1. Introduction
Cancellations of scheduled elective surgeries reduce the operating room efficiency, increase the anxiety of the patients to be operated on as well as their families, lead to ineffective use of human resources and surgical supplies, and adversely impact overall health-related quality measures [
1,
2]. Cancellations of scheduled elective surgeries also impose an extra financial burden on the healthcare system [
3]. The use of an organized multidisciplinary approach or a preoperative outpatient-based clinic has been found to be associated with reduced rates of elective surgery cancellations [
1].
Various reasons, such as inadequate preoperative assessment, patient-related factors, underlying chronic diseases, and administrative or organizational issues, have been put forward for canceling elective surgeries [
2,
4]. Identifying the factors that cause the cancellation of elective surgeries is important in determining the appropriate strategies for improving patient satisfaction, operating room resources, and perception of quality of care [
5]. It has been stated that most of the reasons given for elective surgery cancellations could be prevented or potentially avoided via early assessment and meticulous planning and coordination before the patients to be operated on were hospitalized [
1,
5,
6,
7].
The date an elective surgery is canceled varies between the day the patient is notified of the scheduled surgery date and the day the surgery is scheduled to be performed. Unexpected cancellation of a surgery as late as the day the surgery is scheduled to be performed or even after the patient to be operated on is taken to the operating room has a more significant negative impact on hospital resources than cancellation of the surgery before the date it is scheduled to be performed [
6,
8]. The emotional trauma experienced by patients and their families due to surgery cancellations is another negative result [
9,
10]. Cancellation of elective surgery after the patient is taken to the operating room causes extra emotional distress in patients, in addition to unnecessary costs and ineffective use of hospital resources [
11,
12].
There is limited data in the literature on the cancellation of elective surgeries once the patient is taken to the operating room. In this context, this study was carried out to determine the prevalence and causes of cancellations of elective surgeries once the patient is in the operating room and the clinical course of the patients subject to the surgery cancellation.
2. Materials and Methods
The population of this prospective, cross-sectional study consisted of adult patients scheduled to have elective surgery between January 2022 and January 2023 at a tertiary academic referral center and taken to the operating room. The study protocol was approved by the local ethical committee prior to the conduct of the study (Suleyman Demirel University Faculty of Medicine, Ethical Committee for Clinical Studies, 26.01.2022, 3/33). The study was carried out in accordance with the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from the patients.
The tertiary academic referral center, where the study was conducted is located in the Isparta Province in the Mediterranean Region of Turkey. According to 2022 statistics, the population of the province is 445,325. The center has 595 in-patient beds. A total of 34,658 medical and surgical patients were hospitalized at the center in 2022. The center has a total of 18 operating rooms used by different departments. The regular working hours of the operating rooms are 8 AM to 6 PM on weekdays except for public holidays.
Of the patients included in the study population, the patients who underwent emergency, obstetric, or minor elective surgeries that do not require filling out anesthesiology assessment sheets preoperatively and surgeries that were scheduled outside the official working days, i.e., Saturday and Sunday were excluded from the study. In addition, surgeries scheduled on the final operation list for that day or subsequently added to the operation list and canceled before the patients were taken to the operating room were also not evaluated within the scope of this study. Of the remaining patients, the patients whose surgeries were canceled by either the anesthetist or surgeon after the patient was taken to the operating room and before or after the induction of general anesthesia were included in Group 1, and the ones whose surgeries were completed were included in Group 2.
All patients scheduled to have surgery were assessed preoperatively by the attending physician based on the type of surgery to be had and the American Society of Anesthesiologists physical status class in the outpatient clinics of the Anesthesiology and Reanimation Department. The surgeries were scheduled depending on the results of the preoperative assessment.
The follow-up data of the patients subject to the surgery cancellation were obtained from the medical files of the patients available in the hospital or queried directly from the patients over the phone.
Patients’ demographic characteristics, i.e., age and gender; clinical characteristics, i.e., body mass index (BMI) and American Society of Anesthesiologists physical status class; and surgery details, i.e., the department where the surgery was performed/scheduled to be performed, and the month and the day the surgery was performed/scheduled to be performed were obtained from patients’ medical files and preoperative anesthesiology assessment sheets, and recorded. Comorbidities of patients subject to surgery cancellation, reasons for cancellation, and the clinical course of the patients subject to the cancellation during the 30 days after the cancellation were prospectively obtained and recorded into a structured worksheet designed for patients whose surgeries were canceled [
11,
12].
The reasons for cancellation were provided by the attending anesthesiologists or surgeons and categorized as potentially avoidable or unavoidable based on their opinions. The guidelines of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) were used to grade arterial hypertension [
13,
14]. Patients with systolic blood pressures≥180 mm Hg or diastolic blood pressures≥110 mm Hg were considered to have stage 3 or higher hypertension, and their surgeries were canceled. Potentially avoidable cancellations were those that could have been avoided if adequate preoperative assessment had been made or the hospital personnel had conducted the necessary communications before the scheduled date and time of the surgery. The definitions of potentially avoidable or unavoidable surgery cancellations were included in the structured worksheet for the attending anesthesiologists or surgeons who are to fill out the worksheet to read.
The prevalence of elective surgery cancellations after the patient is taken to the operating room was determined as the study’s primary outcome. The study's secondary outcomes included the factors potentially contributing to the elective surgery cancellations, such as the department where the surgery was performed/scheduled to be performed, and the month and the day the surgery was performed/scheduled to be performed. In order to ensure the integrity and validity of the study's findings, statistical analyses were performed using Jamovi project 2.3.28 (Jamovi, version 2.3.28, 2023, retrieved from
https://www.jamovi.org) and JASP 0.17.3.0 (Jeffreys’ Amazing Statistics Program, version 0.17.3.0, 2023, retrieved from
https://jasp-stats.org) software packages, which are recognized for their robust statistical capabilities.
Prior to conducting any inferential statistical tests, the normal distribution characteristics of continuous variables were rigorously analyzed using Shapiro-Wilk, Kolmogorov-Smirnov, and Anderson-Darling tests. This step was pivotal in determining the statistical tests for subsequent analyses. The Mann-Whitney U test, known for its non-parametric nature and efficacy in comparing medians, was used to compare the variables not conforming to a normal distribution.
Categorical variables, such as the department where the surgery was performed/scheduled to be performed, and the month and the day the surgery was performed/scheduled to be performed, were analyzed using Pearson’s chi-square test, a test used as a standard in medical research for comparing proportions among independent groups. The Fisher-Freeman-Halton test was used in tables with more cells than in a 2x2 table. Probability (p) statistics of ≤ 0.05 were deemed to indicate statistical significance, in line with conventional standards in medical research to minimize Type I errors.
3. Results
The study sample consisted of 7482 patients. Of these patients, 67 whose surgeries were canceled were included in Group 1. Accordingly, the prevalence of cancellations of elective surgeries once the patient is in the operating room was 0.9%. The remaining 7415 patients were included in Group 2.
The distribution of the patients’ demographic and clinical characteristics by the patient groups is shown in
Table 1. Group 1 was significantly older than Group 2 (p<0.001). There was no significant difference between the groups in median BMI values (p=0.523). On the other hand, the number of patients categorized as American Society of Anesthesiologists physical status class III was significantly higher in Group 1 than in Group 2 (p<0.001). In parallel, the number of patients with American Society of Anesthesiologists physical status class 1 was significantly higher in Group 2 than in Group 1 (
Table 1).
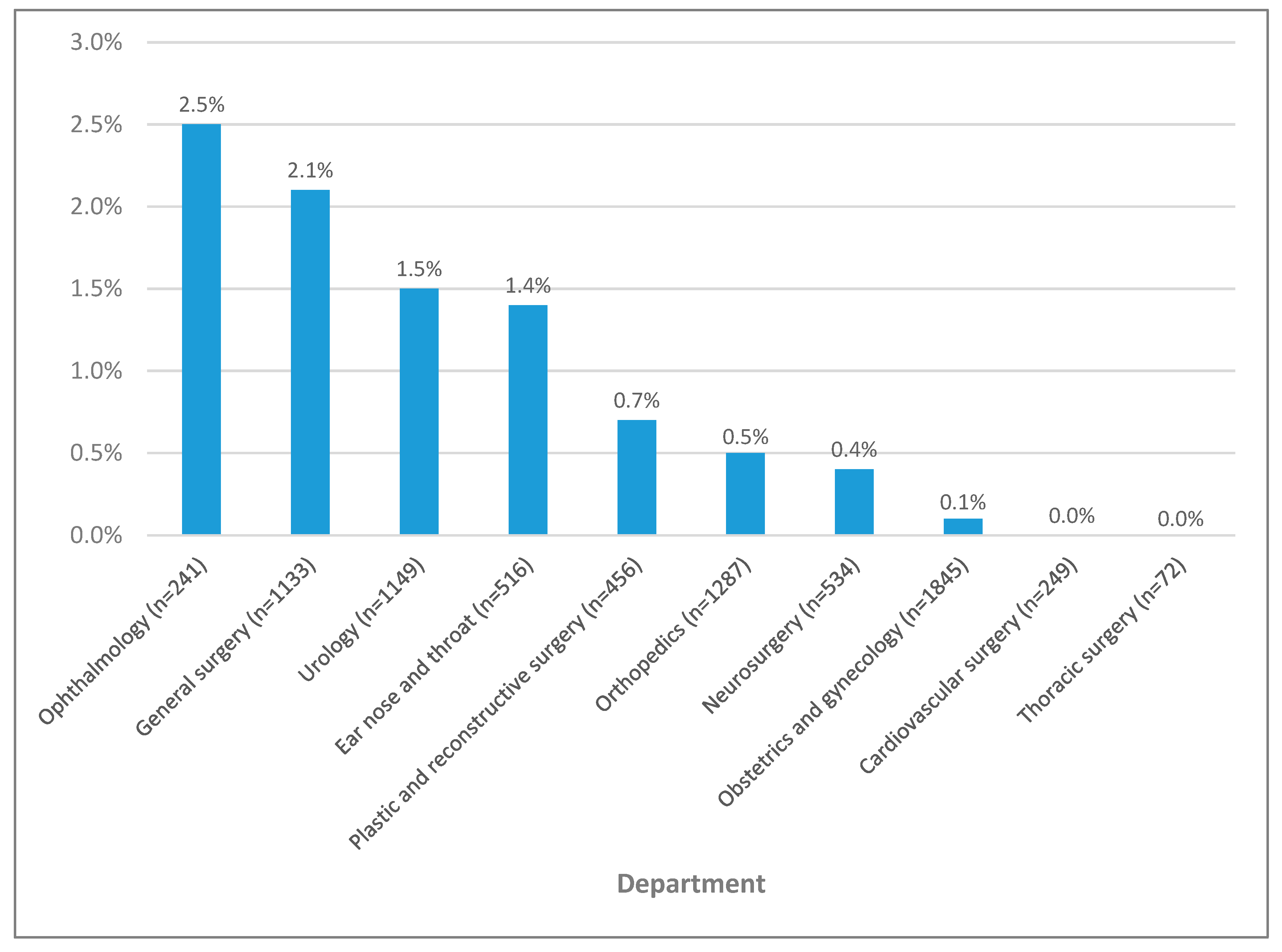
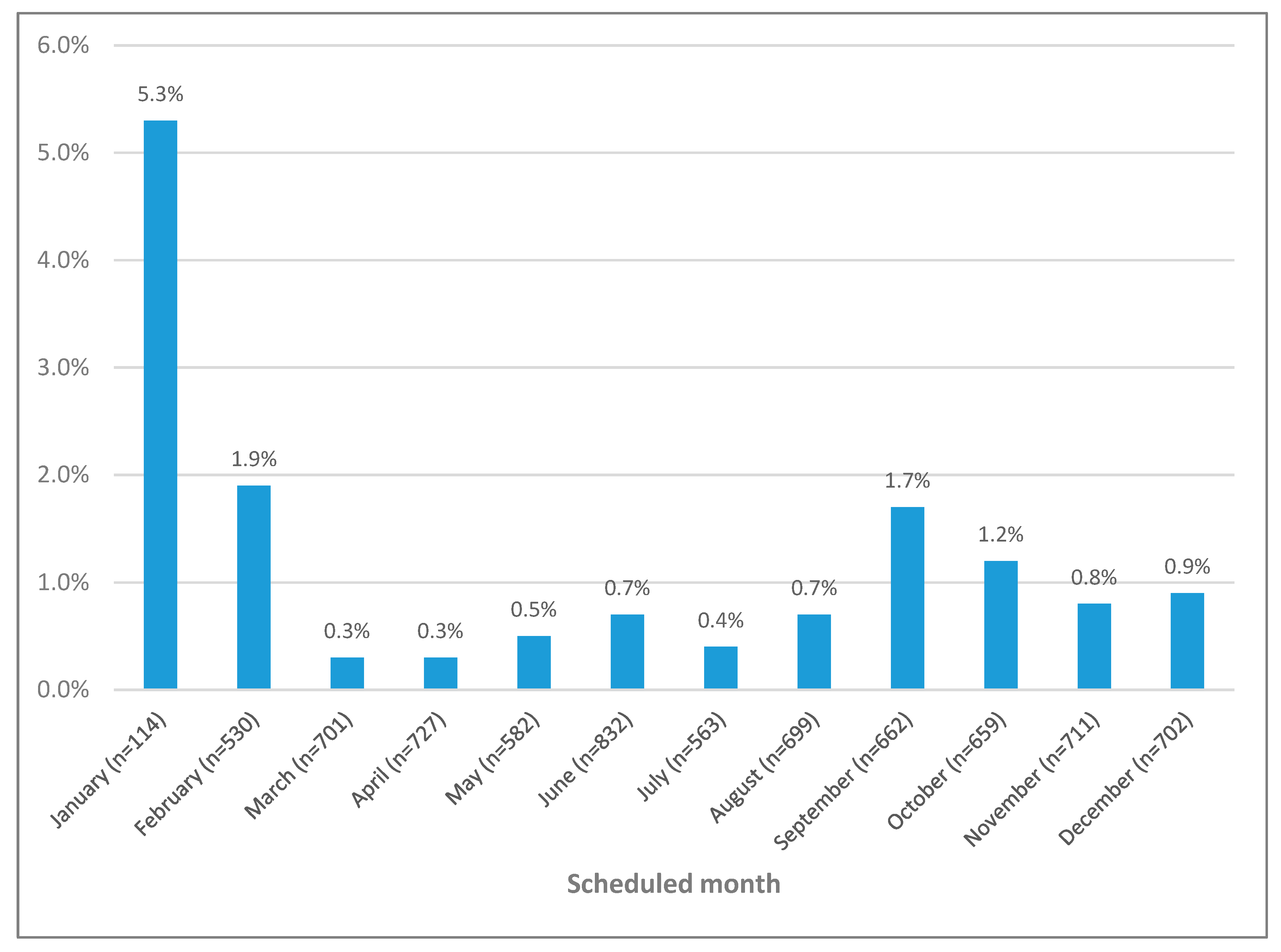
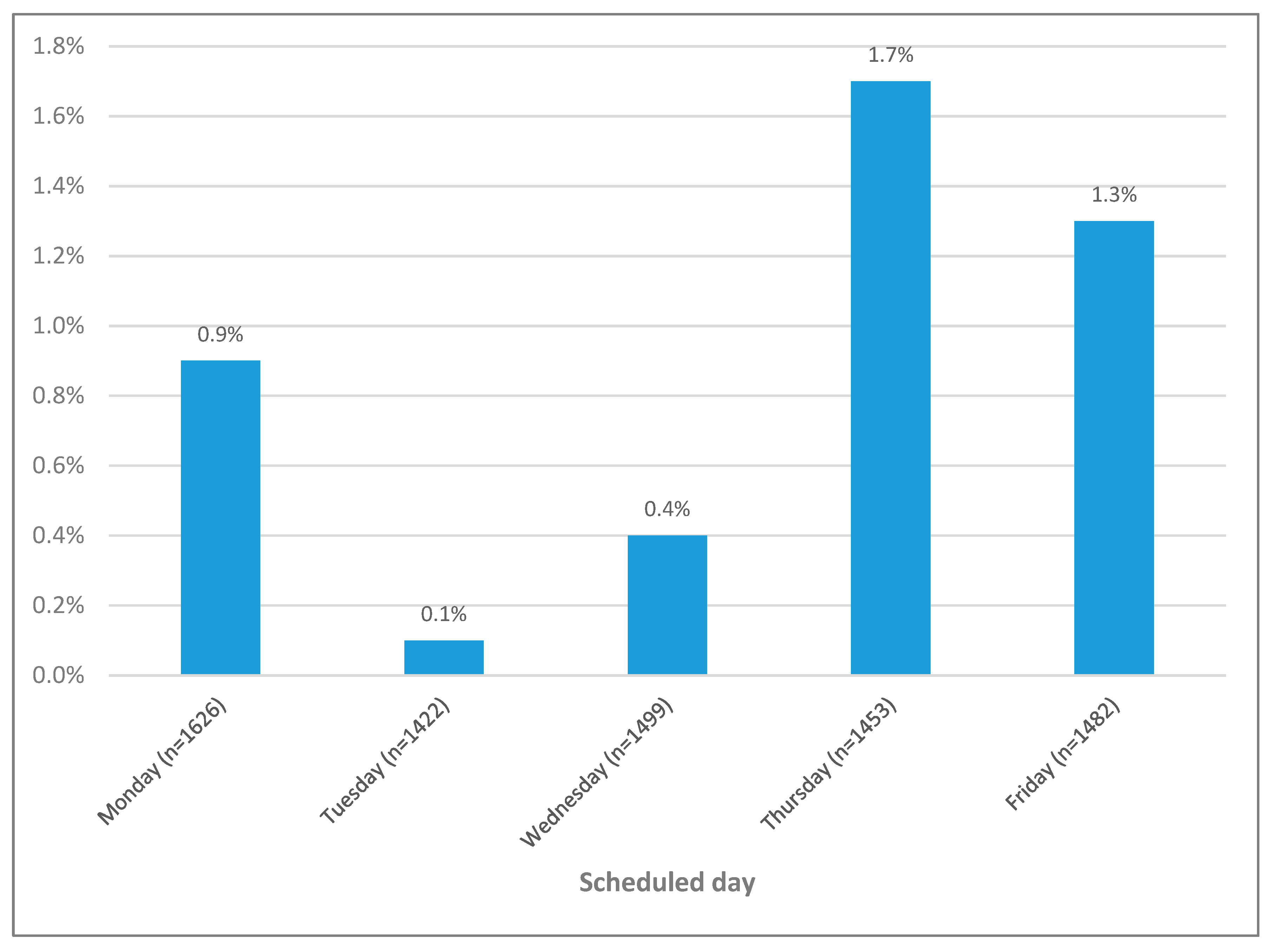
There were also significant differences between the groups in terms of the department where the surgery was performed/scheduled to be performed, and the month and the day the surgery was performed/scheduled to be performed(p<0.05) (
Table 2). The department with the highest cancellation rate of elective surgeries was ophthalmology (2.5%), followed by general surgery (2.1%), urology (1.5%), and ear, nose and throat (1.4%) (
Figure 1). The month with the highest cancellation rate of elective surgeries was January (5.3%), followed by February (1.9%) and September (1.7%) (
Figure 2). In terms of the days when the elective surgeries were canceled, the cancellation rates of elective surgeries scheduled for Tuesday and Wednesday were lower than those scheduled for other days of the week (
Figure 3).
The reasons for elective surgery cancellations are given in
Table 3. Stage 3 or 4 hypertension (46.3%) and smoking on the day of the scheduled surgery (26.9%) were the most frequently cited reasons for elective surgery cancellations. Of the causes given for the cancellations of elective surgeries, 59.7% were evaluated as potentially avoidable causes.
As for the clinical course of the patients subject to the cancellation during the 30 days after the cancellation, 53 (79.0%) patients underwent surgery after the cancellation of the surgery. Most (98.1%) of these surgeries were performed in the same hospital.
4. Discussion
The study findings show that less than one percent of the elective surgeries were canceled once the patients were taken to the operating room. The elective surgery cancellation rates were found to be higher in ophthalmology, general surgery, urology, and ear, nose, and throat departments than in others. However, a preliminary analysis of the factors impacting elective surgery cancellations indicated the necessity for a detailed analysis. More than half the reasons given for elective surgery cancellations were categorized as potentially avoidable factors. Most of these factors were associated with patients’ medical conditions. In this context, increasing the awareness of the patients for surgery, improving the communication between patient and physician as well as between patient and hospital administration, and preoperatively assessing the patients for elective surgeries are likely to reduce elective surgery cancellation rates.
There are only a few studies in the literature on elective surgery cancellations after the patients are taken to the operating room. In two of these studies with seven- and eight-year study periods, surgery cancellation rates after the patients were taken to the operating room were reported as <0.01% and 0.21%, respectively [
11,
12]. In comparison, in this study, which had a one-year study period, the prevalence of cancellations of elective surgeries once the patient is in the operating room was determined as 0.9%. There were also significant methodological differences between this study and the said two studies. Hori et al. [
11] evaluated 30 patients whose surgeries were canceled after they were taken to the operating room and prepared for general anesthesia. Eighteen of these patients had their surgeries canceled before the induction of general anesthesia, and 12 after the induction of general anesthesia. The primary reasons given for the cancellations after the induction of general anesthesia were anaphylactic shock (n=3) and arrhythmias (n=4). In Perroca et al.’s study [
15], surgery cancellations were stratified according to whether they occurred before the preparation and arrangement of the operating room or after the operating room was prepared and anesthetic-surgical procedures were started. In comparison, in this study, the surgery cancellations were not stratified as such.
Hori et al. [
11] and Chang et al. [
12] reported the surgery cancellation rates after the induction of general anesthesia as 40% and 12.7%, respectively. In comparison, in this study, none of the 67 surgery cancellations were made after the induction of general anesthesia. Surgery cancellations after initiating general anesthesia are rare and primarily made due to unexpected and unpredicted changes in the patient’s clinical condition [
11,
12,
15].
Fitzsimons et al. [
16] investigated 43 cardiac surgery cancellations made after the patients were taken to the operating room and before the initiation of surgical incisions. These 43 surgery cancellations constituted 0.84% of all surgeries conducted during the four-year study period. Similar surgery cancellation rates have been reported in other studies [
17,
18]. The findings of these studies have not been compared with those of the said studies that specifically addressed cardiac surgery cancellations due to technical differences specific to heart surgeries.
Stratifying the reasons for surgery cancellations as potentially avoidable or unavoidable may not be considered a precise method [
3,
7,
12]. As a matter of fact, while Hori et al. [
11] categorized 36.7% of the reasons given for surgery cancellations before the induction of general anesthesia as potentially avoidable, stating that they could have been prevented by improving the preoperative assessment of the patients in terms of their medical problems, 59.7% of the reasons given for surgery cancellations before the induction of general anesthesia in this study were categorized as potentially avoidable. In different studies, the rate of potentially avoidable reasons among the reasons given for elective surgery cancellations before the induction of general anesthesia has been estimated between 60 to 70% [
3,
7,
15]. It is not an easy task to compare these studies due to the heterogeneities in patient groups and methodologies. However, detailed preoperative assessment of the patients stands out as the most effective measure to prevent surgery cancellations [
11].
Previous studies grouped the causes of surgery cancellations as patient-related, facility-related, and surgery-related [
2,
3,
4,
5,
7,
19,
20]. The characteristics of the patients, hospital facilities, the medical and administrative staff, and the socioeconomic status of the patient populations have been cited as the primary components of patient-related, facility-related, and surgery-related causes resulting in surgery cancellations [
21]. We did not use such stratifications due to the narrower focus of the study addressing only the cancellations made once the patient was taken to the operating room. Becker et al. [
22] investigated the non-medical risk factors that lead to postponing elective surgeries. They found that advanced age, retirement, and nursing home residence were the risk factors for surgery cancellation and rescheduling. Along these lines, in this study, the patients whose surgeries were canceled were significantly older, and a higher number of patients whose surgeries were canceled were categorized as American Society of Anesthesiologists physical status class III compared to the patients whose surgeries were completed as scheduled. Even though the patients whose surgeries were canceled were significantly older than those whose surgeries were completed as scheduled, the fact that their median age was below 65 may be a confounding factor. We did not separately investigate the impact of each demographic and clinical characteristic on cancellation rates. Nevertheless, we detected that the reasons for surgery cancellations were mainly related to the patients’ medical conditions and may thus be considered patient-related reasons.
The study's prospective design was its primary strength since it allowed a more accurate data collection process. This study did not address the cancellations made before the patients were taken to the operating room. Thus, the study's single-center design, along with the fact that only the cancellations made after the patients were taken to the operating room were taken into consideration, may limit the generalizability of this study’s findings to other settings. In addition, the significance level of the statistical analyses conducted according to the department where the surgery was performed/scheduled to be performed, and the month and the day the surgery was performed/scheduled to be performed may be questioned due to the smaller sizes of each subgroup. Lastly, we had difficulty explaining the unexpectedly higher surgery cancellation rates observed in January, which is likely associated with administrative issues.
5. Conclusions
The prevalence of elective surgery cancellations after the patients were taken to the operating room was less than one percent (0.9%). Most surgery cancellations were related to patients’ medical conditions and lack of surgery awareness. More than half of the reasons given for surgery cancellations were categorized as potentially avoidable. Therefore, improving the surgery awareness of the patients, establishing effective communication with the patients, and preoperatively assessing patients for elective surgical procedures are likely to reduce elective surgery cancellation rates after the patients are taken to the operating room.This section is not mandatory but can be added to the manuscript if the discussion is unusually long or complex.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization: M.S.Ö. and F.A.S., Methodology: M.S.Ö. and F.A.S., Software: Y.A., Validation: M.S.Ö., P.K, Formal Analysis: A.K., Investigation: M.S.Ö. and E.S.Ö., Resources: M.S.Ö. and E.S.Ö., Data Curation: Y.A. and P.K., Writing – Original Draft Preparation: M.S.Ö. and Y.A, Writing – Review & Editing: M.S.Ö., F.A.S., and P.K., Visualization: Y.A., Supervision: M.S.Ö. and P.K., Project Administration: M.S.Ö., Funding Acquisition: Not applicable (As per the provided information, there is no external funding).
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol was approved by the local ethical committee prior to the conduct of the study (Suleyman Demirel University Faculty of Medicine, Ethical Committee for Clinical Studies, 26.01.2022, 3/33). The study was carried out in accordance with the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from the patients.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We extend our deepest gratitude to Mr. Gökhan Karakoç and the Model Statistic Center for their expertise and support in the biostatistical analysis and reporting of this study (
www.modelistatistik.com).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Umeno, Y.; Ishikawa, S.; Kudoh, O.; Hayashida, M. Effects of the Multidisciplinary Preoperative Clinic on the Incidence of Elective Surgery Cancellation. J. Med Syst. 2022, 46, 1–8. [Google Scholar] [CrossRef]
- Wongtangman, K.; Azimaraghi, O.; Freda, J.; Ganz-Lord, F.; Shamamian, P.; Bastien, A.; Mirhaji, P.; Himes, C.P.; Rupp, S.; Green-Lorenzen, S.; et al. Incidence and predictors of case cancellation within 24 h in patients scheduled for elective surgical procedures. J. Clin. Anesthesia 2022, 83, 110987. [Google Scholar] [CrossRef]
- Sukwana, A.; Mrara, B.; Oladimeji, O. Prevalence and Causes of Elective Surgical Cancellations: Findings from a Rural Tertiary Hospital in the Eastern Cape, South Africa. Healthcare 2023, 11, 270. [Google Scholar] [CrossRef]
- Altun, A.Y.; Özer, A.B.; Aksoku, B.T.; Karatepe. ; Kilinç, M.; Erhan,.L.; Demirel, I.; Bolat, E. Evaluation of the Reasons for the Cancellation of Elective Procedures at Level 3 University Hospital on the Day of Surgery. J. PeriAnesthesia Nurs. 2020, 35, 514–517. [Google Scholar] [CrossRef]
- Feleke, M.G.; Chichiabellu, T.Y.; Ayalew, T.L. Magnitude and reasons of surgery cancellation among elective surgical cases in Wolaita Sodo University Comprehensive Specialized Hospital, Southern Ethiopia, 2021. BMC Surg. 2022, 22, 30. [Google Scholar] [CrossRef]
- Naik, S.V.; Dhulkhed, V.K.; Shinde, R.H. A prospective study on operation theater utilization time and most common causes of delays and cancellations of scheduled surgeries in a 1000-bedded tertiary care rural hospital with a view to optimize the utilization of operation theater. Anesthesia: Essays Res. 2018, 12, 797–802. [Google Scholar] [CrossRef]
- Kaddoum, R.; Fadlallah, R.; Hitti, E.; El-Jardali, F.; El Eid, G. Causes of cancellations on the day of surgery at a Tertiary Teaching Hospital. BMC Heal. Serv. Res. 2016, 16, 259. [Google Scholar] [CrossRef]
- McKendrick, D.R.A.; Cumming, G.P.; Lee, A.J. A 5-year observational study of cancellations in the operating room: Does the introduction of preoperative preparation have an impact? Saudi J. Anaesth. 2014, 8, 8–S14. [Google Scholar] [CrossRef]
- Viftrup, A.; Dreyer, P.; Nikolajsen, L.; Holm, A. Surgery cancellation: A scoping review of patients' experiences. J. Clin. Nurs. 2021, 30, 357–371. [Google Scholar] [CrossRef]
- Scheenstra, B.; A Princée, A.M.; Imkamp, M.S.V.; Kietselaer, B.; Ganushchak, Y.M.; Hof, A.W.J.V.; Maessen, J.G. Last-minute cancellation of adult patients scheduled for cardiothoracic surgery in a large Dutch tertiary care centre. Eur. J. Cardio-Thoracic Surg. 2021, 61, 225–232. [Google Scholar] [CrossRef]
- Hori, Y.; Nakayama, A.; Sakamoto, A. Surgery cancellations after entering the operating room. JA Clin. Rep. 2016, 2, 40. [Google Scholar] [CrossRef]
- Chang, J.-H.; Chen, K.-W.; Chen, K.-B.; Poon, K.-S.; Liu, S.-K. Case review analysis of operating room decisions to cancel surgery. BMC Surg. 2014, 14, 47. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef]
- Misra, S. Systemic hypertension and non-cardiac surgery. Indian J. Anaesth. 2017, 61, 697–704. [Google Scholar] [CrossRef]
- Perroca, M.G.; Jericó, M.d.C.; Facundin, S.D. Surgery cancelling at a teaching hospital: implications for cost management. Rev. Latino-Americana de Enferm. 2007, 15, 1018–1024. [Google Scholar] [CrossRef]
- Fitzsimons, M.G.; Dilley, J.D.; Moser, C.; Walker, J.D. Analysis of 43 Intraoperative Cardiac Surgery Case Cancellations. J. Cardiothorac. Vasc. Anesthesia 2016, 30, 19–22. [Google Scholar] [CrossRef]
- Lau, H.-K.; Chen, T.-H.; Liou, C.-M.; Chou, M.-C.; Hung, W.-T. Retrospective analysis of surgery postponed or cancelled in the operating room. J. Clin. Anesthesia 2010, 22, 237–240. [Google Scholar] [CrossRef]
- Farasatkish R, Aghdaii N, Azarfarin R, Yazdanian F. Can preoperative anesthesia consultation clinic help to reduce operating room cancellation rate of cardiac surgery on the day of surgery? Middle East J Anaesthesiol 2009, 20, 93–96. [Google Scholar]
- Denis, A.; Montreuil, J.; Harvey, E.J.; Berry, G.K.; Reindl, R.; Bernstein, M. Cancellations and delays of emergent orthopedic operations at a Canadian level 1 trauma centre. Can. J. Surg. 2022, 65, E382–E387. [Google Scholar] [CrossRef]
- Desta, M.; Manaye, A.; Tefera, A.; Worku, A.; Wale, A.; Mebrat, A.; Gobena, N. Incidence and causes of cancellations of elective operation on the intended day of surgery at a tertiary referral academic medical center in Ethiopia. Patient Saf. Surg. 2018, 12, 25. [Google Scholar] [CrossRef]
- Tewfik, G.L.; Rodriguez-Aponte, C.; Zhang, K.; Ezzat, B.; Suri, P.; Chaudhry, F. Outcomes and Disposition of Patients After Case Cancellation on Day of Surgery for Reasons Attributed to Medical or Anesthetic Care: A Retrospective Cohort Analysis. Obstet. Anesthesia Dig. 2022, 135, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.; Huschak, G.; Petzold, H.-C.; Thieme, V.; Stehr, S.; Bercker, S. Non-medical risk factors associated with postponing elective surgery: a prospective observational study. BMC Med Ethic- 2021, 22, 90. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).