Submitted:
01 July 2023
Posted:
14 July 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Government Stringency Index
Statistical analysis
Results
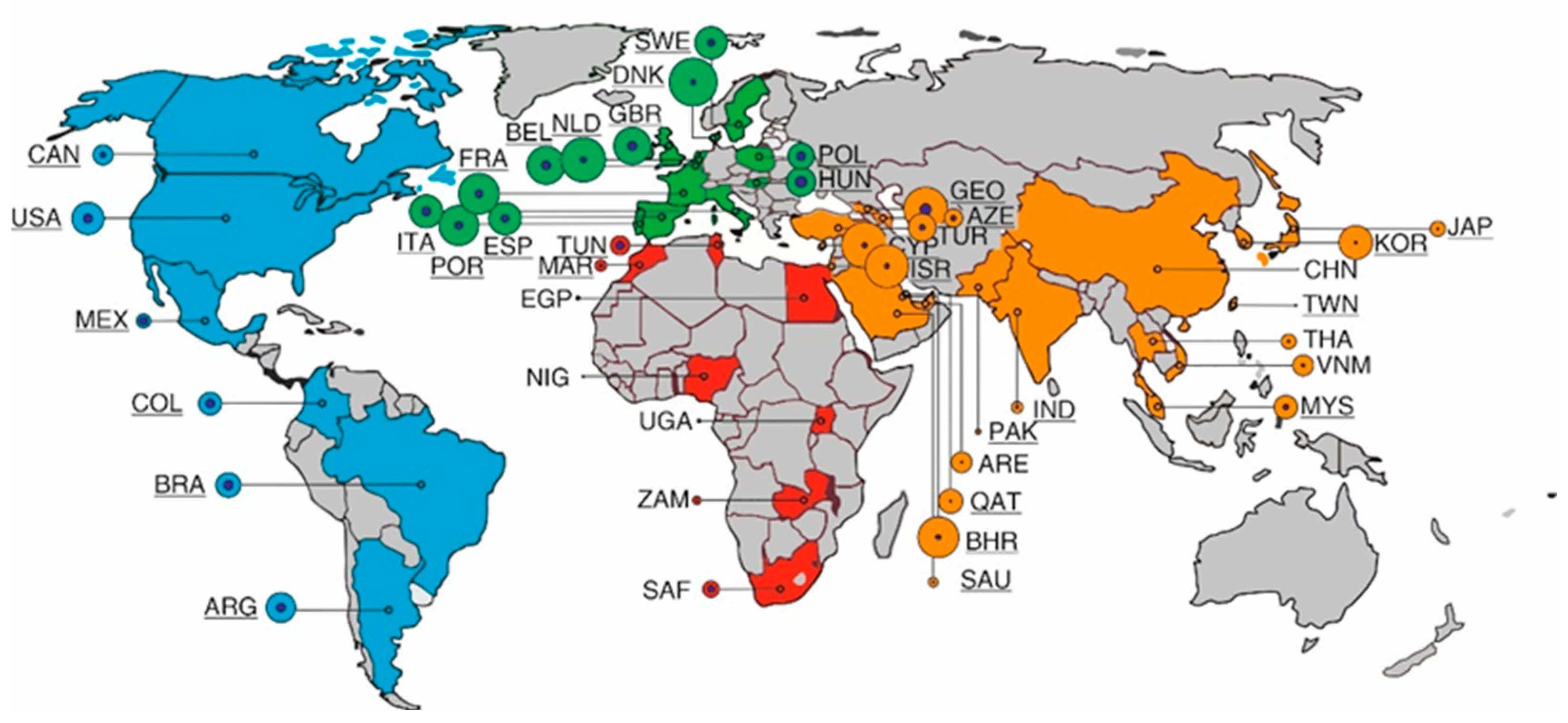
| Continent and Country or Territory | Population (as of 2020)[16,17] | Cases (cumulative per million people; March 31, 2022) | Deaths(cumula-tive per million people; March 31, 2022) | Vacci-nation rate (per March 31, 2022) | GDP per capita (US$)2020 | HDI |
| Asia | ||||||
| Azerbaijan | 10.1391.77 | 76.450 | 935 | 47.19 | 5083 | 756 |
| Bahrain | 1.701.575 | 376.128 | 998 | 69.56 | 19514 | 852 |
| China | 1.439.323.776 | 155 | 3 | 86.02 | 10370 | 761 |
| Cyprus | 1.207.359 | 475.863 | 1046 | 72.02 | 26372 | 887 |
| Georgia | 3.989.167 | 440.071 | 4470 | 31.59 | 4447 | 812 |
| India | 1.396.378.127 | 30.360 | 367 | 59.66 | 1811 | 645 |
| Israel | 8.655.535 | 413.196 | 1109 | 65.99 | 37488 | 919 |
| Japan | 126.476.461 | 52.547 | 226 | 79.86 | 34813 | 919 |
| Malaysia | 32.365.999 | 123.263 | 1029 | 78.74 | 10631 | 810 |
| Pakistan | 220.892.340 | 20.618 | 129 | 51.41 | 1446 | 557 |
| Qatar | 2.881.053 | 134.050 | 251 | 88.5 | 56026 | 848 |
| Saudi Arabia | 34.813.871 | 29.563 | 248 | 69.88 | 18691 | 854 |
| South Korea | 51.269.185 | 252.734 | 313 | 86.73 | 31327 | 916 |
| Taiwan | 23.816.775 | 969 | 36 | 76.66 | 28306 | 949 |
| Thailand | 69.799.978 | 50.222 | 349 | 71.8 | 6198 | 777 |
| Turkey | 84.339.067 | 173.963 | 1148 | 62.3 | 12038 | 820 |
| United Arab Emirates | 9.890.402 | 94.372 | 243 | 96.22 | 40438 | 890 |
| Vietnam | 97.338.579 | 96.471 | 423 | 79.15 | 2655 | 704 |
| Africa | ||||||
| Egypt | 102.334.404 | 4.552 | 220 | 30.89 | 4028 | 707 |
| Morocco | 36.910.560 | 31.053 | 428 | 32.56 | 2818 | 686 |
| Nigeria | 206.139.589 | 1.168 | 14 | 4.52 | 2396 | 539 |
| South Africa | 59.308.690 | 62.060 | 1669 | 29.81 | 5659 | 709 |
| Tunisia | 11.818.619 | 83.835 | 2292 | 53.2 | 3780 | 740 |
| Uganda | 45.741.007 | 3.468 | 76 | 17.01 | 891 | 544 |
| Zambia | 18.383.955 | 15.813 | 198 | 11.62 | 1273 | 584 |
| Europe | ||||||
| Belgium | 11.589.623 | 326.663 | 2638 | 78.52 | 45189 | 931 |
| Denmark | 5.792.202 | 519.331 | 963 | 82.5 | 56202 | 940 |
| France | 65.273.511 | 376.011 | 2097 | 77.84 | 35785 | 901 |
| Hungary | 9.660.351 | 185.528 | 4558 | 59.13 | 14368 | 854 |
| Italy | 60.461.826 | 246.758 | 2697 | 79.23 | 29359 | 892 |
| Netherlands | 17.134.872 | 446.569 | 1255 | 72.17 | 46345 | 944 |
| Poland | 37.846.611 | 149.482 | 2886 | 64.23 | 14660 | 880 |
| Portugal | 10.196.709 | 362.778 | 2097 | 92.6 | 19771 | 864 |
| Spain | 46.754.778 | 241.981 | 2149 | 86.09 | 24939 | 904 |
| Sweden | 10.099.265 | 235.250 | 1724 | 74.98 | 51539 | 945 |
| United Kingdom | 67.886.011 | 313.253 | 2846 | 72.49 | 43020 | 932 |
| America | ||||||
| United States | 331.002.651 | 237.189 | 2905 | 65.77 | 58203 | 926 |
| Canada | 37.742.154 | 90.526 | 977 | 81.92 | 42258 | 929 |
| Colombia | 50.882.891 | 117.294 | 2691 | 67.93 | 5892 | 767 |
| Brazil | 212.559.417 | 138.962 | 3064 | 75.1 | 8228 | 765 |
| Argentina | 45.195.774 | 198.529 | 2812 | 81.18 | 11334 | 845 |
| Mexico | 128.932.753 | 44.346 | 2532 | 61.19 | 8909 | 779 |
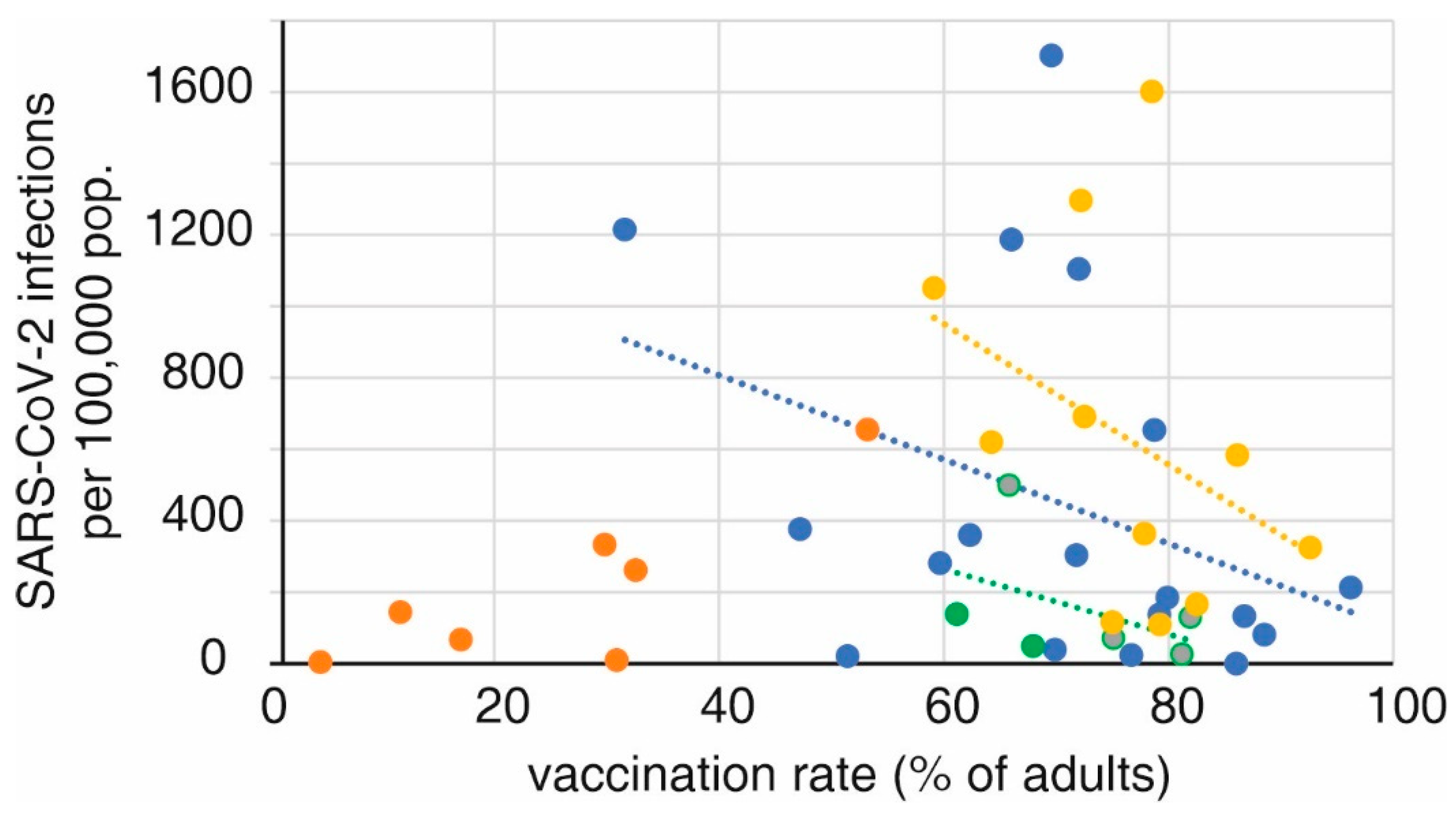
Prevention of SARS-CoV-2 infection by vaccination
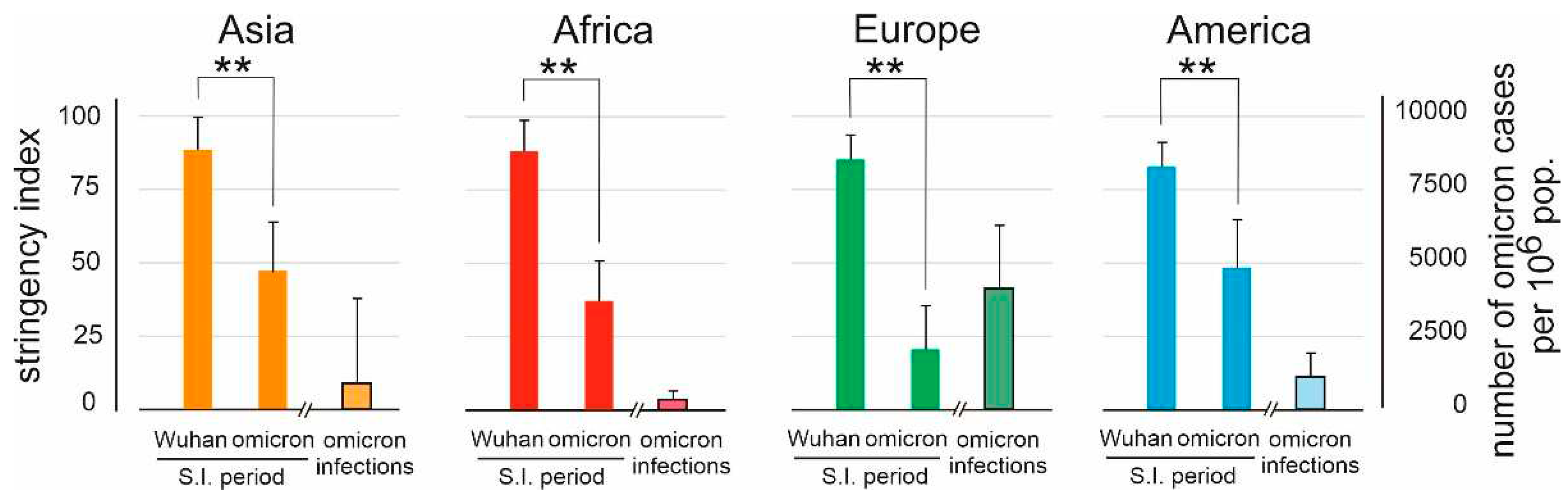
Societal restrictions
Introduction and effect of a COVID pass
Discussion
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020 Feb 20;382(8):727-733. [CrossRef]
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020 Mar 19;91(1):157-160. [CrossRef]
- Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020 Apr;76:71-76. [CrossRef]
- Hiscott J, Alexandridi M, Muscolini M, Tassone E, Palermo E, Soultsioti M, Zevini A. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020 Jun;53:1-9. [CrossRef]
- Shah SGS, Farrow A. A commentary on "World Health Organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19)". Int J Surg. 2020 Apr;76:128-129. [CrossRef]
- WHO Coronavirus (COVID-19) dashboard. (n.d.). WHO.int. Retrieved June 3, 2022, from https://covid19.who.int/.
- Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, Hasell J, Macdonald B, Beltekian D, Max Roser M (2020) - "Coronavirus Pandemic (COVID-19)". Published online at OurWorldInData.org. Retrieved from: https://ourworldindata.org/coronavirus [assessed october 22,2022].
- Greer SL, King EJ, da Fonseca EM, Peralta-Santos A. The comparative politics of COVID-19: The need to understand government responses. Glob Public Health. 2020 Sep;15(9):1413-1416. [CrossRef]
- Khailany RA, Safdar M, Ozaslan M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 2020 Jun;19:100682. [CrossRef]
- Golob JL, Lugogo N, Lauring AS, Lok AS. SARS-CoV-2 vaccines: a triumph of science and collaboration. JCI Insight. 2021 ;6(9):e149187. 10 May. [CrossRef]
- Rijkers GT, Weterings N, Obregon-Henao A, Lepolder M, Dutt TS, van Overveld FJ, Henao-Tamayo M. Antigen Presentation of mRNA-Based and Virus-Vectored SARS-CoV-2 Vaccines. Vaccines (Basel). 2021;9(8):848. [CrossRef]
- Chen LH, Petersen E, Blumberg L, Piyaphanee W, Steffen R. COVID-19 health passes: current status and prospects for a global approach. J Travel Med. 2021 Oct 11;28(7):taab118. [CrossRef]
- Ward JK, Gauna F, Gagneux-Brunon A, Botelho-Nevers E, Cracowski JL, Khouri C, Launay O, Verger P, Peretti-Watel P. The French health pass holds lessons for manda-tory COVID-19 vaccination. Nat Med. 2022 Feb;28(2):232-235. [CrossRef]
- Wang B, Ping Y. A comparative analysis of COVID-19 vaccination certificates in 12 countries/regions around the world: Rationalising health policies for international travel and domestic social activities during the pandemic. Health Policy. 2022 Aug;126(8):755-762. [CrossRef]
- Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, Webster S, Cameron-Blake E, Hallas L, Majumdar S, Tatlow H. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. 2021;5(4):529-538. [CrossRef]
- Human Development Reports. https://hdr.undp.org/data-center/human-development-index [assessed June 23, 2023].
- The World Bank. https://data.worldbank.org/ [assessed June 23, 2023].
- Stobart A, Duckett S. Australia's Response to COVID-19. Health Econ Policy Law. 2022 Jan;17(1):95-106. [CrossRef]
- Alshammari TM, Alenzi KA, Alnofal FA, Fradees G, Altebainawi AF. Are countries' precautionary actions against COVID-19 effective? An assessment study of 175 countries worldwide. Saudi Pharm J. 2021 May;29(5):391-409. [CrossRef]
- Cao X, Li Y, Zi Y, Zhu Y. The shift of percent excess mortality from zero-COVID policy to living-with-COVID policy in Singapore, South Korea, Australia, New Zealand and Hong Kong SAR. Front Public Health. 2023 Mar 20;11:1085451. [CrossRef]
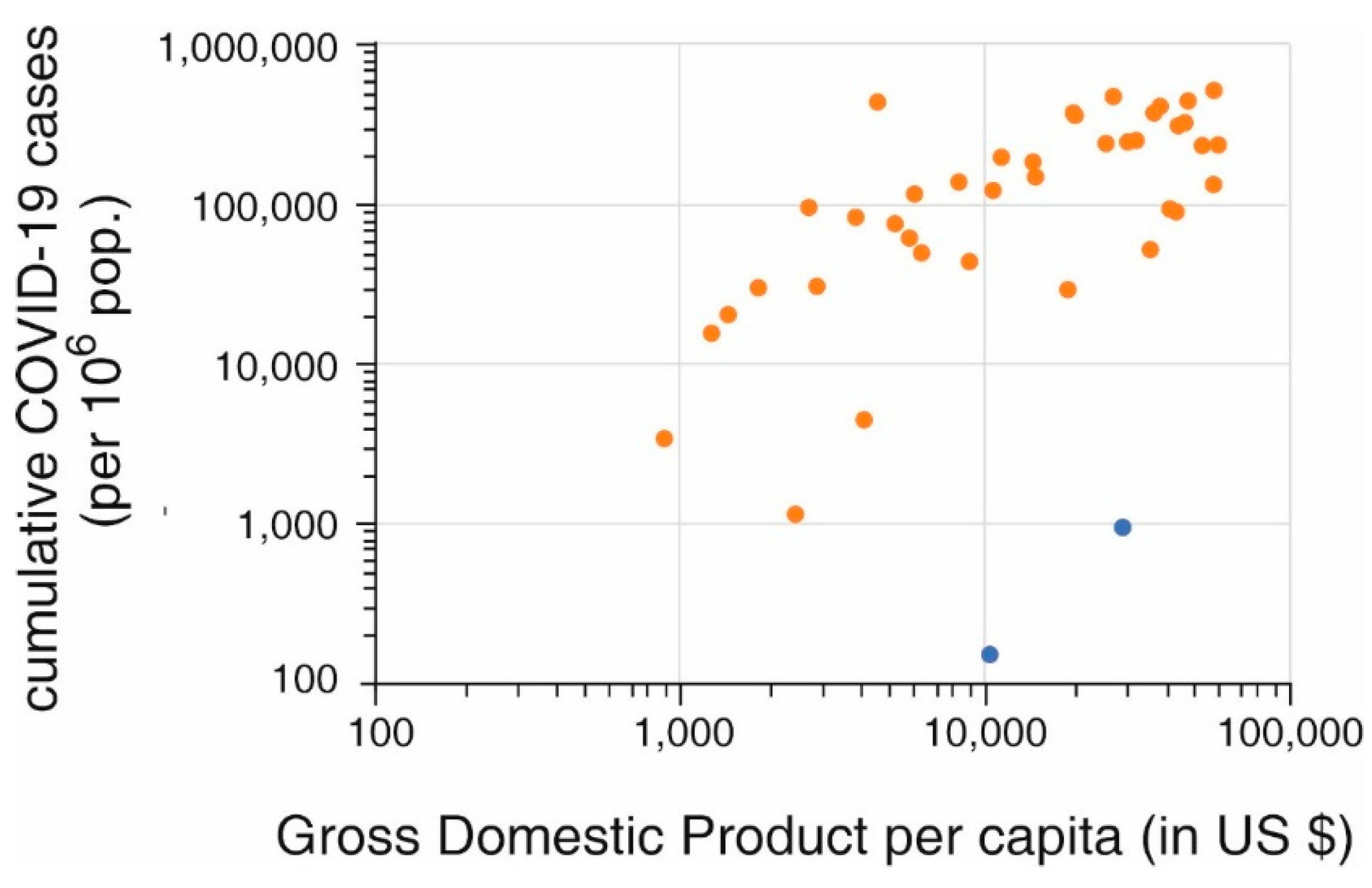
- Pardhan S, Drydakis N. Associating the Change in New COVID-19 Cases to GDP per Capita in 38 European Countries in the First Wave of the Pandemic. Front Public Health. 2021 Jan 20;8:582140. [CrossRef]
- Pettit SD, Jerome KR, Rouquié D, Mari B, Barbry P, Kanda Y, Matsumoto M, Hester S, Wehmas L, Botten JW, Bruce EA. 'All In': a pragmatic framework for COVID-19 testing and action on a global scale. EMBO Mol Med. 2020 Jun 8;12(6):e12634. [CrossRef]
- Gupta M, Wahl B, Adhikari B, Bar-Zeev N, Bhandari S, Coria A, Erchick DJ, Gupta N, Hariyani S, Kagucia EW, Killewo J, Limaye RJ, McCollum ED, Pandey R, Pomat WS, Rao KD, Santosham M, Sauer M, Wanyenze RK, Peters DH. The need for COVID-19 research in low- and middle-income countries. Glob Health Res Policy. 2020 Jul 1;5:33. [CrossRef]
- Dzinamarira T, Dzobo M, Chitungo I. COVID-19: A perspective on Africa's capacity and response. J Med Virol. 2020 Nov;92(11):2465-2472. [CrossRef]
- Burki, TK. Undetected COVID-19 cases in Africa. Lancet Respir Med. 2021 Dec;9(12):e121. [CrossRef]
- Català M, Pino D, Marchena M, Palacios P, Urdiales T, Cardona PJ, Alonso S, López-Codina D, Prats C, Alvarez-Lacalle E. Robust estimation of diagnostic rate and real incidence of COVID-19 for European policymakers. PLoS One. 2021 Jan 7;16(1):e0243701. [CrossRef]
- Msemburi W, Karlinsky A, Knutson V, Aleshin-Guendel S, Chatterji S, Wakefield J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature. 2023 Jan;613(7942):130-137. [CrossRef]
- Vandrevala T, Montague A, Terry P, Fielder MD. Willingness of the UK public to volunteer for testing in relation to the COVID-19 pandemic. BMC Public Health. 2022 Mar 22;22(1):565. [CrossRef]
- Taylor, L. Covid-19: Omicron drives weekly record high in global infections. BMJ. 2022;376:o66. [CrossRef]
- Willyard, C. What the Omicron wave is revealing about human immunity. Nature. 2022 Feb;602(7895):22-25. [CrossRef]
- Kishore K, Jaswal V, Pandey AK, Verma M, Koushal V. Utility of the Comprehensive Health and Stringency Indexes in Evaluating Government Responses for Containing the Spread of COVID-19 in India: Ecological Time-Series Study. JMIR Public Health Surveill. 2023 Feb 10;9:e38371. [CrossRef]
- Liu Y, Rocklöv J. The effective reproductive number of the Omicron variant of SARS-CoV-2 is several times relative to Delta. J Travel Med. 2022 ;29(3):taac037. 31 May. [CrossRef]
- Ren SY, Wang WB, Gao RD, Zhou AM. Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity, transmission, and vaccine resistance. World J Clin Cases. 2022 Jan 7;10(1):1-11. [CrossRef]
- Sharun K, Tiwari R, Dhama K, Rabaan AA, Alhumaid S. COVID-19 vaccination passport: prospects, scientific feasibility, and ethical concerns. Hum Vaccin Immunother. 2021 Nov 2;17(11):4108-4111. [CrossRef]
- Hall MA, Studdert DM. Privileges and Immunity Certification During the COVID-19 Pandemic. JAMA. 2020 Jun 9;323(22):2243-2244. [CrossRef]
- Andeweg SP, de Gier B, Eggink D, van den Ende C, van Maarseveen N, Ali L, Vlaemynck B, Schepers R, Hahné SJM, Reusken CBEM, de Melker HE, van den Hof S, Knol MJ. Protection of COVID-19 vaccination and previous infection against Omicron BA.1, BA.2 and Delta SARS-CoV-2 infections. Nat Commun. 2022 Aug 12;13(1):4738. [CrossRef]
- Keyel AC, Russell A, Plitnick J, Rowlands JV, Lamson DM, Rosenberg E, St George K. SARS-CoV-2 Vaccine Breakthrough by Omicron and Delta Variants, New York, USA. Emerg Infect Dis. 2022 Oct;28(10):1990-1998. [CrossRef]
- Du Z, Hong H, Wang S, Ma L, Liu C, Bai Y, Adam DC, Tian L, Wang L, Lau EHY, Cowling BJ. Reproduction Number of the Omicron Variant Triples That of the Delta Variant. Viruses. 2022 Apr 15;14(4):821. [CrossRef]
- Wang C, Liu B, Zhang S, Huang N, Zhao T, Lu QB, Cui F. Differences in incidence and fatality of COVID-19 by SARS-CoV-2 Omicron variant versus Delta variant in relation to vaccine coverage: A world-wide review. J Med Virol. 2023 Jan;95(1):e28118. [CrossRef]
- Ward IL, Bermingham C, Ayoubkhani D, Gethings OJ, Pouwels KB, Yates T, Khunti K, Hippisley-Cox J, Banerjee A, Walker AS, Nafilyan V. Risk of covid-19 related deaths for SARS-CoV-2 omicron (B.1.1.529) compared with delta (B.1.617.2): retrospective cohort study. BMJ. 2022 Aug 2;378:e070695. [CrossRef]
- Lorenzo-Redondo R, Ozer EA, Hultquist JF. Covid-19: is omicron less lethal than delta? BMJ. 2022 Aug 2;378:o1806. [CrossRef]
- Kim YY, Choe YJ, Kim J, Kim RK, Jang EJ, Lee H, Yi S, Lee S, Park YJ. Vaccine Effectiveness Against Severe Disease and Death for Patients With COVID-19 During the Delta-Dominant and Omicron-Emerging Periods: A K-COVE Study. J Korean Med Sci. 2023 Mar 20;38(11):e87. [CrossRef]
- Dobrowolska K, Brzdęk M, Zarębska-Michaluk D, Rzymski P, Rogalska M, Moniuszko-Malinowska A, Szymanek-Pasternak A, Jaroszewicz J, Dutkiewicz E, Kowalska J, Sikorska K, Flisiak R. Differences between the course of SARS-CoV-2 infections in the periods of the Delta and Omicron variants dominance in Poland. Pol Arch Intern Med. 2023 Jan 5:16403. [CrossRef]
- Intawong K, Chariyalertsak S, Chalom K, Wonghirundecha T, Kowatcharakul W, Ayood P, Thongprachum A, Chotirosniramit N, Noppakun K, Khwanngern K, Teacharak W, Piamanant P, Khammawan P. Reduction in severity and mortality in COVID-19 patients owing to heterologous third and fourth-dose vaccines during the periods of delta and omicron predominance in Thailand. Int J Infect Dis. 2023 Jan;126:31-38. [CrossRef]
- Mahmoudi J, Xiong C. How social distancing, mobility, and preventive policies affect COVID-19 outcomes: Big data-driven evidence from the District of Columbia-Maryland-Virginia (DMV) megaregion. PLoS One. 2022 Feb 17;17(2):e0263820. [CrossRef]
- Gambau B, Palomino JC, Rodríguez JG, Sebastian R. COVID-19 restrictions in the US: wage vulnerability by education, race and gender, Applied Economics, 2022, 54:25, 2900-2915. [CrossRef]
- World Health Organization. Virtual press conference on COVID-19 & Other Global Health Emergencies. 17 March, 2023. https://www.who.int/publications/m/item/virtual-press-conference-on-covid-19---otherglobal- health-emergencies.
- Harris, E. WHO Declares End of COVID-19 Global Health Emergency. JAMA. 2023 Jun 6;329(21):1817. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





