1. Introduction
Cardiovascular disease (CVD) increases the duration of hospitalization, number of visits to doctors, and risks of morbidity and mortality in patients with chronic inflammatory diseases, especially rheumatoid arthritis (RA). In addition, CVD increases treatment costs for patients with RA and represents a significant burden on the healthcare system [
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12]. Most studies and meta-analyses on RA and CVD have shown that patients with RA have a 50-60% higher risk of developing CVD than the general population [
1,
2,
3,
4,
5,
6,
7,
8,
9]. In addition, patients with RA have an increased risk for mortality due to CVD, especially chronic ischemic heart disease, acute myocardial infarction, and acute cerebrovascular disease [
3,
6,
9,
10,
11,
12].
Several tools are used for assessing the risk of cardiovascular death and non-fatal events in the general population based on risk factors. The European Society of Cardiology (ESC) (2021) recommends the use of the Systematic Coronary Risk Estimation 2 (SCORE 2) risk prediction algorithm for assessing the risk of CVD in European populations [
13]. The ESC recommends that for patients with RA, the relative risk estimate obtained from the SCORE 2 score should be multiplied by 1.4 for men and 1.5 for women if two of the three following criteria are met: duration of RA >10 years, detection of positive rheumatoid factors (RF) or anti-citrulline antibodies (anti-CCP), or presence of extra-articular manifestations of RA [
13]. Traditional risk factors for CVD include modifiable factors, such as arterial hypertension, dyslipidemia, insulin resistance, diabetes, cigarette smoking, and low physical activity, and non-modifiable factors, such as genes, race, age, and sex [
13]. Although the percentage of smokers in western developed countries is decreasing, it is still quite high in Eastern Europe, and still has a significant impact on cardiovascular risk and mortality from CVD [
10,
11,
12,
13].
In this prospective cohort clinical study, we investigated the prevalence of cigarette smoking in patients with RA and analyzed the relationship between cigarette smoking and CVD in patients diagnosed with RA (investigation group) and osteoarthritis (OA) (control group), and in CVD- or symptomatic heart failure (HF)-naïve patients, compared with the general population of Croatia.
2. Materials and Methods
This is a prospective, clinical, cohort study of 201 patients selected from the Rheumatology Center of University Hospital Osijek. Of the included patients, 124 diagnosed with RA were included in the study group, whereas 77 with OA were assigned to the control group. The patients were selected from a department database (not digital at the time of recruitment). We searched the database manually and included all eligible patients according to the inclusion and exclusion criteria outlined below. The time for inclusion lasted for one year. The participants were followed up for an average of 8 years and 4±3 months between 2008/9 and 2016/17.
The participants and their families were instructed to report any changes in their health status, including the occurrence of CVD or new CVD risk factors, any other disease, surgery, or RA flare (a list was provided) by telephone, e-mail or personal visit. The inclusion criteria for this study were as follows: diagnosis of RA and OA for patients in the study and control groups, respectively, by a rheumatologist according to the American College of Rheumatology classification criteria; provision of signed informed consent; and permanent residence in one of the five counties in Eastern Croatia. The exclusion criteria were as follows: diagnosis of any form of CVD or symptomatic HF prior to inclusion, refusal to participate after the initial (inclusion) visit, permanent cessation of residence in one of the five counties of eastern Croatia during the study period, or unavailability during the study. The exclusion CVD were: any type of myocardial infarction or angina pectoris, significant coronary disease proven on diagnostic tests, symptomatic or asymptomatic ischemic cardiomyopathy, stroke or transient ischemic attack, acute or chronic dissection or aneurysm of the aorta, penetrating aortic ulcer or intramural hematoma, symptomatic or asymptomatic peripheral arterial disease. Any patient suspected on CVD based on recorded or detected signs, symptoms or tests was also excluded.
All included participants (study and control groups) were scheduled for initial (inclusion) and final visits (if available), whereas the patients in the study group were scheduled for annual visits for the assessment of RA activity. At the initial visit, all participants completed a comprehensive case report form (CRF): questionnaire, physical examination, and laboratory tests. The examinations comprised completion of the questionnaire, which was written in Croatian; physical examination, including measurement of blood pressure three times at 10-minute intervals (the average value was used for analysis), weight, height, and waist and hip circumference; assessment of general health and pain intensity using visual analog scales; completion of the Disease Activity Score 28 with C-reactive protein (DAS28-CRP) scale (RA group only) [
14], arthritis severity index for OA of the hand (OA group only) [
15], Lequesne index for OA of the hip and knee (OA group only) [
15], and the Croatian version of the Health Assessment Questionnaire (both RA and OA groups) [
16]; electrocardiography performed using a 12-channel electrocardiograph; and collection of venous blood for laboratory analysis of erythrocyte sedimentation rate and C-reactive protein, total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides, creatinine, blood glucose, and glycosylated hemoglobin levels (both RA and OA groups). An oral glucose load test was also performed when indicated. The RF and anti-CCP levels of the patients with RA were measured. All forms were completed by a physician based on the information obtained.
Annual visits were scheduled for the study group to assess RA activity, visit CRF hat to be completed. RA activity was assessed by calculating the DAS28 scores of the patients, and updating their data on diseases (CVD and non-CVD), CVD risk factors, and medication use. At the final visit, the patients were required to complete final visit CRF: questionnaire with items on CVD, CVD risk factors, non-CVD diseases, medications used, and surgeries underwent during the study period. Examinations and laboratory tests performed at the initial (inclusion) visit were also performed at the final visit.
For participants who died or become unavailable during the study period special CRF was made; if died the cause and time of death and data on known CVD risk factors were recorded.
All study original source documents are stored in registries in hospitals archive in paper form because study was conducted before hospital started to implement centralized information system.
All CRF-s are available in Supplementary Material.
2. Statistical Methods
Descriptive statistics were used to describe and summarize the study data. Inferential statistics were applied to test our hypotheses. An independent samples t-test was used to check the significance of mean differences. Levene’s test was performed and depending on the results, a t-test assuming equal or unequal variance was used to determine statistical significance between groups. A chi-square test of independence was used to analyze the relationships between qualitative variables. Fisher's exact test was used when assumptions for the chi-square test were not met. The level of significance was set at p < 0.05, and 0.05 <p < 0.10 was considered as a tendency (marginally significant).
3. Results
Of the 201 participants included in this study between 2008/9 and 2016/17, 124 had RA and 77 had OA. A total of 137 participants (82 patients with RA and 55 patients with OA) completed the study. The reasons for not completing the questionnaire were death (58 patients; 41 with RA and 17 with OA), refusal to continue the study, or relocation (6 patients; 1 with RA and 5 with OA).
At the initial visit, the study (RA) group included 25 men and 99 women, whereas the control (OA) group included 11 men and 66 women. The average age of the patients in the RA group was 59.78 years, whereas that of those in the OA group was 64.23 years. Of the patients with RA, 90.2% tested positive for RF.
At the final visit, the RA group included 82 patients, whereas the OA group included 55 patients (total number of patients: 137). The average age of the patients in the RA group was 65.5 years, whereas that of those in the OA group was 71.2 years.
Fifty-eight of the 201 patients included in the study died during the eight-year follow-up period. Of these, 41 (9 men and 32 women) were in the RA group, whereas 17 (three men and 14 women) were in the OA group. Six of the patients were lost to follow-up. The average age of the deceased patients at the time of death was 74.3 years (71.6 years for the RA group and 76.9 years for the OA group), with CVD being the cause of death for 39 of the 58 deceased (29 of 41 for the RA group and 10 of 17 for the OA group).
The number of smokers in the RA group was consistently significantly higher than that in the OA group throughout the study period (
Table 1).
The number of smokers in the RA group was also significantly higher than that in the general population (p<0.0001). The prevalence of cigarette smoking among the deceased in the RA group was higher than that among the deceased in the OA group (
Table 2).
The trends in the prevalence of smoking during the study period did not change significantly in either group (
Table 3 and
Table 4).
In the RA group, cigarette smoking was significantly associated with the incidence of CVD in current smokers (p=0.028) and in patients with a history of smoking (p=0.016). This association was not observed in the OA group (
Table 5 and
Table 6).
Although there was a trend of increased mortality of smokers in the RA group (33.1%) compared to the OA group (22.1%), and increased mortality from CVD in the RA group (70.7%) compared to the OA group (58.8%), the result was not statistically significant, possibly owing to the small size of the sample (
Table 6).
4. Discussion
Smoking causes a systemic pro-inflammatory state through affecting the immune systems, cellular and humoral components [
17,
18]. Chronic cigarette smoking appears to disrupt cellular regulatory activity, inflammatory responses, and morphological, physiological, biochemical, and enzymatic responses through its impact on innate and adaptive immune responses [
17,
18,
19]
. According to Bracke et al., smoking increased the expression of the mouse pulmonary macrophage and dendritic cell enzyme matrix metalloproteinase (MMP)-12 (macrophage elastase) [
20]
. Additionally linked to the pathophysiology of RA is MMP-12 [
21,
22]
. In contrast to osteoarthritis, RA synovial tissue had higher levels of MMP-12 messenger RNA[
21]
, and overexpressing MMP-12 in transgenic rabbits significantly worsened arthritic lesions, leading to severe synovial thickening, pannus formation, prominent macrophage infiltration at an early stage, and a marked destruction of articular cartilage at a later stage [
21,
22]
. Also, studies have shown that smokers had greater proMMP-2 and proMMP-9 levels than non-smokers. It has also been suggested that MMP-9 produced by RA synovial fibroblasts may directly contribute to joint deterioration in RA [
23,
24]
.
Chronic smoke exposure frequently results in leukocytosis with reduced leukocyte function [
17,
25,
26], and long-term smoking lowers serum immunoglobulin and specific antibody response levels [
17,
26]. Despite these findings, higher autoantibody levels—particularly anti-nuclear and anti-RF—could explain why autoimmune disorders like RA are more likely to develop [
17].
Higher levels of fibrinogen, CRP, ICAM-1, E-selectin, and pro-inflammatory cytokines (e.g., TNF-, IL-1, IL-5, IL-6, IL-8, IL-13) in smokers, which is correlated with current and past smoking exposure, are evidence of the induction of an inflammatory response [
27,
28,
29,
30,
31,
32]. TNF-, IL-1, and IL-6 are crucial in the etiopathogenesis of RA, but also CVD [
32,
33].
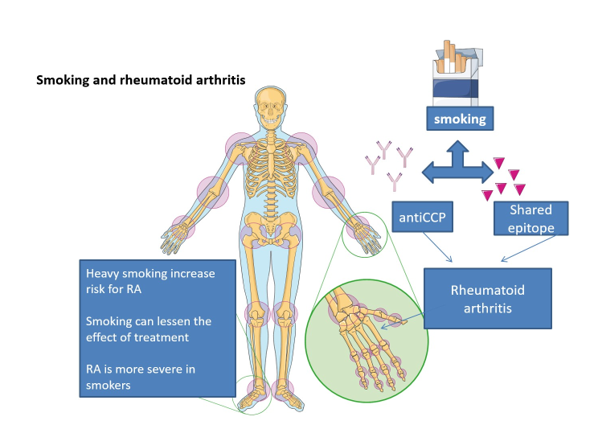
Autoantibodies against citrullinated proteins can trigger autoimmune response and it can be found in many RA patients [
34]. Smoking is known to cause immunological responses that are HLA-DR-restricted to autoantigens modified by citrullination. Smokers clearly run a higher risk of producing anti-CCP antibodies, and in genetically predisposed persons with the common epitope HLA-DRB1 gene, this risk seems to be correlated with the severity of the condition [
35,
36,
37].
Cigarette smoking is a significant risk factor for CVD. An active smoker and a passive smoker have a 50% and 30% chance of dying due to smoking, respectively. The average lifespan of a smoker is shortened by approximately 10 years [
13]. Smoking combined with RA increases the risk of CVD by approximately 25%-50%. [
38,
39]. In the present study, the prevalence of smoking in the RA (study) group was significantly higher than that in the OA (control) group and the general population of Croatia, which is one of the highest in Europe (31.1%) [
40]. In addition, the prevalence of cigarette smoking among the deceased in the RA group was higher than that among the deceased in the OA group, as well that among all the deceased and living participants with CVD combined.
Trends in the prevalence of cigarette smoking in the study and control groups did not change significantly. This suggests that smokers have an increased risk for RA. The trend of continued smoking in patients with RA may be attributed to attempts to reduce stress caused by RA symptoms. Cigarette smoking is an important modifiable risk factor for RA. The correlation between cigarette smoking and RA has been proven in epidemiological, in vivo, and animal studies [
41]. Smoking increases the risk of developing RA by approximately 40%–50% with a certain dose-dependent effect, which is consistent with our results [
41,
42,
43]. Previous studies have shown that both current and former smokers with RA have more severe symptoms, more severe joint damage, and a poorer response to therapy than those who have never smoked [
43,
44,
45,
46]. However, the reason underlying the trend of continued cigarette smoking in patients with RA remains unclear. Among the smokers in the RA group in the present study, current and former smokers, patients who completed the study, and the deceased showed a significantly increased incidence of CVD, which is in accordance with the existing knowledge on the association between smoking and CVD [
13].
Limitations
This study has some limitations. First, data on smoking habits were obtained using self-report questionnaires that were completed by the investigators by information obtained from participants; thus, the responses provided could not be confirmed. Second, data for the deceased were obtained from the coroner's records, which were not written by doctors. However, these data are used by the National Health Institute and are considered valid for official statistics reports; notably, statistical mortality analyses are only for demonstrating the magnitude of a problem, because of the sample was too small and relevant statistical analyses could not be conducted; thus, the mortality results may be accidental endpoints.
5. Conclusions
Only a few studies have been conducted to investigate the correlation between smoking, RA and CVD. Smoking still represents the mayor public health problem in the world especially in Eastern Europe where prevalence of smokers is among the highest in Europe. Thus, further studies are needed to clarify the association between RA and smoking. Moreover, clinicians should endeavor to encourage and educate patients with RA on the importance of smoking cessation.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, S1: CRF RA initial visit, S2: CRF OA initial visit, S3: CRF RA annual visit, S4 CRF RA final visit, S5 CRF RA final visit - unavailable, S6 CFR OA final visit, S7 CRF OA final visit- unavailable, S8: HAQ form, S9: Lequesene hip OA form, S 10: Lequesene knee OA form, S 11: OA fist index form, S12: DAS20 CRP form
Author Contributions
DB: Conceptualization, Investigation, Writing – Original Draft Preparation, DK: Investigation, Formal Analysis, IB: Methodology, Investigation, Formal Analysis, Writing – Review & Editing, SN: Formal Analysis, Supervision.
Funding
No funding was received for this study.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the ethics committees of University Hospital Osijek and Faculty of Medicine Osijek (No: 602-04/21-08/07).
Informed Consent Statement
Written informed consent was obtained from all participants.
Data Availability Statement
The datasets used or analyzed in this study are available from the corresponding author upon request. All source documents (pre-selection documents, initial visit questionnaire and test results, annual visit questionnaire and test results, final visit questionnaire and test results are in paper form, written in Croatian and consist participants identification data. If requested all participants identification data has to be removed (name, surname, social security number, personal identification number) All the information in the datasets consist participants identification data and are written in Croatian, also if requested identification data has to be removed.
Conflicts of Interest
The authors declare no competing interests.
References
- John H, Kitas G, Toms T, Goodson N. Cardiovascular co-morbidity in early rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2009, 23, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Mackey RH, Kuller LH, Deane KD, Walitt BT, Chang YF, Holers VM, i sur. Rheumatoid Arthritis, Anti-Cyclic Citrullinated Peptide Positivity, and Cardiovascular Disease Risk in the Women's Health Initiative. Arthritis Rheumatol. 2015, 67, 2311–2322. [Google Scholar] [CrossRef] [PubMed]
- Sakai R, Hirano F, Kihara M, Yokoyama W, Yamazaki H, Harada S, i sur. High prevalence of cardiovascular comorbidities in patients with rheumatoid arthritis from a population-based cross-sectional study of a Japanese health insurance database. Mod Rheumatol. 2016, 26, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Avina-Zubieta JA, Thomas J, Sadatsafavi M, Lehman AJ, Lacaille D. Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. 2012, 71, 1524–1529. [Google Scholar] [CrossRef] [PubMed]
- Janssens HJ, Arts PG, Schalk BW, Biermans MC. Gout and rheumatoid arthritis, both to keep in mind in cardiovascular risk management: A primary care retrospective cohort study. Joint Bone Spine. 2016, 25. [Google Scholar]
- Lévy L, Fautrel B, Barnetche T, Schaeverbeke T. Incidence and risk of fatal myocardial infarction and stroke events in rheumatoid arthritis patients. A systematic review of the literature. Clin Exp Rheumatol. 2008, 26, 673–679. [Google Scholar]
- Chung WS, Lin CL, Peng CL, Chen YF, Lu CC, Sung FC, Kao CH. Rheumatoid arthritis and risk of acute myocardial infarction--a nationwide retrospective cohort study. Int J Cardiol. 2013, 168, 4750–4754. [Google Scholar] [CrossRef]
- Meune C, Touzé E, Trinquart L, Allanore Y. High risk of clinical cardiovascular events in rheumatoid arthritis: Levels of associations of myocardial infarction and stroke through a systematic review and meta-analysis. Arch Cardiovasc Dis. 2010, 103, 253–261. [Google Scholar] [CrossRef]
- Siebert S, Lyall DM, Mackay DF, et al. Characteristics of rheumatoid arthritis and its association with major comorbid conditions: cross-sectional study of 502 649 UK Biobank participants. RMD Open 2016, 2, e000267. [Google Scholar] [CrossRef]
- Christophe Meune, Emmanuel Touze, Ludovic Trinquart and Yannick Allanore. Trends in cardiovascular mortality in patients with rheumatoid arthritis over 50 years: a systematic review and meta-analysis of cohort studies. Rheumatology 2009, 48, 1309–1313. [Google Scholar] [CrossRef]
- Inge, A.M. van den Oever, Alper M. van Sijl and Michael T. Nurmohamed. Management of cardiovascular risk in patients with rheumatoid arthritis: evidence and expert opinion. Ther Adv Musculoskel Dis. 2013, 5, 166–181. [Google Scholar]
- Nurmohamed MT, Heslinga M, Kitas GD. Cardiovascular comorbidity in rheumatic diseases. Nat Rev Rheumatol. 2015, 11, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Frank L J Visseren and others, 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). European Heart Journal 2021, 42, 3227–3337.
- DAS-score. nl. Disease activity score in rheumatic arthritis. Web address: http//www.das-score.nl. Access date: 12.01.2009.
- Lequesne, M. Indices of severity and disease activity for osteoarthritis. Semin Arthritis Rheum. 1991, 20, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Kirwan JR, Reeback JS. Stanford health assesment questionnaire modified to asses disability in British patients with rheumatoid arthritis. Br J Rheumatol 1986, 25, 206–209. [Google Scholar] [CrossRef]
- Sopori, M. Effects of cigarette smoke on the immune system. Nat. Rev. Immunol. 2002, 2, 372–377. [Google Scholar] [CrossRef]
- Holt, P.G. , Keast D. Environmentally induced changes in immunological function: Acute and chronic effects of inhalation of tobacco smoke and other atmospheric contaminants in man and experimental animals. Bacteriol. Rev. 1977, 41, 205–216. [Google Scholar] [CrossRef]
- Harel-Meir, M. , Sherer Y., Shoenfeld Y. Tobacco smoking and autoimmune rheumatic diseases. Nat. Clin. Pract. Rheumatol. 2007, 3, 707–715. [Google Scholar] [CrossRef]
- Bracke, K. , Cataldo D., Maes T., Gueders M., Noël A., Foidart J.M., Brusselle G., Pauwels R.A. Matrix metalloproteinase-12 and cathepsin D expression in pulmonary macrophages and dendritic cells of cigarette smoke-exposed mice. Int. Arch. Allergy Immunol. 2005, 138, 169–179. [Google Scholar] [CrossRef]
- Liu, Y. , Aryee M.J., Padyukov L., Fallin M.D., Hesselberg E., Runarsson A., Reinius L., Acevedo N., Taub M., Ronninger M., et al. Epigenome-wide association data implicate DNA methylation as an intermediary of genetic risk in rheumatoid arthritis. Nat. Biotechnol. 2013, 31, 142–147. [Google Scholar] [CrossRef]
- Wang, H. , Yu M., Ochani M., Amella C.A., Tanovic M., Susarla S., Li J.H., Wang H., Yang H., Ulloa L., et al. Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature. 2003, 421, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Raitio, A. , Tuomas H., Kokkonen N. Levels of matrix metalloproteinase-2, -9 and -8 in the skin, serum and saliva of smokers and non-smokers. Arch. Dermatol. Res. 2005, 297, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Xue M., McKelvey K., Shen K., Minhas N., March L., Park S.Y., Jackson C.J. Endogenous MMP-9 and not MMP-2 promotes rheumatoid synovial fibroblast survival, inflammation and cartilage degradation. Rheumatology (Oxford) 2014.
- Kawada, T. Smoking-induced leukocytosis can persist after cessation of smoking. Arch. Med. Res. 2004, 35, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.D. , Houchens D.P., Kluwe W.M., Craig D.K., Fisher G.L. Effects of mainstream and environmental tobacco smoke on the immune system in animals and humans: A review. Crit. Rev. Toxicol. 1990, 20, 369–395. [Google Scholar] [CrossRef]
- Cozen, W. , Diaz-Sanchez D., Gauderman J.W. Th1 and Th2 cytokines and IgE levels in identical twins with varying levels of cigarette consumption. J. Clin. Immunol. 2004, 24, 617–622. [Google Scholar] [CrossRef]
- Arnson, Y. , Shoenfeld Y., Amital H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J. Autoimmun. 2010, 34, 258–265. [Google Scholar] [CrossRef]
- Yoshida, Y. , Tanaka T. Interleukin 6 and rheumatoid arthritis. Biomed. Res. Int. 2014. [Google Scholar] [CrossRef]
- Klimiuk, P.A. , Fiedorczyk M., Sierakowski S., Chwiecko J. Soluble cell adhesion molecules (sICAM-1, sVCAM-1, and sE-selectin) in patients with early rheumatoid arthritis. Scand. J. Rheumatol. 2007, 36, 345–350. [Google Scholar] [CrossRef]
- Klimiuk, P.A. , Sierakowski S., Latosiewicz R., Cylwik J.P., Cylwik B., Skowronski J., Chwiecko J. Soluble adhesion molecules (ICAM-1, VCAM-1, and E-selectin) and vascular endothelial growth factor (VEGF) in patients with distinct variants of rheumatoid synovitis. Ann. Rheum. Dis. 2002, 61, 804–809. [Google Scholar] [CrossRef]
- Gibbons, L.J. , Hyrich K.L. Biologic therapy for rheumatoid arthritis: Clinical efficacy and predictors of response. BioDrugs. 2009, 23, 111–124. [Google Scholar] [CrossRef]
- Bedeković, D.; Bošnjak, I.; Šarić, S.; Kirner, D.; Novak, S. Role of Inflammatory Cytokines in Rheumatoid Arthritis and Development of Atherosclerosis: A Review. Medicina 2023, 59, 1550. [Google Scholar] [CrossRef]
- Wegner, N. , Lundberg K., Kinloch A., Fisher B., Malmström V., Feldmann M., Venables P.J. Autoimmunity to specific citrullinated proteins gives the first clues to the etiology of rheumatoid arthritis. Immunol. Rev. 2010, 233, 34–54. [Google Scholar] [CrossRef]
- Klareskog, L. , Stolt P., Lundberg K., Källberg H., Bengtsson C., Grunewald J., Rönnelid J., Harris H.E., Ulfgren A.K., Rantapää-Dahlqvist S., et al. A new model for an etiology of rheumatoid arthritis: Smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheumatol. 2006, 54, 38–46. [Google Scholar]
- Gregersen, P.K. , Silver J., Winchester R.J. The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheumatol. 1987, 30, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- Mattey, D.L. , Dawes P.T., Clarke S. Relationship among the HLA-DRB1 shared epitope, smoking, and rheumatoid factor production in rheumatoid arthritis. Arthritis Rheumatol. 2002, 47, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Baghdadi LR, Woodman RJ, Shanahan EM, Mangoni AA. The impact of traditional cardiovascular risk factors on cardiovascular outcomes in patients with rheumatoid arthritis: a systematic review and meta-analysis. PLoS One. 2015, 10, e0117952. [Google Scholar]
- Castellanos-De La Hoz, J., J. Amaya-Amaya, N. Molano-Gonzalez, F. Gutierrez-Infante, J. M. Anaya and A. Rojas-Villarraga. The infuence of cigarette smoking on disease activity and joint erosions in rheumatoid arthritis: A sysrematic review ant metha-analysis. Annals of the Rheumatic Diseases. 2013, 72, 387–387. [Google Scholar] [CrossRef]
- Stevanović R, Capak, Benjak T. CROATIAN HEALTH STATISTICS YEARBOOK 2018. Publisher: Croatian Institute of Public Health. Croatia, Zagreb, 2019, X, 337.
- Chang, K., S. M. Yang, S. H. Kim, K. H. Han, S. J. Park and J. I. Shin. Smoking and Rheumatoid Arthritis. International Journal of Molecular Sciences. 2015, 15, 22279–22295. [Google Scholar] [CrossRef]
- Di Giuseppe, D., A. Discacciati, N. Orsini and A. Wolk. Cigarette smoking and risk of rheumatoid arthritis: a dose-response meta-analysis. Arthritis Research & Therapy. 2014, 16. [Google Scholar]
- Sugiyama, D., K. Nishimura, K. Tamaki, G. Tsuji, T. Nakazawa, A. Morinobu, isur. Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Annals of the Rheumatic Diseases. 2010, 69, 70–81. [Google Scholar] [CrossRef]
- Karakoc, M., I. Batmaz, M. A. Sariyildiz, M. Tahtasiz, R. Cevik, E. Tekbas, i sur. The relationship of metabolic syndrome with disease activity and the functional status in patients with rheumatoid arthritis. Journal of clinical medicine research. 2012, 4, 279–85. [Google Scholar] [PubMed]
- Heliovaara, M., K. Aho, A. Aromaa, P. Knekt and A. Reunanen. Smoking and risk of rheumatoid arthritis. Journal of Rheumatology. 1993, 20, 1830–1835. [Google Scholar] [PubMed]
- Corrao, S., S. Messina, G. Pistone, L. Calvo, R. Scaglione and G. Licata. Heart involvement in Rheumatoid Arthritis: Systematic review and meta-analysis. International Journal of Cardiology. 2013, 167, 2031–2038. [Google Scholar] [CrossRef] [PubMed]
Table 1.
Incidence and prevalence for smokers alive and deceased at final visit.
Table 1.
Incidence and prevalence for smokers alive and deceased at final visit.
| PREVALENCE (%) |
RA*INCLUSION VISIT 2008/9. (N=124) |
OA** INCLUSION VISIT 2008/9. (N=77) |
RA* FINAL VISIT 20016/17. (N=82) |
OA** FINAL VISIT 2016/17. (N=55) |
| MALE SEX |
20,2 |
14,3 |
19,5 |
18,2 |
| FEMALE SEX |
79,8 |
85,7 |
80,5 |
81,8 |
| SMOKING EVER |
46,8 |
27,3 |
52,4 |
25,5 |
| PRESENT SMOKING |
21,8 |
14,3 |
29,3 |
10,9 |
| SMOKERS – DECEASED |
.. |
.. |
36,6 (N=41) |
29,4 (N=17) |
| INCIDENCE (%) |
|
|
|
|
| CVD$– ALIVE |
.. |
.. |
31,7 |
30,9 |
| SIGNIFICANT INFECTION – ALIVE |
.. |
.. |
9,8 |
9,1 |
| NEOPLASTIC DISEASE – ALIVE |
.. |
.. |
7,3 |
10,9 |
| TOTAL DECEASED |
.. |
.. |
33,1 (N=124) |
22,1 (N=77) |
| CVD$ DECEASED |
.. |
.. |
70,7 (N=41) |
58,8 (N=17) |
| TOTAL CVD$ (ALIVE + DECEASED) |
.. |
.. |
43,9 (N=123) |
37,5 (N=72) |
| NEOPLASTIC DISEASE TOTAL (ALIVE + DECEASED) |
.. |
.. |
8,9 (N=123) |
11,1 (N=72) |
| SIGNIFICANT INFECTION TOTAL (ALICE + DECEASED) |
.. |
.. |
9,8 (N=123) |
6,9 (N=72) |
Table 2.
Prevalence of deaths among smokers.
Table 2.
Prevalence of deaths among smokers.
| |
RA* % (N=41) |
OA** % (N=17) |
TOTAL %(N=58) |
| SMOKERS |
36,6 |
29,4 |
34,5 |
| MALE SEX |
22 |
17,6 |
20,7 |
| FEMALE SEX |
78 |
82,4 |
79,3 |
Table 3.
Prevalence of smokers an initial visit, RA-OA 2008/9.
Table 3.
Prevalence of smokers an initial visit, RA-OA 2008/9.
| PREVALENCE RA*-OA** 2008/9. |
STATISTICALLY SIGNIFICANT DIFFERENCE |
ꭓ2 |
p |
| SMOKING EVER |
YES – RA* IS HIGHER |
7,573 |
0,006 |
| PRESENT SMOKING |
NO |
1,737 |
0,187 |
Table 4.
Prevalence of smokers and incidence of diseases at final visit, RA-OA 2016/17.
Table 4.
Prevalence of smokers and incidence of diseases at final visit, RA-OA 2016/17.
| RA*-OA** 2016/17. |
STATISTICALLY SIGNIFICANT DIFFERENCE |
ꭓ2 |
p |
| CVD$ INCIDENCE |
NO |
0,01 |
0,912 |
| SMOKING EVER PREVALENCE |
YES – RA* IS HIGHER |
9,866 |
0,002 |
| PRESENT SMOKING PREVALENCE |
YES – RA* IS HIGHER |
6,488 |
0,011 |
| SIGNIFICANT INFECTION INCIDENCE |
NO |
0,17 |
0,896 |
| NEOPLASTIC DISEASE INCIDENCE |
NO |
NA |
0,543 |
Table 5.
Statistically significant association between cigarette smoking and CVD incidence.
Table 5.
Statistically significant association between cigarette smoking and CVD incidence.
| |
RA* 2016/17. |
ꭓ2 |
p |
OA** 2016/17. |
ꭓ2 |
p |
| CVD$ INCIDENCE AND SMOKING EVER |
YES |
4,849 |
0,028 |
NO |
.. |
0,322 |
| CVD$ INCIDENCE AND PRESENT SMOKING |
YES |
5,781 |
0,016 |
NO |
.. |
0,369 |
Table 6.
Comparison of CVD and cigarette smoking (alive + deceased) at the final visit.
Table 6.
Comparison of CVD and cigarette smoking (alive + deceased) at the final visit.
2016/17.
N= RA* 123
N= OA** 72 |
RA* - ALIVE |
RA* - DECEASED |
OA**- ALIVE |
OA** - DECEASED |
STATISTICALLY SIGNIFICANT DIFFERENCE |
ꭓ2 |
p |
| CVD$ TOTAL INCIDENCE (ALIVE + DECEASED) |
26 |
28 |
17 |
10 |
NO |
0,767 |
0,381 |
| SMOKING EVER PREVALENCE |
43 |
15 |
14 |
5 |
YES RA*>OA** |
8,196 |
0,004 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).