1. Introduction
Pseudoaneurysm of the middle meningeal artery (MMA) after trauma is an uncommon entity. The most common clinical manifestation of traumatic pseudoaneurysm in MMA is an epidural hematoma (EDH). In 1957, Schulze, reported the firstcase of traumatic pseudoaneurysm in the MMA presenting with EDH [
1]. Intracerebral hemorrhage (ICH) with subdural hematoma (SDH) is an extremely rare presentation [
2,
3,
4,
5,
6,
7,
8]. The mechanism of acute and delayed ICH development due to the rupture of MMA pseudoaneurysms is not well understood. Inappropriate craniotomy might result in a failure to identify pseudoaneurysms, and intraoperative rupture of a pseudoaneurysm might also cause a difficult operation. Here, we discuss the pathophysiological mechanisms of acute and delayed ICH due to rupture of atraumatic MMA pseudoaneurysm. We also suggest pitfalls of surgical treatment, especially in regard to the extent of craniotomy and the timing of intraoperative rupture of pseudoaneurysm.
2. Mechanism of acute and delayed ICH due to rupture of MMA pseudoaneurysm
At the point where the MMA enters the cranial cavity, its histologic appearancechanges to that of a cerebral artery. Defects in the media are extremely common [
9], and these structural characteristics may influence the susceptibility of meningeal arteries to aneurysmal formation after trauma [
10]. Rupture of a pseudoaneurysm in the MMA after trauma commonly leads to EDH. Salazar et al., reported a pulsating round dilation of the MMA attached to the outer surface of the dura mater [
11]. Other researchers described a pseudoaneurysm in the MMA after trauma leading to EDH that was located on the outer dura layer [
1,
12,
13,
14,
15]. Uncommonly, these may result in SDH or ICH. However, the exact mechanism of ICH development after rupture of MMA pseudoaneurysm remains poorly understood.
2.1. Acute ICH development
Rumbaugh et al., suggested that SDH or ICH may result from the rupture of a pseudoaneurysm in the MMA, particularly if the dura has been torn; however, they did not present a case of dura tear resulting in ICH [
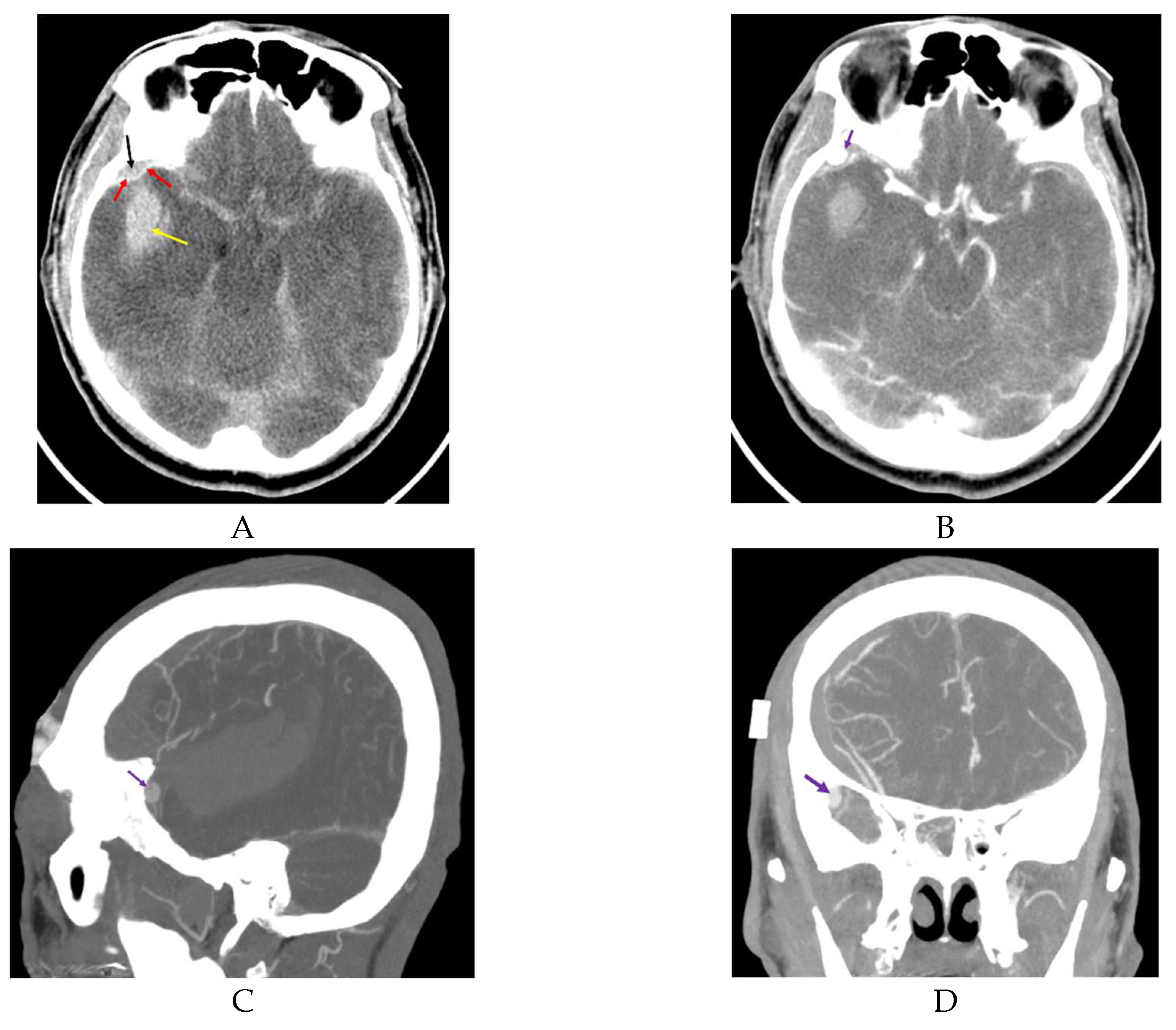
16]. Kumar et al., and Moon et al., reported cases with acute small EDH and ICH from rupture of a pseudoaneurysm in the MMA after trauma [
6,
7] (
Figure 1).
In both reports, the authors mentioned that brisk epidural bleeding during bone flap removal and dura tear were detected. Moon et al., proposed that a rupture of a pseudoaneurysm rupture in the MMA contacting with a dural defect could cause ICH via the dura tear [
6] (
Figure 2).
Figure 1 and
Figure 2 demonstrate that rupture of a pseudoaneurysm in the MMA with a dura tear results in small EDH and acute ICH. In situations where there is a dura tear, rupture of a pseudoaneurysm located in the epidural space produces EDH at the initial stage of the rupture and subsequently results in ICH via the dura tear.
Lim et al., reported that an irregular-shaped pseudoaneurysm arising from the MMA on the inner surface of the intact dura was observed during an operation performed on the second day after trauma [
8]. In that case, active bleeding from the pseudoaneurysm was observed; however, the mechanism underlying acute ICH was unclear. Intact dura mater was observed during the operation. An alternative explanation is that the MMA was exposed in the intradural space without the cover of the dural border cell layer [
17]. Damage to the MMA exposed in the intradural space might result in ICH. However, we could not confirm this hypothesis because the location of the MMA was not disclosed.
2.2. Delayed ICH development
The dura mater has three distinct layers. The outer layer is the thinnest layer, at 2 μm thick, whereas the inner layer is 8 μm thick and adhered to the arachnoid trabeculae. The middle vascular layer, within which the MMA runs, varies in thickness [
18]. In other brain operations, the operator may observe the MMA on the outer surface of the dura, but may not identify the groove of the MMA in the inner surface of the dura mater. In the middle cranial fossa, clinicians may observe vascular marking, as seen in
Figure 3.
Some investigators have suggested that in cases of delayed ICH, the continuous pressure of the pseudoaneurysm thins the inner layer of the dura mater and consequently causes SDH or ICH [
10,
18]. Pseudoaneurysm of the MMA in cases with delayed ICH has been shown to be attached to the inner surfaceof the dura mater [
3,
4,
5,
19,
20]. It is thought that a pseudoaneurysm develops after a small tear in the MMA, which is sealed off by a clot, later recanalizingand forming a false lumen. The suspicion of a traumatic pseudoaneurysm in the MMA should be considered in patients who show delayed and abrupt neurological deterioration because of ICH after trauma [
3]. In most reported casesof delayed ICH due to a pseudoaneurysm in the MMA, the usual delay between trauma and abrupt neurological deterioration varies from 3 to 30 days [
21]. Even so, at 11 months after trauma, delayed ICH from a pseudoaneurysm in the MMA could develop [
3]. Sometimes, neither families nor patients recognize previous head trauma [
22].
3. Preoperative diagnosis of pseudoaneurysm
3.1. Suspicion of pseudoaneurysm
Although its incidence is rare, the concurrence of head trauma, skull fracture located in the temporal area, and delayed neurological deterioration suggests the presence of a MMA pseudoaneurysm. About 70% of cases of pseudoaneurysm in the MMA after trauma are associated with a fracture crossing the MMA in the temporal region [
23]. De Andrade et al., suggested that as manyas 30% of patients with EDH and fracture crossing the groove for the MMA may have pseudoaneurysms [
24].
The first extracranial segment of the MMA is from its origin to its entry into the foramen spinosum. At the level of the foramen spinosum, the artery bends anteriorly and laterally to follow the temporal fossa. After its entry into the cranial cavity, the MMA follows a lateral course grooving the greater sphenoid wing. The intracranial segment of the MMA is divided into three portions. The first is the temporobasal segment, where the artery follows the temporal fossa and curves upward, becoming the second or temporopterional segment. After passing the pterional region, the artery enters in the coronal segment where it follows the coronal suture to end at the region of the bregma [
25].
3.2. Acute ICH following rupture of pseudoaneurysm
In preoperative diagnoses, acute ICH originating from an MMA pseudoaneurysm gives rise to the suspicion of a spontaneously ruptured cerebral aneurysm that might have caused the patient’s trauma [
26]. If acute ICH following trauma is in contact with the dura mater, clinicians should perform computed tomography (CT) angiography to detect pseudoaneurysm. Paiva et al., and Marvin et al., reported that CT angiography detected pseudoaneurysm in the MMA [
18,
27]. Moon et al., and Kumar et al., identified the presence of a small EDH in contact with a large ICH due to rupture of pseudoaneurysm in the MMA [
6,
7]. From the mechanism of development of acute ICH following rupture of an MMA pseudoaneurysm, we can expect that intense contrast enhancement of the lesion adjacent to the EDH might indicate a pseudoaneurysm in the MMA.
3.3. Delayed ICH due to rupture of pseudoaneurysm
Delayed ICH due to bleeding of a pseudoaneurysm in the MMA develops from 3 days to 11 months after trauma [
2,
3,
4,
5,
19,
20,
28], and in some patients, an unknown time since the trauma [
22]. These patients demonstrate delayed clinical deterioration following improvement of symptoms after trauma [
2,
3,
4,
19,
28]. In patients with delayed ICH from a pseudoaneurysm in the MMA, CT angiography shows no EDH and ICH contacting the dura mater [
2,
19,
28]. We can expect these presentations given the mechanism of delayed ICH due to pseudoaneurysm in the MMA. In delayed ICH from pseudoaneurysm in the MMA, pressure from the pseudoaneurysm slowly thins the dura mater until it finally attaches to the inner layer of the dura mater, rather than the outer layer. Consequently, rupture of this pseudoaneurysm does not result in EDH. Pseudoaneurysm adhesion to the brain cortex might promote the development of ICH or SDH [
5,
6,
20].
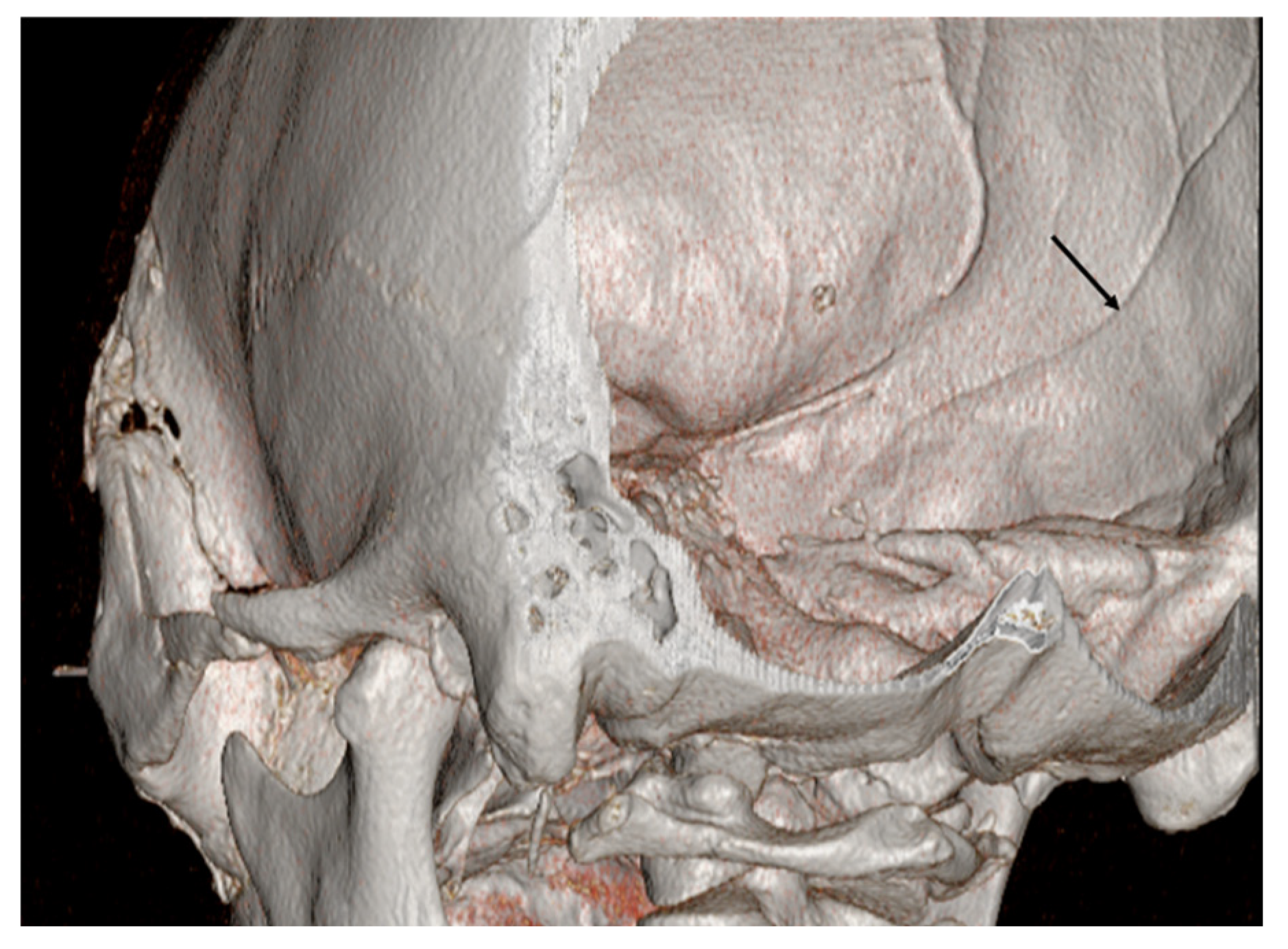
3.4. Importance of preoperative angiography
Pseudoaneurysm may be missed because cerebral angiography is seldom performed as a result of the introduction of CT and magnetic resonance imaging in patients after trauma. Higazi et al., reported the importance of angiography in the evaluation of pseudoaneurysm in the MMA after trauma [
29].Bozzetto-Ambrosi et al., reported a case of a 39-year-old man who underwent ICH removal [
30]. The ICH developed after the patient fell down and hit his head on the floor [
30]. Emergency craniotomy and ICH removal were performed without preoperative angiography. This patient showed a pseudoaneurysm in the posterior branch of the MMA as confirmed by postoperative angiography. Bozzetto-Ambrosi et al., treated the pseudoaneurysm with an endovascularapproach [
30]. If preoperative angiography had been performed, these authors could have removed the ICH and treated the pseudoaneurysm in one surgicaloperation. However, in the case of Bozzetto-Ambrosi et al., the operator thoroughly inspected the hematoma cavity and contents, but found no particular abnormal tissue [
30]. In this case, the bleeding pathology was located in the dura mater. A small craniotomy could not locate the pseudoaneurysm in the dura mater, thereby resulting in a second treatment.
Aoki et al., did not perform preoperative angiography before removal of a recurrent acute SDH because of a rapid progressive deterioration the patient’s condition [
4]. During removal of a SDH, unexpectedly profuse bleeding developed from a pseudoaneurysm in the MMA. Aoki et al., suspected a pseudoaneurysm of the middle cerebral artery immediately after profuse bleeding [
4]. After failing to control bleeding by temporary clipping of the M1 portion, Aoki et al., performed an extensive craniectomy [
4]. Close inspection of the bleeding site showed that the lesion projected directly from the inner surface of the dura mater. After excising the pseudoaneurysm, hemostasis by coagulation of the MMA was easily achieved. Preoperative angiography provides useful information for the treatment of pseudoaneurysm in the MMA. Surgeons can expect intraoperative rupture of pseudoaneurysm and avoid a second operation or endovascular treatment. Reconstructive CT angiography can raise suspicions of a pseudoaneurysm. In CT angiography, pseudoaneurysm without connection to an intracranial vessel has been observed (
Figure 4).
However, pseudoaneurysm is not always observed by CT angiography [
2].It is possible that CT angiography will miss a diagnosis of pseudoaneurysm. We therefore recommend that CT angiography should be performed for patients with suspicion of pseudoaneurysm in the MMA. If CT angiography does not identify pseudoaneurysm, the clinician should perform cerebral angiography.
4. Operative treatment
Pouyanne et al., reported one of the most dramatic presentations of delayed ICH of pseudoaneurysm in the MMA in 1959 [
5]. In that case, the patient fully recovered but then demonstrated a devastating temporal lobe hemorrhage 1 month later and showed severely impaired neurological status. Traumatic pseudoaneurysm of the MMA is not a benign lesion. Therefore, clinicians should perform aggressive treatment for patients with ICH due to rupture of the MMA after trauma. Although a few cases with spontaneous resolution of pseudoaneurysm in MMA have been reported [
31,
32], we recommend aggressive treatment, particularly if associated with ICH.
4.1. Craniotomy
Wang et al., reported a case of EDH only, without ICH, originating from a pseudoaneurysm in the MMA [
33]. They described rapid bleeding from the skull base in an operation to remove the EDH; however, they could not locate the hemorrhage and could stop the bleeding only by tenting suture during the EDH removal. In this operation, the operator did not suspect pseudoaneurysm of the MMA and performed craniotomy for the EDH removal. After a correct diagnosis of pseudoaneurysm in the MMA by CT angiography, Wang et al., performed another extension craniotomy and identified an extradural pseudoaneurysm about 4 × 4 cm in diameter [
33]. Correct craniotomy covering the skull base for removal of pseudoaneurysm in the MMA should be performed via interpretation of CT angiography.
Aoki et al., reported extensive craniectomy, including the temporal base, after a failure to control bleeding by temporary clipping of the M1 portion during removal of an SDH that originated from a pseudoaneurysm in the MMA [
4]. The surgeon could successfully excise the pseudoaneurysm and control the bleeding. In operations for pseudoaneurysm in the MMA, surgeons should perform wide craniotomy including the proximal and distal MMAs of the pseudoaneurysm.
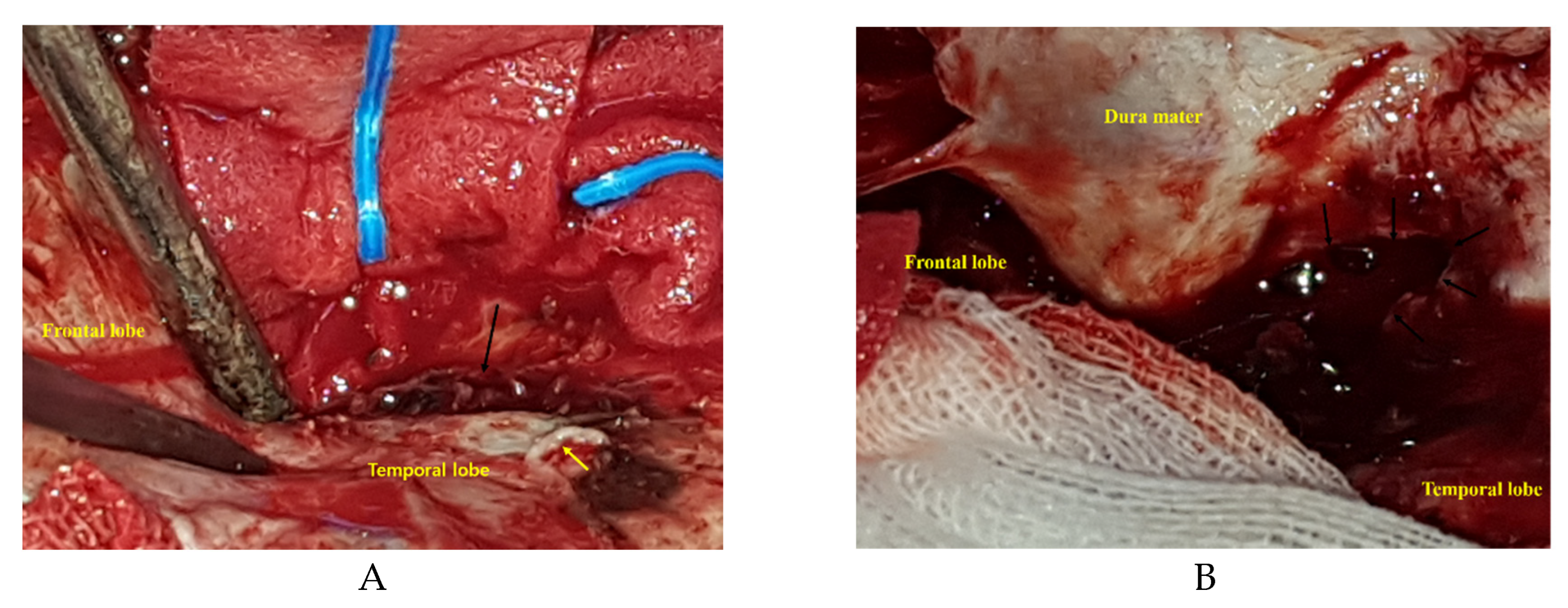
4.2. Intraoperative rupture from pseudoaneurysm in MMA
In operations of acute ICH for pseudoaneurysm in the MMA, intraoperative rupture just after bone flap removal developed in two patients [
6,
7]. Moon et al., described a pseudoaneurysm attached to the outer surface of the dura mater accompanied by abrupt bleeding just after bone flap removal [
6]. Kumar et al., also reported brisk extradural bleeding after bone flap removal [
7].
In operations for delayed ICH from pseudoaneurysm in the MMA, intraoperative rupture from the pseudoaneurysm developed in two cases. One casedeveloped active bleeding from the MMA after dural opening [
22]. In this case, the exact relationship between the dura mater and the pseudoaneurysm could not be identified. In another case, unexpected profuse bleeding from the pseudoaneurysm in the MMA developed just after evacuation of the SDH [
4]. Knowledge regarding the mechanism underlying delayed ICH development due to pseudoaneurysm suggests intraoperative rupture of pseudoaneurysm canbe expected during both ICH removal and dural opening.
In our opinion, during operations for acute ICH removal, intraoperative rupture of pseudoaneurysm might occur after bone flap removal because the pseudoaneurysm is attached to the outer surface of the dura mater. During surgery for delayed ICH removal, intraoperative bleeding from the pseudoaneurysm may occur after hematoma removal or dural opening because of the attachment of the pseudoaneurysm to the inner surface of the dura mater.
4.3. Treatment of pseudoaneurysm
In cases of acute ICH from rupture of a pseudoaneurysm in the MMA [
6,
7,
8], we identified detailed information for treatment of the pseudoaneurysm. In six cases with delayed ICH [
2,
3,
4,
19,
22,
28], we obtained operative information for treatment of pseudoaneurysm. In operations for pseudoaneurysm, we found several characteristics of the pseudoaneurysm. In the operative field, Ku mar et al., reported that the surgeon did not find a well-formed aneurysm wall [
7]. In that case, cauterization of the MMA and occlusion of the foramen spinosum with bone wax were performed to control bleeding from the pseudo aneurysm. In acute ICH for a pseudoaneurysm of the MMA, a surgeon may not find pseudoaneurysm in the operative field. Also, in reports of surgical treatment for pseudoaneurysm presenting as ICH [
4,
6,
8], surgeons have excised the pseudoaneurysm and cauterized the MMA to control bleeding. Moon et al., utilized excision of a pseudoaneurysm and coagulated the MMA after several unsuccessful trials of cauterizations of pseudoaneurysm for bleeding control [
6]. Aoki et al., reported that after excision of a pseudoaneurysm, hemostasis was easily controlled by coagulation of the MMA [
4]. Sometimes, simple coagulation of the pseudoaneurysm can result in uncontrolled bleeding. We suggest excision of a pseudoaneurysm is the first step of the operation followed by coagulation of the MMA.
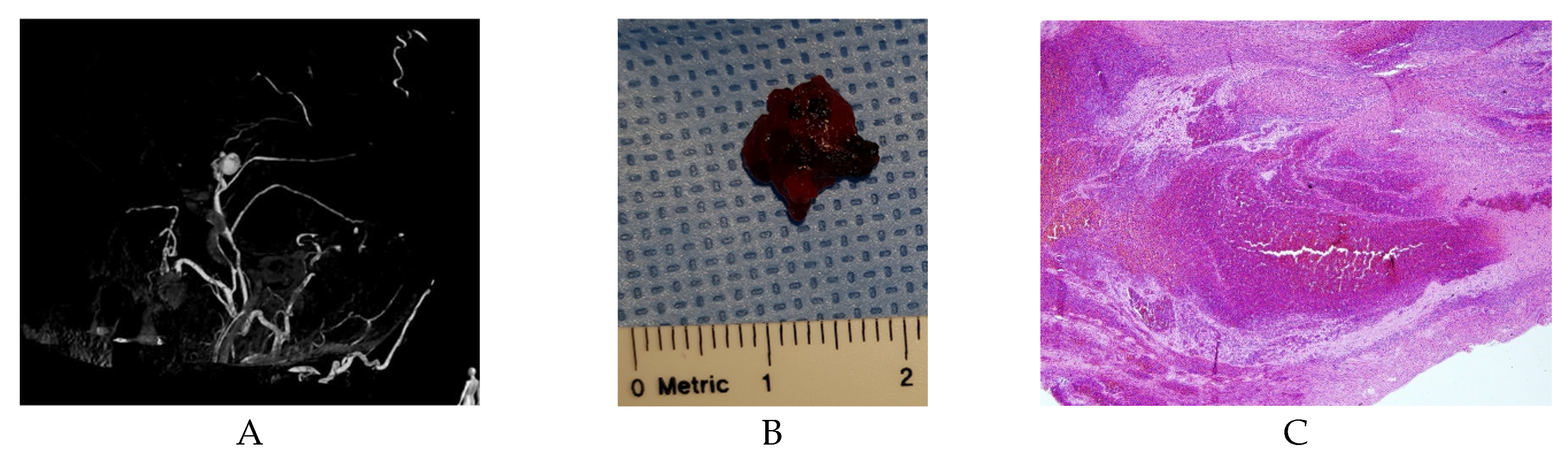
5. Pathology of pseudoaneurysm
A partial rupture of the MMA after trauma can be repaired by clot formation
that contains the intraluminal blood [
34]. Several researchers have reported performing pathological examination of the pseudoaneurysm in the MMA after trauma [
4,
12,
15,
29,
33,
35]. Microscopic examination of a pseudoaneurysm revealed a fibrotic capsule adjacent to a tear in the arterial wall [
21]. On histological examination of pseudoaneurysm presenting with acute ICH, the tissue had no normal vascular structure (
Figure 5B and 5C). In delayed ICH presentation, histological examination of the aneurysmal sac demonstrated fibrous organization, organized hematoma, and deposits of hemosiderin [
4,
5].
6. Conclusion
In cases of acute ICH due to rupture of pseudoaneurysm in the MMA, the pseudoaneurysm is in contact with the outer layer of the dura mater and usually ruptured during removal of the bone flap. In cases of delayed ICH resulting from rupture of pseudoaneurysm of the MMA, the pseudoaneurysm is attached to the inner layer of the dura mater and may be ruptured upon dura opening or hematoma removal. Surgeons should perform extensive craniotomy surrounding a pseudoaneurysm and remain aware of the intraoperative rupture of pseudoaneurysm.
Author Contributions
Conceptualization, Y.H.K. and M.S.K.; methodology, Y.H.K. and M.S.K.; software, Y.H.K. and M.S.K.; validation, Y.H.K. and M.S.K.; formal analysis, Y.H.K. and M.S.K.; investigation, Y.H.K. and M.S.K.; resources, Y.H.K. and M.S.K.; data curation, Y.H.K. and M.S.K.; writing—original draft preparation, Y.H.K. and M.S.K.; writing—review and editing, Y.H.K. and M.S.K.; visualization, Y.H.K. and M.S.K.; supervision, Y.H.K. and M.S.K.; project administration, Y.H.K. and M.S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting reported results can be found in references.
Acknowledgments
We thank to Online English (onleng.com.au) for English correction.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schulze, A. Unusual forms of epidural hematoma. Zentralbl Neurochir 1957, 17, 40–47. [Google Scholar] [PubMed]
- Wu, X.; Jin, Y.; Zhang, X. Intraparenchymal hematoma caused by rupture of the traumatic pseudoaneurysm of middle meningeal artery. J Craniofac Surg 2014, 25, e111–e113. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Ahmad, F.U.; Mahapatra, A.K. Traumatic middle meningeal artery aneurysm causing intracerebral hematoma: a case report and review of literature. Surg Neurol 2006, 66, 321–323. [Google Scholar] [CrossRef]
- Aoki, N.; Sakai, T.; Kaneko, M. Traumatic aneurysm of the middle meningeal artery presenting as delayed onset of acute subdural hematoma. Surg Neurol 1992, 37, 59–62. [Google Scholar] [CrossRef]
- Pouyanne, H.; Leman, P.; Got, M.; Gouaze, A. Traumatic arterial aneurysm of the left middle meningeal artery. Rupture one month after the accident. Temporal intracerebral hematoma. Intervention. Neurochirurgie 1959, 5, 311–315. [Google Scholar] [PubMed]
- Moon, J.U.; Youn, S.W.; Suh, J.H.; Kim, M.S. Acute intraparenchymal hemorrhage caused by rupture of a traumatic pseudoaneurysm of the middle meningeal artery : A case report. Interdisciplinary Neurosurgery, 2020; 22, 100801. [Google Scholar]
- Kumar, R.J.; Sundaram, P.K.; Gunjkar, J.D. Traumatic giant pseudoaneurysm of the middle meningeal artery causing intracerebral hematoma. Neurol India, 2011; 59, 921–922. [Google Scholar]
- Lim, D.H.; Kim, T.S.; Joo, S.P.; Kim, S.H. Intracerebral hematoma caused by ruptured traumatic pseudoaneurysm of the middle meningeal artery : a case report. J Korean Neurosurg Soc 2007, 42, 416–418. [Google Scholar] [CrossRef]
- Hassler, O. Medial defects in the meningeal arteries. J Neurosurg 1962, 19, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, R.A.; Kugler, H. False Aneurysms of the Middle Meningeal Artery. J Neurosurg 1964, 21, 92–96. [Google Scholar] [CrossRef]
- 11. Salazar, F.J.; Vaquero, J.; Garcia, S.R.; Rossi, E.; Martinez, R.; Martinez, P.; Santos, H.; Bravo, G. Traumatic false aneurysms of the middle meningeal artery. Neurosurgery 1986, 18, 200–203. [Google Scholar] [CrossRef]
- Garza-Mercado, R.; Rangel, RA. Extradural hematoma associated with traumatic middle meningeal artery pseudoaneurysm: report of two cases. Neurosurgery 1979, 5, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Dilenge, D.; Wuthrich, R. Traumatic aneurysm of the middle meningeal artery. Neurochirurgia (Stuttg) 1962, 4, 202–206. [Google Scholar]
- Hirsch, J.F.; David, M.; Sachs, M. Traumatic intracranial arterial aneurysms. Neurochirurgie 1962, 8, 189–201. [Google Scholar] [PubMed]
- Auld, A.W; Aronson, H.A; Gargano, F. Aneurysm of the middle meningeal artery. A case report. Arch Neurol, 1965; 13, 369–371. [Google Scholar] [CrossRef]
- Rumbaugh, C.L.; Bergeron, R.T.; Kurze, T. Intracranial vascular damage associated with skull fractures. Radiographic aspects. Radiology 1972, 104, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Kohyama, S.; Kakehi, Y.; Yamane, F.; Ooigawa, H.; Kurita, H.; Ishihara, S. Subdural and intracerebral hemorrhage caused by spontaneous bleeding in the middle meningeal artery after coil embolization of a cerebral aneurysm. J Stroke Cerebrovasc Dis 2014, 23, e433–e435. [Google Scholar] [CrossRef] [PubMed]
- Marvin, E.; Laws, L.H.; Coppens, J.R. Ruptured pseudoaneurysm of the middle meningeal artery presenting with a temporal lobe hematoma and a contralateral subdural hematoma. Surg Neurol Int 2016, 7, S23–S27. [Google Scholar] [CrossRef] [PubMed]
- Kulanthaivelu, K; Siddiqui, S.M.; Prasad, C.; Shashidhar, A. Traumatic Pseudoaneurysm of Middle Meningeal Artery with Delayed Presentation as Intracerebral Hematoma: A Report with Review of Literature. Neurol India 2021, 69, 1820–1823. [CrossRef]
- Kia-Noury, M. Traumatic intracranial aneurysm of the medial meningeal artery after skull base fracture. Zentralbl Neurochir 1961, 21, 351–357. [Google Scholar] [PubMed]
- Roski, R.A.; Owen, M.; White, R.J.; Takaoka, Y.; Bellon, E.M. Middle meningeal artery trauma. Surg Neurol 1982, 17, 200–203. [Google Scholar] [CrossRef]
- Bruneau, M.; Gustin, T.; Zekhnini, K.; Gilliard, C. Traumatic false aneurysm of the middle meningeal artery causing an intracerebral hemorrhage: case report and literature review. Surg Neurol 2002, 57, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Kawano, T.; Kaneko, Y.; Ooasa, T.; Ooigawa, H.; Ogasawara, S. Traumatic lesions of the bilateral middle meningeal arteries--case report. Neurol Med Chir (Tokyo) 2002, 42, 221–223. [Google Scholar] [CrossRef]
- de Andrade, A.F.; Figueiredo, E.G.; Caldas, J.G.; Paiva, W.S.; De Amorim, R.L.; Puglia, P.; Frudit, M.; Teixeira, M.J. Intracranial vascular lesions associated with small epidural hematomas. Neurosurgery 2008, 62, 416–421. [Google Scholar] [CrossRef]
- Bonasia, S.; Smajda, S.; Ciccio, G.; Robert, T. Middle Meningeal Artery: Anatomy and Variations. AJNR Am J Neuroradiol 2020, 41, 1777–1785. [Google Scholar] [CrossRef]
- Albert, F.K.; Oldenkott, P.; Sigmund, E. Subarachnoid hemorrhage and intracerebral hematoma in injury of the middle meningeal artery (aneurysma spurium). Zentralbl Neurochir 1989, 50, 153–156. [Google Scholar] [PubMed]
- Paiva, W.S.; de Andrade, A.F.; Amorim, R.L.; Figueiredo, E.G.; Teixeira, M.J. Traumatic pseudoaneurysm of the middle meningeal artery causing an intracerebral hemorrhage. Case Rep Med 2010, 2010, 219572. [Google Scholar] [CrossRef]
- Montanari, E.; Polonara, G.; Montalti, R.; Vivarelli, M.; Ricciuti, R.A.; Giorgetti, R.; Tagliabracci, A. Delayed Intracerebral Hemorrhage After Pseudoaneurysm of Middle Meningeal Artery Rupture: Case Report, Literature Review, and Forensic Issues. World Neurosurg 2018, 117, 394–410. [Google Scholar] [CrossRef] [PubMed]
- Higazi, I.; el-Banhawy, A.; el-Nady, F. Importance of angiography in identifying false aneurysm of the middle meningeal artery as a cause of extradural hematoma. Case report. J Neurosurg 1969, 30, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto-Ambrosi, P.; Andrade, G.; Azevedo-Filho, H. Traumatic pseudoaneurysm of the middle meningeal artery and cerebral intraparenchymal hematoma: case report. Surg Neurol 2006, 66 Suppl 3, S29–S31. [Google Scholar] [CrossRef]
- Shah, Q.; Friedman, J.; Mamourian, A. Spontaneous resolution of traumatic pseudoaneurysm of the middle meningeal artery. AJNR Am J Neuroradiol 2005, 26, 2530–2532. [Google Scholar]
- Srinivasan, A.; Lesiuk, H.; Goyal, M. Spontaneous resolution of posttraumatic middle meningeal artery pseudoaneurysm. AJNR Am J Neuroradiol 2006, 27, 882–883. [Google Scholar]
- Wang, C.H; Lee, H.C.; Cho, D.Y. Traumatic pseudoaneurysm of the middle meningeal artery: possible indicators for early diagnosis in the computed tomography era. Surg Neurol 2007, 68, 676–681. [Google Scholar] [CrossRef]
- Shah, Q.A.; Hurst, R.W. Endovascular Treatment of a Traumatic Pseudo Aneurysm of the Middle Meningeal Artery. Radiol Case Rep 2006, 1, 73–76. [Google Scholar] [CrossRef]
- Nayil, K.; Ramzan, A.; Makhdoomi, R.; Wani, A.; Zargar, J.; Shaheen, F. Incidental traumatic pseudoaneurysm of the middle meningeal artery: case report and literature review. Turk Neurosurg 2012, 22, 239–241. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).