervous system |
| COVID-19 | Coronavirus disease 2019 |
| EPI | The National Expanded Programme on Immunization |
| HCW | Health care worker |
| JOD | Jordanian dinar |
| MMR | Measles mumps rubella |
| MoH | Ministry of Health |
| MR | Measles Rubella |
| PACV | Parent Attitudes about Childhood Vaccines |
| VPD | Vaccine-preventable disease |
References
- Rota, P.A.; Moss, W.J.; Takeda, M.; de Swart, R.L.; Thompson, K.M.; Goodson, J.L. Measles. Nature Reviews Disease Primers 2016, 2, 16049. [Google Scholar] [CrossRef]
- Portnoy, A.; Jit, M.; Ferrari, M.; Hanson, M.; Brenzel, L.; Verguet, S. Estimates of case-fatality ratios of measles in low-income and middle-income countries: a systematic review and modelling analysis. Lancet Glob Health 2019, 7, e472–e481. [Google Scholar] [CrossRef]
- Sbarra, A.N.; Mosser, J.F.; Jit, M.; Ferrari, M.; Ramshaw, R.E.; O’Connor, P.; Krause, L.K.; Rogowski, E.L.B.; Portnoy, A. Estimating national-level measles case-fatality ratios in low-income and middle-income countries: an updated systematic review and modelling study. Lancet Glob Health 2023, 11, e516–e524. [Google Scholar] [CrossRef] [PubMed]
- Misin, A.; Antonello, R.M.; Di Bella, S.; Campisciano, G.; Zanotta, N.; Giacobbe, D.R.; Comar, M.; Luzzati, R. Measles: An Overview of a Re-Emerging Disease in Children and Immunocompromised Patients. Microorganisms 2020, 8, 276. [Google Scholar] [CrossRef]
- Leung, A.K.C.; Hon, K.L.; Leong, K.F. Rubella (German measles) revisited. Hong Kong Med J 2019, 25, 134–141. [Google Scholar] [CrossRef]
- Goodson, J.L.; Seward, J.F. Measles 50 Years After Use of Measles Vaccine. Infect Dis Clin North Am 2015, 29, 725–743. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Lee, A.D.; Clemmons, N.S.; Redd, S.B.; Poser, S.; Blog, D.; Zucker, J.R.; Leung, J.; Link-Gelles, R.; Pham, H.; et al. National Update on Measles Cases and Outbreaks - United States, January 1-October 1, 2019. MMWR Morb Mortal Wkly Rep 2019, 68, 893–896. [Google Scholar] [CrossRef]
- Durrheim, D.N.; Crowcroft, N.S.; Strebel, P.M. Measles - The epidemiology of elimination. Vaccine 2014, 32, 6880–6883. [Google Scholar] [CrossRef]
- Wang, R.; Jing, W.; Liu, M.; Liu, J. Trends of the Global, Regional, and National Incidence of Measles, Vaccine Coverage, and Risk Factors in 204 Countries From 1990 to 2019. Front Med (Lausanne) 2021, 8, 798031. [Google Scholar] [CrossRef] [PubMed]
- Marin, M.; Broder, K.R.; Temte, J.L.; Snider, D.E.; Seward, J.F. Use of combination measles, mumps, rubella, and varicella vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2010, 59, 1–12. [Google Scholar]
- Hayman, D.T.S. Measles vaccination in an increasingly immunized and developed world. Hum Vaccin Immunother 2019, 15, 28–33. [Google Scholar] [CrossRef]
- Pacenti, M.; Maione, N.; Lavezzo, E.; Franchin, E.; Dal Bello, F.; Gottardello, L.; Barzon, L. Measles Virus Infection and Immunity in a Suboptimal Vaccination Coverage Setting. Vaccines (Basel) 2019, 7, 199. [Google Scholar] [CrossRef]
- Muñoz-Alía, M.; Muller, C.P.; Russell, S.J. Antigenic Drift Defines a New D4 Subgenotype of Measles Virus. J Virol 2017, 91. [Google Scholar] [CrossRef]
- Guerra, F.M.; Bolotin, S.; Lim, G.; Heffernan, J.; Deeks, S.L.; Li, Y.; Crowcroft, N.S. The basic reproduction number (R(0)) of measles: a systematic review. Lancet Infect Dis 2017, 17, e420–e428. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Galvani, A.P. Exacerbation of measles mortality by vaccine hesitancy worldwide. Lancet Glob Health 2023, 11, e478–e479. [Google Scholar] [CrossRef] [PubMed]
- Wilder-Smith, A.B.; Qureshi, K. Resurgence of Measles in Europe: A Systematic Review on Parental Attitudes and Beliefs of Measles Vaccine. J Epidemiol Glob Health 2020, 10, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Novilla, M.L.B.; Goates, M.C.; Redelfs, A.H.; Quenzer, M.; Novilla, L.K.B.; Leffler, T.; Holt, C.A.; Doria, R.B.; Dang, M.T.; Hewitt, M.; et al. Why Parents Say No to Having Their Children Vaccinated against Measles: A Systematic Review of the Social Determinants of Parental Perceptions on MMR Vaccine Hesitancy. Vaccines (Basel) 2023, 11, 926. [Google Scholar] [CrossRef] [PubMed]
- Itiakorit, H.; Sathyamoorthi, A.; O’Brien, B.E.; Nguyen, D. COVID-19 Impact on Disparity in Childhood Immunization in Low- and Middle-Income Countries Through the Lens of Historical Pandemics. Curr Trop Med Rep 2022, 9, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Castrejon, M.M.; Leal, I.; de Jesus Pereira Pinto, T.; Guzmán-Holst, A. The impact of COVID-19 and catch-up strategies on routine childhood vaccine coverage trends in Latin America: A systematic literature review and database analysis. Hum Vaccin Immunother 2022, 18, 2102353. [Google Scholar] [CrossRef] [PubMed]
- Ho, L.L.; Gurung, S.; Mirza, I.; Nicolas, H.D.; Steulet, C.; Burman, A.L.; Danovaro-Holliday, M.C.; Sodha, S.V.; Kretsinger, K. Impact of the SARS-CoV-2 pandemic on vaccine-preventable disease campaigns. Int J Infect Dis 2022, 119, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Yunusa, A.; Cabral, C.; Anderson, E. The impact of the Covid-19 pandemic on the uptake of routine maternal and infant vaccines globally: A systematic review. PLOS Glob Public Health 2022, 2, e0000628. [Google Scholar] [CrossRef] [PubMed]
- Hamson, E.; Forbes, C.; Wittkopf, P.; Pandey, A.; Mendes, D.; Kowalik, J.; Czudek, C.; Mugwagwa, T. Impact of pandemics and disruptions to vaccination on infectious diseases epidemiology past and present. Hum Vaccin Immunother 2023, 19, 2219577. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Leave no one behind: guidance for planning and implementing catch-up vaccination. Available online: https://www.who.int/publications/i/item/9789240016514 (accessed on 12 October 2023).
- Allan, A.; UNICEF Jordan. Routine Childhood Immunizations. Available online: https://www.unicef.org/jordan/stories/routine-childhood-immunizations (accessed on 12 October 2023).
- Jordanian Ministry of Health. National vaccination programme. Available online: https://tinyurl.com/w37bmd2y (accessed on 12 October 2023).
- the World Health Organization Regional Office for the Eastern Mediterranean. Measles-rubella vaccine in Jordan is safe and effective at saving children’s lives – WHO and UNICEF. Available online: https://www.emro.who.int/jor/jordan-news/measles-rubella-vaccine-in-jordan-is-safe-and-effective-at-saving-childrens-lives-who-and-unicef.html (accessed on 1 October 2023).
- Roya News. Jordan’s Health Minister refutes false claims regarding MR vaccine. Available online: https://en.royanews.tv/news/44837/Jordan’s%20Health%20Minister%20refutes%20false%20claims%20regarding%20MR%20vaccine (accessed on 1 October 2023).
- Jordan News. Conflicting views on vaccines: MoH responds. Available online: https://www.jordannews.jo/Section-109/News/Conflicting-views-on-vaccines-MoH-responds-31125 (accessed on 7 October 2023).
- Abdaljaleel, M.; Barakat, M.; Mahafzah, A.; Hallit, R.; Hallit, S.; Sallam, M. TikTok Content on Measles-Rubella Vaccine in Jordan: A Cross-Sectional Study Highlighting the Spread of Vaccine Misinformation. JMIR Preprints 2023. [Google Scholar] [CrossRef]
- ElSayed, D.A.; Bou Raad, E.; Bekhit, S.A.; Sallam, M.; Ibrahim, N.M.; Soliman, S.; Abdullah, R.; Farag, S.; Ghazy, R.M. Validation and Cultural Adaptation of the Parent Attitudes about Childhood Vaccines (PACV) Questionnaire in Arabic Language Widely Spoken in a Region with a High Prevalence of COVID-19 Vaccine Hesitancy. Trop Med Infect Dis 2022, 7, 234. [Google Scholar] [CrossRef] [PubMed]
- Epitools. Sample size to estimate a proportion or apparent prevalence with specified precision. Available online: https://epitools.ausvet.com.au/oneproportion (accessed on 4 October 2023).
- Abu-Rish, E.Y.; Bustanji, Y.; Abusal, K. Nationwide Routine Childhood Vaccination Coverage During the COVID-19 Pandemic in Jordan: Current Situation, Reasons, and Predictors of Vaccination. Int J Clin Pract 2022, 2022, 7918604. [Google Scholar] [CrossRef] [PubMed]
- Roberton, T.; Weiss, W.; Doocy, S. Challenges in Estimating Vaccine Coverage in Refugee and Displaced Populations: Results From Household Surveys in Jordan and Lebanon. Vaccines (Basel) 2017, 5, 22. [Google Scholar] [CrossRef]
- Bakri, F.G.; Abdelrahim, Z.M.; Alkalbani, A.S.; Khrais, G.M.; Shamroukh, D.S.; Hayajneh, F.A.; Mahafza, A. Seroprevalence of measles, mumps, rubella, and varicella among physicians and nurses in Jordan. Turk J Med Sci 2016, 46, 614–619. [Google Scholar] [CrossRef]
- Bdour, S.; Batayneh, N. Present anti-measles immunity in Jordan. Vaccine 2001, 19, 3865–3869. [Google Scholar] [CrossRef]
- Uddin, M.J.; Adhikary, G.; Ali, M.W.; Ahmed, S.; Shamsuzzaman, M.; Odell, C.; Hashiguchi, L.; Lim, S.S.; Alam, N. Evaluation of impact of measles rubella campaign on vaccination coverage and routine immunization services in Bangladesh. BMC Infectious Diseases 2016, 16, 411. [Google Scholar] [CrossRef] [PubMed]
- Gastañaduy, P.A.; Banerjee, E.; DeBolt, C.; Bravo-Alcántara, P.; Samad, S.A.; Pastor, D.; Rota, P.A.; Patel, M.; Crowcroft, N.S.; Durrheim, D.N. Public health responses during measles outbreaks in elimination settings: Strategies and challenges. Hum Vaccin Immunother 2018, 14, 2222–2238. [Google Scholar] [CrossRef] [PubMed]
- Masadeh, M.M.; Alzoubi, K.H.; Al-Azzam, S.I.; Al-Agedi, H.S.; Abu Rashid, B.E.; Mukattash, T.L. Public awareness regarding children vaccination in Jordan. Hum Vaccin Immunother 2014, 10, 1762–1766. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines (Basel) 2021, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Taim, D.; Eid, H.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. COVID-19 misinformation: Mere harmless delusions or much more? A knowledge and attitude cross-sectional study among the general public residing in Jordan. PLoS One 2020, 15, e0243264. [Google Scholar] [CrossRef] [PubMed]
- Miras, A.P.; Regencia, Z.J.G.; Baja, E.S. ‘I was terrified for my child’: understanding the link between the Dengvaxia® controversy and the measles vaccine hesitancy in Pasay City, Philippines. Journal of Public Health 2023, fdad091. [Google Scholar] [CrossRef] [PubMed]
- Pian, W.; Chi, J.; Ma, F. The causes, impacts and countermeasures of COVID-19 “Infodemic”: A systematic review using narrative synthesis. Inf Process Manag 2021, 58, 102713. [Google Scholar] [CrossRef] [PubMed]
- van Mulukom, V.; Pummerer, L.J.; Alper, S.; Bai, H.; Čavojová, V.; Farias, J.; Kay, C.S.; Lazarevic, L.B.; Lobato, E.J.C.; Marinthe, G.; et al. Antecedents and consequences of COVID-19 conspiracy beliefs: A systematic review. Soc Sci Med 2022, 301, 114912. [Google Scholar] [CrossRef] [PubMed]
- Pertwee, E.; Simas, C.; Larson, H.J. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nature Medicine 2022, 28, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Skafle, I.; Nordahl-Hansen, A.; Quintana, D.S.; Wynn, R.; Gabarron, E. Misinformation About COVID-19 Vaccines on Social Media: Rapid Review. J Med Internet Res 2022, 24, e37367. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Al-Mahzoum, K.; Eid, H.; Assaf, A.M.; Abdaljaleel, M.; Al-Abbadi, M.; Mahafzah, A. Attitude towards HPV Vaccination and the Intention to Get Vaccinated among Female University Students in Health Schools in Jordan. Vaccines 2021, 9, 1432. [Google Scholar] [CrossRef]
- Sallam, M.; Ghazy, R.M.; Al-Salahat, K.; Al-Mahzoum, K.; AlHadidi, N.M.; Eid, H.; Kareem, N.; Al-Ajlouni, E.; Batarseh, R.; Ababneh, N.A.; et al. The Role of Psychological Factors and Vaccine Conspiracy Beliefs in Influenza Vaccine Hesitancy and Uptake among Jordanian Healthcare Workers during the COVID-19 Pandemic. Vaccines (Basel) 2022, 10, 1355. [Google Scholar] [CrossRef]
- Sallam, M.; Eid, H.; Awamleh, N.; Al-Tammemi, A.B.; Barakat, M.; Athamneh, R.Y.; Hallit, S.; Harapan, H.; Mahafzah, A. Conspiratorial Attitude of the General Public in Jordan towards Emerging Virus Infections: A Cross-Sectional Study Amid the 2022 Monkeypox Outbreak. Trop Med Infect Dis 2022, 7, 411. [Google Scholar] [CrossRef]
- Mahameed, H.; Al-Mahzoum, K.; AlRaie, L.A.; Aburumman, R.; Al-Naimat, H.; Alhiary, S.; Barakat, M.; Al-Tammemi, A.B.; Salim, N.A.; Sallam, M. Previous Vaccination History and Psychological Factors as Significant Predictors of Willingness to Receive Mpox Vaccination and a Favorable Attitude towards Compulsory Vaccination. Vaccines (Basel) 2023, 11, 897. [Google Scholar] [CrossRef]
- Zimmerman, T.; Shiroma, K.; Fleischmann, K.R.; Xie, B.; Jia, C.; Verma, N.; Lee, M.K. Misinformation and COVID-19 vaccine hesitancy. Vaccine 2023, 41, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.; Moore, A.C.; Sahm, L.J.; Fleming, A. Parent Attitudes about Childhood Vaccines: Point Prevalence Survey of Vaccine Hesitancy in an Irish Population. Pharmacy 2021, 9, 188. [Google Scholar] [CrossRef] [PubMed]
- Al-Regaiey, K.A.; Alshamry, W.S.; Alqarni, R.A.; Albarrak, M.K.; Alghoraiby, R.M.; Alkadi, D.Y.; Alhakeem, L.R.; Bashir, S.; Iqbal, M. Influence of social media on parents’ attitudes towards vaccine administration. Hum Vaccin Immunother 2022, 18, 1872340. [Google Scholar] [CrossRef] [PubMed]
- Sabahelzain, M.M.; Moukhyer, M.; Bosma, H.; van den Borne, B. Determinants of Measles Vaccine Hesitancy among Sudanese Parents in Khartoum State, Sudan: A Cross-Sectional Study. Vaccines 2022, 10, 6. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Obohwemu, K.; Christie-de Jong, F.; Ling, J. Parental childhood vaccine hesitancy and predicting uptake of vaccinations: a systematic review. Prim Health Care Res Dev 2022, 23, e68. [Google Scholar] [CrossRef] [PubMed]
- Jinarong, T.; Chootong, R.; Vichitkunakorn, P.; Songwathana, P. Muslim parents’ beliefs and factors influencing complete immunization of children aged 0–5 years in a Thai rural community: a qualitative study. BMC Public Health 2023, 23, 1348. [Google Scholar] [CrossRef]
- Rodrigues, F.; Block, S.; Sood, S. What Determines Vaccine Hesitancy: Recommendations from Childhood Vaccine Hesitancy to Address COVID-19 Vaccine Hesitancy. Vaccines (Basel) 2022, 10, 80. [Google Scholar] [CrossRef]
- Krishnendhu, V.K.; George, L.S. Drivers and barriers for measles rubella vaccination campaign: A qualitative study. J Family Med Prim Care 2019, 8, 881–885. [Google Scholar] [CrossRef]
- Cooper, S.; Schmidt, B.M.; Sambala, E.Z.; Swartz, A.; Colvin, C.J.; Leon, N.; Wiysonge, C.S. Factors that influence parents’ and informal caregivers’ views and practices regarding routine childhood vaccination: a qualitative evidence synthesis. Cochrane Database Syst Rev 2021, 10, Cd013265. [Google Scholar] [CrossRef] [PubMed]
- Nuwarda, R.F.; Ramzan, I.; Weekes, L.; Kayser, V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines (Basel) 2022, 10, 1595. [Google Scholar] [CrossRef] [PubMed]
- Biggs, A.T.; Littlejohn, L.F. Vaccination and natural immunity: Advantages and risks as a matter of public health policy. Lancet Reg Health Am 2022, 8, 100242. [Google Scholar] [CrossRef] [PubMed]
- Marin, M.; Fiebelkorn, A.P.; Bi, D.; Coleman, L.A.; Routh, J.; Curns, A.T.; McLean, H.Q. Adverse Events Among Young Adults Following a Third Dose of Measles-Mumps-Rubella Vaccine. Clinical Infectious Diseases 2021, 73, e1546–e1553. [Google Scholar] [CrossRef]
- Sharma, R.; Gaur, A. Adverse events associated with Measles and Rubella vaccination campaign 2019 in India. Clin Exp Vaccine Res 2021, 10, 44–46. [Google Scholar] [CrossRef]
- Ruggiero, K.M.; Wong, J.; Sweeney, C.F.; Avola, A.; Auger, A.; Macaluso, M.; Reidy, P. Parents’ Intentions to Vaccinate Their Children Against COVID-19. J Pediatr Health Care 2021, 35, 509–517. [Google Scholar] [CrossRef]
- Damnjanović, K.; Graeber, J.; Ilić, S.; Lam, W.Y.; Lep, Ž.; Morales, S.; Pulkkinen, T.; Vingerhoets, L. Parental Decision-Making on Childhood Vaccination. Front Psychol 2018, 9, 735. [Google Scholar] [CrossRef]
- Hurstak, E.E.; Paasche-Orlow, M.K.; Hahn, E.A.; Henault, L.E.; Taddeo, M.A.; Moreno, P.I.; Weaver, C.; Marquez, M.; Serrano, E.; Thomas, J.; et al. The mediating effect of health literacy on COVID-19 vaccine confidence among a diverse sample of urban adults in Boston and Chicago. Vaccine 2023, 41, 2562–2571. [Google Scholar] [CrossRef]
- von Lengerke, T.; Helmer, S.; Tomsic, I.; Pischke, C.R.; Wegwarth, O.; Kendel, F.; Härter, M. Education Level and Attitudes to Vaccination in the General Population: An Analysis of Representative Surveys Conducted by the German Federal Centre for Health Education, 2012 to 2018. Dtsch Arztebl Int 2021, 118, 96–97. [Google Scholar] [CrossRef]
- Napolitano, F.; Della Polla, G.; Capano, M.S.; Augimeri, M.; Angelillo, I.F. Vaccinations and Chronic Diseases: Knowledge, Attitudes, and Self-Reported Adherence among Patients in Italy. Vaccines (Basel) 2020, 8, 560. [Google Scholar] [CrossRef] [PubMed]
| Variable | Category | N 5 (%) |
|---|---|---|
| Age | < 40 years | 213 (54.5) |
| ≥ 40 years | 178 (45.5) | |
| Sex | Male | 118 (30.2) |
| Female | 273 (69.8) | |
| Offspring | 1 or 2 | 173 (44.2) |
| 3 or more | 218 (55.8) | |
| Educational level | High school or less | 97 (24.8) |
| Undergraduate | 245 (62.7) | |
| Postgraduate | 49 (12.5) | |
| Governorate | Center | 265 (67.8) |
| North | 98 (25.1) | |
| South | 28 (7.2) | |
| Occupation | Employed (HCW 3) | 52 (13.3) |
| Employed (non-HCW) | 171 (43.7) | |
| Unemployed | 168 (43.0) | |
| History of chronic disease | Yes/not sure | 104 (26.6) |
| No | 287 (73.4) | |
| Health insurance | Yes | 319 (81.6) |
| No | 72 (18.4) | |
| Monthly income of household | ≤ 1000 JOD 4 | 315 (80.6) |
| > 1000 JOD | 76 (19.4) | |
| Parental COVID-19 1 vaccine uptake | None/single dose | 62 (15.9) |
| Primary series | 259 (66.2) | |
| Booster doses | 70 (17.9) | |
| Parental influenza vaccine uptake | None | 230 (58.8) |
| Not sure | 45 (11.5) | |
| Yes | 116 (29.7) | |
| Uptake of Routine Childhood Immunizations | None | 12 (3.1) |
| Not sure | 8 (2.0) | |
| Yes | 371 (94.9) | |
| Uptake of non-Routine Childhood Immunizations | None | 325 (83.1) |
| Not sure | 16 (4.1) | |
| Yes | 50 (12.8) | |
| Child MR 2 vaccine uptake | None | 180 (46.0) |
| Not sure | 61 (15.6) | |
| Yes | 150 (38.4) |
| Variable | Category | MR 4 vaccine acceptance | p, χ2 | |
|---|---|---|---|---|
| Acceptance | Hesitancy/resistance | |||
| N 5 (%) | N (%) | |||
| Age | < 40 years | 34 (16.0) | 179 (84.0) | .177, 1.820 |
| ≥ 40 years | 20 (11.2) | 158 (88.8) | ||
| Sex | Male | 20 (16.9) | 98 (83.1) | .237, 1.398 |
| Female | 34 (12.5) | 239 (87.5) | ||
| Offspring | 1 or 2 | 34 (19.7) | 139 (80.3) | .003, 8.898 |
| 3 or more | 20 (9.2) | 198 (90.8) | ||
| Educational level | High school or less | 11 (11.3) | 86 (88.7) | .508, 1.353 |
| Undergraduate | 34 (13.9) | 211 (86.1) | ||
| Postgraduate | 9 (18.4) | 40 (81.6) | ||
| Governorate | Center | 41 (15.5) | 224 (84.5) | .385, 1.911 |
| North | 10 (10.2) | 88 (89.8) | ||
| South | 3 (10.7) | 25 (89.3) | ||
| Occupation | Employed (HCW 2) | 10 (19.2) | 42 (80.8) | .462, 1.544 |
| Employed (non-HCW) | 23 (13.5) | 148 (86.5) | ||
| Unemployed | 21 (12.5) | 147 (87.5) | ||
| History of chronic disease | Yes/not sure | 14 (13.5) | 90 (86.5) | .904, .015 |
| No | 40 (13.9) | 247 (86.1) | ||
| Health insurance | Yes | 47 (14.7) | 272 (85.3) | .266, 1.239 |
| No | 7 (9.7) | 65 (90.3) | ||
| Monthly income of household | ≤ 1000 JOD 3 | 44 (14.0) | 271 (86.0) | .854, .034 |
| > 1000 JOD | 10 (13.2) | 66 (86.8) | ||
| Previous parent vaccination history score | < 3 | 22 (10.4) | 190 (89.6) | .032, 4.586 |
| ≥ 3 | 32 (17.9) | 147 (82.1) | ||
| Previous child vaccination history score | < 4 | 25 (11.4) | 194 (88.6) | .121, 2.399 |
| ≥ 4 | 29 (16.9) | 143 (83.1) | ||
| PACV score 1 | ≤ 23 | 3 (1.5) | 200 (98.5) | <.001, 53.948 |
| > 23 | 51 (27.1) | 137 (72.9) | ||
| Behavior construct | ≤ 8 | 19 (9.0) | 193 (91.0) | .002, 9.145 |
| > 8 | 35 (19.6) | 144 (80.4) | ||
| Safety and efficacy construct | ≤ 10 | 4 (1.8) | 224 (98.2) | <.001, 66.786 |
| > 10 | 50 (30.7) | 113 (69.3) | ||
| Trust construct | ≤ 6 | 25 (10.0) | 225 (90.0) | .004, 8.458 |
| > 6 | 29 (20.6) | 112 (79.4) | ||
| Model | aOR (95% CI) 2 | p |
|---|---|---|
| MR 1 vaccine acceptance vs. MR vaccine hesitancy/rejection | ||
| Nagelkerke R2 = 0.392 | ||
| Age < 40 years | 1.27 (0.60–2.69) | .529 |
| Age ≥ 40 years | Ref. | |
| Offspring 1 or 2 | 2.10 (1.01–4.34) | .046 |
| Offspring 3 or more | Ref. | |
| Previous parent vaccination history score < 3 | 0.62 (0.31–1.23) | .174 |
| Previous parent vaccination history score ≥ 3 | Ref. | |
| Previous child vaccination history score < 4 | 0.51 (0.25–1.05) | .068 |
| Previous child vaccination history score ≥ 4 | Ref. | |
| Behavior construct score > 8 | 2.62 (1.30–5.30) | .007 |
| Behavior construct score ≤ 8 | Ref. | |
| Safety and efficacy construct score > 10 | 23.61 (8.14–68.4) | <.001 |
| Safety and efficacy construct score ≤ 10 | Ref. | |
| Trust construct score > 6 | 1.40 (0.69–2.86) | .350 |
| Trust construct score ≤ 6 | Ref. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





