1. Introduction
This paper presents the results of an experimental investigation for analyzing ribcage motion during respiration with a portable RESPIRholter device that is based on an IMU (Inertial Measuring Unit) sensor. The aim of the report is to propose a procedure for creating a database on respiration evaluation with numerical values of monitored motion of the ribcage looking at the sixth rib as the most representative one.
In general, respiration is evaluated looking at the respiration frequency, although using also measures of the rib cage motion too. There are three different methods that are currently used to evaluate respiration in terms of respiratory rate, namely using other physiological parameters such as ECG or peripherical blood oxygen saturation, considering movements of the rib cage, and measuring the inhaled or exhaled air flow. Spirometry, as a standard in clinical practice, is used to analyze the respiratory system status, requiring an active participation from the subjects under testing. An accurate method can be considered a procedure using a combination of accelerometer and gyroscope data to evaluate the respiration with an error of 0.7 respiratory acts [
1]. Other methods can be worked out with a minor efficiency like those using optical fibers with an error of 1 respiratory act [
1,
2] or piezoelectric-piezoresistive sensor with an error of even 1.8 respiratory acts [
1,
3]. Different techniques are also tried to monitor respiratory rate by measuring rib cage movements as for example reported in [
4,
5,
6,
7,
8] from research results. Limitations of these new methodologies are related to high cost, difficulty in practical implementation, and need of an operator during the testing. An interesting new method is based on the SENSIRIB device [
9,
10,
11] that still requires the presence of an operator during testing. The SENSIRIB device has been used as basis for the development of the RESPIRholter solution,[
12], as a convenient tool for respiration evaluation in a continuous monitoring of respiratory acts without any operator assistance. In addition, the device’s full functionality is accessibleby a patient using RESPIRholter on their own, with features of cost effective, lightweight, and comfortable aspects. Indeed, both RESPIRholter and SensiRib are able to collect more data from respiration acts than any other device, as for example angular motion and linear acceleration of the rib cage in terms of the sixth rib. In addition, this numerical measure of the ribcage motion permits an accurate evaluation of the respiration in terms of biomechanical aspects. In addition, the RESPIRholter device as presented in [
12] is a diagnostic device that does not require an active participation from the subject under testing and can be even used in non-reactive patients as those with dementia or children. Previous experiences with RESPIRholter, as in [
13,
14,
15] suggest the feasibility of the device for procedures in a campaign for deducing statistical data that can be used for future new diagnostics of respiration acts.
In this paper, the results of implementing RESPIRholter as a device for respiration monitoring during long periods are discussed, coming from a first pilot experimental campaign involving 10 healthy subjects and 7 patients at the Thoracic Surgery Unit of the University Hospital Policlinico Tor Vergata in Rome. This pilot experimental campaign explores, for the first time, the differences between volunteers and patients who underwent thoracic surgery in terms of numerical values by characterizing respiratory rate and respiratory act motion using angle displacement and acceleration of ribcage.
2. Materials and Methods
A practical evaluation of respiration can be worked out with numerical values by analyzing the motion parameters of the ribcage during respiration in terms of displacement of ribcage reference points and their motion quality. The experimental evaluation can be performed using RESPIRholter device in a procedure that can be planned for data collection during long periods and successive data elaboration, like for any other medical holter protocol.
2.1. Respiration characteristics
Respiration is a complex movement that involves the skeletal structure, the muscular complex, and various organs in addition to the pulmonary system, which is its main beneficiary. The resulting movement of the chest is indicative of the functionality and efficiency of the respiratory act, which takes the form of an adequate flow of air in the pulmonary system. Thus, respiration can be monitored and objectively evaluated by analyzing such ribcage motion in terms of both muscle actions and ribcage bone motions. The movement of the rib cage involves both the bone structure and the muscular structure in a synergistic way, determining not only characteristic movements but the consequent expansion and contraction of the lung tissues in precisely allowing the flow of air during respiration.
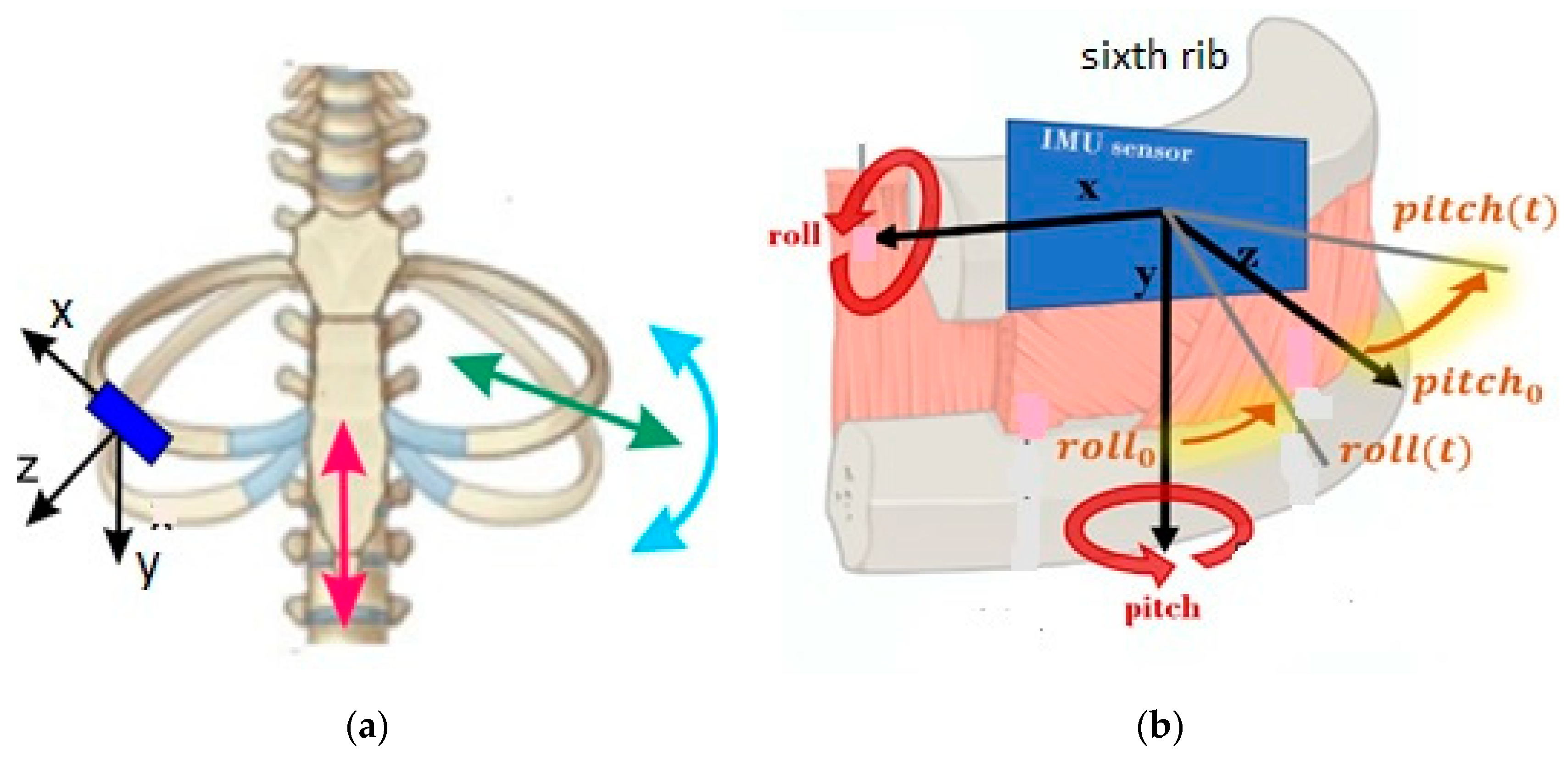
The ribcage motion during respiration can be characterized by four basic movements, as summarized in
Figure 1a). The so-called pump-handle movement is indicated by the red arrow in
Figure 1a) as referring to the sternum swinging upward and outward as produced by the rib system motion. The so-called bucket-handle movement is indicated by the light blue arrow in
Figure 1a) and it involves the lower ribs that moves laterally and upward as the handle of a bucket. The so-called caliper movement, indicated by the red arrow in
Figure 1a), is due to the lowest ribs swinging laterally. A very limited torsion movement is experienced by ribs when twisting around costovertebral joints.
The monitoring and numerical analysis of the movements in
Figure 1a) can be worked out by looking at the motion characteristics of a representative rib of the rib cage. Main motion data can refer to the movement frequency, angular excursions of the rib, and linear accelerations of a reference rib point as significant kinematic parameters for the quality and quantity of respiration motion.
Figure 1b) shows a scheme for a measuring system of those motion parameters of a respiratory act by using an IMU (Inertial Measuring Unit) as detecting sensor in a properly located position on a rib by considering the sensing reference axes. The roll angle is the rotation angle about X axis of the sensor reference whereas the pitch angle is a rotation around the Y axis, as shown in
Figure 1b). Correspondingly the acceleration components of the rib reference point are those of the origin of the sensor reference frame. Thus, the accelerometer and gyroscope of the IMU can acquire those data with a proper sampling frequency.
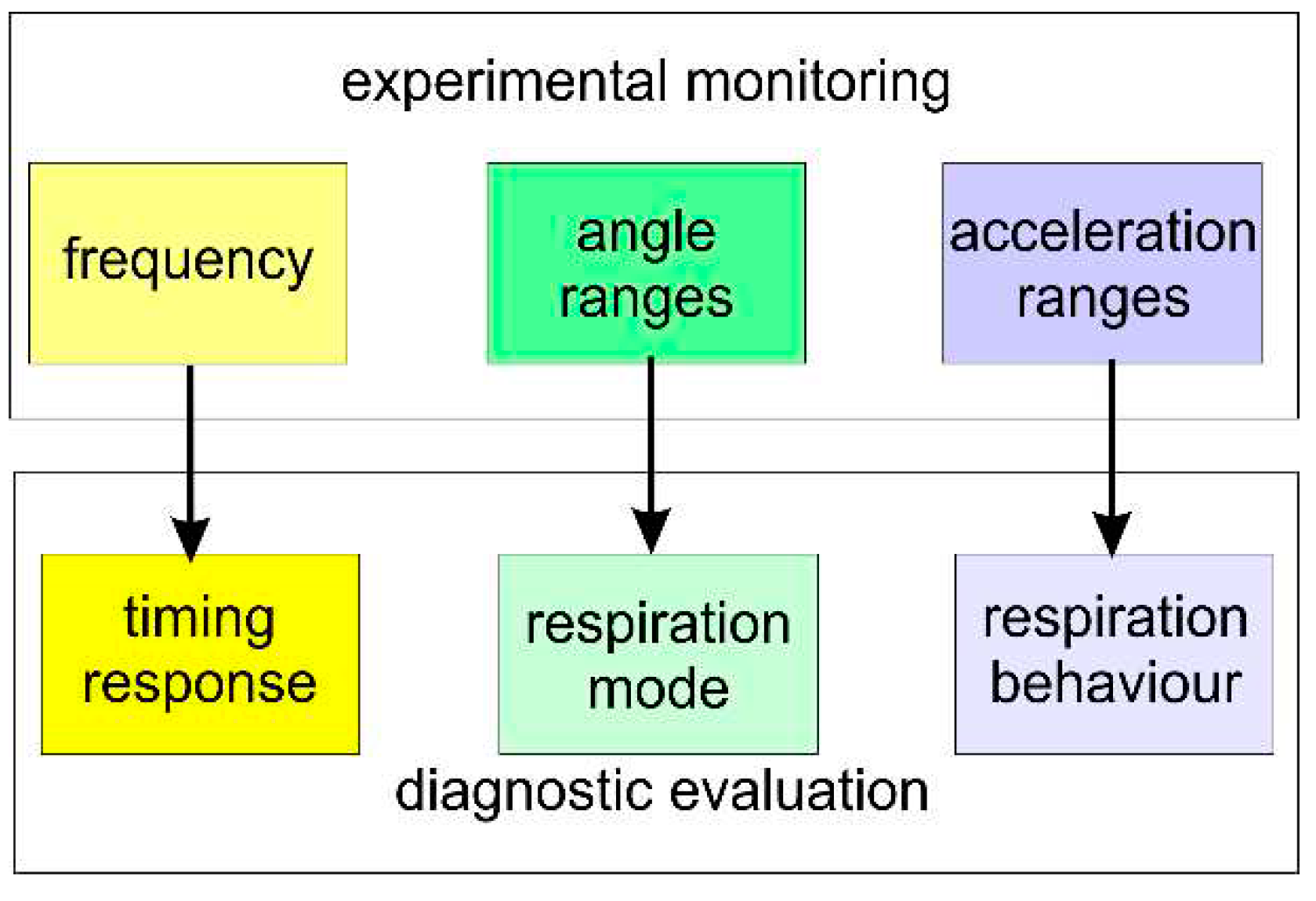
Such an acquisition of the time data can be evaluated as a characteristic of respiration with values of the respiratory frequency; the angular excursions can be indicative of the respiration efficiency; and the acceleration ranges can be useful in evaluating the quality of the respiratory act, as summarized in
Figure 2.
2.2. Respiration Evaluation by Means of RESPIRholter
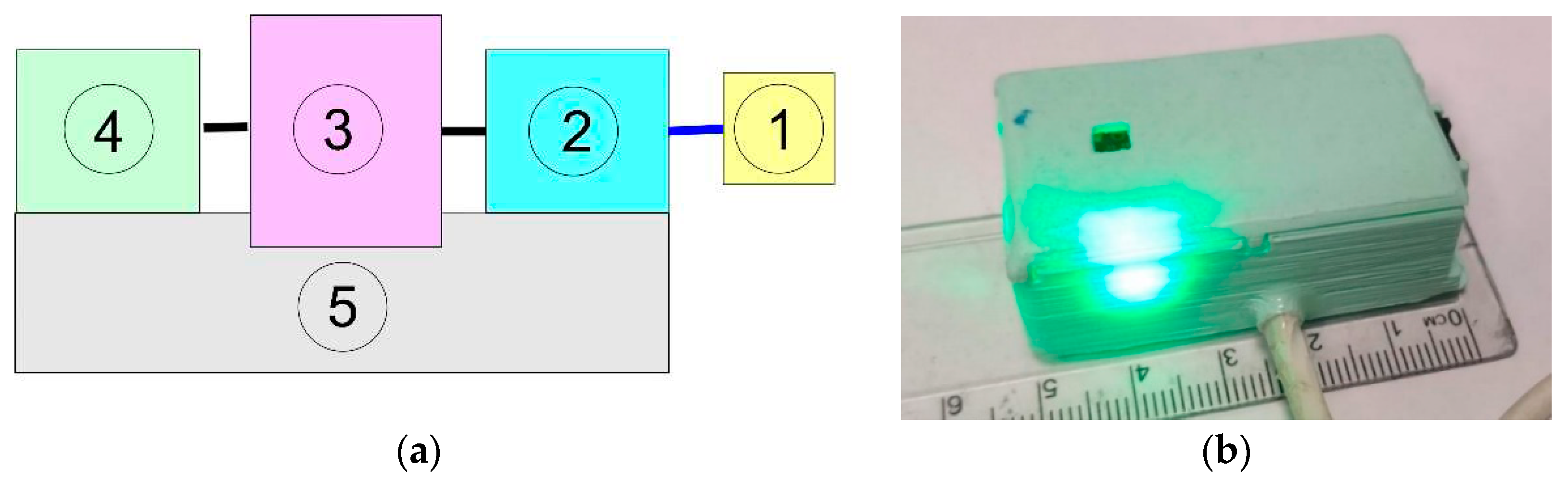
To acquire rib motion data, a specific device was designed, named RESPIRholter [
12,
13], whose aim is to acquire specifically acceleration and angle ranges of the VI cost that is considered the most representative of the ribcage motion during respiration. The measured angle ranges reflect the expansion of the rib cage, since the more the rib rotates, the more the volume of the rib cage increases with corresponding airflow. The acceleration of a reference point on the rib give indication on the smoothness and regularity of respiratory acts while looking at the second order kinematics of the motion to measure respiration behavior not in general directly appreciated by just vision inspection. Thus, the used IMU as the sensing unit of the RESPIRholter device acquires the acceleration components along the three axe of the reference frame and the roll and pitch angles of the VI rib according to the scheme in
Figure 1b) within the structure of the device illustrated in
Figure 3a). One the main features of the RESPIRholter device is summarized in the prototype in
Figure 3b) showing the small design with a lightweight structure that permit a fairly easy installation and usage.
The main frame of the RESPIRholter prototype is the box that contains an Arduino NANO 33 IoT board equipped with a 6-axis LSM6DSL IMU sensor. A MicroSD is included as storage unit, powered by the 5 V power output of the Arduino microcontroller. The device communicates the starting in-operation to the user through blink sequences of a low power LED with just 1W of power consumption, including alert of malfunctioning with LED lighting frequency. The power supply is provided by a power bank through a micro-USB connector cable. The RESPIRholter prototype has a size of 55mm x 30mm x 16mm and weighs only 33 g, as shown in
Figure 3b).
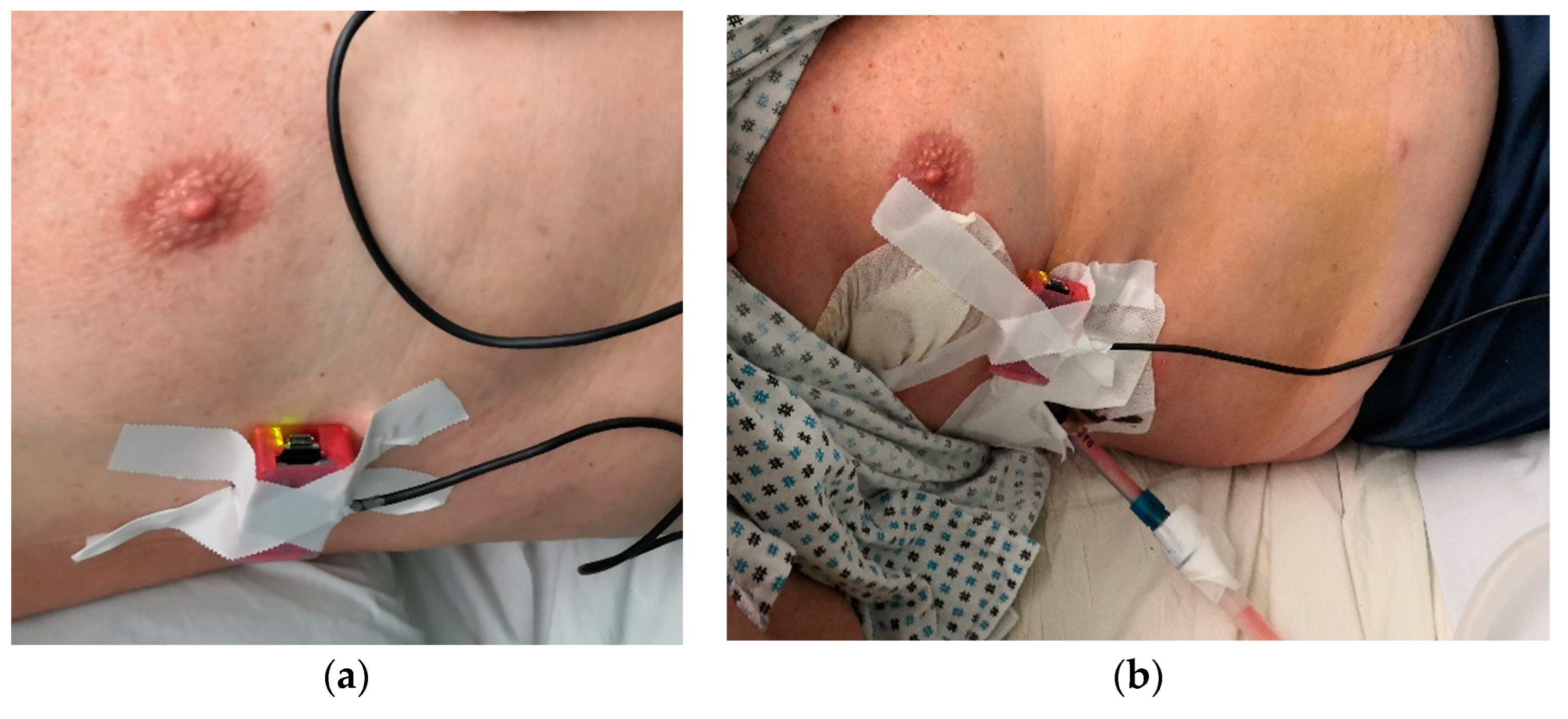
The small and lightweight design of the RESPIRholter prototype permits an easy installation of the device on the rib VI of a person, either in a healthy person or in a thoracic operated patient, as shown in
Figure 4, with a quite comfortable set up.
2.3. Procedure for a Campain of Testing
RESPIRholter was set up to perform a 6-hour long operation with acquisition sampling of 1 minute each 20 minutes for each motion parameter. The acquired data are elaborated through a customized user-friendly RESPIRholter code in MATLAB with a post-processing check that can be adjusted with diagnostic-like comments by a physician. Clicking on preview option, a physician operator can have a quick look at the acquisitions and eventually acquisitions can be deleted when they are not considered valid, while on the contrary, clicking on execute option, the data acquisition and post-processing elaboration are operated automatically up to a final summarizing report.
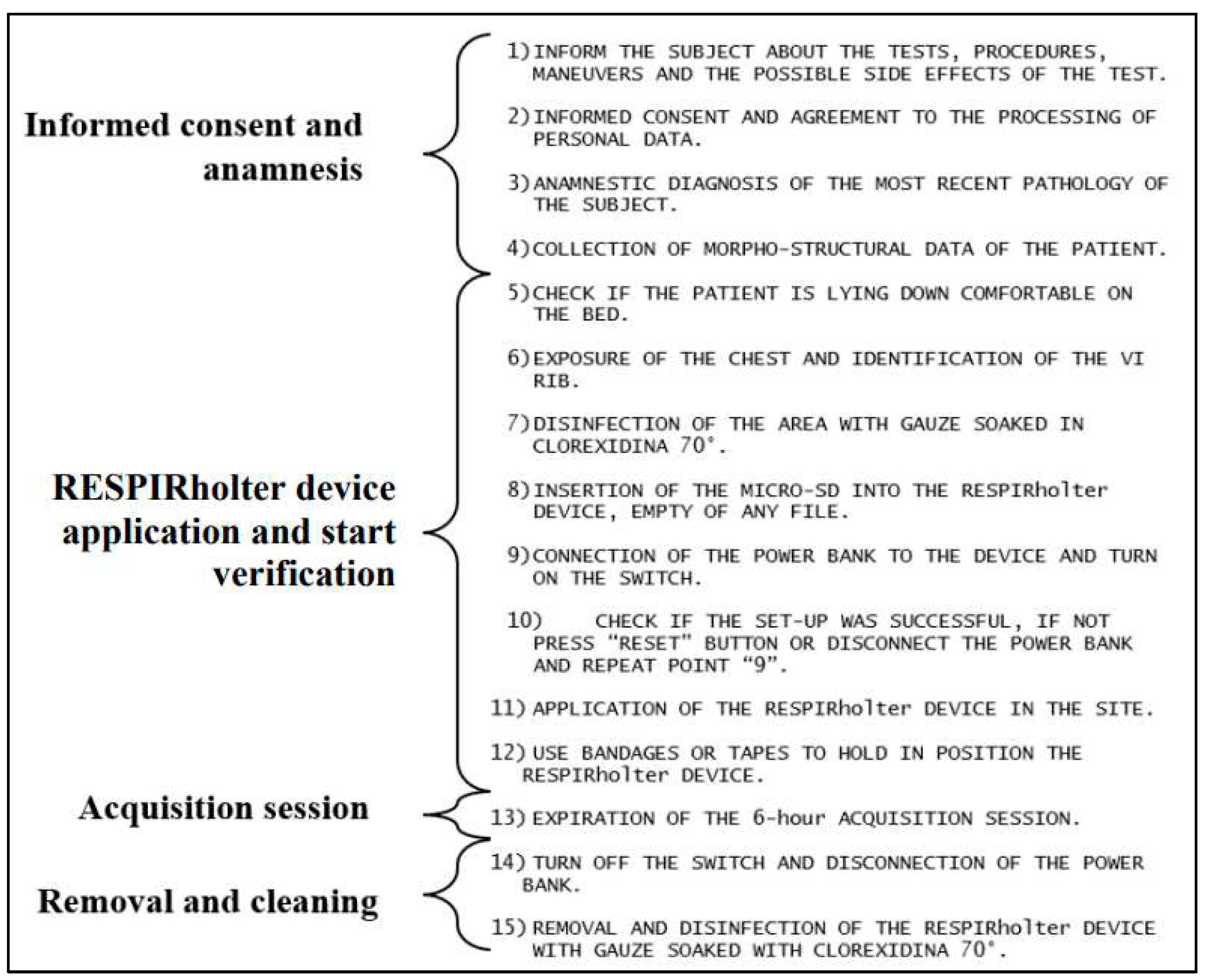
The testing procedure is designed together with a specifically designed protocol to standardize the experimental conditions and the activity during testing as summarized in the step-by-step list in
Figure 5.
The first step with points 1 to 4 is to give and collect data for the informed consensus from a patient under testing. The purpose of the testing, the processing of personal data, and how the experiment will be carried out are explained in detail to permit a patient to sign an informed consent form. A brief medical anamnesis interview is then carried out including the identification of anthropometric data such as height and weight, biographical data, and relevant information about behaviors, diseases, and previous surgeries.
The second step with points 5 to 12 refers to the preparation and application of the RESPIRholter device. The intersection between the anterior axillary line and the sixth rib is identified as the point of application, and the area of the thorax is disinfected with chlorhexidine 2%. Then, the device is prepared and tested once connected to a power bank as to be ready to be fixed with silk patch as shown in the example in
Figure 4.
The third step with point 13 refers to the acquisition session lasting six hours during the night with the patient lying on the bed.
The last step with points 14 and 15 is run to remove the RESPIRholter device and re-disinfecting the device and the surrounding skin of the patient where the device was installed.
In the post-processing data elaboration, the first step is to divide each acquisition into five segments with same time duration including all the initial and final intervals with all data. Then, the designed RESPIRholter code automatically computes an algebraic average of the five acquisitions for each motion parameter. The acquired data are stored and then visualized in the form of plots. The average of all the acquisitions is obtained next as the algebraic average of the averages yet. In addition, the RESPIRholter code is designed to permit the physician to select a representative plot and a selected plot as per diagnosis purposes in a synthetic representation of the results. An automatic report will contain those main representative plots to facilitate a physician to have a summarized view of the acquired data of the motion parameters during respiration in the 6 hours of sampling.
The above procedure is well suited to be used in a campaign of testing with several volunteers under testing to collect results of comparable value for a statistically significant evaluation of the respiration characteristics. Considering the statistical prescription to identify a proper number of samples as reported in [
16] and looking at the possible volunteers of chest operated patients in a reasonable period of few months, a first campaign was planned to have at least 7 patients as the recurrent number in the report [
16], even if not in the same range of age.
3. Results
An experimental campaign was planned with a group of 10 chest operated patients and a group of 10 healthy volunteers to have a comparison of the operation effects and the recovery status after a thorax surgery operation. Unfortunately, only 7 patients were finally available with proper characteristics of chest operation. Each test was conducted following the designed protocol in
Figure 5 with satisfactory results referring to the angles and acceleration components of the reference point including a medical-clinical analysis of interpretation of the acquired data. In addition, during the testing several reasons and occurrences, like unexpected malfunctioning due to patients’ movements and acquisition stopping for patient walking to bathroom, the number of valuable acquisitions during the six-hour period were reduced to 10 to have the same number for all the tested person. Thus, the results elaboration was conducted on the best or valid 10 acquisitions of 1 minute during the six-hour period.
As an illustrative example, a case study is reported to show the results of the procedure with results valuable in a testing campaign with comparable results among the tested volunteers, either healthy one or patient ones. The reported case of study is also useful to prove that the experimental numerical evaluation of respiration can be of practical significance and even of the expected utility in a clinical diagnosis.
3.1. Results of an Illustrative Case of Study
The case study refers to the first test in the campaign and reports results for a 59-year-old man with a BMI of 34.2, who was operated for a pulmonary lobectomy surgery. The data acquisition in his chest operated condition was worked out during the night between the first and second postoperative day. The RESPIRholter device was installed at the intersection angle between the sixth rib and the anterior axillary line on the left hemithorax,
Figure 4 in agreement with the protocol in
Figure 5. A pleural drainage was applied during surgery at the fourth intercostal space with no interference with RESPIRholter device. The patient on the first postoperative day was monitored with a good respiration by good peripheral oxygen saturation. On the second postoperative day, peripheral oxygen saturation was down to SpO2 92% (good condition are usually indicated with >94%) so that an oxygen therapy was applied in nasal cannulae with 2 liters/min.
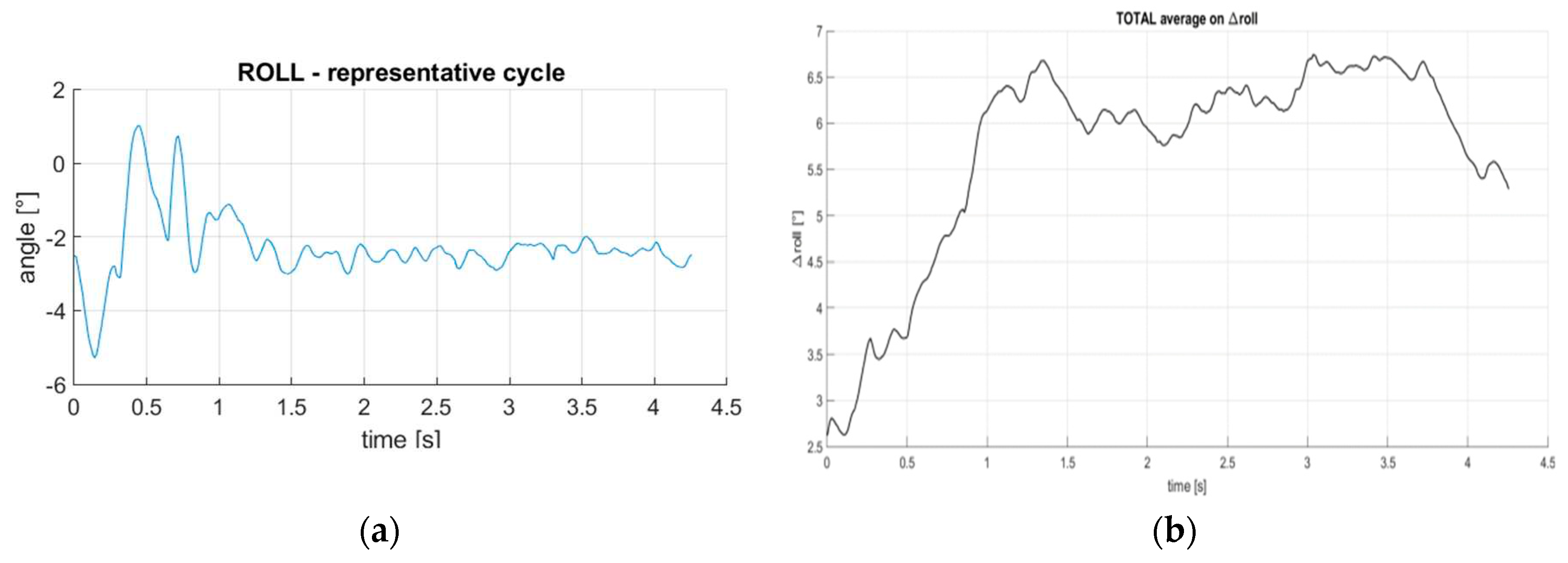
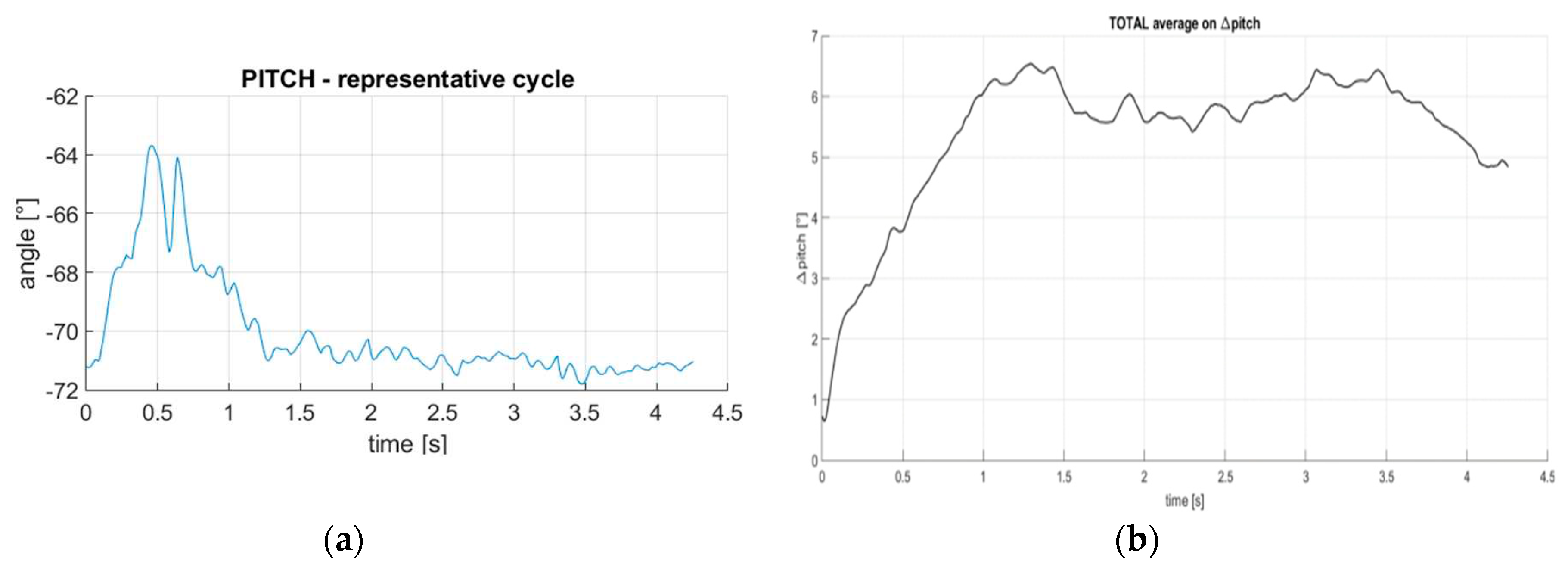
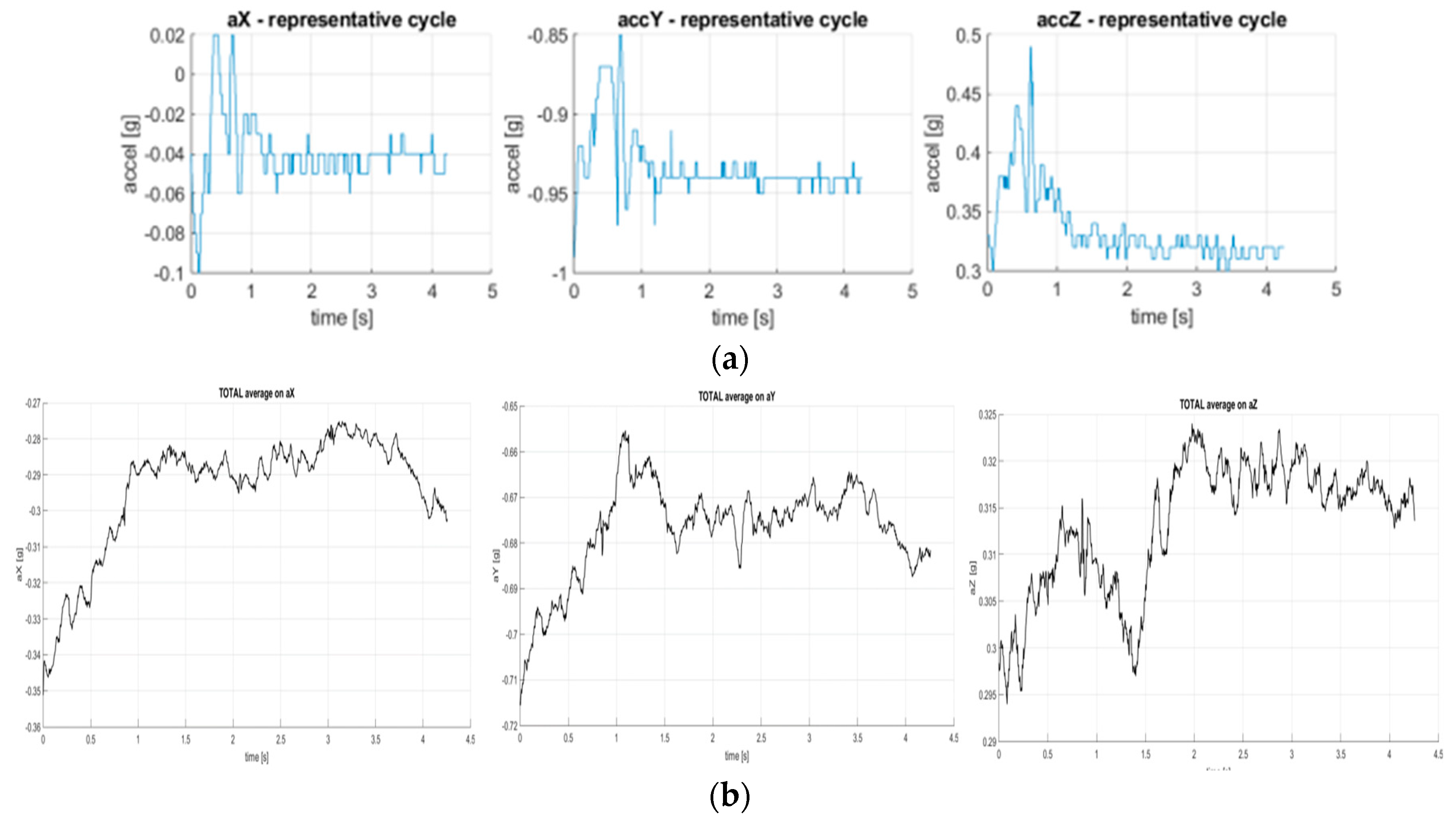
The results of data acquisition are summarized in the plots in
Figure 6,
Figure 7 and
Figure 8 referring both to direct representative acquisitions and average computation results.
The elaboration and interpretation of the acquired have detected respiration of the patient throughout the six hours of acquisition with regular breathing cycles followed by a stage of apnea.
Figure 6a) for roll angle shows the typical kinematics of respiration with apnea period that is indicated by the loss of cyclic motion replaced by a quasi-constant motion. The numerical variations on the main motion can be due both to the real functionality of respiration with not a smooth behavior and, mostly, to the compliance of the skin and adipose layer tissue in correspondence of the rib where ethe IMU is installed. Of clinical significance for the apnea condition is the roll range of the movement which can be noted of about 6 deg in the first part as regular cyclic part in contrast with the quasi-stationary phase of the apnea.
Figure 7b) that is calculated from the average of the average cycles, does not clearly detect such an apnea condition that seems to have few occurrences during the period of the acquisitions, although the effect is evident in a loss of a clear cyclic behavior that is nevertheless characterized by a roll average range of about 6 deg yet.
Similar situation is detected in the plots in
Figure 7 representing the acquired pitch motion with the anomaly of the apnea condition that is characterized by a first cyclic part followed by a quite longer quasi-stationary ribcage motion. Gain the angular variation is a significant parameter with almost 8 deg in addition to the temporal evolution.
The data acquired in terms of acceleration components as reported in
Figure 8 and
Table 1, confirm even more clearly the anomaly of the respiration with apnea. In particular, in
Figure 8a) data acquired with respect to X axis show a reduction in accelerations during the stationary apnea phases with respect to the cyclic phase indicating an excessive stationarity of the respiratory movement up to a minimum range of 0,02 g. In
Figure 8b) the few apneas seem not affecting the average values and a cyclic behavior is still observable. Similarly, the Y acceleration component shows a similar reduction of the acceleration variation in the stationary phase up to less than 0.02 g with the average computation with small values due to the more limited motion in general. Even more significant is the result with the acquired acceleration along the Z axis with a very limited cyclic part and a strongly reduced value for the quasi-stationary apnea period from almost 0.8 g up to less than 0.02 g. The main numerical data are summarized in
Table 1 as those coming from the 10 valid acquisitions during the six-hour period of acquisitions.
3.2. Statistic Elaboration of Testing Results
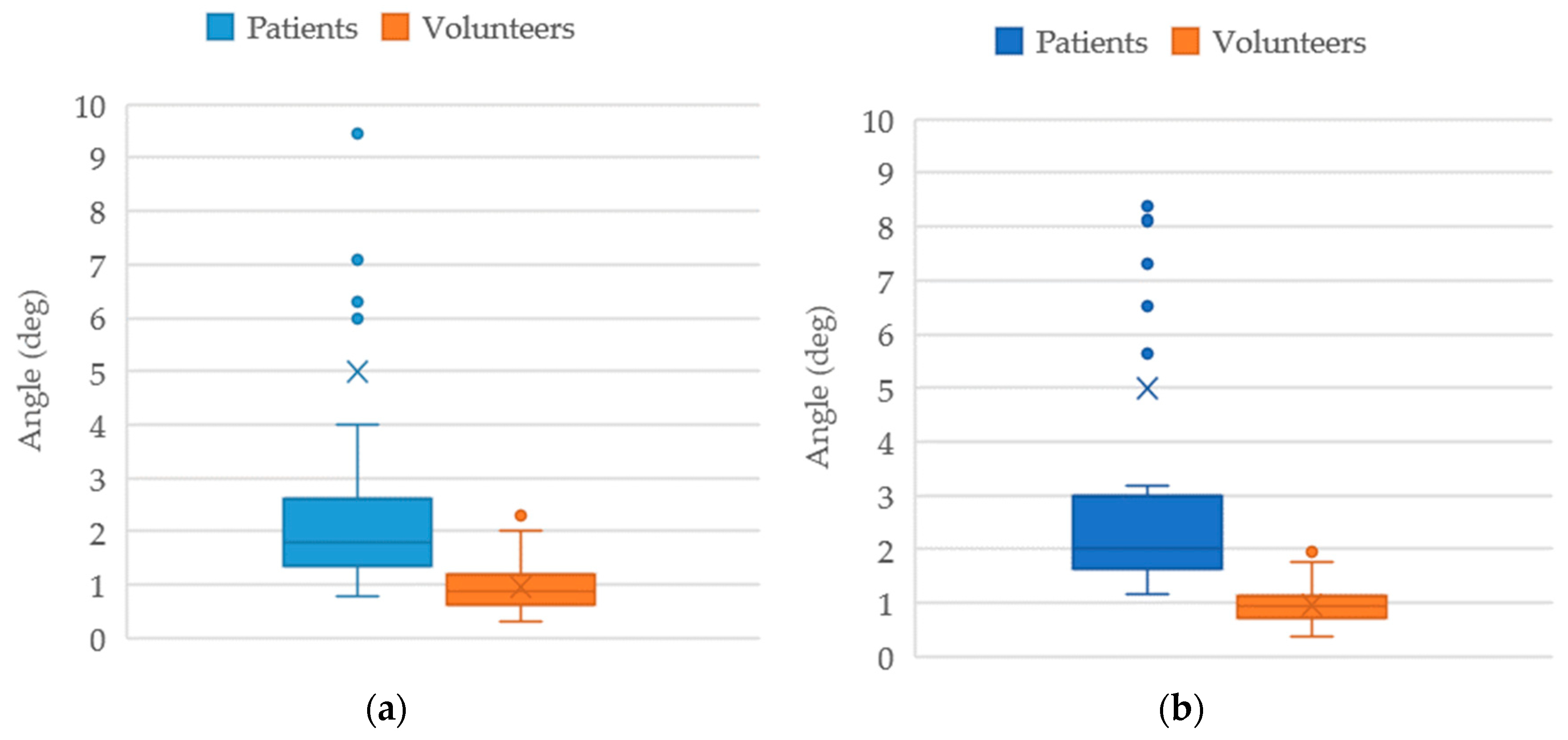
A statistical elaboration of the data results during this first campaign from tests with 7 chest operated patients and 10 healthy volunteers is reported in
Figure 9,
Figure 10 and
Figure 11.
Descriptive statistics have been performed for healthy volunteers or patients after surgery. With these first campaign results, the sample size does not consent the execution of a parametric statistical elaboration. In
Figure 9a), the average roll motion shows a difference from 0.97 deg in healthy people to 4.99 deg in patients after surgery, with a much larger standard deviation. In
Figure 9b), the average pitch motion gives a difference from 0.96 deg in healthy people to 5.00 deg in patients after surgery, again with a much larger variability in behavior. This indicates that the operated patient shows a respiration motion with much maximal type breathing and larger rib motion that in healthy people, as indicated by the value of increased average and range.
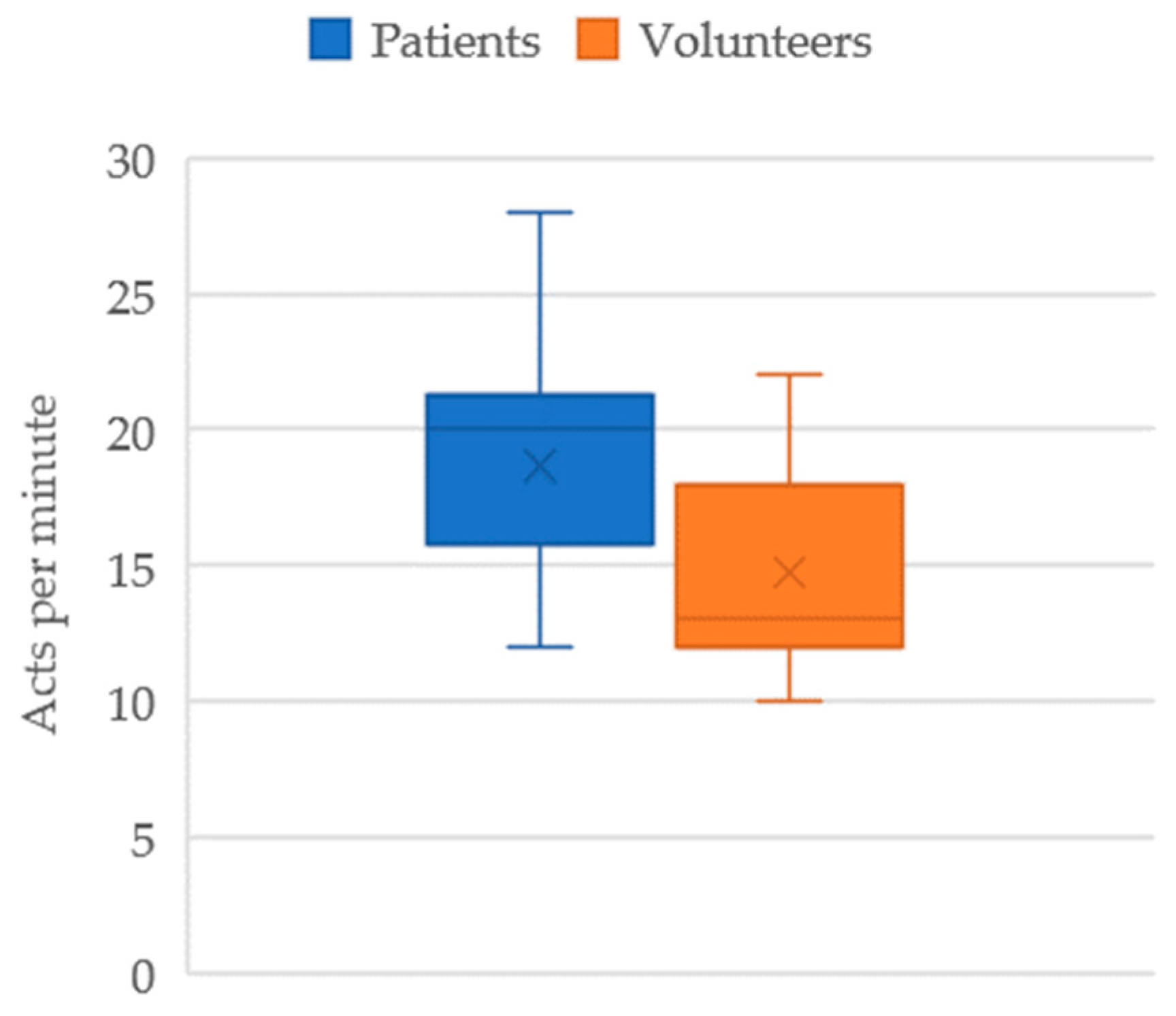
This behavior is also reflected in the respiratory rate statistics in
Figure 10, which shows a difference from 13acts/minute in healthy volunteers (that is in agreement with the literature as in [
1]), to 20.00acts/minute in patients after surgery. The respiratory rate is, therefore, increased in patients after surgery who appear to be tachypneic as indicated by the larger value of the average in addition to the higher standard deviation.
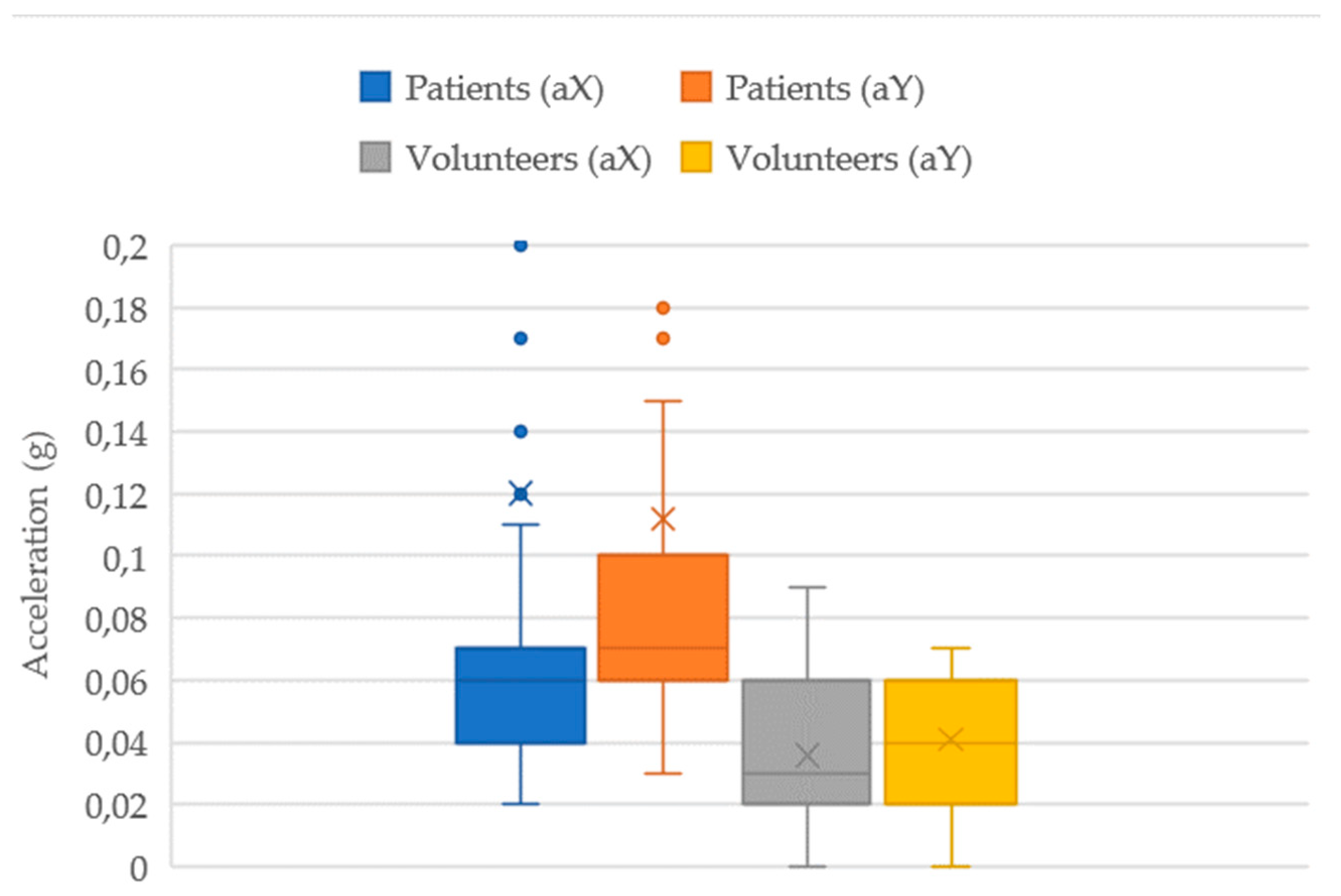
In
Figure 11 the statics elaboration results are reported referring to the variations of the X and Y acceleration components neglecting the Z component that does not show significant variation. The X and Y acceleration components in standard deviation remains quite similar in healthy volunteers whereas the average is detected almost equal. On the contrary, in patent volunteers the Y acceleration components shows much larger deviation with an increased average with respect to X components. The boxplots in
Figure 11 indicate that healthy volunteers show a smooth rib cage motion both in X-axis (laterally) and the Y-axis (downward), whereas patients after surgery show a staggered downward (Y) motion when compared to the lateral (X) component. The results indicated that in general the patients after surgery perform a respiration with a ribcage motion that is characterized by a deeper faster breathing similar to a maximal regular type with a ragged breathing.
In summary, the first campaign results give a first database of respiration statistic characteristics of patients after surgery with values that have been used for comparison of data of healthy volunteers to show the soundness and feasibility of the proposed database and procedure yet.
5. Conclusions
The paper presents results of a first campaign of testing by comparing data of an experimental respiration evaluation from healthy people and thorax operated-surgery operated patients. The reported results show clear numerical values that can be used for diagnostic purposes. Indeed, the aim of the work is to propose a procedure that can be useful to create a suitable database with the selected numerical parameters of rib cage motion during respiration using the biomechanical movement of sixth rib. A first database can be even considered with the results of this first testing campaign, giving clear indication of aspects for future work in more proper selection of tested subjects with proper common characteristics and conditions, and in plans for more repeated tests during the pre an postoperative period.
6. Patents
Marco Ceccarelli, Portable device for measuring the movement of human ribs, Patent no. IT. 102021000005726, 21-3 2023.
Marco Ceccarelli, Vincenzo Ambrogi, Lucrezia Puglisi, Matteo Aquilini, Ventilatory holter device, Patent no. IT. 102021000008585, 18-4-2023.
Author Contributions
Conceptualization, M.C. and V.A.; methodology, M.C., M.D., V.A. and M.R.; software, M.D. and M.R.; validation, M.D. and M.R; formal analysis, M.C., M.D., and V.A.; investigation, M.C., M.D., V.A. and M.R.; resources, MC and V.A.; data curation, M.D. and M.R.; writing—original draft preparation, MC. and M.D.; writing—review and editing, M.C., M.D., V.A. and M.R; visualization, MC. and M.D.; supervision, MC. and V.A.; project administration, M.C.; funding acquisition, M.C.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Policlinico di Tor Vergata, Rome, with protocol code RS. 197.22 on 15 November 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Liu H, Allen J, Zheng D, Chen F. Recent development of respiratory rate measurement technologies. Physiol Meas. 2019 Jul 1;40(7):07TR01.
- Krehel M, Schmid M, Rossi R, Boesel L, Bona GL, Scherer L. An Optical Fibre-Based Sensor for Respiratory Monitoring. Sensors. 2014 Jul 21;14(7):13088–13101.
- Yang J, Chen B, Zhou J, Lv Z. A Low-Power and Portable Biomedical Device for Respiratory Monitoring with a Stable Power Source. Sensors. 2015 Aug 11;15(8):19618–19632.
- Alfverti, A., Cesareo, A.: A wearable device for the continuous monitoring of the respiratory rate, patent nr. WO 2019/012384, Italy, 11 January 2019.
- Ciocchetti, M., et al.: Smart textile based on fiber bragg grating sensors for respiratory monitoring: design and preliminary trials. Biosensors 5(3), 602–615 (2015).
- Freeman J. F. et al., Devices and methods for respiratory variation monitoring by measurement of respiratory volumes, motion and variability, patent WO2012021900A1, 16.02.2012.
- Devices and methods for respiratory variation monitoring by measurement of respiratory volumes, motion and variability, Patent WO2012012384A1 of 2019.
- Gentili Biffi G., Device for monitoring of respiration functions, patent IT1222263B, Italy, 21/06/1990.
- Ceccarelli, M.: Portable device for measuring the movement of human ribs, patent n. 102021000005726, Italy, 13 March 2021.
- Ceccarelli, M., Puglisi, L., Mesiti, F., Aquilini, M., Ambrogi, V.: A device for experimental characterization of biomechanics of breathing and coughing. In: 26th ABCM International Congress of Mechanical Engineering, Florianópolis, paper COB-2021-0273 (2021).
- Ceccarelli, M., Papuc, P.E., Taje, R., Aquilini, M., and Ambrogi, V.: A Biomechanics Analysis of Ventilation in Thorax Operated Patients. International Journal of Clinical Studies & Medical Case Reports 15(1), 1-3 (2021).
- Ceccarelli, M., Ambrogi, M., Puglisi, L., Aquilini, M.: Ventilatory holter device, patent no. IT102021000008585, Italy, 18-4-2023.
- Aquilini, M.: RESPIRholter a device for breathing monitoring, master thesis in mechatronic engineering. University of Tor Vergata, Roma (2022).
- Aquilini, M., Ceccarelli, M.: Design and Testing of RESPIRholter Device for Respiratory Monitoring In: Niola, V., Gasparetto, A., Quaglia, G., Carbone, G. (eds) Advances in Italian Mechanism Science-IFToMM Italy 2022 pages 480-488. Springer, Cham. [CrossRef]
- Aquilini, M., Ceccarelli, M., D’onofrio, M., Ambrogi, V.: An Experimental Characterization of Respiration Biomechanics by a Holter Device. In: Proceedings of 5th Jc-IFToMM International 2022, Volume 5, Pages 80-87. ISSN 2436-9330. [CrossRef]
- Chiaromonte C., Calculation of the sample number, Internal report, University of Rome Tor Vergata, Rome, 14/07/2020. (in Italian).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).