1. Introduction
Nowadays, advances in clinical techniques and biomaterials have facilitated the broadening of indications for immediate implant treatment [
1,
2]. Over the years, different types of implants and their positioning and loading protocols have evolved from the first protocols with the aim to obtain faster and easier surgical treatment times [
3]. The immediate placement of dental implants in extraction sockets was described for the first time by Schulte and Heimke more than 40 years ago [
4]. Since then and as recently reported, preclinical, clinical, and radiological studies have allowed significant advances in understanding the hard and soft tissue alterations in post-extraction sites [
5]. Then, it has been reported that the immediate dental implant loading procedure provides substantial advantages for the patient [
6]. Thus, the immediate implant placement and provisionalization in post-extractive sockets have been proposed. As an example, Mura and collaborators [
6], in a retrospective 5-year analysis of immediately loaded tapered implants placed in post-extraction sockets, have shown promising results concerning the implant survival, the soft tissue response, and the peri-implant marginal bone condition. Moreover, Han et al. [
7] performed a comparison between survival, stability, and possible complications of immediately loaded tapered implants placed either in post-extraction or in healed sockets, and complications and failures were not reported to be significantly different between these two groups.
On the other hand, Mello et al. [
8] conducted a systematic review with meta-analysis on the implant survival and possible peri-implant tissue modifications. Comparing immediate implant insertion in fresh extraction sockets and implant positioning in healed sites, they found that delayed implants reported a significantly higher survival in respect to immediate implants. Contrarily, no differences were reported between the two groups as regards the marginal bone loss, the Implant Stability Quotient (ISQ) values, and the pocket probing depth. Similar results were reported in a recent systematic review [
9] that compared post-extraction alveolar ridge preservation and the immediate implant insertion. Other authors, instead, asserted that an immediate implant insertion placement could be considered in post-extraction sites, since a limited amount of bone resorption was described [
10]. However, other techniques, such as socket preservation using biomaterials and/or membranes, may be preferred when these conditions are not present.
In 2015 Kashi et al. [
11] led an in vitro study on polyurethane foam sheets with the aim to evaluate the primary stability of titanium implants inserted with different angle degrees. For this purpose, artificial bone types II and IV were used, as well as angulations of 0, 10, and 20 degrees and implants inserted with 10 degrees of angulation in a type II artificial bone revealed a better primary stability. When using a polyurethane in vitro model also mimicking an extraction site, instead, it was also demonstrated that the implant design could have a pivotal role in obtaining an adequate primary stability in challenging situations [
12]. Moreover, Yim et al. [
13], in a bovine bone in vitro study, reported that in peri-implant bone defects varying from 2 to 8 mm, decreased ISQ values and increased Periotest values were observed with the increase of the defect width.
Thus, the aim of the present study was to compare the stability of two types of conical implants (TAC and INTRALOCK) and a cylindrical one (CYROTH), when inserted with an angulation of 15-20 degrees in 10 and 20 Pounds per Cubic Foot (PCF) low density polyurethane blocks with or without the presence of a cortical lamina (30 PCF in density), potentially mimicking the post-extraction condition in vivo.
2. Materials and Methods
2.1. Implants Description
Three types of implants were used for tests in each experimental condition:
TAC conical implants (Aon Implants, Grisignano di Zocco, Italy);
INTRALOCK conical implants (Intra-Lock System Europa Spa, Salerno, Italy);
CYROTH cylindrical implants (Aon Implants, Grisignano di Zocco, Italy).
All implants had the same dimensions (4 × 15 mm).
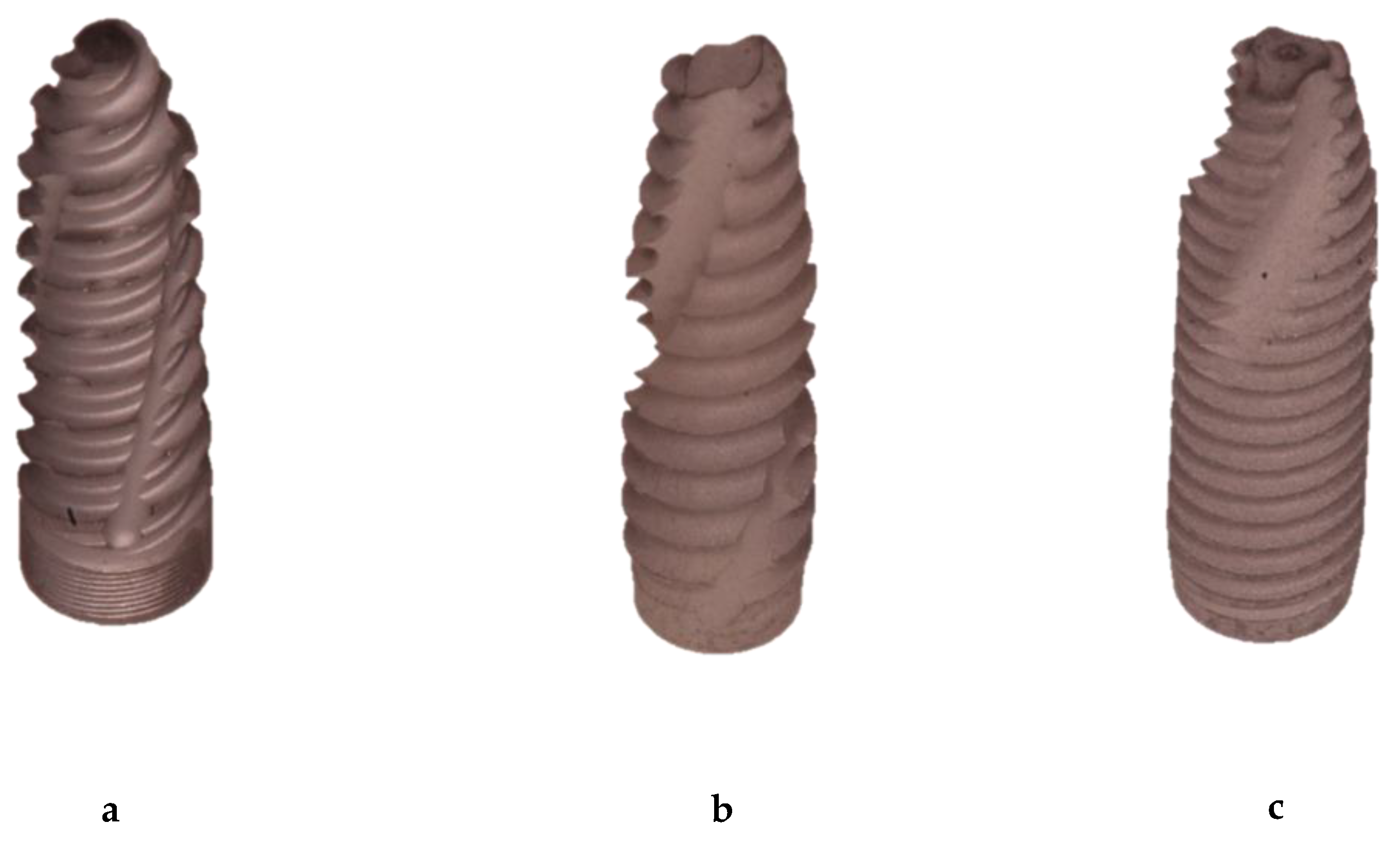
TAC implant macromorphology showed a more tapered and less aggressive collar shape, instead, threads were sharper and more aggressive. They presented a single-threaded design and there was a flat implant apex.
INTRALOCK implants had a more pronounced conical shape and a 2 mm wider enlargement of the profile on the most coronal portion. The threads presented a triple pitch of the coil and there was a round apex.
CYROTH cylindrical implants had a slightly tapered collar with less aggressive threads, which tended to compress and deform the material rather than cutting it. They presented also a conical apex (
Figure 1).
2.2. Drilling Protocol and Implants Insertion
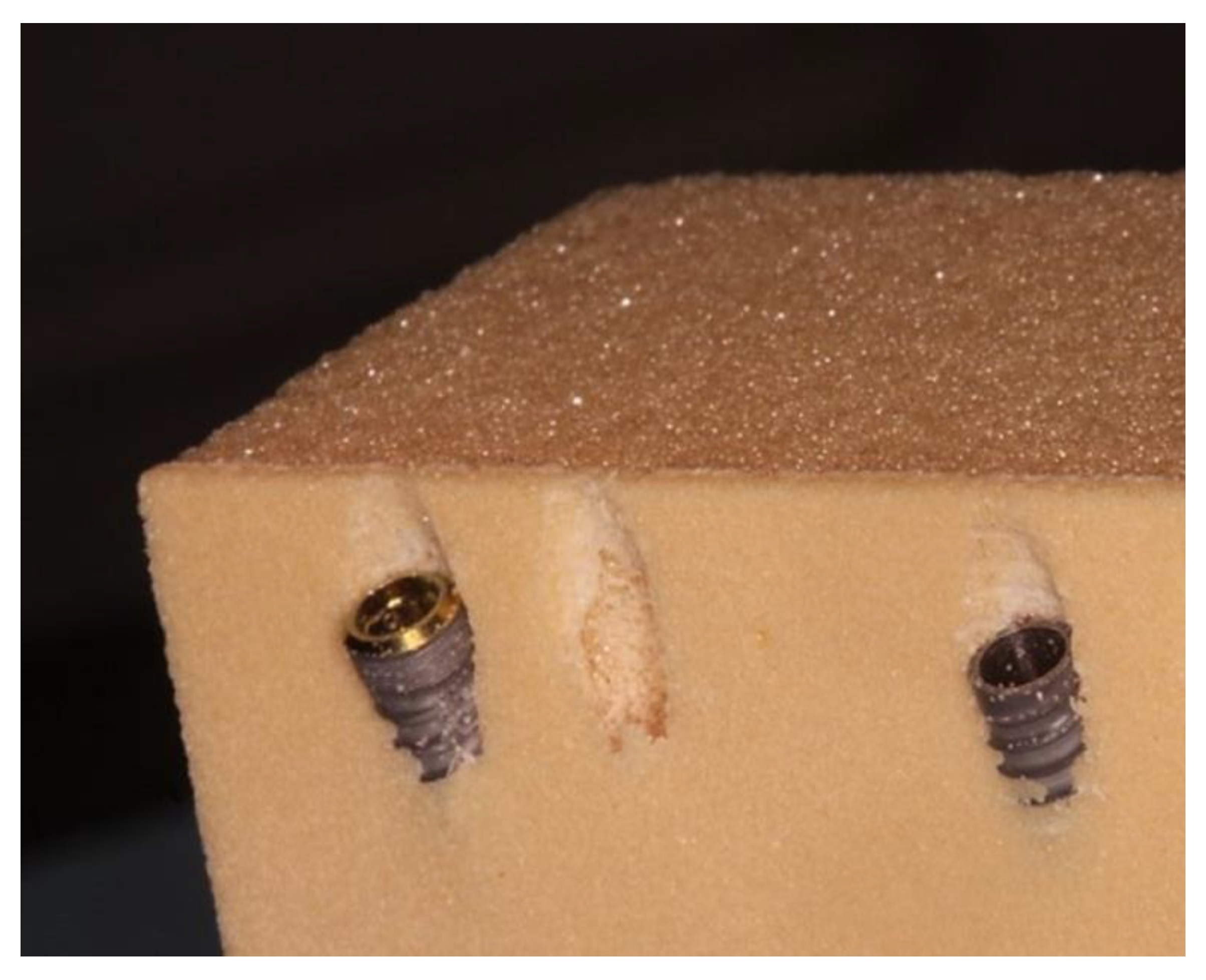
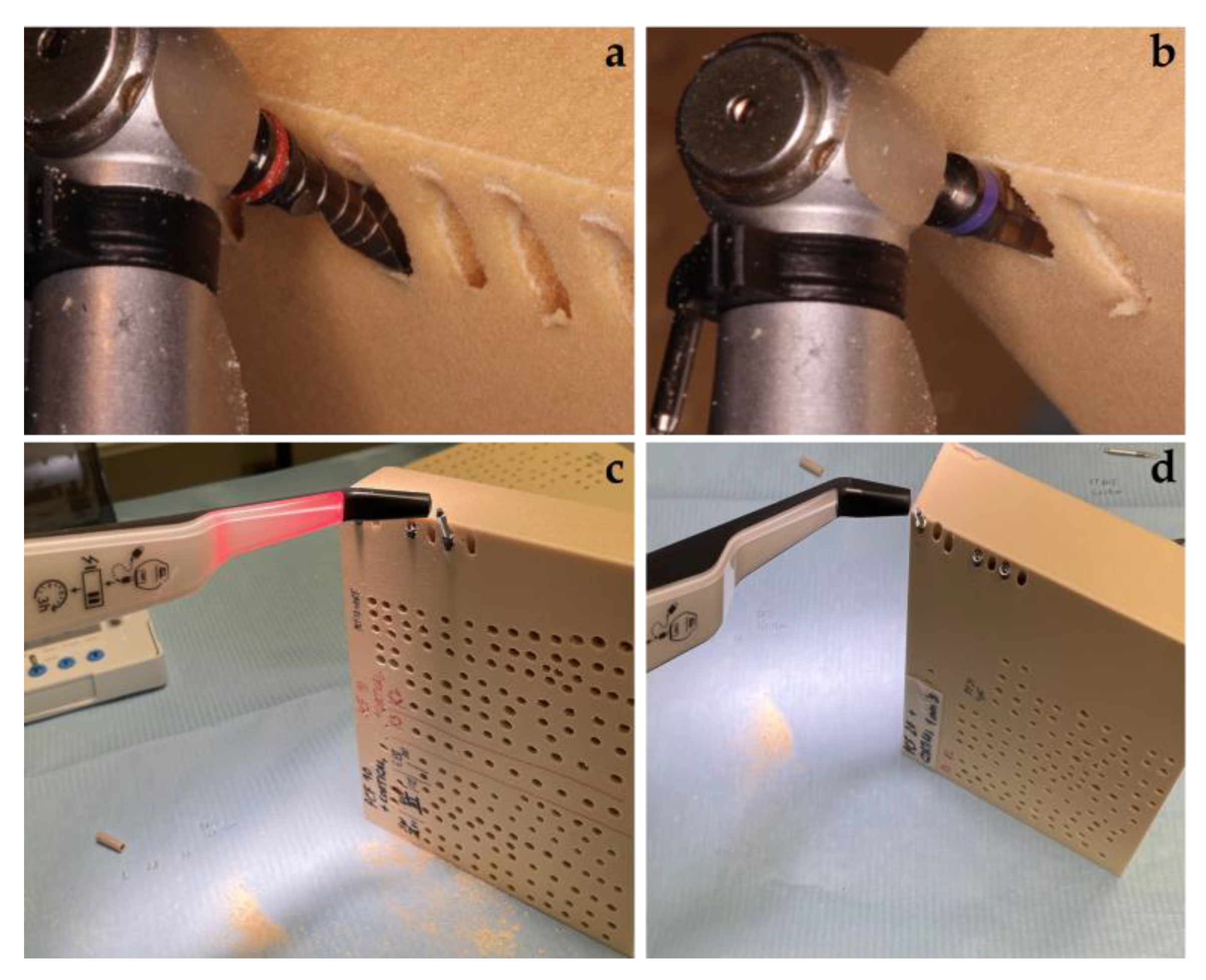
The drilling protocol was performed by using an initial lanceolate bur at 300 rpm for all implants, followed by a 2.2 mm bur (AUN22300DR000, Aon Implants, Grisignano di Zocco, Italy) for TAC and CYROTH implants or a 2.0 mm bur (D-2015, Intra-Lock System Europa Spa, Salerno, Italy) for INTRALOCK implants, both used at 300 rpm. In order to finalize protocols, TAC and CYROTH implants were drilled with a 3.2 mm bur (AUN32000DR000, Aon Implants, Grisignano di Zocco, Italy), whereas INTRALOCK implants with a 4 mm conical bur (D-CT4D, Intra-Lock System Europa Spa, Salerno, Italy), both at 300 rpm. For this purpose, a Bien Air Chiropro (Bien Air SA, Bienne, Switzerland) surgical implant motor was used. The final implant insertion was performed at 30 rpm with a 50 N standardized torque value and an inclination of 15-20 degrees, and then, the IT and RT were evaluated in the last 1 mm during the implant seating, considered at 2 mm below the polyurethane block superficial profile. The n° 78 Smart Peg (Osstell AB, Gothenburg, Sweden) was used to evaluate the RFA of Bucco-Lingual (RFA-BL) and Mesial-Distal (RFA-MD) values (
Figure 2 and
Figure 3).
As regards polyurethane foam blocks, they are constituted by a well-known material used to mimic the natural bone, since it has pronounced mechanical characteristics, avoiding human variables or particular handling and preservation treatments whilst preserving similar bone properties [
14,
15,
16,
17]. Nowadays, it is also preferred to cadaver or animal bones for ethical reasons, and it is used as an alternative material to perform biomechanical tests regarding orthopedic or dental medical devices [
18,
19,
20].
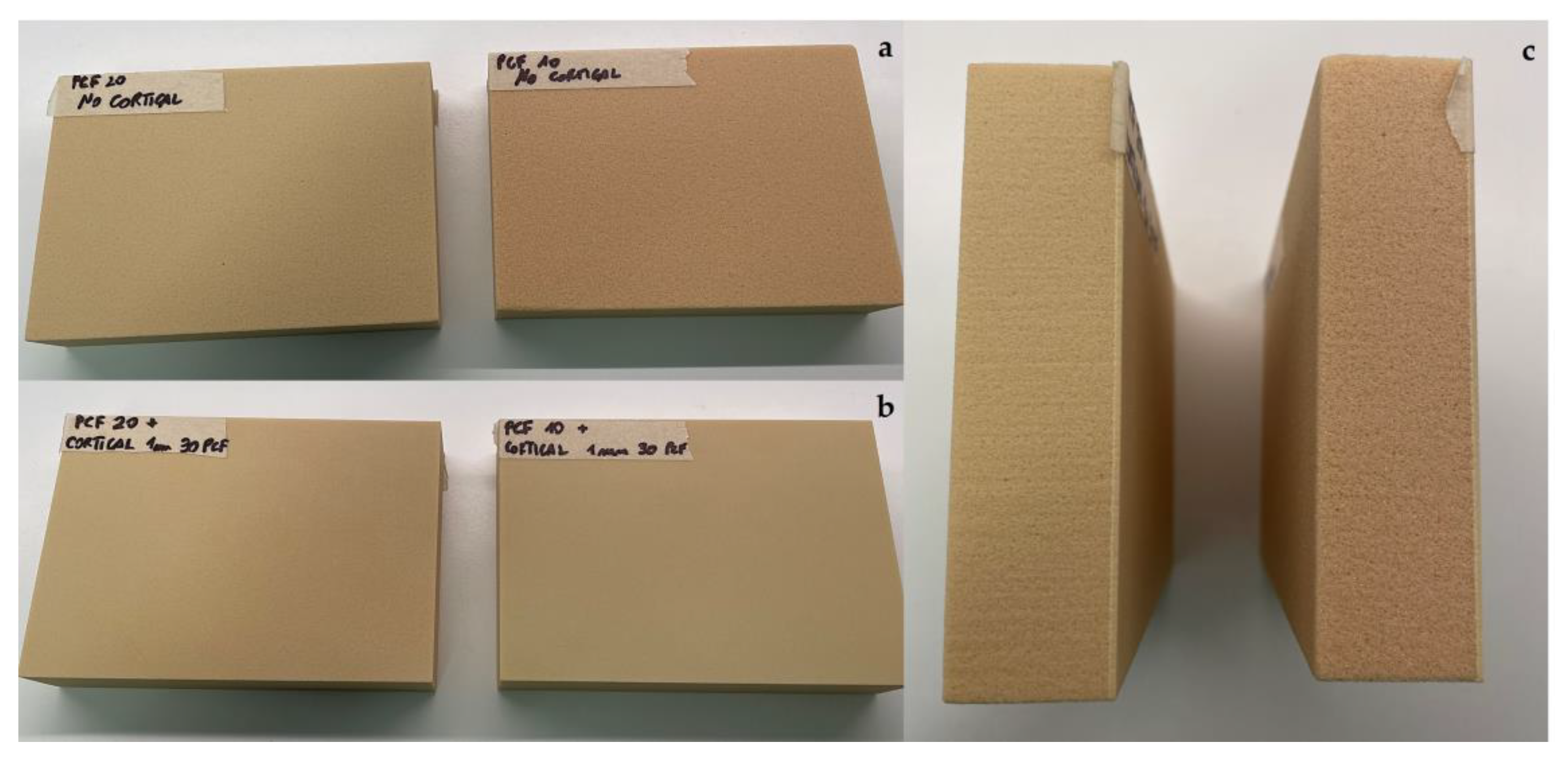
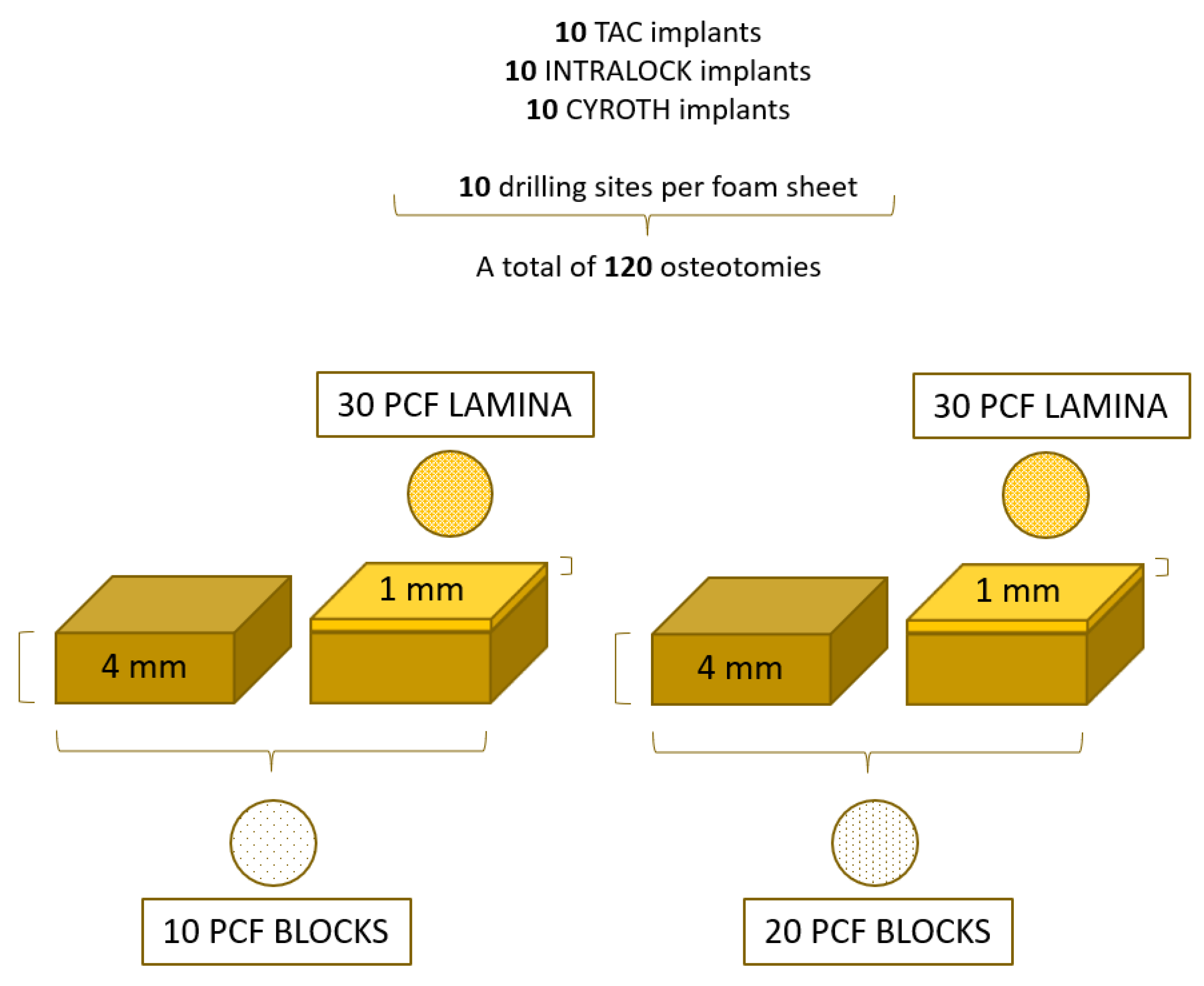
In this study were used 4-mm thickness blocks with densities of 10 and 20 PCF (Sawbones Europe AB, Malmö, Sweden), corresponding to a density of 0.16 g/cm
3 and 0.32 g/cm
3, mimicking a D3 and D2 natural bone types, respectively. In addition, a 1-mm thickness sheet with a density of 30 PCF (corresponding to a density of 0.48 g/cm
3, similar to the D1 bone type) was added to the previous blocks when used to mimic the cortical bone [
21] (
Figure 4).
At the end, 10 implant sites were prepared for each implant type in all polyurethane densities, obtaining a total of 120 osteotomies (
Figure 5).
2.3. Statistical Analysis
Power analysis and sample size planning were calculated using the ANCOVA statistical test (effect size: 0.48, α err: 0.05; power (1-β): 0.95; numerator df: 10; number of groups: 3; number of covariates: 12), using G*Power 3.1.9.7 program. The result of the minimum sample size necessary to achieve a statistically significant output was 116 implant sites and a total of 120 sites were performed in this study. The Shapiro–Wilk test was applied to evaluate the normal distribution of data. Subsequently, the differences between the IT, RT, and RFA values of the study groups were evaluated using a one-way analysis of variance (ANOVA) test, followed by Bonferroni post-hoc test. A p-value < 0.05 was considered statistically significant. The research data and the statistical analysis were elaborated using the statistical software package GraphPad 9.0 (Prism, San Diego, CA, USA). Data were expressed as the mean ± Standard Deviation (SD).
3. Results
The experimental results related to the IT, RT, RFA-BL, and RFA-MD values evaluation and comparison are reported in
Table 1. These values were obtained from independent measurements related to different implants inserted in each artificial bone condition.
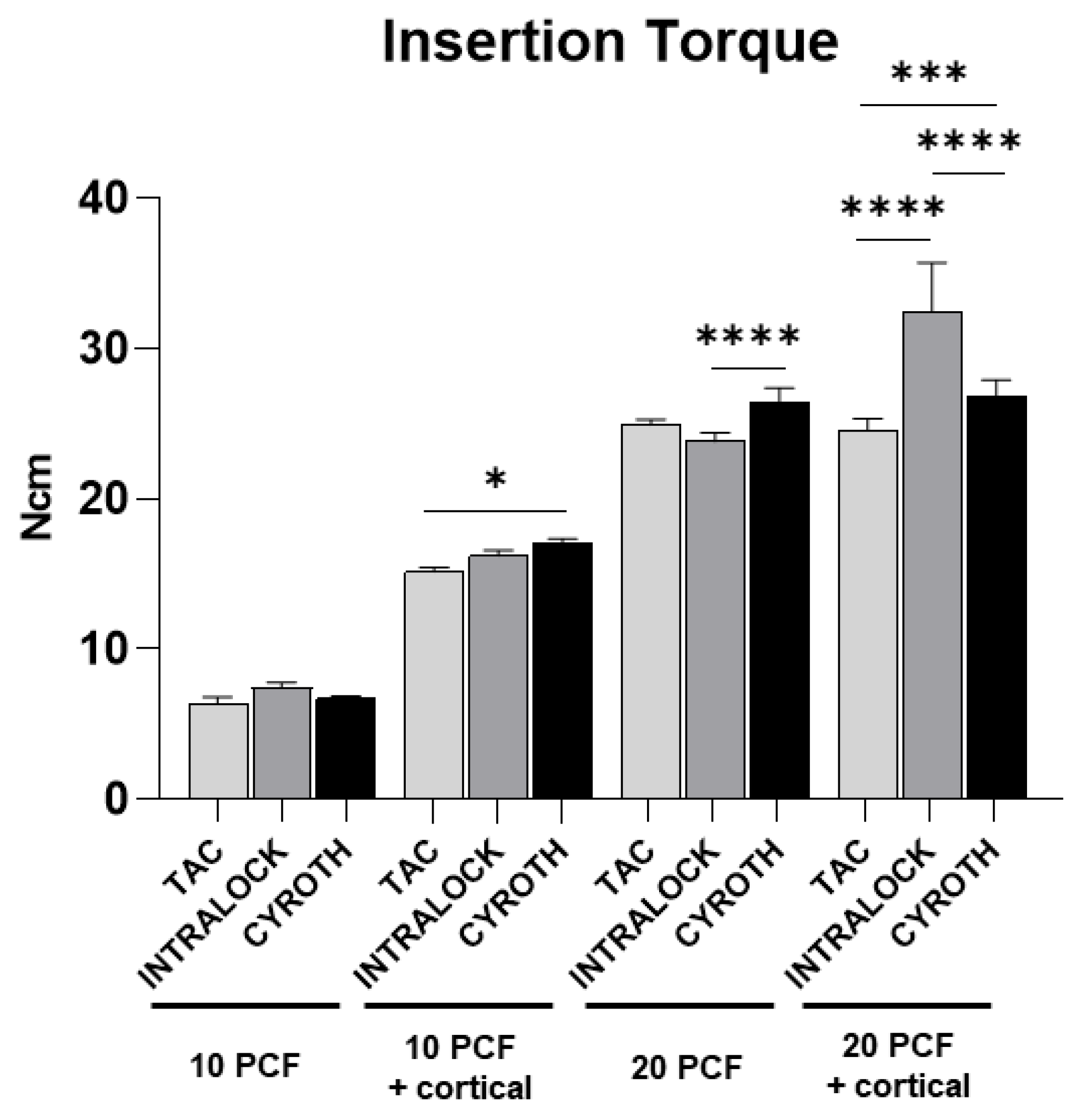
3.1. Insertion Torque Evaluation
IT values appeared directly proportional to the polyurethane density, showing lower values in the lowest-density block of 10 PCF in density without the cortical sheet for all implant types, with a mean ± SD of 6.39 ± 0.41, 7.44 ± 0.34, and 6.73 ± 0.16 Ncm for TAC, INTRALOCK, and CYROTH implants, respectively. Specifically, TAC implants showed the lowest IT value (5.90 Ncm), but without statistically significant differences. On the other hand, higher values were found in the block of 10 PCF density with the cortical sheet (with a mean ± SD of 15.16 ± 0.30 Ncm for TAC, 16.23 ± 0.36 Ncm for INTRALOCK, and 17.06 ± 0.30 Ncm for CYROTH implants), in the block of 20 PCF density without the cortical sheet (with a mean ± SD of 24.93 ± 0.34 Ncm for TAC, 23.83 ± 0.59 Ncm for INTRALOCK, and 26.42 ± 0.96 Ncm for CYROTH implants), and in the block of 20 PCF density with the cortical sheet (with a mean ± SD of 24.63 ± 0.72 Ncm for TAC, 32.44 ± 3.28 Ncm for INTRALOCK, and 26.87 ± 1.04 Ncm for CYROTH implants). In particular, INTRALOCK implants showed the highest IT value (37.20 Ncm) in the highest-density block with significant differences in respect to the others (p<0.0001).
Figure 6 reported all the statistically significant differences concerning IT measurements expressed by the implant types in the different experimental artificial bone densities.
Statistically significant higher values were found for CYROTH implants when inserted in the block of 10 PCF density with the cortical sheet and in the block of 20 PCF density without the cortical sheet compared to TAC and INTRALOCK implants, respectively, as well as for those inserted in the block of 20 PCF density with the cortical sheet, when compared to TAC implants. Conversely, INTRALOCK implants showed a statistical significance only when inserted in the highest-density block, reporting comparable results to CYROTH implants in the blocks of 10 PCF density with and without the cortical sheet.
Overall, TAC implants resulted in slightly lower IT values in all the experimental conditions, except for the blocks of 10 and 20 PCF densities with the cortical sheet. However, they exhibited good IT values in all situations (14.7-25.5 Ncm) that were compatible with the mechanical implant stability, except for the block of 10 PCF density without the cortical sheet but showing no statistical differences with other implants’ values.
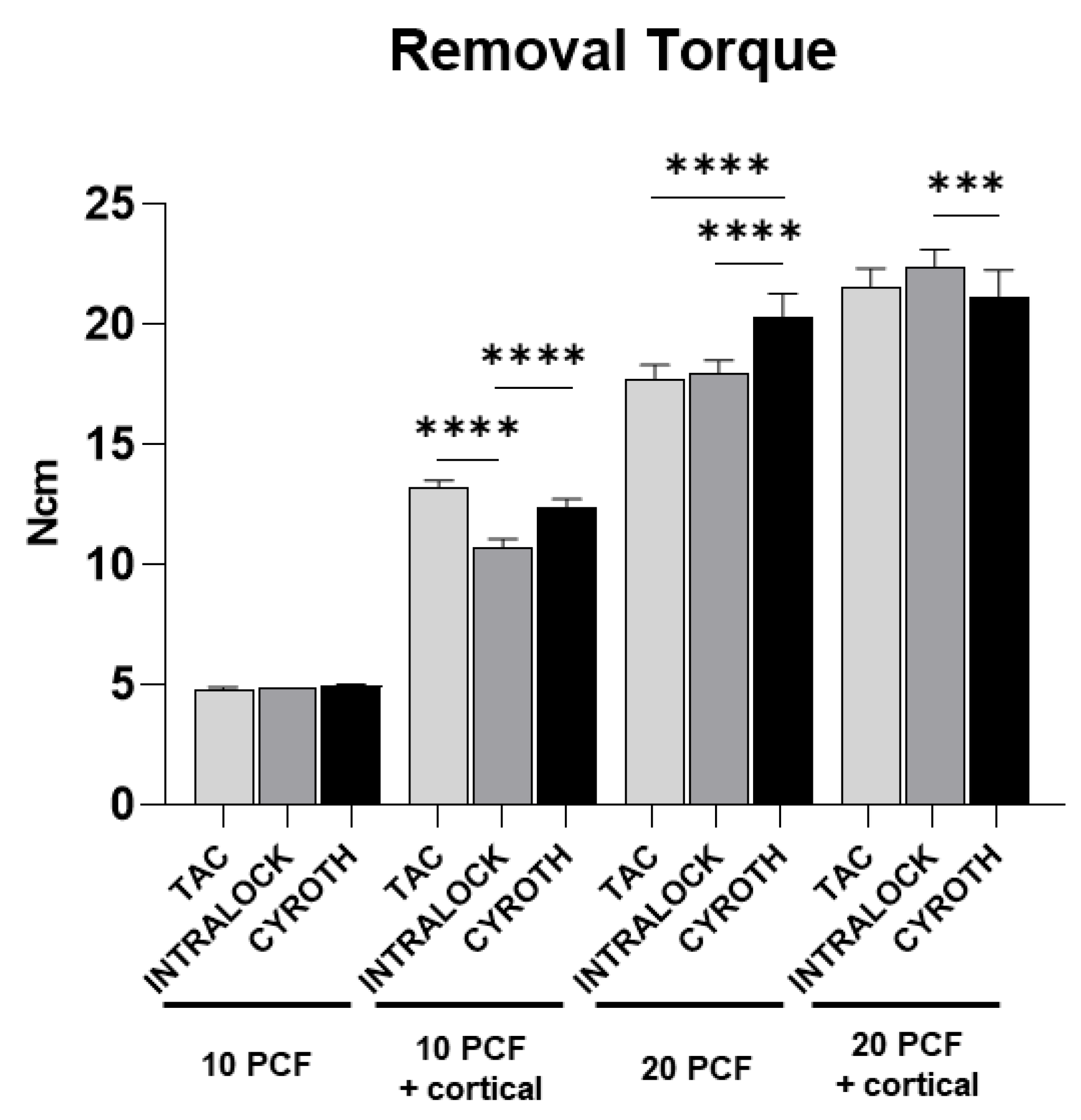
3.2. Removal Torque Evaluation
RT values were proportional to the polyurethane density as well, showing the highest values in the block of 20 PCF with the cortical sheet (with a mean ± SD of 21.60 ± 0.75 Ncm for TAC, 22.41 ± 0.72 Ncm for INTRALOCK, and 21.15 ± 1.14 Ncm for CYROTH implants) and the lowest ones in the block of 10 PCF density without the cortical sheet (with a mean ± SD of 4.81 ± 0.10 Ncm for TAC, 4.90 ± 0.00 Ncm for INTRALOCK, and 4.95 ± 0.08 Ncm for CYROTH implants). TAC implants showed the lowest RT values in the latest mentioned block (4.70 Ncm), whereas the highest results were reported by INTRALOCK implants in the thickest block of 20 PCF density with the cortical sheet (23.50 Ncm).
Figure 7 showed that RT values of all implant types inserted in the block of 10 PCF density without the cortical sheet were very low (about 5.00 Ncm), without reaching a statistical significance.
INTRALOCK and TAC implants reported comparable values in all experimental conditions, except for the 10 PCF density block with the cortical sheet, where both TAC and CYROTH implants showed significantly higher results (p<0.0001). CYROTH implants also showed significantly higher RT values in respect to both other implants in the block of 20 PCF density without the cortical sheet. On the other hand, INTRALOCK implants reported the highest results in the block of 20 PCF density with the cortical sheet, but showing a statistical significance only when compared to CYROTH implants.
For all implants the RT was always lower than the correspoding IT. Higher differences between IT and RT values were found for INTRALOCK implants (more than 10 Ncm in the 20 PCF density block with the cortical sheet) compared with TAC and CYROTH implants (4-6 Ncm lower). In the lowest-density block there were lower differences between IT and RT values.
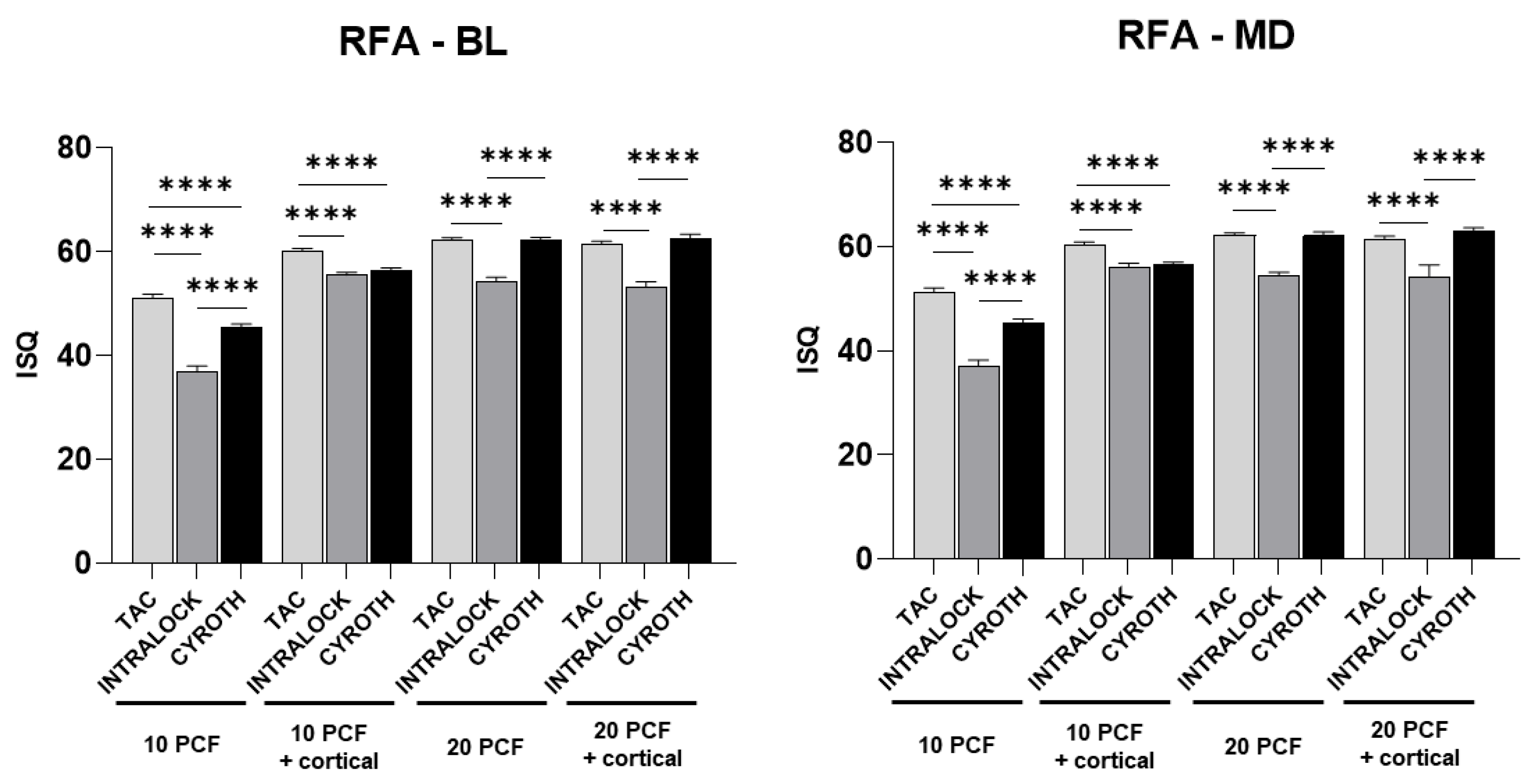
2.3. Resonance Frequency Analysis Evaluation
RFA values, instead, were consistently higher for conical TAC implants in all the experimental conditions, especially in the lowest-density blocks (for example, with a mean ± SD of 51.20 ± 0.92 ISQ in the 10 PCF density block without the cortical sheet and 60.40 ± 0.52 ISQ in the 10 PCF density block with the cortical sheet, compared to 37.00 ± 1.25 and 56.00 ± 0.82 ISQ of INTRALOCK, and 45.30 ± 0.82 and 56.50 ± 0.53 ISQ of CYROTH implants in the same conditions), reaching the statistical significance (p<0.0001). Only in 20 PCF density blocks with and without the cortical sheet ISQ values were similar for conical TAC (61.50 ± 0.53 and 62.20 ± 0.42 ISQ, respectively) and cylindrical CYROTH implants (62.90 ± 0.74 and 62.10 ± 0.74 ISQ, respectively), both significantly higher than those of INTRALCOK implants (
Figure 8).
4. Discussion
Primary stability is considered as the crucial factor to reach implant success and it was demonstrated to be mostly affected by implant macro-geometry and IT [
22,
23]. In particular, reaching an ideal primary stability in the posterior maxilla, corresponding to a D3 bone, represents a key factor for an immediate implant loading protocol, due to the low density of bone [
24]. Thus, in this in vitro study the effect of different dental implant shapes with the same dimensions on the IT, RT, and primary stability has been evaluated after their insertion in polyurethane foam blocks with different densities simulating a poor natural bone and post-extraction sites.
In the past, other authors [
25] proposed to use a tapered design of the implant in order to improve primary stability in a low-quality bone, since this macro-geometry was able to increase the pressure on the cortical bone in poor bone regions. This fact could be relevant when implants are immediately or early loaded in poor quality bone districts.
In this study, TAC implants have a the more tapered and less aggressive coronal portion compared to the other implants used. In fact, the implant insertion proceeded easily and progressively increasing the IT since the final positioning, without undergo deviations and preserving the superficial profile of the material. Compared to INTRALOCK and CYROTH implants, there was a reduction in IT values that, however, allowed a more precise implant positioning without affecting the prepared site or excessively stressing the internal portion of the Cone-Morse connection. Interestingly, the registered ISQ values were the highest in all situations, even in low-density blocks (51.20 ± 0.92, 60.40 ± 0.52, 62.30 ± 0.48, and 61.50 ± 0.53 ISQ for 10 and 20 PCF density blocks without and with the cortical sheet, respectively), more likely due to the precise fitting of the implant during the insertion process, without being subjected to deviations. Regarding the implant threads and differently from the INTRALOCK profile and apex, these implants had a more cutting and aggressive thread profile, which could be able to penetrate the polyurethane material, even without the use of a drilling protocol. This fact could be especially useful in post-extraction conditions since it could help directing the implant insertion and its adjustment when necessary and without the affection of the coronal portion.
On the other hand, the INTRALOCK implant’s macro-geometry is more conical than TAC implants and it has a 2 mm wider profile in the most coronal portion. This latter could be probably responsible of the higher IT values in the 20 PCF density block with the cortical sheet. In fact, the torque value increases when this part of the implant engages the polyurethane, even if it may cause a slight deviation of the implant during the insertion towards the extraction defect. This phenomenon is frequently seen when inserting a post-extraction implant in the maxilla of a patient when the implant used has a wider profile in its coronal portion and meets a higher density in the palatal bone [
26]. This fact could also contribute to decrease the ISQ values, because the implant does not exactly fit into the prepared site, but undergo a slight deviation, in part losing contact with the polyurethane. This phenomenon becomes more significant in lower density blocks (36.80 ± 1.23 ISQ in the 10 PCF block without the cortical sheet).
CYROTH cylindrical implants, instead, presented a tapered coronal portion and a slight conicity when moving towards the apex, as well as less aggressive threads that tended to compress and deform the material rather than cutting it. This morphology resulted in good IT values, except for the lowest-density block (6.73 ± 0.16 Ncm), but producing a slight deviation toward the defect, as for INTRALOCK implants. This fact, together with the macro-geometry, could determine a significant decrease in ISQ values in respect to TAC implants, especially in 10 PCF density blocks (45.30 ± 0.82 and 56.50 ± 0.53 ISQ), but never lower than INTRALOCK implants.
As described in literature [
27], not always a high IT corresponds to a high ISQ, but high RFA values may be more desirable than a high IT for an immediate loading protocol to guarantee a better bone-to-implant contact. In this context, analyzing data reported in this study for post-extraction conditions, it was possible to assess that all implants presented IT values > 15 Ncm in all polyurethane densities, except for the 10 PCF block without the cortical sheet, with highest values for INTRALOCK implants (32.44 ± 3.28 Ncm in the 20 PCF block with the cortical sheet), but considering a possible loss of direction during implant insertion. Contrarily, they always showed the lowest ISQ values in all situations (from 36.80 ± 1.23 to a maximum of 56.00 ± 0.82 ISQ in 10 PCF blocks without and with the cortical sheet, respectively) when compared to CYROTH and TAC implants. In specific, these latter also showed higher ISQ values than CYROTH, especially in the lowest-density bone (51.20 ± 0.92 in comparison with 45.30 ±0.82 ISQ). Thanks to their threads profile and apex shape, besides the conical macro-morphology, TAC implants may be considered as the most performing implants for immediate loading simulation in post-extraction sites in all the artificial bone densities tested, as also corroborated by previous studies [
28]. Probably, when using TAC implants in low-density bones, a higher value of under-preparation (from 3.2 mm to 2.2 mm) could also help reaching a higher IT value, which in combination with their high ISQ value make these implants appropriate also for immediate loading in low-density bones [
21].
At the end, it is necessary to shed the light on the due limitations of this in vitro study that, albeit presenting comfortable data and a standardized artificial bone model [
29], could obviously never be comparable to an ex vivo or clinical study. Even if the use of a polyurethane material could offer preliminary information on the biomechanical behavior of dental implants in different bone consistencies [
19], further experimental and clinical studies to corroborate these results on implant stability are needed. The analyzed parameters could be affected by physiological or pathological patient’s conditions and by other variables concerning the bone density, such as the presence of natural bone or other grafting materials.
5. Conclusions
The present in vitro study performed in low-density polyurethane foam blocks demonstrated that the conical implant shape could be considered the most performing in post-extraction conditions, due to the higher primary stability values reported, in spite of the IT ones. In particular, TAC implants macro-morphology has reported the best results in terms of ISQ in all the polyurethane conditions and especially in lower density blocks, besides adequate values of IT and RT. Although further experimental studies are needed, in future a more standardized site under-preparation could help obtaining higher IT values to make these implants ideal for an immediate loading protocol in low-density bones.
Author Contributions
Conceptualization, L.C., U.C. and A.P.; methodology, L.C. and M.T.; software, T.R.; validation, T.R., N.D.P. and L.M.; formal analysis, T.R. and H.H.S.H.; investigation, L.C.; resources, L.C. and U.C.; data curation, T.R., H.H.S.H. and N.D.P.; writing—original draft preparation, L.C., M.T., A.P., T.R. and N.D.P.; writing—review and editing, A.P., U.C. and N.D.P.; visualization, F.I.; supervision, L.C. and A.P.; project administration, L.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article and available on request from the corresponding author.
Acknowledgments
We thank AoN Implants S.r.l. Company (Grisignano di Zocco, Vicenza, Italy) and Intra-Lock System Europa SpA Company (Salerno, Italy) for providing the implants at no cost.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gautam, S.; Bhatnagar, D.; Bansal, D.; Batra, H.; Goyal, N. Recent Advancements in Nanomaterials for Biomedical Implants. Biomed. Eng. Adv. 2022, 100029. [Google Scholar] [CrossRef]
- Araújo, M.G.; Silva, C.O.; Souza, A.B.; Sukekava, F. Socket Healing with and without Immediate Implant Placement. Periodontol. 2000 2019, 79, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Dhami, B.; Shrestha, P.; Gupta, S.; Pandey, N. Immediate Implant Placement: Current Concepts. J. Nepal. Soc. Periodontol. Oral Implantol. 2019, 3, 18–24. [Google Scholar] [CrossRef]
- Schulte, W.; Heimke, G. The Tübinger Immediate Implant. Quintessenz 1976, 27, 17–23. [Google Scholar] [PubMed]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant Placement Post Extraction in Esthetic Single Tooth Sites: When Immediate, When Early, When Late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Mura, P. Immediate Loading of Tapered Implants Placed in Postextraction Sockets: Retrospective Analysis of the 5-year Clinical Outcome. Clin. Implant Dent. Relat. Res. 2012, 14, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Han, C.-H.; Mangano, F.; Mortellaro, C.; Park, K.-B. Immediate Loading of Tapered Implants Placed in Postextraction Sockets and Healed Sites. J. Craniofac. Surg. 2016, 27, 1220–1227. [Google Scholar] [CrossRef]
- Mello, C.C.; Lemos, C.A.A.; Verri, F.R.; Dos Santos, D.M.; Goiato, M.C.; Pellizzer, E.P. Immediate Implant Placement into Fresh Extraction Sockets versus Delayed Implants into Healed Sockets: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 1162–1177. [Google Scholar] [CrossRef]
- Yu, X.; Teng, F.; Zhao, A.; Wu, Y.; Yu, D. Effects of Post-Extraction Alveolar Ridge Preservation versus Immediate Implant Placement: A Systematic Review and Meta-Analysis. J. Evid. Based. Dent. Pract. 2022, 101734. [Google Scholar] [CrossRef]
- Chappuis, V.; Araújo, M.G.; Buser, D. Clinical Relevance of Dimensional Bone and Soft Tissue Alterations Post-extraction in Esthetic Sites. Periodontol. 2000 2017, 73, 73–83. [Google Scholar] [CrossRef]
- Kashi, A.; Gupta, B.; Malmstrom, H.; Romanos, G.E. Primary Stability of Implants Placed at Different Angulations in Artificial Bone. Implant Dent. 2015, 24, 92–95. [Google Scholar] [CrossRef]
- Karl, M.; Irastorza-Landa, A. Does Implant Design Affect Primary Stability in Extraction Sites. Quintessence Int 2017, 48, 219–224. [Google Scholar]
- Yim, H.; Lim, H.-C.; Hong, J.-Y.; Shin, S.-I.; Chung, J.-H.; Herr, Y.; Shin, S.-Y. Primary Stability of Implants with Peri-Implant Bone Defects of Various Widths: An in Vitro Investigation. J. Periodontal Implant Sci. 2019, 49, 39–46. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Piattelli, A.; Iezzi, G.; Orlando, F.; Arosio, P. Cortical Thickness, Bone Density, and the Insertion Torque/Depth Integral: A Study Using Polyurethane Foam Blocks. Int. J. Oral Maxillofac. Implants 2021, 36. [Google Scholar] [CrossRef]
- Petrini, M.; Tumedei, M.; Cipollina, A.; D’Ercole, S.; Carmine, M.S. Di; Piattelli, A.; Re, M.; Iezzi, G. Fixture Length and Primary Stability: An In Vitro Study on Polyurethane Foam. Appl. Sci. 2022, 12, 2683. [Google Scholar] [CrossRef]
- Hollensteiner, M.; Fürst, D.; Esterer, B.; Augat, P.; Schrödl, F.; Hunger, S.; Malek, M.; Stephan, D.; Schrempf, A. Novel Bone Surrogates for Cranial Surgery Training. J. Mech. Behav. Biomed. Mater. 2017, 72, 49–51. [Google Scholar] [CrossRef]
- Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopedic Devices and Instruments. ASTM F-1839-08; . ASTM International: West Conshohocken, PA, USA, 2021.
- Comuzzi, L.; Tumedei, M.; Romasco, T.; Petrini, M.; Afrashtehfar, K.I.; Inchingolo, F.; Piattelli, A.; Di Pietro, N. Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets. J. Funct. Biomater. 2023, 14, 10. [Google Scholar] [CrossRef] [PubMed]
- Tsolaki, I.N.; Tonsekar, P.P.; Najafi, B.; Drew, H.J.; Sullivan, A.J.; Petrov, S.D. Comparison of Osteotome and Conventional Drilling Techniques for Primary Implant Stability: An In Vitro Study. J. Oral Implant. 2016, 42, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.S.; Shepherd, D.E.; Hukins, D.W. Compressive properties of commercially available polyurethane foams as mechanical models for osteoporotic human cancellous bone. BMC Musculoskelet Disord. 2008, 9, 137. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; Covani, U.; Romasco, T.; Petrini, M.; Montesani, L.; Piattelli, A.; Di Pietro, N. Primary Stability Assessment of Conical Implants in Under-Prepared Sites: An In Vitro Study in Low-Density Polyurethane Foams. Appl. Sci. 2023, 13, 6041. [Google Scholar] [CrossRef]
- Staedt, H.; Palarie, V.; Staedt, A.; Wolf, J.M.; Lehmann, K.M.; Ottl, P.; Kämmerer, P.W. Primary Stability of Cylindrical and Conical Dental Implants in Relation to Insertion Torque—a Comparative Ex Vivo Evaluation. Implant Dent. 2017, 26, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, M.V.; Elias, C.N.; Cavalcanti Lima, J.H. The Effects of Superficial Roughness and Design on the Primary Stability of Dental Implants. Clin. Implant Dent. Relat. Res. 2011, 13, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Pommer, B.; Hof, M.; Fädler, A.; Gahleitner, A.; Watzek, G.; Watzak, G. Primary implant stability in the atrophic sinus floor of human cadaver maxillae: impact of residual ridge height, bone density, and implant diameter. Clin Oral Implants Res. 2014, 2, 109–13. [Google Scholar] [CrossRef] [PubMed]
- Wilson Jr, T.G.; Miller, R.J.; Trushkowsky, R.; Dard, M. Tapered Implants in Dentistry: Revitalizing Concepts with Technology: A Review. Adv. Dent. Res. 2016, 28, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.J.; Levin, B.P.; Egbert, N.; Saito, H.; Nevins, M. Use of a Novel Implant with an Inverted Body-Shift and Prosthetic Angle Correction Design for Immediate Tooth Replacement in the Esthetic Zone: A Clinical Case Series. Int J Periodontics Restorative Dent. 2021, 2, 195–204. [Google Scholar] [CrossRef]
- Lages, F.S.; Douglas-de Oliveira, D.W.; Costa, F.O. Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: A systematic review. Clin Implant Dent Relat Res. 2018, 1, 26–33. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Di Pietro, N.; Romasco, T.; Montesani, L.; Piattelli, A.; Covani, U. Are Implant Threads Important for Implant Stability? An In Vitro Study Using Low-Density Polyurethane Sheets. Eng 2023, 4, 1167–1178. [Google Scholar] [CrossRef]
- ASTM F1839; Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. American Society for Testing and Materials; ASTM: West Conshohocken, PA, USA, 2008. [Google Scholar]
Figure 1.
Representative images of the implants used in the present study: (a) INTRALOCK, (b) TAC, and (c) CYROTH implants from the bottom (first line), lateral (second line), and top (third line) views.
Figure 1.
Representative images of the implants used in the present study: (a) INTRALOCK, (b) TAC, and (c) CYROTH implants from the bottom (first line), lateral (second line), and top (third line) views.
Figure 2.
An example of the insertion of INTRALOCK (on the left) and TAC (on the right) implants up to 2 mm below the polyurethane profile and at 15-20 degrees of inclination.
Figure 2.
An example of the insertion of INTRALOCK (on the left) and TAC (on the right) implants up to 2 mm below the polyurethane profile and at 15-20 degrees of inclination.
Figure 3.
Representative images of the implant site preparation, implant insertion, and measurements: (a) Implant site preparation with 15-20 degrees of inclination; (b) Implant insertion; (c-d) Resonance Frequency Analysis (RFA) measurements.
Figure 3.
Representative images of the implant site preparation, implant insertion, and measurements: (a) Implant site preparation with 15-20 degrees of inclination; (b) Implant insertion; (c-d) Resonance Frequency Analysis (RFA) measurements.
Figure 4.
Representative images of the different blocks used: (a-b) polyurethane blocks of 20 and 10 Pounds per Cubic Foot (PCF) in density without and with the cortical sheets; (c) a detail of 20 and 10 PCF polyurethane blocks and the cortical sheets.
Figure 4.
Representative images of the different blocks used: (a-b) polyurethane blocks of 20 and 10 Pounds per Cubic Foot (PCF) in density without and with the cortical sheets; (c) a detail of 20 and 10 PCF polyurethane blocks and the cortical sheets.
Figure 5.
Schematic illustration of the osteotomies performed and the study design.
Figure 5.
Schematic illustration of the osteotomies performed and the study design.
Figure 6.
Bar graphs related to the distribution of Insertion Torque (IT) values expressed by each implant type in the different artificial bone conditions. Data were expressed as means ± Standard Deviation (SD). (*p<0.05, ***p<0.001, ****p<0.0001).
Figure 6.
Bar graphs related to the distribution of Insertion Torque (IT) values expressed by each implant type in the different artificial bone conditions. Data were expressed as means ± Standard Deviation (SD). (*p<0.05, ***p<0.001, ****p<0.0001).
Figure 7.
Bar graphs related to the distribution of Removal Torque (RT) values expressed by all the implant types in different artificial bone conditions. Data are expressed as means ± SD. (*** p < 0.001, **** p < 0.0001).
Figure 7.
Bar graphs related to the distribution of Removal Torque (RT) values expressed by all the implant types in different artificial bone conditions. Data are expressed as means ± SD. (*** p < 0.001, **** p < 0.0001).
Figure 8.
Bar graphs related to the distribution of RFA values in the Bucco-Lingual (BL, on the left) and Mesial-Distal (MD, on the right) orientations expressed by each implant type in the different artificial bone conditions. Data are expressed as means ± SD. (****p<0.0001).
Figure 8.
Bar graphs related to the distribution of RFA values in the Bucco-Lingual (BL, on the left) and Mesial-Distal (MD, on the right) orientations expressed by each implant type in the different artificial bone conditions. Data are expressed as means ± SD. (****p<0.0001).
Table 1.
Statistic values of the Insertion Torque (IT), Removal Torque (RT), and Resonance Frequency Analysis in the Bucco-Lingual (RFA-BL) and Mesial-Distal (RFA-MD) orientations, related to the different experimental conditions tested for each type of implant (TAC, INTRALOCK, and CYROTH). SD: Standard Deviation.
Table 1.
Statistic values of the Insertion Torque (IT), Removal Torque (RT), and Resonance Frequency Analysis in the Bucco-Lingual (RFA-BL) and Mesial-Distal (RFA-MD) orientations, related to the different experimental conditions tested for each type of implant (TAC, INTRALOCK, and CYROTH). SD: Standard Deviation.
| IT |
10 PCF |
20 PCF |
| |
NO CORTICAL |
CORTICAL |
NO CORTICAL |
CORTICAL |
| |
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
| Min |
5.90 |
6.90 |
6.50 |
|
14.70 |
15.70 |
16.60 |
|
24.50 |
22.50 |
24.50 |
|
23.50 |
28.40 |
25.50 |
|
| Max |
6.90 |
7.80 |
6.90 |
|
15.70 |
16.70 |
17.60 |
|
25.50 |
24.50 |
27.40 |
|
25.50 |
37.20 |
28.40 |
|
| Mean |
6.39 |
7.44 |
6.73 |
|
15.16 |
16.23 |
17.06 |
|
24.93 |
23.83 |
26.42 |
|
24.63 |
32.44 |
26.87 |
|
| SD (±) |
0.41 |
0.34 |
0.16 |
|
0.30 |
0.36 |
0.30 |
|
0.34 |
0.59 |
0.96 |
|
0.72 |
3.28 |
1.04 |
|
| RT |
10 PCF |
20 PCF |
| |
NO CORTICAL |
CORTICAL |
NO CORTICAL |
CORTICAL |
| |
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
| Min |
4.70 |
4.90 |
4.80 |
|
12.70 |
10.00 |
12.00 |
|
16.60 |
16.90 |
18.60 |
|
20.50 |
21.50 |
19.70 |
|
| Max |
4.90 |
4.90 |
5.10 |
|
13.70 |
11.00 |
13.00 |
|
18.60 |
18.60 |
21.50 |
|
22.50 |
23.50 |
22.50 |
|
| Mean |
4.81 |
4.90 |
4.95 |
|
13.20 |
10.72 |
12.40 |
|
17.70 |
17.94 |
20.33 |
|
21.60 |
22.41 |
21.15 |
|
| SD (±) |
0.10 |
0.00 |
0.08 |
|
0.31 |
0.36 |
0.34 |
|
0.63 |
0.57 |
0.98 |
|
0.75 |
0.72 |
1.14 |
|
| RFA - BL |
10 PCF |
20 PCF |
| |
NO CORTICAL |
CORTICAL |
NO CORTICAL |
CORTICAL |
| |
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
| Min |
50.00 |
35.00 |
44.00 |
|
60.00 |
55.00 |
56.00 |
|
62.00 |
53.00 |
61.00 |
|
61.00 |
52.00 |
62.00 |
|
| Max |
52.00 |
38.00 |
46.00 |
|
61.00 |
56.00 |
57.00 |
|
63.00 |
55.00 |
63.00 |
|
62.00 |
55.00 |
64.00 |
|
| Mean |
51.00 |
36.80 |
45.40 |
|
60.20 |
55.50 |
56.40 |
|
62.30 |
54.20 |
62.20 |
|
61.50 |
53.30 |
62.60 |
|
| SD (±) |
0.82 |
1.23 |
0.70 |
|
0.42 |
0.53 |
0.52 |
|
0.48 |
0.92 |
0.63 |
|
0.53 |
0.95 |
0.84 |
|
| RFA - MD |
10 PCF |
20 PCF |
| |
NO CORTICAL |
CORTICAL |
NO CORTICAL |
CORTICAL |
| |
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
TAC |
INTRALOCK |
CYROTH |
|
| Min |
50.00 |
35.00 |
44.00 |
|
60.00 |
55.00 |
56.00 |
|
62.00 |
53.00 |
61.00 |
|
61.00 |
52.00 |
62.00 |
|
| Max |
52.00 |
38.00 |
46.00 |
|
61.00 |
57.00 |
57.00 |
|
63.00 |
55.00 |
63.00 |
|
62.00 |
58.00 |
64.00 |
|
| Mean |
51.20 |
37.00 |
45.30 |
|
60.40 |
56.00 |
56.50 |
|
62.20 |
54.40 |
62.10 |
|
61.50 |
54.30 |
62.90 |
|
| SD (±) |
0.92 |
1.25 |
0.82 |
|
0.52 |
0.82 |
0.53 |
|
0.42 |
0.70 |
0.74 |
|
0.53 |
2.21 |
0.74 |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).