Submitted:
02 June 2023
Posted:
05 June 2023
You are already at the latest version
Abstract
Keywords:
1. Summary
2. Ethics Approval
3. Data Description
3.1. Data Composition
- Low cardiovascular risk – CHA2DS2-VASc = [0; 1]
- Intermediate cardiovascular risk – CHA2DS2-VASc = [2; 3]
- High cardiovascular risk – CHA2DS2-VASc = [3; 9]
| Subject Area | Biomedical Imaging, Ophthalmology |
|---|---|
| More specific subject area | Retinal OCT-A volumes analysis for cardiovascular risk prediction |
| Type of data | Image, CSV |
| How data were acquired | Swept-source OCT-A Instrument name : PLEX Elite 9000® (Carl Zeiss Meditec Inc., Dublin, OH, USA) |
| Data format | DICOM for volumes, Bitmap for en face images |
| Experimental factors | Pupillary dilatation with tropicamide 0.5% if signal strength < 8/10 |
| Experimental features | Macular angiography 6 x 6-mm |
| Main data source location | University Hospital of Dijon, Dijon 21000, France |
| Data accessibility | https://rasta.u-bourgogne.fr/ |
- « sup » for superficial plexus or « deep » for deep plexus or « cc » for choriocapillaris plexus
- « OD » for right eye or « OS » for left eye
-
« AnomAlies Rétiniennes précoces au cours du Diabète de type 1 » (AwARD; Early Retinal Anomalies in Type 1 Diabetes) [26]: to specify early retinal microvascular abnormalities by measuring the area of the central retinal avascular zone on SS OCT-A images of patients with type 1 diabetes without diabetic retinopathy (ID-RCB: 2017-A02724-49)95 eyes of 95 patients, from 02/23/2018 to 02/28/2020
-
RETINORM: control group of the AwARD study137 eyes of 75 volunteers, from 04/12/2021 to 11/25/2021
-
« Retinal Microvascular Changes in Familial Hypercholesterolemia: Analysis with Swept-Source Optical Coherence Tomography Angiography » (FAMILIPO) [27]: to analyze the association between retinal vascular density and the presence of atherosclerosis assessed with the Coronary Artery Calcium score and compare SS OCT-A quantitative parameters between patients with familial hypercholesterolemia (FH) and healthy volunteers from the AwARD study without a history of FH162 eyes of 81 patients with FH, from 10/21/2020 to 10/27/2021
-
« Obstructive sleep apnea and Retinal vascular NETwork » (ORNET): to describe retinal microvascular characteristics with SS OCT-A in a population with obstructive sleep apnea syndrome (OSAS) and to compare them with healthy volunteers (ID-RCB: 2018-A02204-51)159 eyes of 79 patients with OSAS and 62 eyes of 33 volunteers without OSAS, from 07/01/2020 to 02/14/2023
-
« Réseau Microvasculaire Rétinien et Chirurgie Cardiaque de revascularisation coronarienne » (MRCC; Retinal Microvascular Network and Coronary Revascularization Cardiac Surgery): to study, in patients scheduled for coronary revascularization cardiac surgery with extracorporeal circulation, the discriminative capacity of retinal vascular density to predict the occurrence of acute renal failure defined by the KDIGO criterion [28] within 7 days of surgery (ID-RCB: 2021-A02895-36)33 eyes of 33 patients, from 06/07/2022 to 03/06/2023
-
« Giant cell arteritis study » (GIANT): to describe retinal microvasculature on SS OCT-A in patients with giant cell arteritis without ophthalmological symptom56 eyes of 40 patients, from 11/21/2017 to 10/18/2022
-
« Evaluation intelligente de la Rétinopathie diabétique » (EviRed; Intelligent Assessment of Diabetic Retinopathy): to propose SS OCT-A analysis to better predict the risk of diabetic retinopathy than the current classification of diabetic retinopathy mainly based on fundus photography (ANR: 18-RHUS-0008)118 eyes of 63 patients without diabetic retinopathy, from 06/01/2021 to 01/19/2022
- -
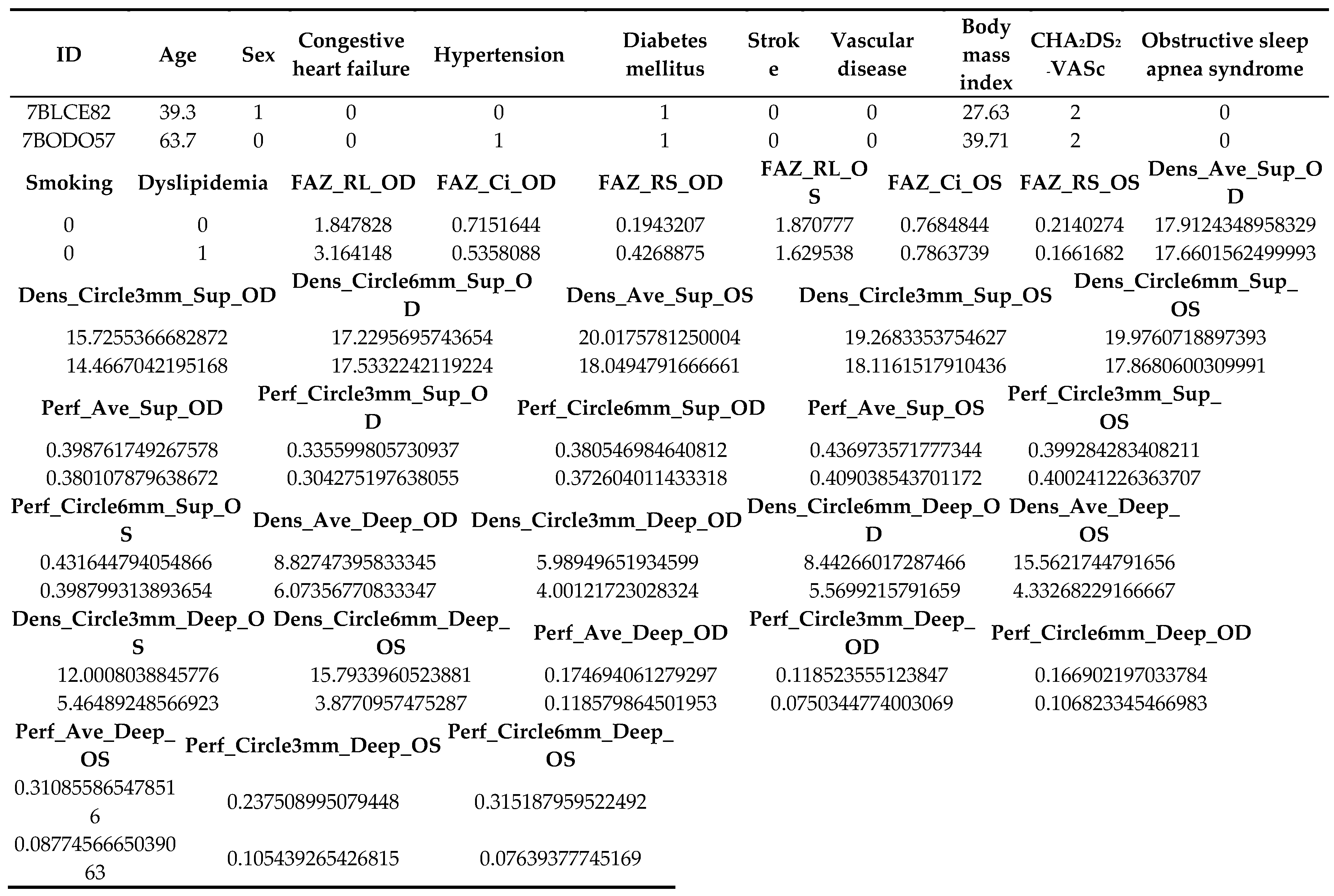
- ID: participant’s anonymous identity code
- -
- Age: age in years at inclusion
- -
- Sex: 0 if male gender, 1 if female gender
- -
- Congestive heart failure: presence of heart failure/moderate-severe cardiac dysfunction with left ventricular ejection fraction ≤ 40%
- -
- Hypertension: presence of hypertension confirmed by ambulatory blood pressure measurement with a systolic blood pressure ≥ 135 mmHg and/or diastolic blood pressure ≥ 85 mmHg
- -
- Diabetes mellitus: presence of diabetes mellitus confirmed by a single blood glucose sample ≥ 2 g/l or confirmed by a second blood glucose sample ≥ 1.26 g/l when the first one is ≥ 1.26 g/L and < 2 g/L
- -
- Stroke: prior stroke or transient ischemic attack or thromboembolism
- -
- Vascular disease: presence of vascular disease (e.g., peripheral artery disease, myocardial infarction, aortic plaque) confirmed by Doppler ultrasonography, coronary angiography/cardiac magnetic resonance imaging (MRI)/myocardial perfusion scintigraphy, or computed tomography angiography, respectively
- -
- Body mass index: body mass divided by the square of height, in kg/m2
- -
- CHA2DS2-VASc: cardiovascular score prediction
- -
- Obstructive sleep apnea syndrome: presence of obstructive sleep apnea syndrome confirmed by respiratory polygraphy or polysomnography
- -
- Smoking: previous or active Smoking
- -
- Dyslipidemia: presence of dyslipidemia confirmed by two blood samples with HDL-c < 0.35g/L or LDL-c > 1.30 g/L and/or TG > 1.5 g/L for patients with cardiovascular risk, and two blood samples with HDL-c < 0.35g/L or LDL-c > 1.60 g/L and/or TG > 1.5 g/L for patients without cardiovascular risk
- -
- OD: oculus dexter (right eye)
- -
- OS: oculus sinister (left eye)
- -
- Fovea Avascular Zone (FAZ) in superficial plexus:
- ○
- FAZ_RL: raw length (perimeter) of the FAZ in mm
- ○
- FAZ_Ci: circularity index of the FAZ ranging from 0 (most irregular circle shape) to 1 (perfect circle shape)
- ○
- FAZ_RS: raw size (area) of the FAZ in mm2
- -
- Vessel density (VD): total length of perfused vasculature per unit area in a region of measurement in units of mm-1. It consists in untangling the entire vasculature in the retina, and measuring its length and then dividing it by the area it originally occupied, ranging from a minimum of 0 (no vessels) and an unbounded maximum
- ○
- Dens_Ave_Sup: VD average in superficial plexus
- ○
- Dens_Circle3mm_Sup: VD in a circle of 3-mm diameter in superficial plexus
- ○
- Dens_Circle6mm_Sup: VD in a circle of 6-mm diameter in superficial plexus
- ○
- Dens_Ave_Deep: VD average in deep plexus
- ○
- Dens_Circle3mm_Deep: VD in a circle of 3-mm diameter in deep plexus
- ○
- Dens_Circle6mm_Deep: VD in a circle of 6-mm diameter in deep plexus
- -
- Perfusion density (PD): total area of perfused vasculature per unit area in a region of measurement ranging from 0 (no perfusion) to 1 (fully perfused)
- ○
- Perf_Ave_Sup: PD average in superficial plexus
- ○
- Perf_Circle3mm_Sup: PD in a circle of 3-mm diameter in superficial plexus
- ○
- Perf_Circle6mm_Sup: PD in a circle of 6-mm diameter in superficial plexus
- ○
- Perf_Ave_Deep: PD average in deep plexus
- ○
- Perf_Circle3mm_Deep: PD in a circle of 3-mm diameter in deep plexus
- ○
- Perf_Circle6mm_Deep: PD in a circle of 6-mm diameter in deep plexus
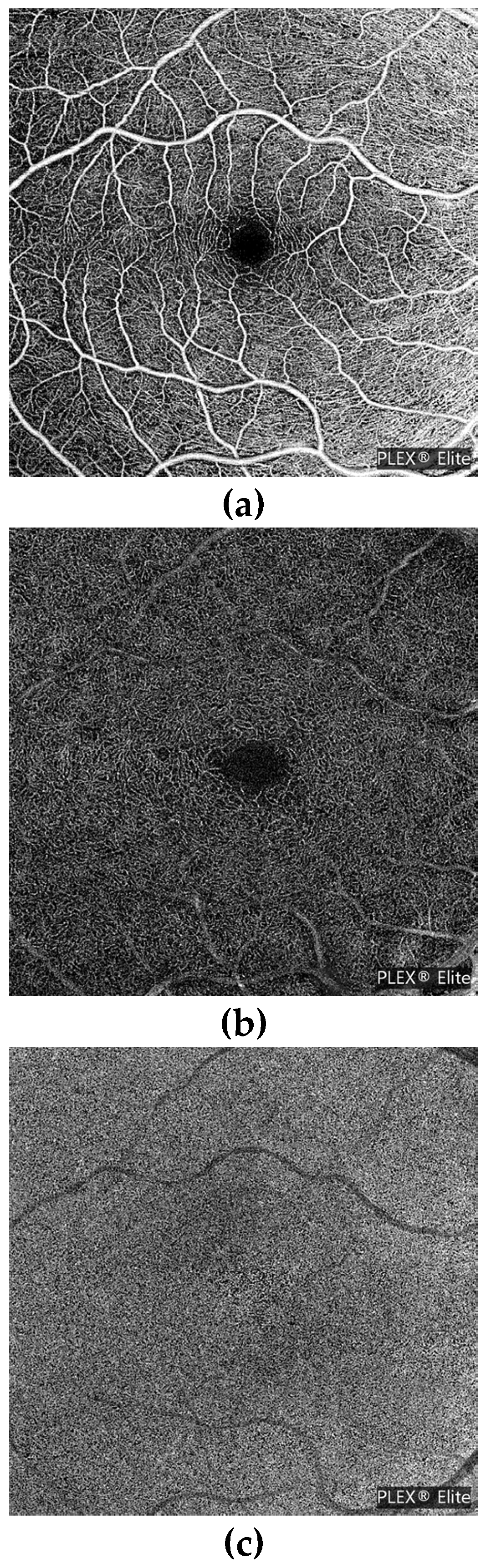
3.2. Swept-Source OCT-A Acquisitions
| Model | Constructor | Technology | Hardware | |||
| PLEX Elite 9000® | Carl Zeiss Meditec Inc, Dublin, USA | Swept Source Optical Coherence Tomography | Optical Micro AngioGraphy (OMAG) | |||
| FOV | Wave length | Slew rate | Axial scan depth | Optical axial resolution | Optical transversal resolution | Number of images in dataset |
| 56° | 1040-1060 nm | 100 000 A-scans/sec | 3.0 mm | 6.3 µm | 20 µm | 2005 en face images 814 angiocubes |
3.3. Quantitative OCT-A Vascular Features
- -
- Superficial and deep slabs (angio and structure)
- -
- Vessel and perfusion traces for superficial and deep slabs
- -
- Superficial and deep vessel and perfusion density maps, color overlay images
- -
- FAZ superficial segmentation
- -
- Density and FAZ quantification results
3.4. Cardiovascular Data
| Risk scheme | Low risk [0 ;1] | Intermediate risk [2 ;3] | High risk [4 ;9] | ||
|---|---|---|---|---|---|
| RASTA (2023) | One or no combination risk factor | One definitive risk factor and 1 or no combination risk factor, or 2 or 3 combination risk factors | Two definitive risk factors, or 1 definitive risk factor and ≥ 2 combination risk factors, or ≥ 4 combination risk factors | ||
| Definitive risk factors: previous stroke/TIA/TE, age > 75 | |||||
| Combination risk factors: heart failure/left ventricular ejection fraction ≤ 40%, hypertension, diabetes, vascular disease, female gender, age 65-74 | |||||
| Risk Factor | Score |
|---|---|
| Congestive heart failure / Left ventricular dysfunction | 1 |
| Hypertension | 1 |
| Age ≥ 75 years | 2 |
| Diabetes mellitus | 1 |
| Stroke / TIA / TE | 2 |
| Vascular disease (prior myocardial infarction, peripheral artery disease, or aortic plaque) | 1 |
| Age 65-74 years | 1 |
| Sex category (i.e., female gender) | 1 |
4. Methods
5. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- WHO. World Health Organization reveals leading causes of death and disability worldwide: 2000-2019. Available online: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019.
- Crea, F.; Camici, P.G.; Bairey Merz, C.N. Coronary microvascular dysfunction: an update. European heart journal 2014, 35, 1101–1111. [Google Scholar] [CrossRef] [PubMed]
- Hughes, S.; Yang, H.; Chan-Ling, T. Vascularization of the Human Fetal Retina: Roles of Vasculogenesis and Angiogenesis. Investigative Ophthalmology & Visual Science 2000, 41, 1217–1228. [Google Scholar]
- Arnould, L.; Binquet, C.; Guenancia, C.; Alassane, S.; Kawasaki, R.; Daien, V.; Tzourio, C.; Kawasaki, Y.; Bourredjem, A.; Bron, A.; et al. Association between the retinal vascular network with Singapore "I" Vessel Assessment (SIVA) software, cardiovascular history and risk factors in the elderly: The Montrachet study, population-based study. PLOS ONE 2018, 13, e0194694. [Google Scholar] [CrossRef]
- Seidelmann, S.B.; Claggett, B.; Bravo, P.E.; Gupta, A.; Farhad, H.; Klein, B.E.; Klein, R.; Carli, M.D.; Solomon, S.D. Retinal Vessel Calibers in Predicting Long-Term Cardiovascular Outcomes. Circulation 2016, 134, 1328–1338. [Google Scholar] [CrossRef]
- Arnould, L.; Guenancia, C.; Azemar, A.; Alan, G.; Pitois, S.; Bichat, F.; Zeller, M.; Gabrielle, P.-H.; Bron, A.M.; Creuzot-Garcher, C.; et al. The EYE-MI Pilot Study: A Prospective Acute Coronary Syndrome Cohort Evaluated With Retinal Optical Coherence Tomography Angiography. Investigative Ophthalmology & Visual Science 2018, 59, 4299–4306. [Google Scholar] [CrossRef]
- Jiang, S.; Fang, C.; Xu, X.; Xing, L.; Sun, S.; Peng, C.; Yin, Y.; Lei, F.; Wang, Y.; Li, L.; et al. Identification of High-Risk Coronary Lesions by 3-Vessel Optical Coherence Tomography. J Am Coll Cardiol 2023, 81, 1217–1230. [Google Scholar] [CrossRef]
- Anderson, K.M.; Wilson, P.W.; Odell, P.M.; Kannel, W.B. An updated coronary risk profile. A statement for health professionals. Circulation 1991, 83, 356–362. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B., Sr.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014, 63, 2935–2959. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S49–73. [Google Scholar] [CrossRef]
- group, S.w.; collaboration, E.C.r. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. European heart journal 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Welles, C.C.; Whooley, M.A.; Na, B.; Ganz, P.; Schiller, N.B.; Turakhia, M.P. The CHADS2 score predicts ischemic stroke in the absence of atrial fibrillation among subjects with coronary heart disease: data from the Heart and Soul Study. American heart journal 2011, 162, 555–561. [Google Scholar] [CrossRef]
- Taşolar, H.; Çetin, M.; Ballı, M.; Bayramoğlu, A.; Otlu, Y.; Türkmen, S.; Aktürk, E. CHA2DS2-VASc-HS score in non-ST elevation acute coronary syndrome patients: assessment of coronary artery disease severity and complexity and comparison to other scoring systems in the prediction of in-hospital major adverse cardiovascular events. Anatolian journal of cardiology 2016, 16, 742–748. [Google Scholar] [CrossRef]
- Kang, I.S.; Pyun, W.B.; Shin, G.J. Predictive value of CHADS2 score for cardiovascular events in patients with acute coronary syndrome and documented coronary artery disease. The Korean journal of internal medicine 2016, 31, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Satilmisoglu, M.H.; Gul, M.; Yildiz, G.; Akgul, O.; Kaya, M.; Cakmak, H.A.; Akkaya, E.; Aslan, S.; Ameri, M.T.; Ozyilmaz, S.O.; et al. Prognostic value of CHA2DS2-VASc score in patients with ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention. Acta cardiologica 2016, 71, 663–669. [Google Scholar] [CrossRef]
- Satılmış, S.; Durmuş, G. Predictive accuracy of CHA(2)DS(2)-VASc score in determining the high thrombus burden in patients with non-ST-elevation myocardial infarction. Acta cardiologica 2021, 76, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.C.; Su, H.M.; Lee, W.H.; Chiu, C.A.; Chi, N.Y.; Tsai, W.C.; Lin, T.H.; Voon, W.C.; Lai, W.T.; Sheu, S.H.; et al. CHA(2)DS(2)-VASc Score and Risk of New-Onset Peripheral Arterial Occlusive Disease in Patients without Atrial Fibrillation. Acta Cardiologica Sinica 2021, 37, 261–268. [Google Scholar] [CrossRef]
- Kurtul, A.; Acikgoz, S.K. Validation of the CHA2DS2-VASc Score in Predicting Coronary Atherosclerotic Burden and In-Hospital Mortality in Patients With Acute Coronary Syndrome. The American journal of cardiology 2017, 120, 8–14. [Google Scholar] [CrossRef]
- Decencière, E.; Zhang, X.; Cazuguel, G.; Laÿ, B.; Cochener, B.; Trone, C.; Gain, P.; Ordóñez-Varela, J.-R.; Massin, P.; Erginay, A.; et al. FEEDBACK ON A PUBLICLY DISTRIBUTED IMAGE DATABASE: THE MESSIDOR DATABASE. Image Analysis & Stereology 2014, 231–234. [Google Scholar] [CrossRef]
- Staal, J.; Abràmoff, M.D.; Niemeijer, M.; Viergever, M.A.; van Ginneken, B. Ridge-based vessel segmentation in color images of the retina. IEEE transactions on medical imaging 2004, 23, 501–509. [Google Scholar] [CrossRef]
- Hoover, A.; Kouznetsova, V.; Goldbaum, M. Locating blood vessels in retinal images by piecewise threshold probing of a matched filter response. IEEE transactions on medical imaging 2000, 19, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Gulshan, V.; Peng, L.; Coram, M.; Stumpe, M.C.; Wu, D.; Narayanaswamy, A.; Venugopalan, S.; Widner, K.; Madams, T.; Cuadros, J.; et al. Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. Jama 2016, 316, 2402–2410. [Google Scholar] [CrossRef] [PubMed]
- Decencière, E.; Cazuguel, G.; Zhang, X.; Thibault, G.; Klein, J.-C.; Meyer, F.; Marcotegui, B.; Quellec, G.; Lamard, M.; Danno, R.; et al. TeleOphta: Machine learning and image processing methods for teleophthalmology. Innovation and Research in BioMedical engineering 2013, 34, 196–203. [Google Scholar]
- Khan, S.M.; Liu, X.; Nath, S.; Korot, E.; Faes, L.; Wagner, S.K.; Keane, P.A.; Sebire, N.J.; Burton, M.J.; Denniston, A.K. A global review of publicly available datasets for ophthalmological imaging: barriers to access, usability, and generalisability. Lancet Digit Health 2021, 3, e51–e66. [Google Scholar] [CrossRef]
- Eid, P.; Creuzot-Garcher, C.; Aho, L.S.; Gabrielle, P.H.; Charpin, E.; Haddad, D.; Steinberg, L.A.; Bron, A.; Verges, B.; Arnould, L. Early Retinal Microvascular Changes Assessed with Swept-Source OCT Angiography in Type 1 Diabetes Patients without Retinopathy. Journal of clinical medicine 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- Eid, P.; Arnould, L.; Gabrielle, P.H.; Aho, L.S.; Farnier, M.; Creuzot-Garcher, C.; Cottin, Y. Retinal Microvascular Changes in Familial Hypercholesterolemia: Analysis with Swept-Source Optical Coherence Tomography Angiography. J Pers Med 2022, 12. [Google Scholar] [CrossRef]
- Summary of Recommendation Statements. Kidney international supplements 2012, 2, 8–12. [CrossRef]
- Laíns, I.; Wang, J.C.; Cui, Y.; Katz, R.; Vingopoulos, F.; Staurenghi, G.; Vavvas, D.G.; Miller, J.W.; Miller, J.B. Retinal applications of swept source optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA). Prog Retin Eye Res 2021, 84, 100951. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019, 74, 1376–1414. [Google Scholar] [CrossRef]
- Ridker, P.M.; Cook, N.R. Statins: new American guidelines for prevention of cardiovascular disease. Lancet (London, England) 2013, 382, 1762–1765. [Google Scholar] [CrossRef]
- Kuragaichi, T.; Kataoka, Y.; Miyakoshi, C.; Miyamoto, T.; Sato, Y. External validation of pooled cohort equations using systolic blood pressure intervention trial data. BMC research notes 2019, 12, 271. [Google Scholar] [CrossRef] [PubMed]
- Harb, S.C.; Wang, T.K.M.; Nemer, D.; Wu, Y.; Cho, L.; Menon, V.; Wazni, O.; Cremer, P.C.; Jaber, W. CHA(2)DS(2)-VASc score stratifies mortality risk in patients with and without atrial fibrillation. Open heart 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.T.; Campbell, B.C.; Meretoja, A.; Churilov, L.; Lees, K.R.; Donnan, G.A.; Davis, S.M. Pre-stroke CHADS2 and CHA2DS2-VASc scores are useful in stratifying three-month outcomes in patients with and without atrial fibrillation. Cerebrovascular diseases (Basel, Switzerland) 2013, 36, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.H.; Yiu, K.H.; Lau, K.K.; Yiu, Y.F.; Li, S.W.; Lam, T.H.; Lau, C.P.; Siu, C.W.; Tse, H.F. The CHADS2 and CHA2DS2-VASc scores predict adverse vascular function, ischemic stroke and cardiovascular death in high-risk patients without atrial fibrillation: role of incorporating PR prolongation. Atherosclerosis 2014, 237, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Cheng, C.L.; Huang, J.L.; Yang, N.I.; Chang, H.C.; Chang, K.C.; Sung, S.H.; Shyu, K.G.; Wang, C.C.; Yin, W.H.; et al. Mortality prediction using CHADS2/CHA2DS2-VASc/R2CHADS2 scores in systolic heart failure patients with or without atrial fibrillation. Medicine 2017, 96, e8338. [Google Scholar] [CrossRef]
- Yang, H.J.; Wang, G.J.; Shuai, W.; Shen, C.J.; Kong, B.; Huang, H. The Value of the CHADS(2) and CHA(2)DS(2)-VASc Score for Predicting the Prognosis in Lacunar Stroke with or without Atrial Fibrillation Patients. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association 2019, 28, 104143. [Google Scholar] [CrossRef]
- Wagner, S.K.; Fu, D.J.; Faes, L.; Liu, X.; Huemer, J.; Khalid, H.; Ferraz, D.; Korot, E.; Kelly, C.; Balaskas, K.; et al. Insights into Systemic Disease through Retinal Imaging-Based Oculomics. Transl Vis Sci Technol 2020, 9, 6. [Google Scholar] [CrossRef]
- Arnould, L.; Meriaudeau, F.; Guenancia, C.; Germanese, C.; Delcourt, C.; Kawasaki, R.; Cheung, C.Y.; Creuzot-Garcher, C.; Grzybowski, A. Using Artificial Intelligence to Analyse the Retinal Vascular Network: The Future of Cardiovascular Risk Assessment Based on Oculomics? A Narrative Review. Ophthalmol Ther 2023, 12, 657–674. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





