1. Introduction
Over recent years, the weight of pre-pregnant women in childbearing ages, including overweight, obesity, and underweight, is gradually showed an increased trend in developed countries [
1]. The Risk Assessment Monitoring System of pregnant women, followed in different hospitals with maternity services, revealed that abnormal Body Mass Index (BMI) before conception has increased in different parts of the world, especially in medium- and low-income countries, including Greece. A recent cross-sectional study published in 2022 aimed to provide data on the prevalence of BMI in terms of overweight and obesity and its determinants in 12 countries in Europe and revealed that adult obesity was the highest in Greece [
2]. Obesity in Greece is considered as a severe public health problem; in 2015, the prevalence of childhood overweight in ages 4-17 years old was 22.2% and 21.6%, in boys and girls, respectively, while obesity was reported as 9.0% and 7.5% in boys and girls, respectively [
3]. Alarmingly enough, these prevalence results were among the highest rates worldwide showing a major increase (by 52%) in the prevalence of childhood obesity and overweight during the last few decades [
4].
Based on the World Health Organization (WHO), the nutritional status of mothers might be a good predictor on the long-term adverse outcomes of the mothers and their infants [
5]. Notably, pre-pregnancy overweight and obesity, are considered high-risk factors for Gestational Diabetes Mellitus (GDM), hypertension, as well as abnormalities of fetal growth [
6,
7,
8].
Recent research has shown that obesity has severe consequences on health because it may increase the risk of several diseases, such as diabetes mellitus type 2, hypertension, insulin resistance, dyslipidemia, coronary heart disease, stroke, respiratory disorders, mental health and cancer [
9]. However, obesity, beyond its direct impacts on mothers’ health status, seems to indirectly affect the child’s health at the next stages of their life. Primarily, maternal pre-pregnant obesity probably affects negatively the fetus, and the fetal growth in all stages. Several researchers investigated the effect of maternal obesity on infants’ birth weight [
10,
11,
12,
13]. More to the point, it has been reported that obese pregnant women were more likely to give birth of large birth weight babies (macrosomic neonate). This was mainly explained by the elevation in maternal glucose levels causing neonatal hyperglycemia and hyperinsulinemia that accelerates fetal growth [
14]. Moreover, pre-pregnancy underweight is well documented to increase the risk of premature babies and small gestational aged newborns [
15].
A systematic review and meta-analysis showed a strong relationship between maternal obesity and cesarean delivery and complicated births requiring instrumental delivery [
16]. In addition, extensive evidence in the literature supports a positive link-age between the incidence of cesarean sections and obesity [
17].
There is also substantial evidence that obesity in mothers is associated with some respiratory complications such as asthma in childhood. This implication could be possibly attributed to the fact that maternal obesity might influence fetal lung development and the fetal immune system in the early stages of pregnancy [
18]. For example, in a recent study in UK, the researchers examined the association between high maternal BMI during pregnancy and respiratory tract infections in children. This study revealed a significant relationship between wheezing and maternal obesity [
19]. Similar findings were recently reported in Boston, USA, which showed that maternal pre-pregnancy obesity was considered as an independent risk factor for developing childhood respiratory tract infection [
20].
In parallel to the association of different health problems among children born by mothers of abnormal high BMI, another study in Sweden investigated the effects of maternal BMI and gestational weight gain on the risk of developing type 1 diabetes in the offspring. This study identified maternal obesity as a risk factor for type 1 diabetes in the offspring [
21]. Moreover, these results highlight the importance of public health and antenatal care to promote normal maternal BMI to reduce the incidence of type 1 diabetes among children. Moreover, it is reasonable that if the parents are overweight or obese due to an unhealthy diet, there is a high probability to have overweight or obese children because their children most likely will follow similar unhealthy nutritional patterns within their family members. Accordingly, there is strong evidence that a high prevalence of women in reproductive age do not follow healthy dietary habits like Mediterranean diet in conjunction with a poor lifestyle behavior (e.g., low physical activity, smoking, etc.), which increase the risk of developing overweight and obesity [
22,
23,
24,
25].
To our knowledge, the studies that investigated the multifactorial effect of pre-pregnancy maternal overweight/obesity on childhood health complications at pre-school aged in Greece remain still limited [
22]. Therefore, in the present cross-sectional study, we aimed to examine the potential associations between maternal pre-pregnancy excess body weight and childhood demographic and anthropometric characteristics, as well as perinatal and postnatal outcomes. The results of the current study will provide novel evidence and information concerning pregnancy-related complication in perinatal and postnatal period in Greek mothers and their children, which could give prominence to develop and apply new strategies, policies and interventions to minimize this public health issue.
2. Methods
2.1. Subjects
In the present cross-sectional study, 7047 pre-school children aged 2-5 years old, and their matched mothers, were initially enrolled from nine different Greek regions, from kindergarten schools, playgrounds and elsewhere. Subject data collection was obtained between May 2016 and September 2020. Criteria for the initial enrollment, included, children aged 2-5 years old, whose mothers had a singleton birth before enrollment, independently of parity, 2-5 years and who had non another pregnancy at the interval between the time of this singleton birth delivery and the time of study, i.e., 2-5 years postpartum. Both children and their mothers were disease-free during the postpartum period.
All participant information was confidential. Only children with a possible development of asthma or type 1 diabetes mellitus were included in the study. Seven thousand forty-seven (7047) children and their matched mothers were initially enrolled in the study. Nine hundred eighty-eight (988) of them (14.0%) were missing or had incomplete data and thus excluded from the study. Sample size calculation was based on the use of PS: Power and Sample Size calculator program, while a simple randomization method was carried with the use of a sequence of random binary numbers (e.g., 100,101,011 in which 0 represented enrolment and 1 not enrolment to the study). PS software can calculate the sample size required to detect a specified alternative hypothesis with the needed power, the power with which a specific alternative hypothesis can be detected with a given sample size, or the specific alternative hypotheses that can be detected with a given power and sample size.
Among the remaining 6059 subjects, 861 (14.2%) children were then excluded from the study due to a history of other disease/pathological conditions such as hyperinsulinemia, anemia, hyperlipidemia, type 2 Diabetes, cancer, autism spectrum disorder, motor disorder, mental retardation. The above exclusion was applied to assure whether pre-pregnancy maternal overweight/obesity affected the prevalence of childhood overweight/obesity, independently of other childhood diseases, which may increase the risk of childhood overweight/obesity, like metabolic disorders or hypertension, for which a considerably higher sample size would be required. In addition, the mothers of the enrolled children had not any disease during their pregnancy except for any history of gestational diabetes or pregnancy induced hypertension which had been treated effectively during their gestation.
Neonatal ponderal index was also measured as per protocol [
23]. Mothers reported if they had a pre-term birth (< 37th week) and the data were cross-checked by their medical files. Nevertheless, we detected that there were several lost data regarding the precise week of pre-term birth in the medical records and several of them did not come to an agreement with the mothers’ responses, and thus pre-term birth was treated as a binary variable as before and after of 37th week of pregnancy.
After the above inclusion and exclusion criteria a total of 5198 children and their matched mothers were included in the final analysis, resulting in a final response rate equal to 73.8%. All participant mothers informed in detail about the study and signed a con-sent. The study was in compliance with the World Health Organization (52nd WMA General Assembly, Edinburgh, Scotland, 2000) and approved by the Ethics Committee of the University of the Aegean (ethics approval code: no 12/14.5.2016).
2.2. Study Design
Validated semi-quantitative questionnaires were used to collect the anthropometric and demographic characteristics as well as the perinatal and postnatal outcomes of the study population [
23,
24,
25], 2.5 years after delivery. Data on children anthropometry such as birth weight, height and head circumference were collected by their mother’s gynecologists’ or hospitals’ medical files. Children birth weight of (< 2500gr) was classified as low, (2500 – 4000 gr) as normal and (> 4000gr) as high. A trained dietitian collected all children anthropometric parameters (weight and height) at the age of 2-5 years old as per protocol [
24,
27]. Mother’s and children’s weight was measured using a Seca scale [Seca, Hanover, MD], without shoes, to the nearest 100 grams
, while height was measured using a portable stadiometer (GIMA Stadiometer 27335) with no shoes on, to the nearest 0.1cm. Two international datasets were used to define overweight and obesity in pre-school children and their mothers: the WHO and the International Obesity Task Force (IOTF) data references [
28,
29]. Τhe mode of delivery (vaginal or caesarean section), childhood type 1 diabetes mellitus and asthma data were also recorded also from the given questionnaire. The childhood asthma data was reporting by a specialized pediatrician physician based on the International Study of Asthma and Allergies in Children guidelines report [
30].
Mothers weight and height at the first weeks of pregnancy were measured during a visit to their personal gynecologists or the health care units that followed them. Both mothers’ pre-pregnancy weight and height measured data were retrieved by their medical records. Mothers’ pre-pregnancy BMI was calculated according to the weight and height measured at the first weeks of pregnancy from their personal gynecologists or the health care units that followed them. Clarifying instructions were given to the participating mothers by registered dietitians and nutritionists regarding the completion of questionnaires by a face-to-face interview, while a detailed presentation of the questions to facilitate accurate answers was performed.
2.3. Statistical Analysis
Student’s t-test was used for continuous variables that followed normal distribution. Normality distribution was evaluated by Kolmogorov-Smirnov test. Categorical variables were evaluated by Chi-square. The quantitative variables following normal distribution were presented as mean value ± Standard Deviation (SD). The quantitative non-normally distributed continuous variables are given as median value (Interquartile Range, IQR). The qualitative variables are stated as absolute or relative frequencies. To determine if maternal pre-pregnancy BMI status, as the main independent variable, is independently associated with multiple dependent variables including childhood demographic and anthropometric characteristics and childhood perinatal and postnatal outcomes, multivariate logistic regression analysis was conducted after adjustment for potential confounding such as maternal age, children gender, birth weight, height and head circumference, preterm birth, newborn ponderal index, type of delivery and childhood diabetes I, which showed previously significant effect in pre-pregnancy maternal BMI in univariate analysis. The Statistica 10.0 software, Europe was used to perform the statistical analysis of the survey data (Informer Technologies, Inc., Ham-burg, Germany).
3. Results
3.1. Demographic and anthropometric characteristics and perinatal and postnatal outcomes of the study population
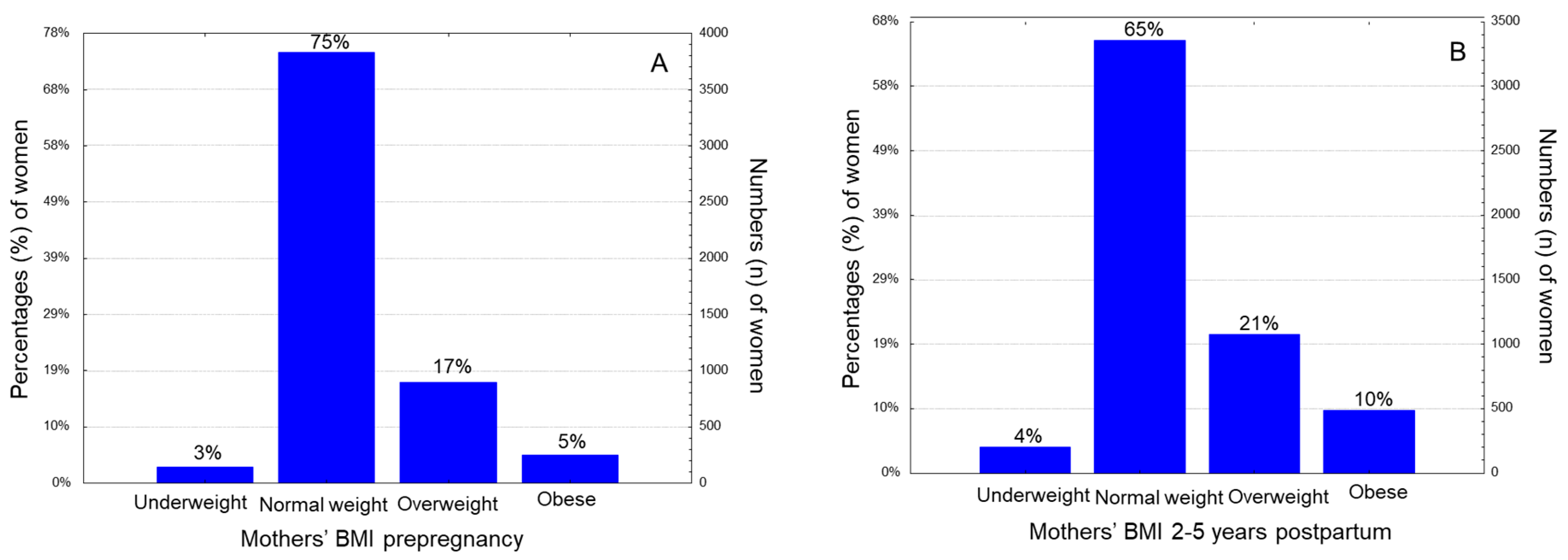
The present cross-sectional study finally included 5198 children, aged 2-5 years old, and their matched mothers who were enrolled 2-5 years after delivery. Seventeen-point four percent (17.4%) of the women were overweight, and 4.9% were obese before pregnancy, based on their BMI classification (
Figure 1A). At the time of study, 2-5 years postpartum, twenty one percent (21.0%) of them were overweight and 9.6% were obese, respectively (
Figure 1B). Overall, 22.3% of participating women were overweight/obese pre-pregnancy and this prevalence was significantly increased to 30.1, 2-5 years postpartum (p
0.0001). Regarding the type of delivery, 43.7% were delivered vaginally and 56.3% by caesarean section. Preterm birth was noted in 30.0% of the women under study. Newborn ponderal index was classified as high in 47.8% of the women under study.
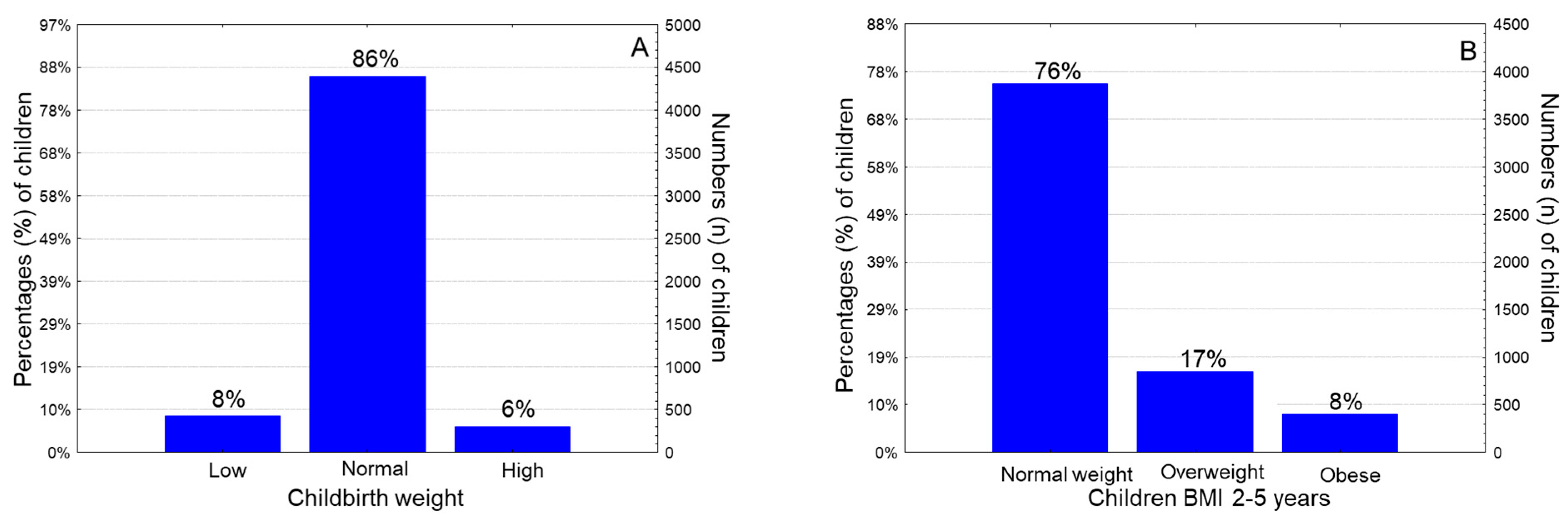
The mean childbirth weight was 3152±461gr (range: 1320-5000 gr), the mean birth height was 46.4±2.7 cm (range: 42-52 cm) and the mean birth head circumference was 36.0±2.0 cm (range: 32-39 cm). Classifying children according to their birth weight, 8.3% of them were categorized as low newborn weight (< 2500 gr), 85.7% of them had normal newborn weight (2500-4000 gr) and 6.0% of them had high new-born weight (>4000gr) (
Figure 2A). Regarding children BMI at the age of 2-5 years old, 16.5% of them were classified as overweight and 7.9% of them were classified as obese and in total 24.3% % of the children were overweight/obese (
Figure 2B).
The mean age of the children was 4
.1 ± 1.2 years (range: 2.0–5.5 years). Concerning children gender, 49.3% of the study children were male, and the rest (50.7%) were female. The mean birth weight was 3152±461gr (range: 1320-5000 gr), the mean birth height was 46.4±2.7 cm (range: 42-52 cm) and the mean birth head circumference was 36.0±2.0 cm (range: 32-39 cm). Classifying children according to their birth weight, 8.3% of them were categorized as low newborn weight (< 2500 gr), 85.7% of them had normal newborn weight (2500-4000 gr) and 6.0% of them had high newborn weight (>4000gr) (
Figure 2A).
Postnatal outcomes revealed that, 4.3 % and 4.5% of the children developed type 1 and asthma, respectively. Regarding children BMI at the age of 2-5 years old, 16.5% of them were classified as overweight and 7.9% of them were classified as obese and in total 24.4% % of the children were overweight/obese at the age of 2-5 years old (
Figure 2B).
3.2. Maternal pre-pregnancy excess weight in association with antrhopometric and demographic characteristics of the participant children
Childhood obesity at the age of 2-5 years old was significantly more frequently observed when maternal pre-pregnancy BMI status was overweight or obese (
Table 1, p<0.0001). Childbirth weight was significantly higher in those children whose mothers were overweight or obese pre-pregnancy compared to newborns whose mothers were underweighted or normal weight, pre-pregnancy (
Table 1, 3269±483 gr vs. 3107±412 gr, p=0.0172). Newborns with high weight status were significantly more frequently observed in children whose mothers were obese during pre-pregnancy period (
Table 1, p=0.0001). Pre-pregnancy maternal BMI status was not associated with childbirth height or head circumference (
Table 1, p>0.05). Pre-pregnancy overweight or obese women were significantly older compared to underweight and normal weight women (
Table 1, p=0.0001). Preterm birth was noted in 30.0% of the women under study.
3.3. Maternal pre-pregnancy excess weight in association with childhood perinatal and postnatal outcomes
Children, whose mothers had an abnormal pre-pregnancy BMI meaning were overweight or obese, were significantly more frequently delivered by caesarean section compared to those whose mothers were underweight or normal weight pre-pregnancy (
Table 1, p=<0.0001). Moreover, children whose mothers were overweight or obese pre-pregnancy showed a significantly higher prevalence for developing diabetes type I (
Table 1, p=0.0009). Non association between maternal pre-pregnancy BMI status and childhood asthma at the age of 2-5 years old was recorded (
Table 1, p>0.05).
3.4. Pre-pregnancy BMI status-Multivariate regression analysis
Multivariate logistic regression analysis revealed that maternal pre-pregnancy excess weight (overweight and obesity) was significantly independently associated with childhood BMI at the age of 2-5 years old, childbirth weight status, type of delivery and childhood diabetes type I (
Table 2, p=0.0001, p=0.0009, p=0.0175 and p=0.0014, respectively). Overweight and obese women before pregnancy had more than two-fold higher odds for delivering children who were overweight or obese at the age of 2-5 years old (
Table 2, p=0.0001). Moreover, overweight, and obese women before pregnancy showed a 95% higher probability to deliver children with high newborn weight (
Table 2, p=0.0009).
Overweight and obese women before pregnancy also had a 71% higher likelihood to deliver their children by caesarean section (
Table 2, p=0.0175). Furthermore, overweight, and obese women before pregnancy showed a 28% higher risk for delivering children developing diabetes type 1 at the next 2-5 years of their life (
Table 2, p=0.0014).
Maternal age, childhood gender, preterm birth and newborn ponderal index did not remain significant in multivariate analysis (
Table 2, p>0.05).
4. Discussion
The present study reported that pre-pregnancy maternal overweight and obesity was associated with high rates of overweight and obesity in their offspring at the age of 2-5 years old. Our data also showed that children whose mothers were overweight or obese pre-pregnancy had higher incidence to be born with high birth weight. In addition, higher prevalence of delivery by caesarean section was recorded when the mother was classified as overweight or obese at pre-pregnancy. Moreover, children whose mothers were overweight or obese pre-pregnancy had higher incidence for developing diabetes type 1 in their life later on. All the above associations remain significant in multivariate analysis after adjusting for multiple confounding factors. These results highlight the importance of early prevention of obesity among Greek women of childbearing age to prevent adverse health outcomes linked to their children at short- and long-term levels such as excess birth weight status, childhood obesity, and diabetes type 1.
Alarmingly enough, our data supported evidence that childhood overweight/obesity at the age of 2-5 years old was more probable when their mothers had overweight or obese BMI status pre-pregnancy. This observation is in line with previous research in the field [
31] among children of a similar age with our study. Previous substantial studies further supported that maternal obesity at pre-pregnancy, during pregnancy and postpartum may be related to higher obesity levels among their children [
32]. In this aspect, literature data were shown that maternal pre-pregnancy obesity may also be related with increased total and visceral fat among children at the age of 9-13 years old [
33]. In line with the above findings, our analysis showed that high newborn weight (>4,000 gr) was more frequently observed in children whose mothers were overweight/obese pre-pregnancy. In support of the previous findings, the bio-physiological pathway of insulin resistance among overweight and obese mothers, leading among others, to elevated glucose levels during pregnancy that has been linked with accelerated fetal growth and large birth weight for newborns [
34]. Further data have also supported the pathway of in uterus child obesity “programing”, where mother’s obesity and abnormal metabolic status may play an important role [
35]. These results in combination with the high rates of obesity in Greece among children, and women at childbearing age, may raise a red flag for the need of early obesity prevention public programs and policies at early pre-pregnancy stages in order to battle the intergenerational cycle of excess weight and abnormal metabolic outcomes.
Furthermore, the positive association of the excess weight (overweight and obesity) at pre-pregnancy timing with childhood anthropometric and demographic characteristics as well as perinatal and postnatal outcomes was evaluated, taking into account several potential confounders. When the multivariable modelling was applied, maternal pre-pregnancy overweight and obesity was related with a high risk of childhood overweight/obesity at the age of 2-5 years old, high birth weight status, caesarean type of delivery and childhood diabetes type 1. More specifically, the analysis showed that overweight and obese women before pregnancy had more than a two-fold higher risk for delivering children who were overweight or obese at the age of 2-5 years old. Our analysis is in line with previous studies supporting the finding of pre-pregnancy association with child obesity [
32,
36]. Among our findings, pre-pregnancy obesity was related with cesarian delivery type. Previous meta-analysis and observational studies also support our finding concerning the association between maternal obesity before pregnancy and caesarean type of delivery [
37,
38]. However, caesarian section usually is strongly necessitated for medical reasons, especially when there is a high probability for severe complications compared to vaginal delivery, such as extremely maternal obesity, preeclampsia, gestational diabetes or hypertension, or chronic diseases such thyroid gland disorders, cardiovascular disease, cancer, multiple sclerosis or other autoimmune diseases [
36,
37,
38]. Also, our data analysis showed that overweight and obese women before pregnancy had a 28% higher risk of delivering children developing diabetes type 1 at the next stages of their life. This finding is in line with several studies; however, inconsistent findings have been reported so far [
39], which strongly emphasizes the necessity for additional research in the underlined mechanisms. Identification of pre-, peri-, and post- natal factors and their influence on maternal and offspring health is very important, as there is a lack of research in this issue, especially in Greece. Such data could contribute to shape future inter-generational prevention and monitoring programs for maternal-child health in Greek population as well as in the whole Mediterranean region.
Recent studies mark the beneficial role of nutrition and physical activity interventions in obesity and metabolic abnormalities among mothers and their offspring [
40,
41]. The health and medical community in Greece could consider excess weight among the priority mutual risk factors for the country’s women of childbearing age and their newborn children. Targeted physical activity and dietary recommendations within the range of Mediterranean diet (that is the healthy dietary pattern of the region) for women at pre-pregnancy period, as well as during and post pregnancy stage could serve as cost-effective planning for maternal and their offspring’s disease prevention [
23,
24,
27].
There is currently strong evidence concerning the need to develop future effective programs to tackle early obesity. This is necessary not only by controlling lifestyle behaviors like infant feeding but also understanding the role of other mechanisms like the effect of perinatal factors such as maternal diet during pregnancy, epigenetics, or microbiome [
42]. Interesting, a recent meta-analysis including all studies up until 15 March 2023 showed that Mediterranean diet-based interventions may have a significant effect on reducing the BMI as well as reducing obesity in children and adolescents aged between 3 and 18 years old [
43].
Up to date, nutrition management has been applied to numerous childhood obesity intervention studies. Diverse forms of nutrition education and counseling, key messages, a Mediterranean-style hypocaloric diet, and nutritional food selection have been implemented as dietary interventions [
44]. However, the currently available data in Greek children remain extremely scarce. In this aspect, it is in our future plans to perform similar studies in in children and adolescent of our country, Greece. The Mediterranean diet includes daily consumption of whole cereals, fruit, vegetables and legumes in moderate proportions, weekly consumption of white meat in low to moderate proportions and occasionally sweets and chocolates in small amounts. Since olive oil is the main lipids source, it has special significance for health. Healthy fruit and vegetables, rich in phytochemicals, are a major proportion of this diet and contribute to the overall nutritional value and bioactivity of its components [
45,
46].
It is reasonable that our study has certain limitations, such as the recall bias of the mothers when reporting the data especially for self-reported questions. Hence, no conclusive evidence concerning causality can be derived because of the cross-sectional design of the present study despite its representative and widely large study population. Another limitation lies with BMI measurement as it is considered as an enough weak tool to calculate body fat because it cannot directly assess it and especially its body distribution. Thus, direct measures of body fat mass using bioelectrical impedance analysis or skinfold measurements will be beneficial in future studies to confirm our findings. The lack of physical activity data and mental status information could also affect our results. Nevertheless, our study is one of the few reported in Greece, that has attempted to evaluate the pre-pregnancy overweight and obesity and its effect on childhood demographic and anthropometric characteristics as well as on perinatal and postnatal outcomes in a widely large representative sample of Greek population concerning pre-school children. Moreover, in our study we focused on whether maternal obesity may affect the prevalence of childhood obesity, independently of other childhood diseases, which may increase the risk for childhood obesity, like metabolic disorders, and for which a considerably larger sample size would be required. In this context, it should be noted that future studies should be conducted on a more appropriate sample size to address the impacts of such diseases in childhood obesity.
5. Conclusions
Maternal pre-pregnancy overweight and obesity rates were related with increased children BMI at the age of 2-5 years old, increased birth weight status, caesarean type of delivery and childhood diabetes type 1. These results highlight the importance of obesity primary prevention efforts among the mothers at pre-pregnancy stages, by reducing a variety of adverse perinatal maternal risk factors, as well as by minimizing their offspring’s adverse health-related outcomes. Considering that obesity, among young women and children, is recognized as a major global wellbeing challenge, particularly in Greece and Mediterranean countries, the aforementioned findings emphasize the crucial requirement for a change towards a healthier lifestyle, including healthier nutritional habits. Additionally, public health policies and interventions should be targeted in obesity population among women of reproducible age to optimize a metabolic healthy inter-generational lifecycle. Moreover, it should be noted that childhood obesity is associated with increased risk of developing several diseases, such as diabetes mellitus, cardiovascular disease, endocrine disorders, autoimmune disorders, cancer, e.t.c., at the next stages of children life. Thus, public health strategies should be informed their mothers in order to reduced childhood obesity pandemic. Public policies are strongly recommended to inform aged reproducible women for the negative effects of childhood obesity concerning the next stages of their life.
Author Contributions
Conceptualization, D.P., S.K.P., D.N.K., and C.G.; methodology, E.P. (Eleni Pavlidou), Z.T., M.M. (Maria Mantzorou), and C.G.; formal analysis, S.T., E.P. (Evmorfia Psara), M.Y., M.S., and G.A..; investigation, E.P. (Eleni Pavlidou), D.P., Z.T., M.M. (Maria Mentzelou) and C.G.; resources, S.T., D.N.K., M.Y., ans M.S.; data curation, E.P. (Eleni Pavlidou), M.M. (Maria Mantzorou), E.P. (Evmorfia Psara), S.K.P., M.S., G.A., and M.M. (Maria Mentzelou); writing—original draft preparation, E.P. (Eleni Pavlidou), D.P., D.N.K., and C.G.; writing—review and editing, E.P. (Eleni Pavlidou), and C.G.; visualization, E.P. (Eleni Pavlidou), D.P., S.K.P., and C.G.; supervision, C.G.; project administration, C.G.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Ethics Committee of the University of the Aegean (ethics approval code: no 12/14.5.2016) and was in compliance with theWorld Health Organization (52nd WMA General Assembly, Edinburgh, Scotland, 2000.
Informed Consent Statement
Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Available upon request to the corresponding author.
Acknowledgments
The authors would like to thank Dr. Teresa Arora for her valuable comments and grammar corrections of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kim, S.Y.; Dietz, P.M.; England, L.; Morrow, B.; Callaghan, W.M. Trends in Pre-Pregnancy Obesity in Nine States, 1993-2003. Obesity (Silver Spring) 2007, 15, 986–993. [Google Scholar] [CrossRef]
- Stival, C.; Lugo, A.; Odone, A.; van den Brandt, P.A.; Fernandez, E.; Tigova, O.; Soriano, J.B.; López, M.J.; Scaglioni, S.; Gallus, S.; et al. Prevalence and Correlates of Overweight and Obesity in 12 European Countries in 2017-2018. Obes Facts 2022. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Current Data in Greek Children Indicate Decreasing Trends of Obesity in the Transition from Childhood to Adolescence; Results from the National Action for Children’s Health (EYZHN) Program. J Prev Med Hyg 2018, 59, E36–E47. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.B.; Kavouras, S.A.; Kallistratos, A.A.; Moraiti, I.P.; Douvis, S.J.; Toutouzas, P.K.; Sidossis, L.S. Eleven-Year Prevalence Trends of Obesity in Greek Children: First Evidence That Prevalence of Obesity Is Leveling Off. Obesity (Silver Spring) 2010, 18, 161–166. [Google Scholar] [CrossRef] [PubMed]
- State of Inequality: Reproductive, Maternal, Newborn and Child Health. Available online: https://www.who.int/data/inequality-monitor/publications/report_2015_rmnch (accessed on 2 September 2022).
- Wei, Y.-M.; Yang, H.-X.; Zhu, W.-W.; Liu, X.-Y.; Meng, W.-Y.; Wang, Y.-Q.; Shang, L.-X.; Cai, Z.-Y.; Ji, L.-P.; Wang, Y.-F.; et al. Risk of Adverse Pregnancy Outcomes Stratified for Pre-Pregnancy Body Mass Index. J Matern Fetal Neonatal Med 2016, 29, 2205–2209. [Google Scholar] [CrossRef] [PubMed]
- Faucett, A.M.; Metz, T.D.; DeWitt, P.E.; Gibbs, R.S. Effect of Obesity on Neonatal Outcomes in Pregnancies with Preterm Premature Rupture of Membranes. Am J Obstet Gynecol 2016, 214, 287.e1–287.e5. [Google Scholar] [CrossRef] [PubMed]
- Langley-Evans, S.C.; Pearce, J.; Ellis, S. Overweight, Obesity and Excessive Weight Gain in Pregnancy as Risk Factors for Adverse Pregnancy Outcomes: A Narrative Review. J Hum Nutr Diet 2022, 35, 250–264. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Ford, E.S.; Bowman, B.A.; Dietz, W.H.; Vinicor, F.; Bales, V.S.; Marks, J.S. Prevalence of Obesity, Diabetes, and Obesity-Related Health Risk Factors, 2001. JAMA 2003, 289, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Baeten, J.M.; Bukusi, E.A.; Lambe, M. Pregnancy Complications and Outcomes among Overweight and Obese Nulliparous Women. Am J Public Health 2001, 91, 436–440. [Google Scholar] [CrossRef]
- Abenhaim, H.A.; Kinch, R.A.; Morin, L.; Benjamin, A.; Usher, R. Effect of Prepregnancy Body Mass Index Categories on Obstetrical and Neonatal Outcomes. Arch Gynecol Obstet 2007, 275, 39–43. [Google Scholar] [CrossRef]
- Kalk, P.; Guthmann, F.; Krause, K.; Relle, K.; Godes, M.; Gossing, G.; Halle, H.; Wauer, R.; Hocher, B. Impact of Maternal Body Mass Index on Neonatal Outcome. Eur J Med Res 2009, 14, 216–222. [Google Scholar] [CrossRef]
- Briese, V.; Voigt, M.; Wisser, J.; Borchardt, U.; Straube, S. Risks of Pregnancy and Birth in Obese Primiparous Women: An Analysis of German Perinatal Statistics. Arch Gynecol Obstet 2011, 283, 249–253. [Google Scholar] [CrossRef]
- Pedersen, J.; Bojsen-Møller, B.; Poulsen, H. Blood Sugar in Newborn Infants of Diabetic Mothers. Acta Endocrinol (Copenh) 1954, 15, 33–52. [Google Scholar] [CrossRef] [PubMed]
- Ronnenberg, A.G.; Wang, X.; Xing, H.; Chen, C.; Chen, D.; Guang, W.; Guang, A.; Wang, L.; Ryan, L.; Xu, X. Low Preconception Body Mass Index Is Associated with Birth Outcome in a Prospective Cohort of Chinese Women. J Nutr 2003, 133, 3449–3455. [Google Scholar] [CrossRef] [PubMed]
- Heslehurst, N.; Simpson, H.; Ells, L.J.; Rankin, J.; Wilkinson, J.; Lang, R.; Brown, T.J.; Summerbell, C.D. The Impact of Maternal BMI Status on Pregnancy Outcomes with Immediate Short-Term Obstetric Resource Implications: A Meta-Analysis. Obes Rev 2008, 9, 635–683. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Lim, J.-Y.; Lim, N.-K.; Ryu, H.M.; Kwak, D.W.; Chung, J.H.; Park, H.J.; Park, H.-Y. Impact of Pre-Pregnancy Body Mass Index and Gestational Weight Gain on the Risk of Maternal and Infant Pregnancy Complications in Korean Women. Int J Obes (Lond) 2022, 46, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Papachatzi, E.; Dimitriou, G.; Dimitropoulos, K.; Vantarakis, A. Pre-Pregnancy Obesity: Maternal, Neonatal and Childhood Outcomes. J Neonatal Perinatal Med 2013, 6, 203–216. [Google Scholar] [CrossRef] [PubMed]
- Håberg, S.E.; Stigum, H.; London, S.J.; Nystad, W.; Nafstad, P. Maternal Obesity in Pregnancy and Respiratory Health in Early Childhood. Paediatr Perinat Epidemiol 2009, 23, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, M.J.; Nino, G.; Hong, X.; Wang, X. Maternal Pre-Pregnancy Weight and Early Life Lower Respiratory Tract Infections in a Low-Income Urban Minority Birth Cohort. Sci Rep 2021, 11, 9790. [Google Scholar] [CrossRef] [PubMed]
- Lindell, N.; Carlsson, A.; Josefsson, A.; Samuelsson, U. Maternal Obesity as a Risk Factor for Early Childhood Type 1 Diabetes: A Nationwide, Prospective, Population-Based Case-Control Study. Diabetologia 2018, 61, 130–137. [Google Scholar] [CrossRef]
- Moschonis, G.; Kaliora, A.C.; Karatzi, K.; Michaletos, A.; Lambrinou, C.-P.; Karachaliou, A.K.; Chrousos, G.P.; Lionis, C.; Manios, Y. Perinatal, Sociodemographic and Lifestyle Correlates of Increased Total and Visceral Fat Mass Levels in Schoolchildren in Greece: The Healthy Growth Study. Public Health Nutr 2017, 20, 660–670. [Google Scholar] [CrossRef]
- Papandreou, D.; Mantzorou, M.; Tyrovolas, S.; Pavlidou, E.; Antasouras, G.; Psara, E.; Poulios, E.; Vasios, G.K.; Giaginis, C. Pre-Pregnancy Excess Weight Association with Maternal Sociodemographic, Anthropometric and Lifestyle Factors and Maternal Perinatal Outcomes. Nutrients 2022, 14, 3810. [Google Scholar] [CrossRef]
- Mantzorou, M.; Papandreou, D.; Vasios, G.K.; Pavlidou, E.; Antasouras, G.; Psara, E.; Taha, Z.; Poulios, E.; Giaginis, C. Exclusive Breastfeeding for at Least Four Months Is Associated with a Lower Prevalence of Overweight and Obesity in Mothers and Their Children after 2–5 Years from Delivery. Nutrients 2022, 14, 3599. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee.; World Health Organ. Tech. Rep. Ser., 1995; Vol. 854.
-
Centers for Disease Control and Prevention National Health and Nutrition Examination Survey (Nhanes): Anthropometry Procedures Manual; Centers for Disease Control and Prevention: Atlanta, 2007.
- Koutelidakis, A.E.; Alexatou, O.; Kousaiti, S.; Gkretsi, E.; Vasios, G.; Sampani, A.; Tolia, M.; Kiortsis, D.N.; Giaginis, C. Higher Adherence to Mediterranean Diet Prior to Pregnancy Is Associated with Decreased Risk for Deviation from the Maternal Recommended Gestational Weight Gain. International Journal of Food Sciences and Nutrition 2018, 69, 84–92. [Google Scholar] [CrossRef]
- World Health Organization WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and de-Velopment. Geneva: World Health Organization, 2006.
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a Standard Definition for Child Overweight and Obesity Worldwide: International Survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Rosa, M.J.; Hartman, T.J.; Adgent, M.; Gardner, K.; Gebretsadik, T.; Moore, P.E.; Davis, R.L.; LeWinn, K.Z.; Bush, N.R.; Tylavsky, F.; et al. Prenatal Polyunsaturated Fatty Acids and Child Asthma: Effect Modification by Maternal Asthma and Child Sex. J Allergy Clin Immunol 2020, 145, 800–807.e4. [Google Scholar] [CrossRef] [PubMed]
- Olson, C.M.; Demment, M.M.; Carling, S.J.; Strawderman, M.S. Associations Between Mothers’ and Their Children’s Weights at 4 Years of Age. Child Obes 2010, 6, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.B.; Mackenzie, K.C.; Gahagan, S. The Effect of Maternal Obesity on the Offspring. Clin Obstet Gynecol 2014, 57, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Wang, J.; Liao, Z.; Zong, X.; Zhang, T.; Xie, X.; Liu, G. Body Composition in Preschool Children and the Association With Prepregnancy Weight and Gestational Weight Gain: An Ambispective Cohort Study. Frontiers in Nutrition 2022, 9. [Google Scholar] [CrossRef] [PubMed]
- Radaelli, T.; Lepercq, J.; Varastehpour, A.; Basu, S.; Catalano, P.M.; Hauguel-De Mouzon, S. Differential Regulation of Genes for Fetoplacental Lipid Pathways in Pregnancy with Gestational and Type 1 Diabetes Mellitus. Am J Obstet Gynecol 2009, 201, 209.e1–209.e10. [Google Scholar] [CrossRef]
- Catalano, P.M.; Farrell, K.; Thomas, A.; Huston-Presley, L.; Mencin, P.; de Mouzon, S.H.; Amini, S.B. Perinatal Risk Factors for Childhood Obesity and Metabolic Dysregulation. Am J Clin Nutr 2009, 90, 1303–1313. [Google Scholar] [CrossRef] [PubMed]
- Birbilis, M.; Moschonis, G.; Mougios, V.; Manios, Y. Obesity in Adolescence Is Associated with Perinatal Risk Factors, Parental BMI and Sociodemographic Characteristics. Eur J Clin Nutr 2013, 67, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.Y.; Kim, S.Y.; Schmid, C.H.; Dietz, P.M.; Callaghan, W.M.; Lau, J.; Curtis, K.M. Maternal Obesity and Risk of Cesarean Delivery: A Meta-Analysis. Obes Rev 2007, 8, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Bebeau, K.A.; Edenfield, A.L.; Hill, A.; Van Buren, E.; Finneran, M.M.; Meglin, M.F. Impact of Pre-Pregnancy Obesity on Cesarean Delivery Rates in Nulliparous Pregnant People Undergoing Induction of Labor. The Journal of Maternal-Fetal & Neonatal Medicine 2022, 0, 1–6. [Google Scholar] [CrossRef]
- Azeredo, C.M.; Cortese, M.; Munger, K.L.; Ascherio, A. Maternal Prepregnancy BMI and Physical Activity and Type 1 Diabetes in the Offspring. Pediatric Diabetes 2021, 22, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, A.; Prowak, M.; Berlandi-Short, V.-M.; Garay, J.; Ramalingam, L. Maternal Obesity: A Focus on Maternal Interventions to Improve Health of Offspring. Frontiers in Cardiovascular Medicine 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Babili, M.G.; Amerikanou, C.; Papada, E.; Christopoulos, G.; Tzavara, C.; Kaliora, A.C. The Effect of Prenatal Maternal Physical Activity and Lifestyle in Perinatal Outcome: Results from a Greek Study. European Journal of Public Health 2020, 30, 328–332. [Google Scholar] [CrossRef]
- Iglesia Altaba I, Larqué E, Mesa MD, Blanco-Carnero JE, Gomez-Llorente C, Rodríguez-Martínez G, Moreno LA. Early Nutrition and Later Excess Adiposity during Childhood: A Narrative Review. Horm Res Paediatr. 2022, 95, 112–119. [CrossRef]
- López-Gil JF, García-Hermoso A, Sotos-Prieto M, Cavero-Redondo I, Martínez-Vizcaíno V, Kales SN. Mediterranean Diet-Based Interventions to Improve Anthropometric and Obesity Indicators in Children and Adolescents: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Adv Nutr. 2023, 29, S2161–8313(23)00296. [CrossRef]
- Kim J, Lim H. Nutritional Management in Childhood Obesity. J Obes Metab Syndr. 2019, 28, 225–235. [CrossRef]
- Naureen Z, Dhuli K, Donato K, Aquilanti B, Velluti V, Matera G, Iaconelli A, Bertelli M. Foods of the Mediterranean diet: tomato, olives, chili pepper, wheat flour and wheat germ. J Prev Med Hyg. 2022, 63 (Suppl. 3), E4–E11. [CrossRef]
- Antonopoulou M, Mantzorou M, Serdari A, Bonotis K, Vasios G, Pavlidou E, Trifonos C, Vadikolias K, Petridis D, Giaginis C. Evaluating Mediterranean diet adherence in university student populations: Does this dietary pattern affect students’ academic performance and mental health? Int J Health Plann Manage. 2020, 35, 5–21. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).