1. Introduction
Since the 1990s, late potentials (LPs) detected using signal-averaged electrocardiography (SAECG) have been reported to be useful for predicting sudden cardiac death (SCD) and fatal arrhythmic events in patients with post-myocardial infarction (MI) status [
1,
2], dilated cardiomyopathy [
3], arrhythmogenic right ventricular cardiomyopathy [
4], cardiac sarcoidosis [
5], and other organic heart diseases.
Recently, Holter electrocardiography (ECG) has also been used to measure LPs [
6], and reports have emerged on the usefulness of Holter-based LPs for predicting SCD/lethal arrhythmia in patients with organic heart disease and chronic kidney disease [
7,
8,
9]. Holter-based LP measurement is expected to become a mainstream test because it is performed simultaneously with routine Holter ECG, saving time for both patients and medical professionals compared to the conventional real-time LP measurement method. However, Holter-based LPs exhibit diurnal variation in post-MI patients [
8], patients with Brugada syndrome [
10,
11], and healthy participants [
12]. Given that 24 consecutive hours of LP data are obtained from Holter electrocardiographs, it is important to determine which method of LP data collection is most useful for stratifying patients by SCD/lethal arrhythmia risk. In previous studies, LP parameters such as filtered QRS duration (fQRS) and root mean square voltage of the terminal 40 ms in the filtered QRS complex (RMS40) captured at the time of the most abnormal or worst (lowest) RMS40 in 24 h [
8,
9,
13] or the most abnormal or worst (highest) fQRS in 24 h [
14] were used as representative Holter-based LP values. However, the timing of collecting SAECG testing data yielding LP parameters most useful for predicting lethal arrhythmias under ordinary daily conditions has not been completely validated. Moreover, factors influencing diurnal variation of LP parameters are not completely understood in patients with post-MI status.
Therefore, this study aimed to identify the optimal timing for LP testing for stratifying risk of post-MI patients and to investigate factors influencing LP diurnal variation in post-MI patients and control participants.
2. Materials and Methods
2.1. Study Design and Ethics
In this retrospective cohort study, we initially enrolled 150 patients with post-MI status and 66 control participants, all of whom underwent high-resolution Holter electrocardiography (H-ECG) from March 2012 to December 2022 (
Figure S1). Among the 150 patients with post-MI status, 33 had clinically sustained ventricular tachycardia (VT) as of March 2021 and were assigned to the MI-VT group, while 117 did not have sustained VT and were assigned to the MI-non-VT group; sustained VT was defined as ≥30 s of consecutive ventricular complexes at a rate of >100 bpm. The control group included 66 participants who underwent outpatient H-ECG for close examination of chest symptoms and ultimately showed no sign of cardiac disease.
The exclusion criteria were as follows: 1) cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy, 2) persistent atrial fibrillation or flutter, 3) right or left bundle branch block and intraventricular conduction delay, 4) permanent pacing with pacemaker or implantable cardioverter defibrillator, 5) atrioventricular block Ⅱ–Ⅲ degree, and 6) channelopathies such as long QT syndrome, Brugada syndrome, and early repolarization syndrome; 24 patients were excluded for these reasons. Finally, 126 patients with post-MI status (MI-VT group, n=23; MI-non-VT group, n=103) and 60 control participants were included in the study (
Figure S1,
Table 1).
The study protocol conformed to the Declaration of Helsinki and was approved by the Medical Ethics Committee of the National Defense Medical College Hospital (approval no. 4692), Saitama, Japan, and the Nihon University School of Medicine, Itabashi Hospital, Tokyo, Japan (approval no. MF-2302-0063). Written informed consent was obtained from all patients.
2.2. Ambulatory ECG Recordings
Patients underwent H-ECG recording during ordinary daily activities at least 3 weeks after MI onset to avoid acute phase electrical instability. Data obtained from the H-ECG system (SpiderView; ELA Medical, Paris, France) were analyzed for routine arrhythmic events. The length of the H-ECG recording conducted for each patient was 24 h.
2.3. Measurement of Holter-based LPs
LPs were recorded for all patients and control participants using the H-ECG system. ECG data were obtained at a sampling rate of 1000 Hz using 16-bit A/D conversion. For LP measurement, ECG data were filtered and ranged from 40 to 250 Hz. Then, the LP signals of 250 complexes were averaged (default setting). Orthogonal X, Y, and Z bipolar leads with silver-silver chloride electrodes (Blue SENSOR®; METS, Tokyo, Japan) were used for all LP recordings. LP parameters were automatically measured by the software during the 24-h time period; parameters assessments were manually edited by expert electrophysiological investigators using Syne Scope (SORIN GROUP, Milano, Italy). The expert electrophysiological investigators were blinded to patient outcomes. LP parameters were assessed independently by two expert electrophysiological investigators, and disagreements were resolved by consensus.
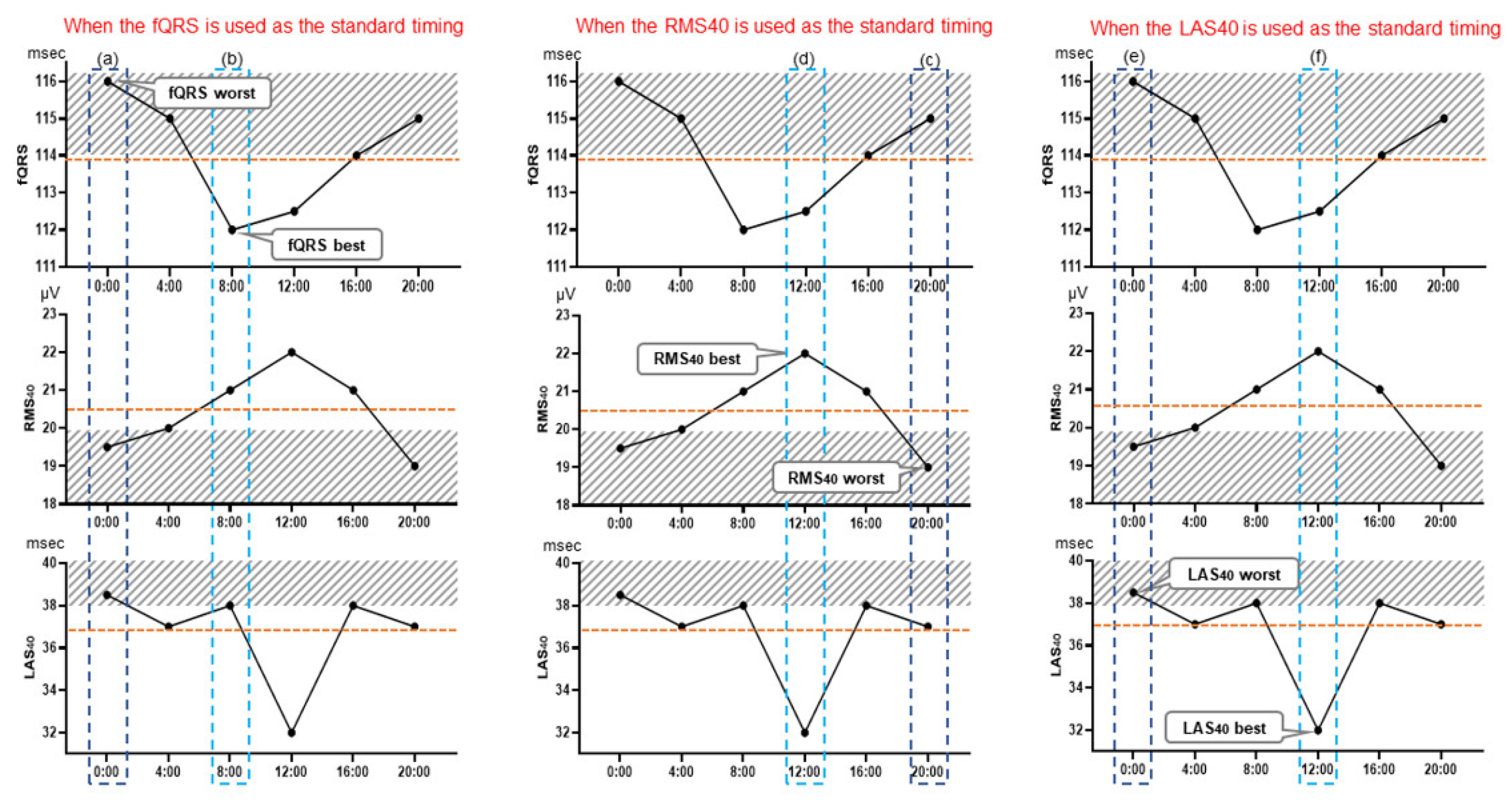
Three LP parameters were evaluated in the 24-h records of the MI-VT, MI-non-VT, and control groups: filtered QRS duration (fQRS) (ms), root mean square voltage of the terminal 40 ms in the filtered QRS complex (RMS40) (µV), and duration of low-amplitude signals <40 μV in the filtered QRS complex terminus (LAS40) (ms). We evaluated each of the LP parameters every 4 h at 6 time points: 0:00, 4:00, 8:00, 12:00, 16:00, and 20:00. To adjust the LP signal for noise level, a Holter-based LP measured at 0.8 µV or less was used; however, if no part of the LP measurement had a noise level below 0.8 µV, the LP parameters were measured over a wider range of up to 2 h before and after the time period to find such a portion, and noise reduction was performed. Then, the signals at times corresponding to the (a) fQRS worst, (b) fQRS best, (c) RMS40 worst, (d) RMS40 best, (e) LAS40 worst, and (f) LAS40 best values relative to the presence of LPs and (g) the 24-h mean values of each of the three LP parameters were selected for evaluation. The averaged signal obtained at each selected time was judged to be positive or negative for the presence of LPs (
Figure 1). LPs were considered to be present when any two of the following three criteria were met: fQRS >114 ms, RMS40 <20 μV, and LAS40>38 ms [
15]. Furthermore, the periodical times (0:00, 4:00, 8:00, 12:00, 16:00 and 20:00) were evaluated as representative times for assessing the presence or absence of LPs. The LP parameters of the signals at these times were judged as LP positive or negative. The body position at the time of LP measurement was estimated manually from the behavior record card.
2.4. Heart Rate Variability Analysis
Heart rate (HR) variability (HRV) analysis was also performed to evaluate autonomic nervous activity using the SpiderView (Ela, Paris, France) at the same time when Holter-based LPs were measured. HRV time- and frequency-domain analyses were conducted at 5-min intervals. For frequency-domain analysis, the RR interval was calculated using fast Fourier transformation. Time-domain analysis included the percent difference between adjacent normal NN intervals greater than 50 ms (PNN50), root mean squared successive differences of NN intervals (RMSSD), mean of 5-min standard deviations of NN intervals (ASDNN) (ms), and standard deviation of the average NN interval for each 5-min segment (SDANN) (ms). For frequency-domain analysis, the power in the low-frequency area (LF), power in the high-frequency area (HF), and power in the low-frequency area/power in the high-frequency area (LF/HF) ratio were also analyzed every 5 min. The power spectra of frequency-domain analysis were defined as follows: total power (TP), <0.4 Hz; power in the very low-frequency range (VLF), 0.0033–0.04 Hz; power in the low-frequency range (LF), 0.04–0.15 Hz; and power in the HF, 0.15–0.40 Hz. Based on a previously published report [
16], LF normalized unit (LFnu) and HF normalized unit (HFnu) were calculated using the following formulas: LFnu = [LF/(TP-VLF)] × 100 and HFnu = [HF/(TP-VLF)] × 100. HRV parameters were evaluated simultaneously with LP parameters whenever the signal had an acceptable noise level of <0.8 µV.
2.5. Statistical Analyses
Data are presented as means±standard deviations for normally distributed continuous variables and as medians (interquartile range: 25th–75th percentile) for non-normally distributed variables. Patient characteristics were compared using the χ2 test for categorical variables, Student’s t-test for continuous and parametric data, and Mann–Whitney U test for nonparametric data. The distribution of continuous variables was evaluated for normality by the Shapiro–Wilk test. Friedman’s analysis of variance (ANOVA) on rank was used to compare LP parameters (fQRS, RMS40, and LAS40) for each LP measurement time. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated using standard formulas. A receiver operating characteristic (ROC) curve was generated, and the area under the curve (AUC) was calculated to determine the LP measurement timing that best predicted VT. Logistic regression analysis was performed to correlate the occurrence of VT with each time of LP measurement (when fQRS, RMS40, andLAS40 were worst; when they were best; and at 0:00, 4:00, 8:00, 12:00, 16:00, and 20:00). Cochran’s Q test was performed to compare LP positivity rates at each time point (0:00, 4:00, 8:00, 12:00, 16:00, and 20:00). Multivariate regression analysis was performed to determine the intensity of diurnal variation of LP parameters and to theoretically consider important factors such as the HR and HRV indices. Because HRV indices (PNN50, RMSSD, ASDNN, SDANN, PNN50, LFnu, VLF, HFnu, and LF/HF) showed skewed distributions, they were natural log-transformed before multiple regression analysis to explore factors influencing the diurnal variation of Holter-based LPs was performed.
Sample size calculation was performed based on the correlation among six repeated measures ANOVA using the R (4.2.3.2 Ver.) (R Foundation for Statistical Computing, Vienna, Austria), a two-tailed hypothesis, an effect size of 0.40, an α error probability of 0.05 with a β level of 10%, between-group variance=5, within-group variance=30, and the desired power analysis of 90% (1-β error probability). This calculation showed that a total sample size of at least 20 participants with sustained ventricular tachycardia (SVT) was required to achieve the desired power. Consequently, a total of 150 patients with MI were included (120 MI-non-SVT participants) to enroll consecutive cases with at least 20 SVT. Ultimately, a total of 126 patients with MI were included based on the inclusion criteria (MI-VT, n=23; MI-non-VT, n=103). All statistical analyses, except for the sample size analysis, were performed using SPSS version 28 (IBM Corp., Armonk, NY, USA). T-tests were two-sided, and p values of <0.05 were considered statistically significant.
3. Results
3.1. Patient Demographics
The demographic data, including age, sex, comorbidities, echocardiographic data, renal function parameters, and medication therapy, were extracted from the electronic medical records of the patients.
Table 1 shows the characteristics of patients and control participants included in the study. The number of patients with diabetes mellitus, culprit coronary lesions of the left atrial descending artery, left ventricular end-diastolic diameter, and amiodarone use post-MI were significantly higher in the MI-VT group than in the MI-non-VT group. Consequently, LVEF was significantly lower in the MI-VT group than in the MI-non-VT group.
3.2. Optimal Measurement Timing for Assessment of Holter-based LPs
In the MI-VT, MI-non-VT, and control groups, Holter-based LPs showed significant diurnal variation for all three parameters (fQRS, RMS40, and LAS40) (
Table 2). In all groups, LPs deteriorated during the nighttime (20:00–8:00) and improved during the daytime (8:00–20:00) (
Table 2). LP-positivity rates of the three groups (MI-VT, MI-non-VT, and control groups) were significantly higher at night and lower during the daytime (p=0.002–0.009) (
Table 3).
Table 4 shows the predictive values associated with Holter-based LPs for each parameter and time point. For each LP parameter, the NPV was not different among the LP parameters (85–89%). However, the PPV in the fQRS worst (61%), RMS40 worst (61%), and LAS40 worst (65%) tended to be better than the other PPVs of LP parameters (43–48%). for each time setting (
Table 4, right). Although the NPV at 16:00 was the lowest, the PPV at 0:00, 4:00, 16:00, and 20:00 (57–61%) tended to be better than that during the daytime (8:00, 12:00) (43–52%).
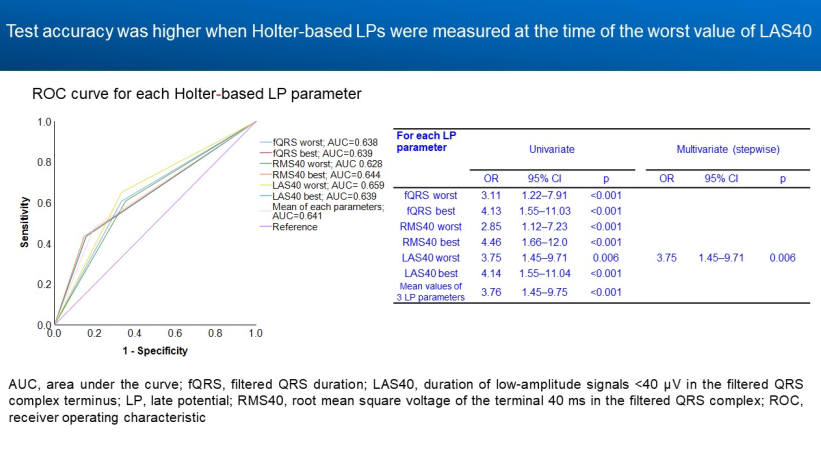
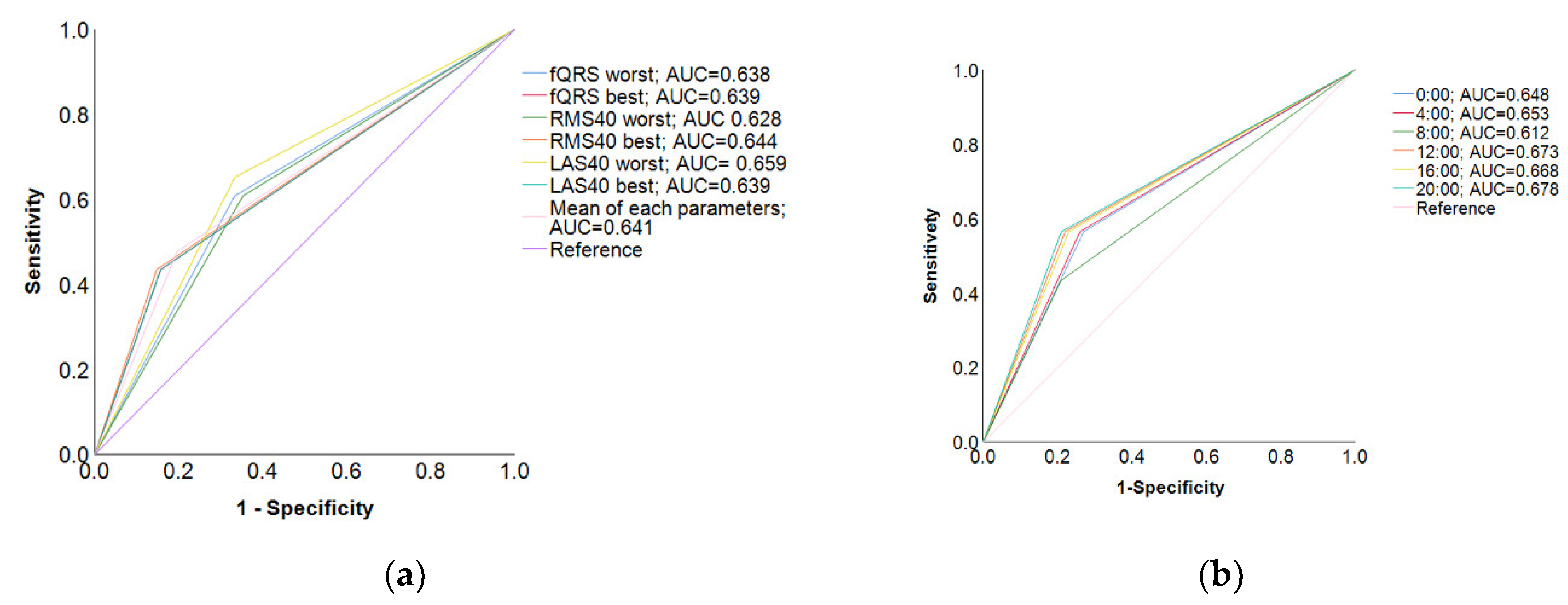
In the ROC curve for each LP parameter, when the timing of the worst LAS40 reading was selected as the standard, the AUC was higher (0.659) and the test accuracy was the highest (
Figure 2a). However, in the ROC curve for each time period (0:00, 4:00, 8:00, 12:00, 16:00, and 20:00), when 20:00 was selected as the standard for LP measurement timing, the AUC was the highest (AUC=0.678) and the SAECG test was highly accurate (
Figure 2b). In the logistic multivariate regression analysis, the highest odds ratio was observed when LAS40 worst timing was used as the standard (odds ratio=3.75, 95% confidence interval [CI]=1.45–9.71, p=0.006) (
Table 5. In each LP parameter). In contrast, the highest odds ratio was observed when 20:00 was selected as the standard for LP measurement timing (odds ratio=4.89, 95% CI=1.88-12.7, p=0.006) (
Table 5. In each time zone).
3.3. Factors Influencing Diurnal Variability in Holter-based LP
In the multiple regression analysis, HR was the factor most influencing diurnal variation of LP parameters in the MI-VT group (fQRS, β=0.180, p=0.037; RMS40, β=0.305, p=0.003; LAS40, β=-0.261, p=0.011) (
Table 6 (a). MI-VT group). In the MI-non-VT group, LP parameters were significantly influenced by noise or parasympathetic nervous activity parameters of HRV, such as logPNN50 or logLF/HF, which are considered a balance of sympathetic, nervous, and parasympathetic nervous activities (
Table 6 (b). MI-non-VT group). These results suggest the involvement of the autonomic nervous system in both the MI-VT and MI-non-VT groups. In addition, logVLF and logASDNN were significant factors in the MI-non-VT group. In contrast, in the control group, diurnal variability of LP parameters was significantly influenced by noise or HR (
Table 6 (c). Control group).
Table 6.
(a). Factors influencing diurnal variation in LP parameters (MI-VT group).
Table 6.
(a). Factors influencing diurnal variation in LP parameters (MI-VT group).
| fQRS |
R=0.490 |
|
R=0.448a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
0.031 |
0.770 |
1.527 |
|
|
|
|
| log Noise (μV) |
0.081 |
0.484 |
1.812 |
|
|
|
|
| log HR (bpm) |
-0.188 |
0.085 |
1.599 |
|
-0.180 |
0.037 |
1.016 |
| log PNN50 (%) |
0.256 |
0.270 |
7.296 |
|
0.433 |
<0.001 |
1.016 |
| log RMSSD (ms) |
0.212 |
0.417 |
9.246 |
|
|
|
|
| log ASDNN (ms) |
-0.180 |
0.382 |
5.771 |
|
|
|
|
| log SDANN (ms) |
-0.021 |
0.832 |
1.325 |
|
|
|
|
| log VLF (ms2) |
0.187 |
0207 |
2.977 |
|
|
|
|
| log HFnu (TP) |
0.183 |
0.140 |
2.070 |
|
|
|
|
| log LF/HF |
0.086 |
0.400 |
1.399 |
|
|
|
|
| RMS40 |
R=0.500 |
|
R=0.305a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
-0.092 |
0.417 |
1.397 |
|
|
|
|
| log Noise (μV) |
-0.018 |
0.881 |
1.550 |
|
|
|
|
| log HR (bpm) |
0.422 |
0.000 |
1.441 |
|
0.305 |
0.003 |
1.000 |
| log PNN50 (%) |
-0.230 |
0.336 |
6.211 |
|
|
|
|
| log RMSSD (ms) |
-0.066 |
0.790 |
6.619 |
|
|
|
|
| log ASDNN (ms) |
0.180 |
0.415 |
5.264 |
|
|
|
|
| log SDANN (ms) |
0.077 |
0.509 |
1.483 |
|
|
|
|
| log VLF (ms2) |
0.076 |
0.648 |
2.971 |
|
|
|
|
| log HFnu (TP) |
0.796 |
0.002 |
7.084 |
|
|
|
|
| log LF/HF |
0.733 |
0.007 |
7.566 |
|
|
|
|
| LAS40 |
R=0.392 |
|
R=0.292a |
| β |
*p |
VIF |
|
β |
p |
VIF |
| body position |
0.013 |
0.916 |
1.492 |
|
|
|
|
| log Noise (μV) |
-0.010 |
0.942 |
1.788 |
|
|
|
|
| log HR (bpm) |
-0.330 |
0.010 |
1.524 |
|
-0.261 |
0.011 |
1.000 |
| log PNN50 (%) |
0.081 |
0.749 |
6.233 |
|
|
|
|
| log RMSSD (ms) |
0.148 |
0.568 |
6.483 |
|
|
|
|
| log ASDNN (ms) |
-0.032 |
0.890 |
5.196 |
|
|
|
|
| log SDANN (ms) |
-0.008 |
0.950 |
1.475 |
|
|
|
|
| log VLF (ms2) |
-0.134 |
0.448 |
2.970 |
|
|
|
|
| log HFnu (TP) |
-0.525 |
0.057 |
7.175 |
|
|
|
|
| log LF/HF |
-0.402 |
0.154 |
7.582 |
|
|
|
|
Table 6.
(b). Factors influencing diurnal variation in LP parameters (MI-non-VT group).
Table 6.
(b). Factors influencing diurnal variation in LP parameters (MI-non-VT group).
| fQRS |
R=0.366 |
|
R=0.353a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
-0.054 |
0.348 |
1.287 |
|
|
|
|
| log Noise (μV) |
-0.036 |
0.529 |
1.308 |
|
|
|
|
| log HR (bpm) |
-0.021 |
0.725 |
1.436 |
|
|
|
|
| log PNN50 (%) |
0.305 |
0.001 |
3.092 |
|
0.298 |
0.001 |
2.945 |
| log ASDNN (ms) |
-0.235 |
0.028 |
4.480 |
|
-0.222 |
0.029 |
4.047 |
| log SDANN (ms) |
0.005 |
0.934 |
1.406 |
|
|
|
|
| log VLF (ms2) |
-0.184 |
0.037 |
3.027 |
|
-0.180 |
0.030 |
2.684 |
| log HFnu (TP) |
-0.038 |
0.692 |
3.680 |
|
|
|
|
| log LF/HF |
0.190 |
0.071 |
4.291 |
|
0.209 |
0.002 |
1.822 |
| RMS40 |
R=0.367 |
|
R=0.327a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
-0.039 |
0.493 |
1.287 |
|
|
|
|
| log Noise (μV) |
0.155 |
0.007 |
1.308 |
|
0.156 |
0.002 |
1.000 |
| log HR (bpm) |
0.046 |
0.446 |
1.436 |
|
|
|
|
| log PNN50 (%) |
-0.241 |
0.007 |
3.092 |
|
-0.208 |
0.003 |
1.903 |
| log ASDNN (ms) |
0.136 |
0.203 |
4.480 |
|
0.206 |
0.003 |
1.902 |
| log SDANN (ms) |
0.075 |
0.209 |
1.406 |
|
|
|
|
| log VLF (ms2) |
0.119 |
0.175 |
3.027 |
|
|
|
|
| log HFnu (TP) |
-0.027 |
0.777 |
3.680 |
|
|
|
|
| log LF/HF |
-0.157 |
0.134 |
4.291 |
|
|
|
|
| LAS40 |
R=0.344 |
|
R=0.314a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
0.029 |
0.617 |
1.287 |
|
|
|
|
| log Noise (μV) |
-0.119 |
0.041 |
1.308 |
|
-0.122 |
0.017 |
1.000 |
| log HR (bpm) |
-0.008 |
0.890 |
1.436 |
|
|
|
|
| log PNN50 (%) |
0.265 |
0.003 |
3.092 |
|
0.219 |
0.002 |
1.903 |
| log ASDNN (ms) |
-0.221 |
0.041 |
4.480 |
|
-0.224 |
0.001 |
1.902 |
| log SDANN (ms) |
-0.086 |
0.154 |
1.406 |
|
|
|
|
| log VLF (ms2) |
-0.008 |
0.929 |
3.027 |
|
|
|
|
| log HFnu (TP) |
0.070 |
0.472 |
3.680 |
|
|
|
|
| log LF/HF |
0.155 |
0.142 |
4.291 |
|
|
|
|
Table 6.
(c). Factors influencing diurnal variation in LP parameters (control group).
Table 6.
(c). Factors influencing diurnal variation in LP parameters (control group).
| fQRS |
R=0.458 |
|
R=0.452a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
-0.035 |
0.556 |
1.352 |
|
|
|
|
| log Noise (μV) |
-0.473 |
<0.001 |
1.271 |
|
-0.484 |
<0.001 |
1.179 |
| log HR (bpm) |
0.139 |
0.050 |
1.948 |
|
0.141 |
0.022 |
1.473 |
| log PNN50 (%) |
-0.048 |
0.631 |
3.860 |
|
|
|
|
| log ASDNN (ms) |
0.118 |
0.332 |
5.753 |
|
|
|
|
| log SDANN (ms) |
-0.024 |
0.705 |
1.530 |
|
|
|
|
| log VLF (ms2) |
-0.105 |
0.298 |
3.985 |
|
|
|
|
| log HFnu (TP) |
-0.150 |
0.319 |
8.789 |
|
-0.129 |
0.028 |
1.356 |
| log LF/HF |
0.004 |
0.982 |
9.626 |
|
|
|
|
| RMS40 |
R=0.396 |
|
R=0.356a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
0.112 |
0.078 |
1.385 |
|
|
|
|
| log Noise (μV) |
0.138 |
0.042 |
1.588 |
|
0.147 |
0.008 |
1.049 |
| log HR (bpm) |
-0.081 |
0.265 |
1.840 |
|
|
|
|
| log PNN50 (%) |
0.123 |
0.249 |
3.925 |
|
0.094 |
0.089 |
1.049 |
| log ASDNN (ms) |
-0.013 |
0.911 |
4.489 |
|
|
|
|
| log SDANN (ms) |
0.035 |
0.552 |
1.227 |
|
|
|
|
| log VLF (ms2) |
-0.075 |
0.407 |
2.837 |
|
|
|
|
| log HFnu (TP) |
-0.027 |
0.768 |
2.795 |
|
|
|
|
| log LF/HF |
0.001 |
0.987 |
1.523 |
|
|
|
|
| LAS40 |
R=0.575 |
|
R=0.563a |
| β |
p |
VIF |
|
β |
p |
VIF |
| body position |
0.032 |
0.558 |
1.352 |
|
|
|
|
| log Noise (μV) |
-0.633 |
<0.001 |
1.271 |
|
-0.609 |
<0.001 |
1.169 |
| log HR (bpm) |
0.240 |
<0.001 |
1.948 |
|
0.245 |
<0.001 |
1.169 |
| log PNN50 (%) |
0.100 |
0.278 |
3.860 |
|
|
|
|
| log ASDNN (ms) |
-0.008 |
0.946 |
5.753 |
|
|
|
|
| log SDANN (ms) |
0.035 |
0.548 |
1.530 |
|
|
|
|
| log VLF (ms2) |
-0.026 |
0.781 |
3.985 |
|
|
|
|
| log HFnu (TP) |
0.051 |
0.715 |
8.789 |
|
|
|
|
| log LF/HF |
0.152 |
0.295 |
9.626 |
|
|
|
|
4. Discussion
When the time of the worst LAS40 reading or nighttime (20:00) was used as the standard time of LP measurement over 24 h, the odds ratio for VT and the accuracy of the SAECG test were higher than for other Holter-based LP measurement times. The times of the worst fQRS and RMS40 readings were also candidates for the standard test times, although they were inferior in terms of odds ratio but not in terms of sensitivity, specificity, NPV, and PPV. Regarding factors influencing diurnal variation of LP parameters, multiple regression analysis revealed HR to be the factor that influenced diurnal variation of LP parameters in the MI-VT group the most. In the MI-non-VT group, LP parameters were significantly influenced by noise and by HRV markers of parasympathetic nervous activity such as logPNN50 and logLF/HF. In the control group, LP parameters were significantly influenced by noise and HR.
4.1. Optimal Measurement Timing of LP for Predicting VT
Amino et al. [
14] reported the usefulness of Holter-based LP assessment as a predictor of rehospitalization in patients with post-MI status. They reported that a positive LP at the time of the worst fQRS value was significantly predictive of rehospitalization. In contrast, in the multicenter collaborative study (Janan Noninvasive Risk Stratification [JANIES] study [
8], when a comparison was made between the predictive value of the readings at the times of the RMS40 worst and best levels, it was concluded that the LP’s measured at the time of the worst RMS40 was more useful, with a higher risk hazard of 8.2 (p=0.003) for fatal arrhythmias in patients with MI. Our study compared the usefulness of all possible patterns for the first time. In direct terms, we compared the usefulness of readings at the times of the worst and best values of fQRS, RMS40, and LAS40, and of all mean values (
Figure 1).
There have also been no comparative studies of optimal LP measurements according to the time of day. In general, the times of the worst fQRS, RMS40, and LAS40 readings often coincided; however, this was not always the case. The determination that the optimal timing for Holter-based LP measurement was when LAS40 was at its worst point was a novel finding. Although LP is an automatic measurement for some electrocardiography models, others require manual editing for Holter-based LP measurements,. in which case fQRS and RMS40 measurements can be influenced by the manual editing of onset and offset settings at the time of LP measurement, and this may cause bias among examiners. However, LAS40 assessment was not affected by manual editing of onset or offset settings. Therefore, using LAS40 to measure LP could help avoid bias among examiners.
4.2. Diurnal Variation of LP and Factors Influencing LP Values
It has been reported that LP varies diurnally in patients with MI [
8,
17,
18] and healthy participants [
12]. In both MI and healthy patients, the late potentials worsened at night and improved during the daytime. An important finding in our study is that each LP parameter in the MI-VT group showed diurnal variation around the cutoff values of the SAECG diagnostic criteria [
16] (i.e., the mean values of fQRS, RMS40 and LAS40 were near 114 ms, 20 μV, and 38 ms, respectively) (
Table 2). Therefore, it is key to consider diurnal variation as it relates to positive/negative LP determination. Factors reported to influence diurnal variation include HR [
19], autonomic nervous system activity [
20], body position [
21], and physical activity [
17,
22]. Goldberger et al. [
20] studied the effects of tilt, epinephrine, isoproterenol, beta-blockers, beta-blockers +atropine, and phenylephrine on LP in 14 healthy participants. The results showed that LP parameters improved with tilt-up and isoproterenol and worsened with epinephrine. Atrial pacing and atropine did not significantly change the LP parameters compared with those observed in healthy participants. In these results, the response to tilt is of interest. The results are consistent with our findings, suggesting that endogenous sympathetic tone and decreased parasympathetic activity may contribute to changes in LP parameters throughout the day. LPs were also influenced by HR, especially in the MI-VT and control groups after 24 h. Among LP parameters, fQRS and LAS40 are considered to be more influenced by HR than by RMS40 because bradycardia directly prolongs fQRS and LAS40. Yoshioka et al. [
21] examined patients with Brugada syndrome and healthy participants and reported that LP parameters were influenced by body position. In our results, body position was not a significant influential parameter for LP parameters in any of the groups in the multivariate analysis (
Table 6). However, this is the first demonstration of diurnal variations of LP parameters, including related to body position. Our results indicate that body position was not a significant factor influencing LP parameter values compared with autonomic activity, HR, or noise level in natural daily activities. Further investigations are required for other cardiac diseases.
4.3. Clinical Implications
Holter-based LP analysis requires the extraction of useful data from a large dataset. Therefore, its use to predict risk requires manpower and imposes a large time burden on cardiologists and technicians. Therefore, artificial intelligence (AI) support will be essential for future applications.
Recently, with AI technology advances, the accuracy of ECG analysis at the μV level has improved [
23]. Based on data from the present study, it is possible to develop AI-supported clinical practices. We believe that this will lead to the widespread use of Holter-based LP assessment.
4.4. Limitations
This study had some limitations. First, the H-ECG recorder used (SpiderViewⓇ) did not have an accelerometer. Although consistency of body position was confirmed to some extent using the activity record card, this assessment was not precise, and information on body position in this study may not necessarily be accurate. Second, the study results only provide data for risk stratification of fatal arrhythmias in patients with post-MI status. Therefore, it should be applied clinically with caution as it may not be indicated in other cardiac diseases such as Brugada syndrome, ARVC, dilated cardiomyopathy, or heart failure.
5. Conclusions
In the Holter-based LP measurement, when the time of the LAS40 worst value or nighttime (20:00) was used as the standard value for predicting VT, both the odds ratio and accuracy of the SAECG test were the highest in patients with MI. In contrast, time points taken when the fQRS and RMS40 were at their worst were also candidates as LP measurement time points. The involvement of the autonomic nervous system, including the HR or noise level, has been suggested as a factor influencing patients with post-MI status and healthy control participants.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Figure S1: Study population.
Author Contributions
Conceptualization, K.H., N.H. and Y.Ka. (Yuji Kasamaki); methodology, K.H., N.H. and Y.Kaw. (Yusuke Kawamura); software, K.H., N.H.; validation, K.H., N.H.; formal analysis, K.H., N.H.; investigation, K.H., N.H; resources, K.H.; data curation, K.H., N.H.; writing—original draft preparation, K.H.; writing—review and editing, K.H. N.H., M.K., Y.Kaw., N.F., A.S., Y.On. (Yosuke Ono), Y.Ob.(Yasuhiro Obuchi), TT, Y.Ka., Y.T.; Supervision, Y.Ka., Y.T; Project administration; Y.T.; Funding acquisition, K.H. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by a Grant-in-Aid for Scientific Research in Japan (JSPS KAKENHI) [Grant Number 20K07816] provided by the Japanese Society for the Promotion of Science.
Institutional Review Board Statement
The study protocol conformed to the Declaration of Helsinki and was approved by the Medical Ethics Committee of the National Defense Medical College Hospital (approval no. 4692), Saitama, Japan and Nihon University School of Medicine, Itabashi Hospital, Tokyo, Japan (approval no. MF-2302-0063).
Informed Consent Statement
Written informed consent was obtained from all patients.
Data Availability Statement
The original contributions presented in this study are included in the manuscript and the supplementary material. Further inquiries can be directed to the corresponding author.
Acknowledgments
The first author (K.H.) would like to express his gratitude and appreciation to his advisor, Hiroaki Shimabukuro, who has been an exceptional mentor and has encouraged the author throughout his studies.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Gomes, J.A.; Winters, S.L.; Stewart, D.; Horowitz, S.; Milner, M.; Barreca, P. A new noninvasive index to predict sustained ventricular tachycardia and sudden death in the first year after myocardial infarction: based on signal-averaged electrocardiogram, radionuclide ejection fraction and Holter monitoring. J Am Coll Cardiol 1987, 10, 349–357. [Google Scholar] [CrossRef]
- Ikeda, T.; Sakata, T.; Takami, M.; Kondo, N.; Tezuka, N.; Nakae, T.; Noro, M.; Enjoji, Y.; Abe, R.; Sugi, K.; et al. Combined assessment of T-wave alternans and late potentials used to predict arrhythmic events after myocardial infarction. A prospective study. J Am Coll Cardiol 2000, 35, 722–730. [Google Scholar] [CrossRef] [PubMed]
- Mancini, D.M.; Wong, K.L.; Simson, M.B. Prognostic value of an abnormal signal-averaged electrocardiogram in patients with nonischemic congestive cardiomyopathy. Circulation 1993, 87, 1083–1092. [Google Scholar] [CrossRef] [PubMed]
- Kamath, G.S.; Zareba, W.; Delaney, J.; Koneru, J.N.; McKenna, W.; Gear, K.; Polonsky, S.; Sherrill, D.; Bluemke, D.; Marcus, F.; et al. Value of the signal-averaged electrocardiogram in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Heart Rhythm 2011, 8, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Yodogawa, K.; Seino, Y.; Ohara, T.; Iwasaki, Y.K.; Hayashi, M.; Miyauchi, Y.; Azuma, A.; Shimizu, W. Prognostic significance of ventricular late potentials in patients with pulmonary sarcoidosis. Heart Rhythm 2018, 15, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Takase, B.; Nagashima, M.; Kasamaki, Y.; Shimabukuro, H.; Soma, M.; Nakayama, T. A novel signal-averaged electrocardiogram and an ambulatory-based signal-averaged electrocardiogram show strong correlations with conventional signal-averaged electrocardiogram in healthy subjects: A validation study. J Electrocardiol 2018, 51, 1145–1152. [Google Scholar] [CrossRef]
- Gatzoulis, K.A.; Tsiachris, D.; Arsenos, P.; Antoniou, C.K.; Dilaveris, P.; Sideris, S.; Kanoupakis, E.; Simantirakis, E.; Korantzopoulos, P.; Goudevenos, I.; et al. Arrhythmic risk stratification in post-myocardial infarction patients with preserved ejection fraction: the PRESERVE EF study. Eur Heart J 2019, 40, 2940–2949. [Google Scholar] [CrossRef]
- Hashimoto, K.; Amino, M.; Yoshioka, K.; Kasamaki, Y.; Kinoshita, T.; Ikeda, T. Combined evaluation of ambulatory-based late potentials and nonsustained ventricular tachycardia to predict arrhythmic events in patients with previous myocardial infarction: A Japanese noninvasive electrocardiographic risk stratification of sudden cardiac death (JANIES) substudy. Ann Noninvasive Electrocardiol 2021, 26, e12803. [Google Scholar] [CrossRef]
- Hashimoto, K.; Kinoshita, T.; Miwa, Y.; Amino, M.; Yoshioka, K.; Yodogawa, K.; Nakagawa, M.; Nakamura, K.; Watanabe, E.; Nakamura, K.; et al. Ambulatory electrocardiographic markers predict serious cardiac events in patients with chronic kidney disease: The Japanese Noninvasive Electrocardiographic Risk Stratification of Sudden Cardiac Death in Chronic Kidney Disease (JANIES-CKD) study. Ann Noninvasive Electrocardiol 2022, 27, e12923. [Google Scholar] [CrossRef]
- Abe, A.; Kobayashi, K.; Yuzawa, H.; Sato, H.; Fukunaga, S.; Fujino, T.; Okano, Y.; Yamazaki, J.; Miwa, Y.; Yoshino, H.; et al. Comparison of late potentials for 24 hours between Brugada syndrome and arrhythmogenic right ventricular cardiomyopathy using a novel signal-averaging system based on Holter ECG. Circ Arrhythm Electrophysiol 2012, 5, 789–795. [Google Scholar] [CrossRef]
- Yoshioka, K.; Amino, M.; Zareba, W.; Shima, M.; Matsuzaki, A.; Fujii, T.; Kanda, S.; Deguchi, Y.; Kobayashi, Y.; Ikari, Y.; et al. Identification of high-risk Brugada syndrome patients by combined analysis of late potential and T-wave amplitude variability on ambulatory electrocardiograms. Circ J 2013, 77, 610–618. [Google Scholar] [CrossRef]
- Nakagawa, M.; Iwao, T.; Ishida, S.; Yonemochi, H.; Fujino, T.; Saikawa, T.; Ito, M. Circadian rhythm of the signal averaged electrocardiogram and its relation to heart rate variability in healthy subjects. Heart 1998, 79, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, T.; Hashimoto, K.; Yoshioka, K.; Miwa, Y.; Yodogawa, K.; Watanabe, E.; Nakamura, K.; Nakagawa, M.; Nakamura, K.; Watanabe, T.; et al. Risk stratification for cardiac mortality using electrocardiographic markers based on 24-hour Holter recordings: the JANIES-SHD study. J Cardiol 2020, 75, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Amino, M.; Yoshioka, K.; Ichikawa, T.; Watanabe, E.; Kiyono, K.; Nakamura, M.; Sakama, S.; Ayabe, K.; Fujii, T.; Hashida, T.; et al. The presence of late potentials after percutaneous coronary intervention for the treatment of acute coronary syndrome as a predictor for future significant cardiac events resulting in re-hospitalization. J Electrocardiol 2019, 53, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Breithardt, G.; Cain, M.E.; el-Sherif, N.; Flowers, N.C.; Hombach, V.; Janse, M.; Simson, M.B.; Steinbeck, G. Standards for analysis of ventricular late potentials using high-resolution or signal-averaged electrocardiography. A statement by a Task Force Committee of the European Society of Cardiology, the American Heart Association, and the American College of Cardiology. Circulation 1991, 83, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Task Force of the European Society of Cardiology, the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Steinbigler, P.; Haberl, R.; Jilge, G.; Steinbeck, G. Circadian variability of late potential analysis in Holter electrocardiograms. Pacing Clin Electrophysiol 1999, 22, 1448–1456. [Google Scholar] [CrossRef]
- Nakamura, M.; Yoshioka, K.; Amino, M.; Watanabe, E.; Fujii, T.; Hashida, T.; Fujibayashi, D.; Kanda, S.; Kobayashi, Y.; Tanabe, T.; Ikari, Y. Late potential as a predictor of re-hospitalization after percutaneous coronary intervention for acute coronary syndrome. Tokai J Exp Clin Med 2016, 41, 172–180. [Google Scholar]
- Kremers, M.S.; Black, W.H.; Lange, R.; Wells, P.J.; Solo, M. Electrocardiographic signal-averaging during atrial pacing and effect of cycle length on the terminal QRS in patients with and without inducible ventricular tachycardia. Am J Cardiol 1990, 66, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, J.J.; Ahmed, M.W.; Parker, M.A.; Kadish, A.H. Assessment of effects of autonomic stimulation and blockade on the signal-averaged electrocardiogram. Circulation 1994, 89, 1656–64. [Google Scholar] [CrossRef]
- Yoshioka, K.; Amino, M.; Nakamura, M.; Kanda, S.; Kobayashi, Y.; Ikari, Y.; Shima, M.; Tanabe, T. Incidence of positive ventricular late potentials differs in postural changes among supine, left, and right lateral decubitus, and prone and sitting positions in Brugada syndrome. Ann Noninvasive Electrocardiol 2015, 20, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Chamiec, T.; Kułakowski, P.; Ceremuzyński, L. Exercise producing alterations in the signal-averaged electrocardiogram in patients after myocardial infarction. Eur Heart J 1995, 16, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, M.; Suzuki, M.; Fujii, H.; Kimura, S.; Nishizaki, M.; Sasano, T. Machine learning of microvolt-level 12-lead electrocardiogram can help distinguish takotsubo syndrome and acute anterior myocardial infarction. Cardiovasc Digit Health J 2022, 3, 179–188. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).