1. Introduction
Since 2019, a new coronavirus infecting humans has been actively circulating around the world. SARS-CoV-2, which is responsible for this pandemic, mainly causes upper and/or lower respiratory tract infections. A progression of these symptoms to more severe forms such as acute distress respiratory syndrome (ADRS) and eventually death is possible and is more likely to appear in patients with risk factors and / or comorbidities including obesity, diabetes, age, hypertension, and cancer [
1]. “Mild” forms of this disease, mainly occurring in young patients, represent most cases and their symptoms disappear after 5 to 14 days. However, silent or asymptomatic hypoxaemia, a clinical presentation specifically reported in COVID-19, is present in a third of patients upon hospital admission and is associated with a very poor outcome [
2]. The lowest recorded pre-hospital oxygen saturation level (O2Sat) predicts death vs discharge such that with every 1% reduction in the lowest O2Sat levels, there is a 13% increase in the odds of an in-hospital death [
3]. The initial home O2Sat level predicts subsequent hospitalization [
4]. Similarly, pulmonary embolism (PE) has been reported to have a 24% cumulative incidence in patients with COVID-19 pneumonia [
5], and abnormal elevated D-dimer levels are associated with thrombosis, poor prognosis and/or increased mortality [
6]. D-dimer levels of >2.590 ng/mL was associated with a 17-fold increase in an adjusted risk of PE in hospitalized patients and was the strongest independent predictor of symptomatic venous thromboembolism (VTE) in patients with COVID-19 [
7]. These features suggest that the administration of early VTE prophylaxis with either unfractionated heparin or low molecular weight heparin could be prescribed in outpatients with risk factors to prevent these thromboembolic phenomena [
8]. Finally, there is increasing evidence that the use in the pre-hospital setting of the News2 score can predict critical illness and improve patient outcomes [
9].
Consequently, early management, at the pre-hospital stage, of patients diagnosed with COVID-19, including evaluating clinical characteristics and comorbidities, screening for happy hypoxemia, NEWS2 score, oxygen saturation, D-dimer titration, by a health professional, are all elements that can have an impact on the prognosis of the disease [
10]. Pre-hospital treatment is likely to have an impact on hospitalizations, resuscitations, and deaths. In this study, we aim to investigate the different pre-hospital pathways of COVID-19 patients treated at our institute [
11], and to evaluate the impact of these pathways on outcomes in term of hospitalization, resuscitation, and death.
2. Materials and Methods
The pre-hospital pathway (PHP) is defined as the set of stages the patient goes through from the onset of symptoms (OS) to their admission to hospital. These different stages generally involve community health professionals, in health facilities (pharmacies, health centers), as well as in medico-social structures when it comes to diagnostic or screening tests, various treatments or monitoring (blood test, oxygen saturation). Some people prefer treatment at home involving consultations with general practitioners or specialists to receive treatment, diagnosis and monitoring.
The study was submitted for approval in advance to an Independent Ethical Committee (IEC) which gave a favorable opinion (No. 2022-010). The IEC considered that this study does not fall under French bioethical law and complies with regulations on the processing of medical data and the Helsinki declaration. The investigators’ declaration to comply with reference method MR 004 was filed prior to this study and was the subject of a declaration in the GDPR/APHM Register No.2020-151.
This is a retrospective study using medical data collected prospectively in 2022, by physicians during the medical treatment of patients presenting at the Institut Hospitalo-Universitaire (IHU) Méditerranée Infection for treatment after being diagnosed with COVID-19. Data recorded between 1 February and 7 March 2022 were selected and extracted from the hospital database for this study. Data from people who objected to their use were excluded.
The primary outcomes in terms of the variables of interest were defined as the number of hospitalizations, resuscitation, and deaths in the study population at the time of interview and in the subsequent 30 days. The explanatory variables were time from OS to treatment (calculated from the recorded dates of events), age, gender, News2 score, medical history (risk factors for COVID-19 disease; diabetes, elevated blood pressure, obesity, cancer, previous episode of COVID-19), symptoms, and treatments, as well as D-dimers levels. In order to complete the descriptive analysis, we asked the hospital information system to check whether any patients in the cohort had been hospitalized, transferred to intensive care, or died in the 30 days following this study.
For the purposes of the study, some data were recoded and, if necessary, created to identify the relevant explanatory variables. The missing data from the modalities of variables, such as the News2 score, were imputed so that the analyses were as relevant as possible.
An estimate of the number of individuals to include was calculated based on the prevalence of the primary outcome (hospitalization rate) in a COVID-19 cohort of > 10 000 patients between wave 1 and wave 4 [
11]. The average prevalence of hospitalization in this cohort was 2.7%, with a decrease of 30% in the last period. The sample size required for a descriptive study in a population of 30 000 patients previously followed in the IHU, with a main event frequency (hospitalization rate) of 2% and an acceptable margin of error of 5% for a 99.9% confidence interval was 85 individuals.
We first describe the population and the main PHPs with their respective duration between OS and presentation at hospital. In a second step, we evaluate the risk factors associated with the outcome using univariate logistic regression. We then used multivariate binary logistical regression to estimate the association between the risk of hospitalization and these care pathway among the other risk factors recognized in the literature (age, obesity, comorbidities, treatments, etc.). Multivariate analysis was modelled using a step-by-step ascending binary logistic regression (Wald) and is confirmed by step-by-step descending binary logistic regression (Wald). Non-significant differences or associations were considered when the p value was >0.05. Variables excluded from the multivariate model-analysis were those for which p values were >0.20 in univariate analysis, if data concerns only a sub-group of the total population or variable redundancy with others in the model. Univariate and multivariate analyses were performed using IBM SPSS Statistics.
3. Results
3.1. Data
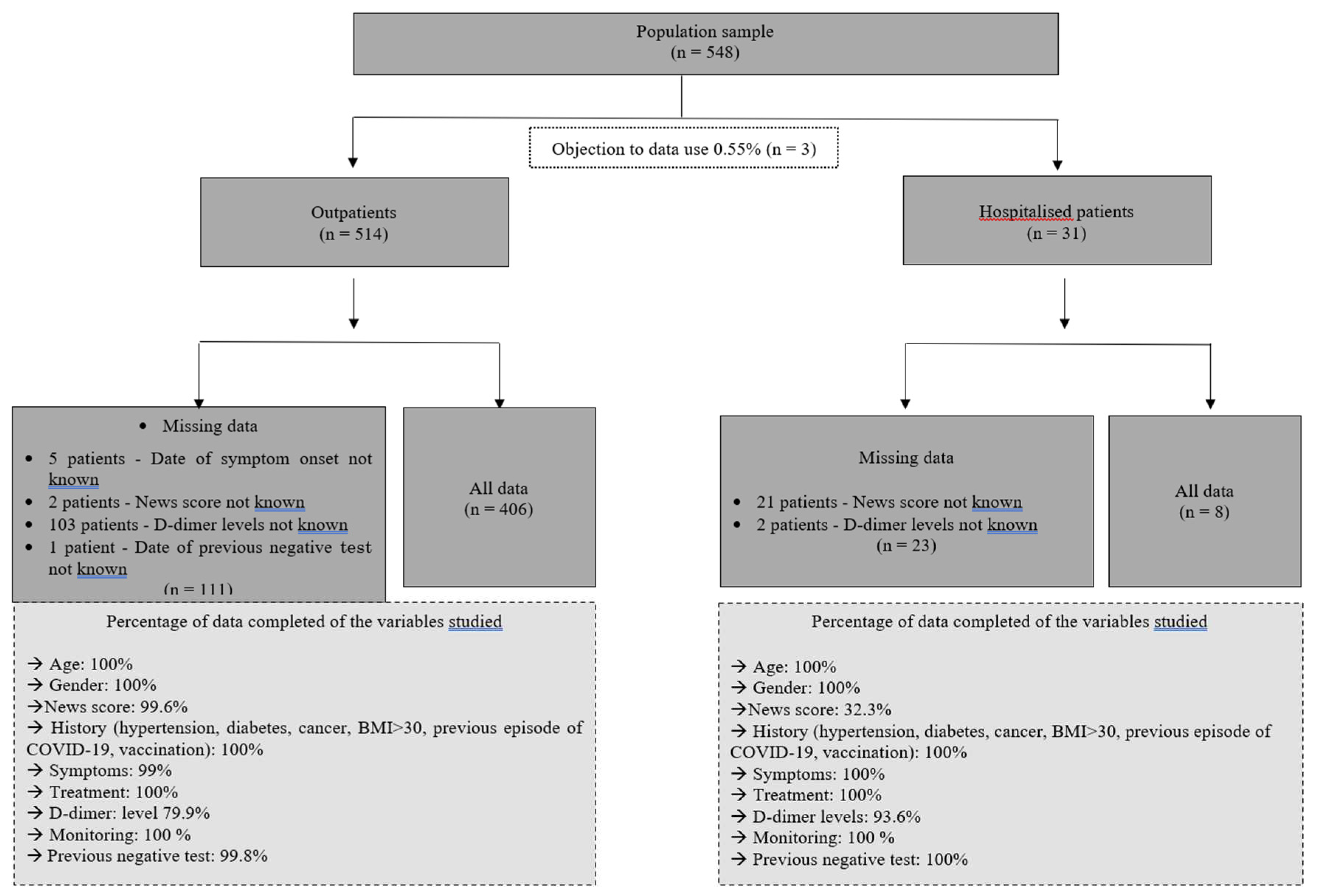
Data quality and sample representativity: A total of 548 data sets collected from 548 consecutively interviewed patients between 1 February and 7 March 2022 were extracted from the database. Three of these 548 patients refused the use of their data (0.55%), resulting in 545 being used for analysis. Among this cohort 514 were seen as outpatients and 31 were seen as hospitalised patients. A detailed analysis of missing data as well as a ratio of data sets available for analysis is presented in the flowchart
Figure 1.
Of the 545 patients, 46 were hospitalised (11.8%), one died within the 30 days following hospitalisation, and one was further admitted to the Intensive Care Unit (ICU). Consequently, among the primary outcome variables, “hospitalisation” only was retained for analysis.
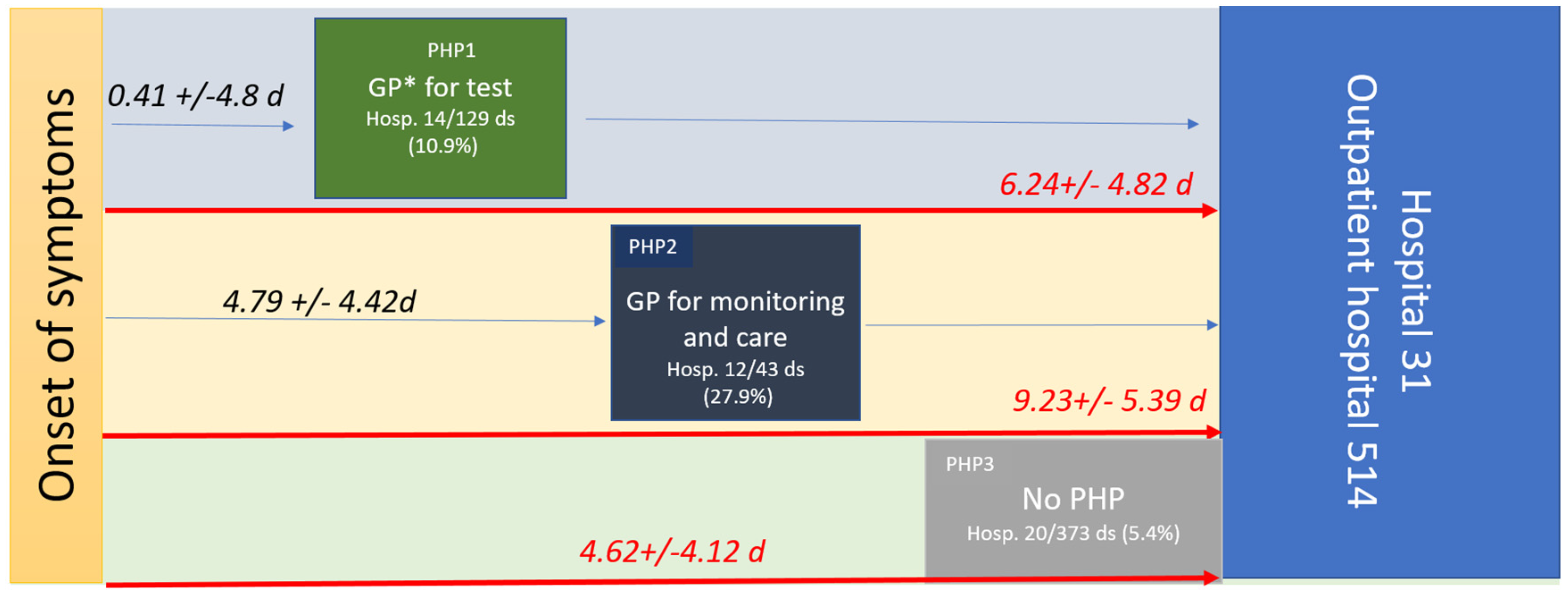
Three mains PHPs were characterised: PHP1 when patients consulted a health professional without having a positive diagnostic test (they were considered to be patients who were either symptomatic or asymptomatic (20.2%) and who came to the doctor to get a diagnostic test prescription); PHP2 when patients consulted a health professional with a positive test (they were considered to be patients who were either symptomatic or asymptomatic (4.7%) and who came to the doctor for treatment); and PHP3, when patients had seen no healthcare professionals in their PHP (
Figure 2).
PHP1 was undertaken by 129 patients and 14 were hospitalised (10.9 %). PHP2 was undertaken by 43 patients and 12 were hospitalised (27.9 %). PHP3 was undertaken by 373 patients and 20 were hospitalised (5.4%). After checking the hospital information system, none of the 499 patients who received treatment at the outpatient department of the hospital, were hospitalised with 30 days of the study period. The hospitalisation rate was significantly higher in PHP2 than in PHP3 or PHP1 , and higher in PHP1 than in PHP3.
The time from OS to any consultation was significantly shorter for patients in PHP1 (0.41 +/- 4.8 days) compared to PHP2 (4.79 +/-4.42 days; p<0.001). Moreover, the time from the OS to hospital admission (PHP duration) was significantly longer in PHP2 (9.23 +/-5.39 days) compared to PHP1 (6.24 +/-4.82 days; p < 0.001) and to PHP3 (4.62+/-4.12; p<0.001), see
Table 1,
Figure 2. Indeed, patients who had seen a health professional (PHP2) arrived later at the hospital. Health monitoring by the GP, including monitoring of oxygen saturation levels (with a prescription for a pulse oximeter) and/or a blood test, was reported in only 21.9 % of symptomatic patients. Although 77.7% to 85.7% of symptomatic patients received at least one medication from their GP, 73.1% were also treated while asymptomatic. Treatment by GPs mainly included azithromycin (39.5%), paracetamol (37.5%), zinc (32.6%), vitamins (20.9%), other antibiotics (19.2%) and corticosteroids in 17.4% of cases, while the treatment provided at the hospital included mainly hydroxychloroquine (62%), azithromycin (80.2%), zinc (82.6%) and anticoagulation (59.6%) (
Table 2).
In univariate analysis (
Table 3), the probability of hospitalisation was significantly higher among men (OR 95% CI; 1.95 [1.05–3.63], p=0.023), older patients (OR 95% CI; 1.06 [1.03–1.08], p<0,001), and those who presented with an elevated News2 score (OR 95% CI; 2,09 [1,73–2,52]), p<0,001). Similarly, the probability of hospitalisation was higher among obese patients (OR 95% CI; 2.17 [1.15–4.10], p=0.015) and those with D-dimers levels >0.5 µg/
mL (OR 95% CI; 6.15 [2.9–12.7], p<0.001). A longer time between OS and hospital admission (PHP duration) was associated with a higher probability of hospitalisation (OR 95% CI; 1.12 [1.7–1.18], p=0,03), as well as a longer time between the onset of symptoms to presentation to healthcare professional (OR 95% CI; 1.07 [1.01–1.13], p=0,02). More than three days between OS and consultation with a GP was also associated with a higher probability of hospitalisation (OR 95% CI; 5.63 [2.93–13.76], p=0.02).
Surprisingly, monitoring (O2Sat/blood pressure/blood analysis, etc.) by the GP during PHP2 was associated with a higher probability of hospitalisation (OR 95%CI; 5.33 [2.51–11.30], p <0.001) as well as the prescription of any COVID treatment by the GP (OR 95% CI; 2.32 [1.23–4.33], p=0.007). Among the different pre-hospital pathways, PHP2 and PHP1 were more frequently associated with a higher probability of hospitalisation than PHP3 (OR 95% CI; 2.15 [1.05–1.39], p=0.036) and (OR 95% CI; 6.83 [3.06–1.3915.27], p<0.001), respectively.
Factors independently associated with outcome (hospitalisation) were being male (OR 95% CI; 2.21 [1.01–4.84], p=0.04), News2 score (OR 95% CI; 2.04 [1.65–2.51], p<0.001), obesity (OR 95% CI; 3.45 [1.48–8.09], p=0.005), D-dimer levels > 0.5 µg/mL (OR 95% CI; 3.45 [1.47–8.12], p=0.005), prolonged time from symptoms to hospital care (PHP duration) (OR 95% CI; 1.07 [1.01–1.14], p=0.03). All things being equal, patients with a PHP2had a higher probability of hospitalisation compared to a PHP3 pre- (OR 95% CI; 4.31 [1.48–12.55], p=0.007).
4. Discussion
Strengths and weaknesses: To our knowledge, this study is the first to identify PHPs in COVID-19 patients. This study is monocentric, and consequently the results presented below are applicable only to our sample. A multicentre study would have made it possible to draw general conclusions as to the observations made on the general population. However, we would have lost precision and would have taken the risk that no effect would be visible in connection with Simpson’s paradox [
17]. Although this is a retrospective study, memory bias is avoided since the data were collected prospectively by doctors using a standardised hospital electronic medical record system at the time of patient treatment which, in addition, led to very little missing data. The results are highly significant, as evidenced by the univariate and multivariate analyses, which were obtained from detailed models and corrected with adjusted odds ratios. We originally aimed to study the impact of PHPs on hospitalisations, admissions to ICU, and deaths. This was impossible since, fortunately, only two patients met the last two criteria. Indeed, this study comes a little late in the unfolding of the pandemic. This study was conducted exclusively on the last wave, when the SARS-CoV2 Omicron variant was dominant. It is likely that access to pre-hospital care has changed during the different epidemic waves since 2020, as has the severity of the disease in relation to the viral genotype [
16]. The impact of vaccination on at-risk patients may also have altered prognosis and, in particular, hospitalisation.
Our study reports that for patients with suspected or confirmed COVID, the shorter the PHP the better the outcome. This has also been reported for other diseases including HIV, sepsis and cancer [
12,
13,
14]. In COVID-19, delaying admission to hospital after the onset of the illness is associated with prolonged SARS-COV-2 shedding [
15], and the time from OS to admission (PHP duration) is significantly associated with death [
16]. Having a test prescribed by a GP (PHP1), as well as having treatment provide by a GP (PHP 2) is a risk factor for hospitalisation. This paradoxical feature may be explained by the prolonged duration of the PHP or the fact that the GPs screen and refer to hospital only the most severe patients. The few deaths and resuscitations in this cohort did not enable us to answer the second question. Of the 499 patients who presented directly at the outpatient department of the hospital and returned home after being investigated and treated, none were subsequently hospitalised in the 30-day follow-up period. This ratio of hospitalisation suggests that standardised treatment might be beneficial to the outcome. Because the late management of patients with asymptomatic hypoxaemia led to a very poor outcome [
2,
17], meticulous screening using home oximetry with virtual monitoring could prevent hospitalisation, resuscitation and/or death [
3,
18]. Some authors suggest using risk prediction scores including a simple interview or clinical examination features to guide hospitalisation, such as for example the SOARS [
17], the News2, and the RECAP [
19] early warning score that can be used by GPs in the pre-hospital management of patients. The measurement of D-dimer levels in the early course of the disease showed that D-dimer levels of up to 1 µg/mL were associated with death and that preventive anticoagulation should improve outcomes [
20,
21,
22]. Pre-hospital management of COVID-19 is likely to have changed during the epidemic, with telemedicine and remote surveillance. In 2020, a prospective cohort study reported that, over 28 days of outpatient monitoring, 10.9% of the patients presented directly to the emergency department and 7.6% required hospitalisation [
4].The role of pre-hospital management would be to avoid hospitalisation, thus limiting hospital overcrowding and its consequences on overall care.
5. Conclusions
Reducing the time between OS and primary care, the early assessment of disease prognosis based on scores, and the monitoring of prognosis-associated variables such as oxygen saturation and D-dimer levels by general practitioners, could help guide hospitalisation, relieving the hospital system while improving patient outcomes (
Figure 3). Such pre-hospital care through specific outpatient care [
4], ad hoc home visits such as “Coronataxi” [
23], a screening and primary care structure [
22], or specialised medical centres for general practitioners should be discussed in preparation for a new pandemic.
Author Contributions
Conceptualization, P.B. and S.G., methodology, L.M., S.G. and P.B.; software, L.M. and F.G.; validation, P.B. and S.G.; formal analysis, L.M. and P.B.; investigation, F.G., writing—original draft preparation, F.G.; writing—review and editing, L.M. and S.G.; supervision, P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by ANR-15-CE36-0004-01 and by ANR “Investissements d’avenir”, Méditerranée infection 10-IAHU-03.
Institutional Review Board Statement
The study was submitted for approval in advance to an Independent Ethical Committee (IEC) which gave a favorable opinion (No. 2022-010). The IEC considered that this study does not fall under French bioethical law and complies with regulations on the processing of medical data and the Helsinki declaration. The investigators’ declaration to comply with reference method MR 004 was filed prior to this study and was the subject of a declaration in the GDPR/APHM Register No.2020-151.
Informed Consent Statement
Patient consent was waived due to the nature of the study. This is a retrospective study using medical data collected prospectively in 2022, by physicians during the medical treatment of patients presenting at the Institut Hospitalo-Universitaire (IHU) Méditerranée Infection for treatment after being diagnosed with COVID-19. Data recorded between 1 February and 7 March 2022 were selected and extracted from the hospital database for this study. However, to complaint to GDPR, patient was informed for the possible use of their data for research purpose and data from people who objected to their use were excluded form the analysis.
Data Availability Statement
The anonymized data base used for this study is available upon request to the corresponding author.
Acknowledgments
Parola P, Lagier JC, Piseth S, Doudier B, Amrane S, and Cassir N, who took part in the organisation of the many interviews
Conflicts of Interest
All authors have no conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- Gautret P, Million M, Jarrot PA, Camoin-Jau L, Colson P, Fenollar F, et al. Natural history of COVID-19 and therapeutic options. Expert Review of Clinical Immunology. 2020 Dec 1;16(12):1159–84.
- Brouqui P, Amrane S, Million M, Cortaredona S, Parola P, Lagier JC, et al. Asymptomatic hypoxia in COVID-19 is associated with poor outcome. Int J Infect Dis 2020 Oct 29.
- Dillon K, Hook C, Coupland Z, Avery P, Taylor H, Lockyer A. Pre-hospital lowest recorded oxygen saturation independently predicts death in patients with COVID-19. Br Paramed J. 2020 Dec 1;5(3):59–65.
- Blair PW, Brown DM, Jang M, Antar AAR, Keruly JC, Bachu VS, et al. The Clinical Course of COVID-19 in the Outpatient Setting: A Prospective Cohort Study. Open Forum Infect Dis. 2021 Feb;8(2): ofab007.
- Bompard F, Monnier H, Saab I, Tordjman M, Abdoul H, Fournier L, et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur Respir J. 2020 Jul;56(1):2001365.
- Lippi G, Favaloro EJ. D-dimer is Associated with Severity of Coronavirus Disease 2019: A Pooled Analysis. Thromb Haemost. 2020 May;120(5):876–8.
- Poor, HD. Pulmonary Thrombosis and Thromboembolism in COVID-19. Chest. 2021 Oct;160(4):1471–80.
- Kyriakoulis KG, Kollias A, Kyriakoulis IG, Kyprianou IA, Papachrysostomou C, Makaronis P, et al. Thromboprophylaxis in Patients with COVID-19: Systematic Review of National and International Clinical Guidance Reports. Curr Vasc Pharmacol. 2022;20(1):96–110.
- Martín-Rodríguez F, López-Izquierdo R, Del Pozo Vegas C, Sánchez-Soberón I, Delgado-Benito JF, Martín-Conty JL, et al. Can the prehospital National Early Warning Score 2 identify patients at risk of in-hospital early mortality? A prospective, multicenter cohort study. Heart Lung. 2020 Oct;49(5):585–91.
- Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020 May 22;369:m1966.
- Million M, Lagier JC, Tissot-Dupont H, Ravaux I, Dhiver C, Tomei C, et al. Early combination therapy with hydroxychloroquine and azithromycin reduces mortality in 10,429 COVID-19 outpatients. Rev Cardiovasc Med. 2021 Sep 24;22(3):1063–72.
- INSIGHT START Study Group, Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N Engl J Med. 2015 Aug 27;373(9):795–807.
- Peltan ID, Brown SM, Bledsoe JR, Sorensen J, Samore MH, Allen TL, et al. ED Door-to-Antibiotic Time and Long-term Mortality in Sepsis. Chest. 2019 May;155(5):938–46.
- Cone EB, Marchese M, Paciotti M, Nguyen DD, Nabi J, Cole AP, et al. Assessment of Time-to-Treatment Initiation and Survival in a Cohort of Patients With Common Cancers. JAMA Netw Open. 2020 Dec 1;3(12):e2030072.
- Xu K, Chen Y, Yuan J, Yi P, Ding C, Wu W, et al. Factors Associated With Prolonged Viral RNA Shedding in Patients with Coronavirus Disease 2019 (COVID-19). Clin Infect Dis. 2020 Jul 28;71(15):799–806.
- Deng Y, Liu W, Liu K, Fang YY, Shang J, Zhou L, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: a retrospective study. Chin Med J (Engl). 2020 Jun 5;133(11):1261–7.
- Chua F, Vancheeswaran R, Draper A, Vaghela T, Knight M, Mogal R, et al. Early prognostication of COVID-19 to guide hospitalisation versus outpatient monitoring using a point-of-test risk prediction score. Thorax. 2021 Jul;76(7):696–703.
- Greenhalgh T, Knight M, Inda-Kim M, Fulop NJ, Leach J, Vindrola-Padros C. Remote management of covid-19 using home pulse oximetry and virtual ward support. BMJ. 2021 Mar 25;372:n677.
- Greenhalgh T, Thompson P, Weiringa S, Neves AL, Husain L, Dunlop M, et al. What items should be included in an early warning score for remote assessment of suspected COVID-19? qualitative and Delphi study. BMJ Open. 2020 Nov 12;10(11):e042626.
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054–62.
- Shi L, Wang Y, Wang YD, Duan GC, Yang HY. D-dimer is associated with the risk of mortality in Coronavirus Disease 2019 patients. Eur Rev Med Pharmacol Sci. 2020 Aug;24(16):8576–9.
- Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020 Jun 16;75(23):2950–73.
- Hippchen T, Kräusslich HG, Merle U. Coronataxi Brings Outpatient Care to COVID-19 Patients. Ann Emerg Med. 2020 Dec;76(6):811–2.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).