Submitted:
25 May 2023
Posted:
29 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction Section:
1.1. The Impacts of COVID-19 on Mental Health of Victims
1.2. How Support from Family & Friends Assist COVID-19 Sufferers
1.3. Importance of Communication Family Members/Friends with both Health Care Providers and Affected Patients
1.5. COVID-19 and Daily Hassles
1.6. The Current Study
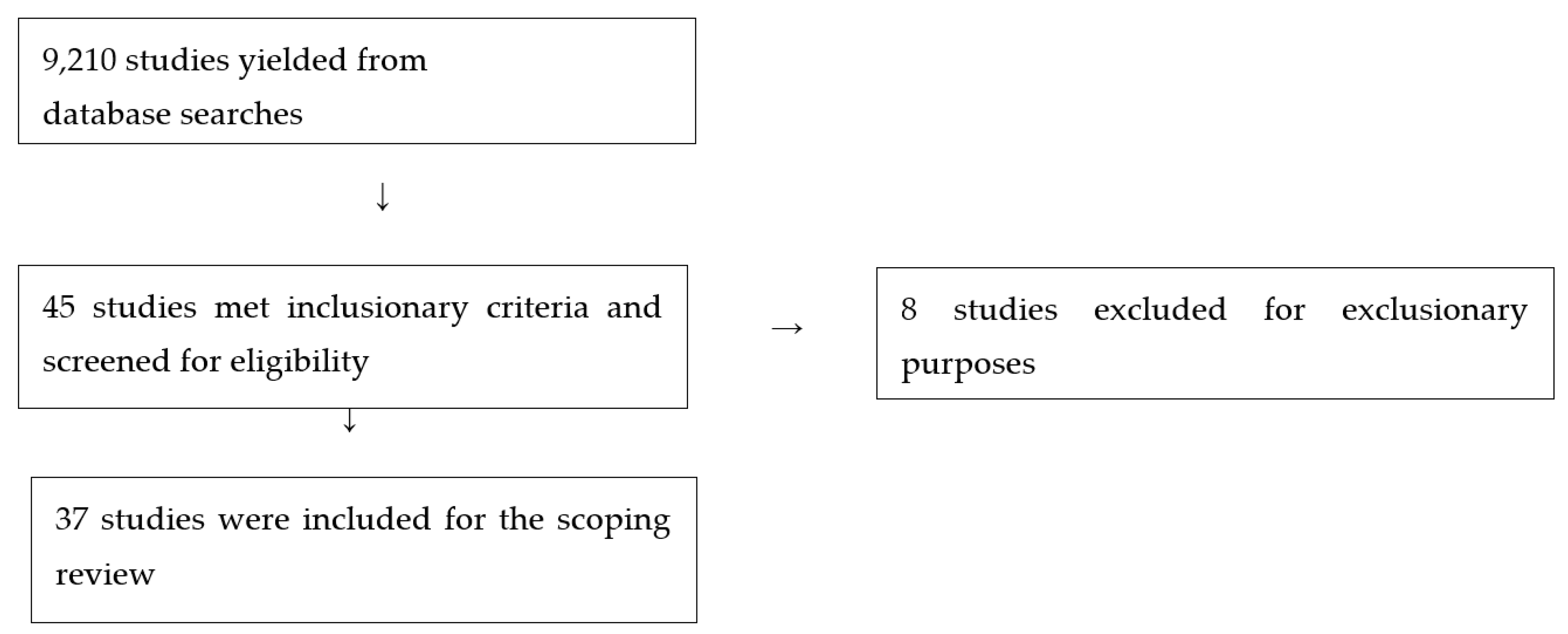
2. Methods
3. Results Section:
4. Discussion Section:
5. Limitations to the Study:
6. Conclusion:
References
- Wu, Z.; McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA, 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO coronavirus COVID-19 dashboard; 2023; Available online: https://covid19.who.int/.
- Cutler, D.M.; Summers, L.H. The COVID-19 pandemic and the $16 trillion virus. JAMA. 2020, 324, 15:1495–1496. [Google Scholar] [CrossRef] [PubMed]
- Thye, A.Y.K; Law, J.W.F.; Tan, L.T.H.; Pusparajah, P.; Ser, H.L.; Thurairajasingam, S.; Letchumanan, V.; Lee, L.H. Psychological Symptoms in COVID-19 Patients: Insights into Pathophysiology and Risk Factors of Long COVID-19. Biology 2022, 11, 61. [Google Scholar] [CrossRef] [PubMed]
- Taquet, M.; Luciano, S.; Geddes, J. R.; Harrison, P. J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2021, 8, 130–140. [Google Scholar] [CrossRef]
- Guo, M.; Kong, M.; Shi, W.; Wang, M.; Yang, H. Listening to COVID-19 survivors: what they need after early discharge from hospital-a qualitative study. Int. J. Qual. Stud. Health Well-being, 2022, 17, 2030001. [Google Scholar] [CrossRef] [PubMed]
- Rajkumari, B.; Akham, N.; Konjengbam, O. K.; Pangambam, A. D.; Ningthoujam, S. D. Post-traumatic stress disorder among COVID-19 survivors in Manipur: A cross-sectional study. Fam. Med. Prim. Care 2022, 11, 2139. [Google Scholar] [CrossRef]
- Wang, B.; Yang, X.; Fu, L.; Hu, Y.; Luo, D.; Xiao, X.; Ju, N.; Zheng, W.; Xu, H.; Fang, Y.; et al. Post-traumatic stress disorder symptoms in COVID-19 survivors 6 Months after hospital discharge: An application of the conservation of resource theory. Front. Psychiatry 2022, 12, 2414. [Google Scholar] [CrossRef]
- Wardani-Diadjeng, S.; Rismaina, P.; Miftahul, J. The Role of family support on self efficacy recovery pregnant women confirmed Covid-19. J. Posit Sch Psychol 2022, 6, 5198–5202. [Google Scholar]
- Aguilar-Latorre, A.; Oliván-Blázquez, B.; Porroche-Escudero, A.; Méndez -Lopez, F.; García-Gallego, V.; Benedé-Azagra, B.; Magallón-Botaya, R. The impact of the COVID-19 lockdown on depression sufferers: a qualitative study from the province of Zaragoza, Spain. BMC Public Health. 2022, 22, 780. [Google Scholar] [CrossRef]
- Luttik, M. L. A.; Mahrer-Imhof, R.; García-Vivar, C.; Brødsgaard, A.; Dieperink, K. B.; Imhof, L.; Ostergaard, B.; Svavarsdottir, E.K.; Konradsen, H. The COVID-19 pandemic: A family affair. J. Fam. Nurs. 2020, 262, 87–89. [Google Scholar] [CrossRef]
- Li, S.; Xu, Q. Family support as a protective factor for attitudes toward social distancing and in preserving positive mental health during the COVID-19 pandemic. J. Health Psychol, 2022, 274, 858–67. [Google Scholar] [CrossRef] [PubMed]
- Voo, T.C.; Senguttuvan, M.; Tam, C.C. Family presence for patients and separated relatives during COVID-19: Physical, virtual, and surrogate. J. Bioeth Inq. 2020, 17, 767–772. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.L.; Turnbull, A.E.; Oppenheim, I.M.; Courtright, K.R. Family-centered care during the COVID-19 era. J. Pain Symptom Manag. 2020, 60, e93–e97. [Google Scholar] [CrossRef] [PubMed]
- Billingsley, L. Using video conferencing applications to share the death experience during the COVID-19 pandemic. J. Radiol Nurs 2020, 39, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Klop, H. T.; Nasori, M.; Klinge, T. W.; Hoopman, R.; de Vos, M.A.; du Perron, C.; van Zuylen, L.; Steegers, M.; ten Tusscher, B.L.; Abbink, F.C.H.; et al. Family support on intensive care units during the COVID-19 pandemic: a qualitative evaluation study into experiences of relatives. BMC Health Serv. Res. 2021, 21, 1–12. [Google Scholar] [CrossRef]
- Mirhosseini, S.; Heshmati Nabavi, F.; Behnam Vashani, H.; Vaghee, S. Evaluating the effect of online psychoeducational support group on perceived stress in family caregivers of COVID-19 survivors. Omeg:J. Death Dying 2022, 0. [Google Scholar] [CrossRef]
- Hado, E.; Friss Feinberg, L. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J. Aging Soc. Policy, 2020, 32, 410–415. [Google Scholar] [CrossRef]
- Karpman, M.; Zuckerman, S.; Gonzalez, D.; Kenney, G.M. The COVID-19 pandemic is straining families’ abilities to afford basic needs. 2020. Available online: https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_2.pdf.
- Sharma, S.V.; Chuang, R.J.; Rushing, M.; Naylor, B.; Ranjit, N.; Pomeroy, M.; Markham, C. Peer reviewed: social determinants of health–related needs during COVID-19 among low-income households with children. Prev. Chronic Dis 2020, 17. [Google Scholar] [CrossRef]
- Gopalan, H.S.; Misra, A. COVID-19 pandemic and challenges for socio-economic issues, healthcare and National Health Programs in India. Diabetes Metab Syndr. 2020, 5, 757–759. [Google Scholar] [CrossRef]
- Patel, J.A.; Nielsen, F.B.H.; Badiani, A.A.; Assi, S.; Unadkat, V.A.; Patel, B.; Ravindrane, R.; Wardle, H. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020, 183, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Gaggero, A.; Fernández-Pérez, Á.; Jiménez-Rubio, D. Effect of the COVID-19 pandemic on depression in older adults: A panel data analysis. Health Policy 2022, 126, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O'Malley, L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D. G.; PRISMA, Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Berntzen, H.; Lind, R.; Alfheim, H.; Tøien, K. Coping in times of disruption and deprivation—Experiences of family members during COVID-19 patients' critical illness: A qualitative study. Nurs. Open 2023. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, T.; Isaksson, M.; Schelin, C.; Lyngå, P.; Schandl, A. Family members' experiences of COVID-19 visiting restrictions in the intensive care unit—A qualitative study. J. Clinc. Nurs. 2023. [Google Scholar] [CrossRef]
- Ghezeljeh, T.N.; Rezaei, M.; Shahrestanaki, S.K.; Milani, A.S. Exploring family caregiver challenges in caring for patients with COVID-19 in intensive care units. Front Public Health. 2023, 11, 1057396. [Google Scholar] [CrossRef]
- Onrust, M.; Visser, A.; van Veenendaal, N.; Dieperink, W.; Luttik, M. L.; Derksen, M. H. G.; van der Meulen, I. C.; van der Meulen, I.C. Physical, social, mental and spiritual functioning of COVID-19 intensive care unit-survivors and their family members one year after intensive care unit-discharge: A prospective cohort study. Intensive Crit Care Nurs, 2023, 75, 103366. [Google Scholar] [CrossRef]
- Apostol-Nicodemus, L.; Tabios, I.K.B.; Limpoco, A.G.O.; Domingo, G.D.P.; Tantengco, O.A.G. Psychosocial distress among family members of COVID-19 patients admitted to hospital and isolation facilities in the Philippines: A prospective cohort study. J. Clin. Med. 2022, 11, 5236. [Google Scholar] [CrossRef]
- Galazzi, A.; Binda, F.; Gambazza, S.; Cantù, F.; Colombo, E.; Adamini, I.; Graselli, G.; Lusignani, M.; Laquintana, D.; Rasero, L. The end of life of patients with COVID-19 in intensive care unit and the stress level on their family members: A cross-sectional study. Nurse Crit Care, 2023, 28, 133–140. [Google Scholar] [CrossRef]
- Greenberg, J.A.; Basapur, S.; Quinn, T. V.; Bulger, J. L.; Schwartz, N. H.; Oh, S.K.; Shah, R.C.; Glover, C. M. Challenges faced by families of critically ill patients during the first wave of the COVID-19 pandemic. Patient Educ. Couns. 2022, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Heesakkers, H.; van der Hoeven, J.G.; Corsten, S.; Janssen, I.; Ewalds, E.; Burgers-Bonthuis, D.; Rettig, T.C.D.; Jacobs, C.; van Santen, S.; Slooter, A.J.C.; et al. Mental health symptoms in family members of COVID-19 ICU survivors 3 and 12 months after ICU admission: a multicentre prospective cohort study. Intensive Care Med. 2022, 48, 322–331. [Google Scholar] [CrossRef]
- Khaleghparast, S.; Ghanbari, B.; Maleki, M.; Zamani, F.; Peighambari, M.M.; Karbalaie, M.H.N.; Mazloomzadeh, S.; Tameshkel, F.S.; Manshouri, S. Anxiety, knowledge and lived experiences of families with COVID-19 patients: A mixed-method multi-center study in Iran. Iran. J. Med. Sci. 2022, 47, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Webb, F. J.; Wiblishauser, M. J.; Sharma, M. COVID-19 infection among family and friends: The psychological impact on non-infected persons. Brain Sci. 2022, 12, 112. [Google Scholar] [CrossRef]
- Jafari-Oori, M.; Ebadi, A.; Moradian, S. T.; Jafari, M. , Dehi, M.; & Fard, F. G. Psychiatric distress in family caregivers of patients with COVID-19. Arch of Psychiatr Nurs. 2022, 37, 69–75. [Google Scholar] [CrossRef]
- Mawaddah, A.; Suza, D. E.; Tarigan, A. P. Family experience while caring for Covid-19 patients during home quarantine. Jurnal Keperawatan 2022, 14, 301–310. [Google Scholar]
- Mejia, C. R.; Alvarez-Risco, A.; Mejía, Y. M.; Quispe, S.C.; Del-Aguila-Arcentales, S.; Serna-Alarcón, V.; Vilela-Estrada, M.A.; Armada, J.; Yáñez, J. A. Stress, depression and/or anxiety according to the death by COVID-19 of a family member or friend in health sciences students in Latin America during the first wave. Sustainability. 2022, 14, 15515. [Google Scholar] [CrossRef]
- Nohesara, S.; Saeidi, M.; Mosavari, H.; Ghalichi, L.; Alebouyeh, M. R. Grief experience among ICU staff with loss of family members during COVID-19 outbreak in Iran: A qualitative study. Front in Psychiatry 2022, 13. [Google Scholar] [CrossRef]
- Robinson-Lane, S.G.; Leggett, A.N.; Johnson, F.U.; Leonard, N.; Carmichael, A.G.; Oxford, G.; Miah, T.; Wright, J.J.; Blok, A.C.; Iwashyna, T.J.; et al. Caregiving in the COVID-19 pandemic: Family adaptions following an intensive care unit hospitalization. J. Clin. Nurs. 2022, 00, 1–2. [Google Scholar] [CrossRef]
- Rostami, M.; Farmani, P.; Hosseinzadeh, Z.; Hajimiri, K.; Amanloo, M.; Soleimani, M.; Dadashi, M. Stress, anxiety and depression among family caregivers of COVID-19 patients in Northwest Iran: A cross-sectional study. J. Iran. Med. Council, 2022, 5, 147–155. [Google Scholar] [CrossRef]
- Bartoli, D.; Trotta, F.; Simeone, S.; Pucciarelli, G.; Orsi, G. B.; Acampora, O.; Di Muzio, M.; Cappitella, C.; Rocco, M. The lived experiences of family members of Covid-19 patients admitted to intensive care unit: A phenomenological study. Heart & Lung, 2021, 50, 926–932. [Google Scholar] [CrossRef]
- Beck, K.; Vincent, A.; Becker, C.; Keller, A.; Cam, H.; Schaefert, R.; Reinhardt, T.; Sutter, R.; Tisljar, K.; Bassetti, S.; et al. Prevalence and factors associated with psychological burden in COVID-19 patients and their relatives: A prospective observational cohort study. PLoS One, 2021, 16, e0250590. [Google Scholar] [CrossRef] [PubMed]
- Borghi, L.; Menichetti, J. Strategies to cope with the COVID-related deaths among family members. Front. Psychiatry, 2021, 12, 622850. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Wittenberg, E.; Sullivan, S.S.; Lorenz, R. A.; Chang, Y. P. The experiences of family members of ventilated COVID-19 patients in the intensive care unit: a qualitative study. Am. J. Hosp. Palliat Care. 2021, 38, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Jarial, K.; Halder, S. Perceived stress and anxiety during pandemic in family members. J. Psychosoc. Res. 2021, 16. [Google Scholar] [CrossRef]
- Joaquim, R.M.; Pinto, A. L.C.B.; Guatimosim, R. F.; de Paula, J. J.; Costa, D. S.; Diaz, A. P.; da Silva, A.G.; Pinheiro, M.I.C.; Serpa, A.L.O.; Miranda, D.M.; et al. Bereavement and psychological distress during COVID-19 pandemics: The impact of death experience on mental health. Curr. Res. Behav. Sci. 2021, 2, 100019. [Google Scholar] [CrossRef]
- Kentish-Barnes, N.; Cohen-Solal, Z.; Morin, L.; Souppart, V.; Pochard, F.; Azoulay, E. Lived experiences of family members of patients with severe COVID-19 who died in intensive care units in France. JAMA Newt. Open 2021, 4, e2113355–e2113355. [Google Scholar] [CrossRef]
- Koçak, O.; Koçak, Ö. E.; Younis, M.Z. The psychological consequences of COVID-19 fear and the moderator effects of individuals’ underlying illness and witnessing infected friends and family. Int. J. Environ. Res. Public Health, 2021, 18, 1836. [Google Scholar] [CrossRef]
- Nakhae, M.; Vagharseyyedin, S. A.; Mahmoudirad, G.; Shahdadi, H. The experience of family caregivers in treatment of COVID-19 patients: a qualitative study. Neuropsychiatr. i Neuropsychol. 2021, 16, 131–137. [Google Scholar] [CrossRef]
- Orsini, A.; Corsi, M.; Pedrinelli, V.; Santangelo, A.; Bertelloni, C.; Dell’Oste, V.; Cordelli, D.; Perrone, A.; Parini, L.; Lanari, M.; et al. Post-traumatic stress, anxiety, and depressive symptoms in caregivers of children tested for COVID-19 in the acute phase of the Italian outbreak. J. Psychiatr. Res. 2021, 135, 256–263. [Google Scholar] [CrossRef]
- Picardi, A.; Miniotti, M.; Leombruni, P.; Gigantesco, A. A qualitative study regarding COVID-19 inpatient family caregivers’ need for supportive care. Clin. Pract. Epidemiol Ment Health. 2021, 17, 161. [Google Scholar] [CrossRef] [PubMed]
- Prakash, J.; Dangi, A.; Chaterjee, K.; Yadav, P., Srivastava; Chauhan, V. S. Assessment of depression, anxiety and stress in COVID-19 infected individuals and their families. Med J. Armed Forces India 2021, 77, S424–S429. [Google Scholar] [CrossRef]
- Rahimi, T.; Dastyar, N.; Rafati, F. Experiences of family caregivers of patients with COVID-19. BMC Fam. Pract. 2021, 22, 137. [Google Scholar] [CrossRef] [PubMed]
- Selman, L.E.; Chamberlain, C.; Sowden, R.; Chao, D.; Selman, D.; Taubert, M.; Braude, P. Sadness, despair and anger when a patient dies alone from COVID-19: A thematic content analysis of Twitter data from bereaved family members and friends. Palliat Med 2021, 35, 1267–1276. [Google Scholar] [CrossRef]
- van Veenendaal, N.; van der Meulen, I. C.; Onrust, M.; Paans, W.; Dieperink, W.; van der Voort, P. H. J. Six-month outcomes in COVID-19 ICU patients and their family members: a prospective cohort study. Healthcare 2021, 9, 865. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Zhang, D.; Xu, D.; Li, X.; Xie, Y. J.; Sun, W.; Lee, E.K.P.; Yip, B.H.K.; Mo, P.K.H.; Xiao, S.; et al. Physical and mental health outcomes including behavior and attitudes in people having social contacts with COVID-19 patients. PLoS One, 2021, 16, e0245945. [Google Scholar] [CrossRef]
- Zhao, YJ.; Zhang, SF.; Li, W.; Zhang, L.; Cheung, T.; Tang, Y.L.; Ng, C.H; Yang, B.X.; Xiang, Y.T. Mental health status and quality of life in close contacts of COVID-19 patients in the post-COVID-19 era: a comparative study. Transl Psychiatry, 2021, 11, 505. [Google Scholar] [CrossRef]
- Mirzaei, A.; Raesi, R.; Saghari, S.; Raei, M. Evaluation of family caregiver burden among COVID-19 patients. Open Public Health J. 2020, 13. [Google Scholar] [CrossRef]
- Mohammadi, F.; Oshvandi, K.; Shamsaei, F.; Cheraghi, F.; Khodaveisi, M.; Bijani, M. The mental health crises of the families of COVID-19 victims: a qualitative study. BMC Fam. Pract. 2021, 22, 94. [Google Scholar] [CrossRef]
- Rizvi Jafree, S.; Momina, A.U.; Naqi, S.A. Significant other family members and their experiences of COVID-19 in Pakistan: A qualitative study with implications for social policy. Stigma Health, 2020, 5, 380. [Google Scholar] [CrossRef]
- Tanoue, Y.; Nomura, S.; Yoneoka, D.; Kawashima, T.; Eguchi, A.; Shi, S.; Harada, N.; Miyata, H. Mental health of family, friends, and co-workers of COVID-19 patients in Japan. Psychiatry Res. 2020, 291, 113067. [Google Scholar] [CrossRef]
- Rees, J.; O'boyle, C.; MacDonagh, R. Quality of life: Impact of chronic illness on the partner. J.R. Soc. Med 2001, 94, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, M.; Langiano, E.; Di Brango, T.; Di Ciocci, L.; Bauco, C.; De Vito, E. Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health Qual Life Outcomes, 2008, 6, 93. [Google Scholar] [CrossRef]
- Manzini, C. S. S.; Vale, F. A. C. D. Emotional disorders evidenced by family caregivers of older people with Alzheimer’s disease. Dement & Neuropsychol, 2022, 14, 56–61. [Google Scholar] [CrossRef]
- García-Alberca, J. M.; Lara, J. P.; Berthier, M. L. Anxiety and depression in caregivers are associated with patient and caregiver characteristics in Alzheimer’s disease. Int J Psychiatry Med 2011, 41, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Beach, S.R.; Schulz, R.; Donovan, H.; Rosland, A.M. Family caregiving during the COVID-19 pandemic. Gerontologist 2021, 61, 650–660. [Google Scholar] [CrossRef]
- Gallagher, S.; Wetherell, M. A. Risk of depression in family caregivers: unintended consequence of COVID-19. BJPsych Open, 2020, 6, e119. [Google Scholar] [CrossRef]
- Feder, S.; Smith, D.; Griffin, H.; Shreve, S.T.; Kinder, D.; Kutney-Lee, A.; Ersek, M. "Why Couldn't I Go in To See Him?" Bereaved Families' Perceptions of End-of-Life Communication During COVID-19. J. Am Geriatr Soc. 2021, 69, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Bevan, J.L.; Pecchioni, L.L. Understanding the impact of family caregiver cancer literacy on patient health outcomes. Patient Educ Couns 2008, 71, 356–364. [Google Scholar] [CrossRef]
- Given, B.; Sherwood, P.R.; Given, C. W. What knowledge and skills do caregivers need? J. Soc. Work Educ. 2008, 44, 115–123. [Google Scholar] [CrossRef]
- Schulz, R.; Martire, L.M. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am. J. Geriatr. Psychiatry 2004, 12, 240–249. [Google Scholar] [CrossRef]
- Tsai, P.F.; Jirovec, M.M. The relationships between depression and other outcomes of chronic illness caregiving. BMC Nurs. 2005, 4. [Google Scholar] [CrossRef] [PubMed]
- De Maria, M.; Tagliabue, S.; Ausili, D.; Vellone, E.; Matarese, M. Perceived social support and health-related quality of life in older adults who have multiple chronic conditions and their caregivers: a dyadic analysis. Soc. Sci. Med. 2020, 262, 113193. [Google Scholar] [CrossRef] [PubMed]
- Adelman, R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver burden: a clinical review. JAMA. 2014, 311, 1052–60. [Google Scholar] [CrossRef]
- Sit, J. W.; Wong, T. K.; Clinton, M.; Li, L. S.; Fong, Y. M. Stroke care in the home: the impact of social support on the general health of family caregivers. J. Clinc. Nurs. 2004, 13, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Abu Bakar, S.H.; Weatherley, R.; Omar, N.; Abdullah, F.; Mohamad Aun, N. S. Projecting social support needs of informal caregivers in Malaysia. Health Soc. Care Community, 2014, 22, 144–154. [Google Scholar] [CrossRef]
- Nightingale, C.L.; Curbow, B.A.; Wingard, J.R.; Pereira, D.B.; Carnaby, G.D. Burden, quality of life, and social support in caregivers of patients undergoing radiotherapy for head and neck cancer: A pilot study. Chronic Illn. 2016, 12, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Chang, H. Y.; Chiou, C. J.; Chen, N. S. Impact of mental health and caregiver burden on family caregivers’ physical health. Arch Gerontol Geriat, 2010, 50, 267–271. [Google Scholar] [CrossRef]
- Reed, C.; Belger, M.; Dell'Agnello, G.; Wimo, A.; Argimon, J.M.; Bruno, G.; Dodel, R.; Haro, J.M.; Jones, R.W. Vellas, Caregiver burden in Alzheimer's disease: differential associations in adult-child and spousal caregivers in the GERAS observational study. Dement. Geriatr. Cogn Disord. Extra 2014, 4, 51–64. [Google Scholar] [CrossRef]
- Hugelius, K.; Harada, N.; Marutani, M. Consequences of visiting restrictions during the COVID-19 pandemic: An integrative review. Int. J. Nurs. Stud. 2021, 121, 104000. [Google Scholar] [CrossRef]
- Munshi, L.; Evans, G.; Razak, F. The case for relaxing no-visitor policies in hospitals during the ongoing COVID-19 pandemic. Can. Med. Assoc. J. 2021, 193, E135–E137. [Google Scholar] [CrossRef] [PubMed]
- Rose, L.; Yu, L.; Casey, J.; Cook, A.; Metaxa, V.; Pattison, N.; Rafferty, A.M.; Ramsay, P.; Saha, S.; Xyrichis, A.; et al. Communication and virtual visiting for families of patients in intensive care during the COVID-19 pandemic: a UK national survey. Ann. Am. Thorac. Soc. 2021, 18, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Digby, R.; Manias, E.; Haines, K. J.; Orosz, J.; Ihle, J.; Bucknall, T.K. Family experiences and perceptions of intensive care unit care and communication during the COVID-19 pandemic. Aust Crit Car 2023, 36, 350–360. [Google Scholar] [CrossRef] [PubMed]
| Author(s) | Participants’ Relationship to victim; Country | Type of Study | Main Findings |
|---|---|---|---|
| Berntzen et al., 2023 [27] | 12 family members of COVID-19 infected patients. (Norway) |
Interview (Qualitative) |
Caring for COVID-19 patient and fear of worsening self-health. Charged with responsibility and feeling guilty. Perceived as not be able to be supportive due to visiting restrictions. Restrictive contact with affected patient. Yearning for day-day status on patient. Trying to cope to meet patients’ needs upon returning from treatment. Not feeling prepared or supported upon patient’s returning. |
| Forsberg et al., 2023 [28] | 14 family members of ICU COVID-19 patients. (Sweden) | Focus group (Qualitative) |
Not being aware of the severity of the illness. Restricted visits, allowable only at the end of treatment and/or patient’s life. Feeling of being unsupported and dealing with all issues by themselves. Indirect communication with ICU staff. Receiving information from ICU staff with little input from themselves. Dissemination of information to other family members. |
| Ghezeljeh et al., 2023 [29] |
12 family members of ICU COVID-19 patients. (Iran). | Interview (Qualitative) |
Lack of knowledge of health status, lack of contact with ICU staff, insufficient information on treatments/medications and inadequate information to assist patients upon discharge. Lack of adequate treatment facilities. Neglect of families from ICU staff. Neglecting to take care of needs of themselves. Feelings of being stigmatized. Anxiety, stress, fear of having a loved one in ICU. Witnessing the health struggles of loved ones. Feelings of perceived separation from loved ones. Blaming possible agents for causing illness. Anticipating worst-case scenarios (death). Responsibility of being a caregiver upon discharge. ICU staff helpful in navigating health issues. Importance of social and financial supports. |
| Onrust et al., 2023 [30] | 56 COVID-19 patients & 67 family members of COVID-19 patientsa. (Netherlands). |
Interview (Qualitative) onrus Questionnaire/Survey (Quantitative) |
Fear associated with possible death of loved one. Hope for loved one’s recovery. Lives contingent on loved one’s treatment. Need for reassurance from ICU staff. Expressed need for peace and solitude. ICU staff perceived as being helpful and caring to both patients and their families. Solace in expression (praying & lighting candles.) |
| Apostol-Nicodemus et al., (2022) [31] | 74 family members of COVID-19 infected patients. (Philippines) | Questionnaire/Survey (Quantitative) |
43% had anxiety upon two weeks of patient’s discharge, 24% had anxiety upon eight weeks of patient’s discharge. 16% had depression upon two weeks of patient’s discharge, 5% had depression upon eight weeks of patient’s discharge. 14% had mixed diagnosis (anxiety & depression) upon two weeks of patient’s discharge, 4% had mixed diagnosis upon eight weeks of patient’s discharge. 10% had moderate family dysfunction upon two weeks of patient’s discharge, 7% had moderate family dysfunction upon eight weeks of patient’s discharge. 10% had moderate family dysfunction upon two weeks of patient’s discharge, 7% had moderate family dysfunction upon eight weeks of patient’s discharge. Decreased economic resource inadequacy decreased upon eight weeks of patient’s discharge. At two weeks upon discharge, patient anxiety and inadequate family resources linked to anxiety. At eight weeks upon discharge, patient anxiety and low educational attainment linked to anxiety symptoms. At two weeks upon discharge, patient depression linked to depressive symptoms. |
| Galazzi et al., 2022 [32] | 56 family members of deceased ICU COVID-19 patients. (Italy) | Interview (Qualitative) Questionnaire/Survey (Quantitative) |
100% wished to see loved one in ICUs; Only 11% did. 50% made a video call with loved one. 96% who made a video call were content and would do it again. 93% who did not do a video call, regret not doing it. 45% could not hold funeral services by law. 38% used psychological support. Deceased patients’ offspring less likely to feel psychological distress than other familial relationships |
| Greenberg et al., 2022 [33] | 62 surrogates of ICU COVID-19 patients. (U.S.) | Interview (Qualitative) |
Difficulty in communication with ICU staff. Difficulty in communication with other family members. Difficulty in comprehending and tracking of medical information. Distress with visiting restrictions in ICUs. |
| Heesakkers et al., 2022 [34] | 166 family members (Iran) |
Questionnaire/Survey (Quantitative) |
Symptoms of anxiety/depression highest in the 3 months after loved ones’ hospital discharges. Symptoms of anxiety/depression higher in the 12 months after loved ones’ discharges. |
| Khaleghparast et al., 2022 [35] | 324 family member participants (Iran) |
Interview (Qualitative) Questionnaire/Survey (Quantitative) |
Anxiety linked to lack of knowledge of status of hospitalized loved one. Severe anxiety higher in spouses of diagnosed loved ones. Anxiety was higher in lower-income individuals and females. |
| Khubchandani et al., 2022 [36] | 2,797 Friends, family members, and acquaintances (US) |
Questionnaire/Survey (Quantitative) |
Knowing at least one family member or friend, being infected with COVID-19, or being hospitalized was more likely to increase the risk of anxiety/depression. |
| Jafari-Oori et al., 2022 [37] | 350 family caregivers of COVID-19 patients (Iran) | Questionnaire/Survey (Quantitative) |
Younger than 20, married, having a child, employed in healthcare, COVID-free, not exercising, taking anti-anxiety medications, poor sleep, having another illness, higher income associated with higher Depression/Anxiety/Stress scores (DAS) and increased Fears associated with COVID-19 (FSV-19). Being married, being employed in healthcare, having COVID-19, not exercising, having another illness, higher income, and being younger were predictors of high anxiety scores. Being married, being employed in healthcare, not exercising, poor sleep, higher income, and being younger were predictors of high stress scores. |
| Mawaddah et al., (2022) [38] | 10 family members of COVID-19 patients. (Indonesia) | Interview (Qualitative) |
Associated physical, economic, psychological, and social stigma burdens with caring for COVID-19 infected patient. Efforts to increase patient’s immune system, family preventive efforts towards COVID-19 transmission, and trying to find out information on patient’s health. Support from family and social support in caring for patient. Family adaption to COVID-19 protocols, developing closer family relations, and spiritual improvement. Encountered obstacles at home in care of patient. Hoping of no social stigma with disease, the pandemic ends soon, and no other families affected by disease. |
| Mejia et al., (2022) [39] | 3,292 college students, 2,789a of them knew someone who died or were diagnosed with COVID-19 (Various countries in Latin America) |
Questionnaire/Survey (Quantitative) |
Anxiety linked to friend dying, close relative and distant relative dying. Severe/moderate depression associated with age, class year, being from Honduras/Chile/Panama, close relative dying, COVID-19 at home, and the respondent being ill. Severe/moderate anxiety associated with gender, age, class year, being from certain countries, having a close relative, distant relative, or friend die, a family member either ill at home or away from home, friend ill or the respondent being ill. Severe/moderate stress associated with being male, age, class year, having a romantic partner, being from Honduras/Chile/Panama, close relative dying, distant relative dying, friend dying, having an ill relative at home, sick relative away from home, ill friend, or respondent being ill |
| Nohesara et al., 2022 [40] | 12 family members of deceased COVID-19 patients. (Iran). | Interview (Qualitative) |
Complex grieving processes with feelings of guilt and issues with emotional expression. New experiences associated with mourning. Developed more empathy for patients with COVID-19. Changing the meanings of death as a normal process of life. Increased need for support at work. |
| Robinson-Lane et al., (2022) [41] | 16 recently discharged ICU COVID-19 patients, and 16 family caregiversa (US) |
Interview (Qualitative) |
Taking on new responsibilities as caregivers. Managing mixed emotions (anxiety, grief, joy) with their loved ones recently discharged from ICU. Engaging in preventive infection control against new infections. Trying to address patient independence with patients’ perceived overbearing of caregiving. The need for continued medical/emotional support in caregiving. |
| Rostami et al., 2022., [42] | 236 family caregivers of COVID-19 patients. (Iran) |
Survey/Questionnaire (Quantitative) |
57% reported symptoms of depression. 70% reported symptoms of anxiety. 55% reported symptoms of stress. Female gender associated with greater levels of stress. Self-employment associated with greater levels of depression. |
| Bartoli et al., 2021 [43] | 14 family members of ICU COVID-19 patients. (Italy) | Interview/Questionnaire (Qualitative) |
Fear associated with course of disease and the unknowns. Fear associated with prior knowledge of ICUs. Fear associated with information about the disease stemming from the media. Feelings of trauma due to being away from loved one due to restrictions of ICUs. Perceived having life on pause in waiting for news of loved one from ICU staff. The realism that COVID-19 impacted their families. Feelings of guilt over loved one’s diagnosis. |
| Beck et al., 2021 [44] | 126 COVID-19 patients and 153a family members (Switzerland) | Interview (Quantitative) |
16% had symptoms of anxiety and 15% had symptoms of depression after 30-days discharge from hospital. Psychological distress associated with having children, not being employed, lower self-perceived overall health status, death of patient, use of psychotropic drugs, lower resilience, higher perceived stress, communicating through video calls or being able to visit the patient, higher perceived overall burden, increased worries about uncertain diagnosis and infection, higher burden of isolation measures and separation from patient, sport as coping strategy, relative was in contact with medical team, received information regarding prognosis, higher burden of not being able to visit patient, missing physical closeness, relative in quarantine, relationship with patient. |
| Borghi et al., 2021 [45] | 246 families of COVID-19 deceased victims. (Italy) | Interview (Qualitative) |
Due to social distancing protocols- coming up with alternative ways to hold funerals. Rationalizing that most victims were older-that they would have eventually died from something else. Lockdowns provided time and space to process loved ones’ deaths. Feeling helpless to not help others and themselves. Conveying the news of the loved ones’ deaths to others. |
| Chen et al., 2021 [46] | 10 family members of COVID-19 ICU patients. (US) |
Interview (Qualitative) |
Higher levels of stress or self-blame on diagnosis of family member diagnosis. Diagnosis associated with familial turmoil. Mixed views on video calls to ICU patient. Perceived poor closure to relationship after death. Needed information to treat and care for loved one. Frustration link of lack of access to knowledge of status. Appreciation of healthcare providers. |
| Jarial et al., 2021 [47] | 31 family members of COVID-19 patient treated in hospital, 34 family members with patient treated at home, and 35 family members with no COVID-19 patients. (India) | Questionnaire/Survey (Quantitative) |
Perceived stress was highest in family members having a loved one treated in the hospital. |
| Joaquim et al., 2021 [48] | 9,024 family members or friends of COVID-19 deceased victims. (Brazil) | Questionnaire/Survey (Quantitative) |
Having friends or family members who died linked to more psychological distress. Already suffering from mental health issues (depression, anxiety, psychotic) was associated with exacerbation of symptoms from having lost a friend or family member. |
| Kentish-Barnes et al., 2021 [49] | 19 family members of deceased ICU COVID-19 patients. (France) | Interview (Qualitative) |
Difficulty in communicating in-person and via telephone with ICU professionals. Communication problems with ICU professionals due to the problem of choice of words, pitch, or tone of conversations. Social distancing restrictions caused feelings of loneliness while loved ones were in the ICUs. Mixed emotions with ICU professionals relaying both positive and negative news. Witnessing the care in ICUs made it feel personable. Meeting ICU professionals established trust. Social distancing protocols made family members feel powerless. ICU professionals were viewed as the “go between” between loved one and family members. Visits helped the family members feel that they were supporting, caring, and providing closure. Social distancing protocols led to both missing the final moments and/or modifications to funeral procedures, ceremonies, and mourning. |
| Koçak et al., 2021 [50] | 2,047 who someone who had been ill or died from COVID and 1,240 those who did not. (Turkey) | Questionnaire/Survey (Quantitative) |
Anxiety, stress, and depression higher in those who had friends or loved ones having been diagnosed or died with COVID-19. Fear of COVID-19 is associated with anxiety, stress, and depression |
| Nakhae et al., 2021 [51] | 16 family caregivers of COVID-19 infected patients. (Iran) | Interview (Qualitative) |
Fear of death of loved one and the ambiguous nature of the disease. Caring difficulties and trying to provide best care. Quarantine issues (isolation) and social support. Technology (internet based) was both harmful and helpful. Distrust of hospital care, preference of caring at home. Home care led to long lasting positive experiences. |
| Orsini et al., 2021 [52] | 58 parents of COVID-19 infected children and 39 parents of non-COVID infected children. (Italy) | Questionnaire/Survey (Quantitative) |
Having children who tested COVID-19 positive, suffering economic hardships, been quarantined, and having a close relative who was diagnosed with COVID-19 were more likely to report moderate/severe anxiety. Having children who tested positive for COVID-19, suffering from economic hardships, and being quarantined were more likely to report moderate/severe depression. |
| Picardi et al., 2021 [53] | 8 participants- all but one were family members of COVID-19 hospitalized patients. (Italy) | Focus Group (Qualitative) |
Need to be constantly informed of the treatments/progress. Perceived as being non-effective or impotent. Reported difficulties with communication (phone, internet) with healthcare providers. Shared their day-to-day burdens (economic issues, lack of medical access) Psychological issues of having hospitalized family member (anxiety) |
| Prakash et al., 2021 [54] | 93 patients who had COVID-19 and 54 family members (India) | Questionnaire/Survey (Quantitative) |
17 (25%) of infected individuals reported some form of depression (mild, moderate, severe, extremely severe) vs. 22 (41%) of family members of infected individuals. 21 (31%) of infected individuals reported some form of anxiety (mild, moderate, severe) vs. 25 (46%) of family members of infected individuals. 9 (13%) of COVID-19 infected individuals reported some form of stress (mild, moderate, severe, extremely severe) vs. 16 (30%) of family members of infected individuals |
| Rahimi et al., 2021 [55] | 13 family caregivers of COVID-19 infected patients. (Iran) | Interview (Qualitative) |
Perceived difference in care for COVID-19 vs. other diseases. The unexpected reoccurring symptoms. Needs of caregivers not met. Need information to treat/care for loved one. Lack of access to healthcare services. Financial problems with caretaking. Unpleasant social, physical, and psychological experiences with care Spirituality/social support strengthen resolves. Coping methods for used for stress. Caregiving led to some positive experiences and sense of self-growth. |
| Selman et al., 2021 [56] | Twitter data was gathered. 196 tweets from 192 from friends and family members of deceased COVID-19 patients. (Various countries) | Tweets-Technology Qualitative Study |
Tweeted about social restrictions limiting ability to visit places of care. Tweets about family members dying alone or without a proper farewell. Tweets about the emotional impacts of having family member severely affected by COVID-19 (e.g., government response to virus, perceived public apathy). Tweets about lack of social support after the death of loved ones or funerals not held as the victim would have wished. Tweets about the importance and support of PPE usage, social distancing, and hygienic practices. |
| van Veenendaal et al., 2021 [57] | 50 COVID-19 patients and 67 family members of COVID-19 patientsa (Netherlands) |
Questionnaire/Survey (Quantitative) |
Showed good physical functioning. 64% went back to work after six months of ICU discharge. Showed good psychological functioning after three and six months after victim’s ICU discharge. 63% reported impaired well-being from the mandatory physical distance from the victim while in the ICU. |
| Xu et al., 2021 [58] | 1,274 non-COVID social contacts and 173 social contacts of COVID-19 patientsa (China). | Questionnaire/Survey | Social contacts of COVID-19 patients were more likely to have anxiety symptoms, depressive symptoms, suicidal ideations/thoughts, PTSD symptoms, somatic symptoms, poorer meaning in life, loneliness, lower HRQOL, more COVID-19 related symptoms, and lower satisfaction with life. Social contacts of COVID-19 patients were more likely to have different perceptions about the epidemic (more worries about infection) higher perceived risk of being infected and longer perceived time for successful epidemic control, paid more to prevent infections, to have visits to a doctor in the past four weeks, and reported lower perceived self-efficacy. |
| Zhao et al., 2021 [59] | 1290 had no close contact with COVID-19 patients and 1169 had close contact with a COVID-19 patienta. (China) |
Questionnaire/Survey (Quantitative) |
Close contact participants who were more likely to report severe depression and fatigue. Close contact participants were more likely to suffer from depression and fatigue if they were younger, had economic issues due to the pandemic, perception of poor or fair health. Close contact participants were likely to suffer from fatigue with they frequently used mass media. |
| Mirzaei et al., 2020 [60] | 210 family caregivers of both inpatient and outpatient COVID-19 patients. (Iran) | Questionnaire/Survey (Quantitative) |
Male caregivers more likely to suffer from objective, subjective, objective-subjective burdens. No difference in the mean scores of the total caregiver burden by gender. |
| Mohammadi et al., 2020 [61] | 16 family members of deceased COVID-19 victims. (Iran) |
Interviews (Qualitative) |
Intense emotional shock from losing loved one. Perceived guilt and fear of transmitting disease to loved one. Lack of proper closure due to sudden death. Lack of proper burial or unreligious burial due to social restrictions Fear of the future due to family instability caused by death of loved one. Feeling of stigmatization by society due to loved one dying. |
| Rizvi Jafree et al., [62] | 20 family members of hospitalized COVID-19 patients. (Pakistan) |
Interviews (Qualitative) |
Social stigmas: Police intimidation, maltreatment by hospital staff, false test results used as revenge, blame/rejection by others, physicians facing stigma from other physicians, discrimination at work, shift locality, and difficulty commuting for necessities due to maltreatment. Struggles: Social distancing, inadequate knowledge of disease, having to replace mothers for care of children, depression and sleeping problems, troubles adjusting to the post-COVID world, and anxiety for children. Strengths: Praying and patience, spirituality, support and assistance from daughters, thankful for what one has, doing household activities never done before, planning a healthy future, using the media as a source of awareness and learning, and exercise. |
| Tanoue et al., 2020 [63] | 16,402 participantsb (Japan) |
Questionnaire/Survey (Quantitative) |
Higher rates of stress associated with family member being diagnosed. |
| Category | Studies |
|---|---|
| Psychosocial feelings: Anxiety, stress, distress, fear associated with COVID-19 infected loved one. | Ghezeljeh et al., 2023; Apostol-Nicodemus et al., 2022; Galazzi et al., 2022; Heesakkers et al., 2022; Khaleghparast et al., 2022.; Khubchandani et al., 2022; Jafari-Oori et al., 2022; Mejia et al., 2022; Robinson-Lane et al., 2022; Rostami et al., 2022; Beck et al., 2021.; Chen et al., 2021; Jarial et al., 2021; Joaquim et al., 2021; Koçak et al., 2021; Orsini et al., 2021; Picardi et al., 2021; Prakash et al., 2021; Rahimi et al., 2021; van Veenendaal et al., 2021; Xu et al., 2021; Zhao et al., 2021; Rizvi Jafree et al., 2020; Tanoue et al., 2020. |
| Perceived Issues with healthcare system(s): Wanting more information on loved one or how to properly care upon discharge. Lack of clear communication. Lack of follow-up care upon returns. Not knowing severity of illness. | Berntzen et al., 2023; Forsberg et al., 2023; Ghezeljeh et al., 2023; Onrust et al., 2023; Greenberg et al., 2022; Robinson-Lane et al., 2022; Bartoli et al., 2022.; Chen et al., 2021; Kentish-Barnes et al., 2021; Nakhae et al., 2021.; Picardi et al., 2021; Rahimi et al., 2021; Rizvi Jafree et al., 2020. |
| Importance of support: Social, emotional, financial support in having a COVID-19 loved one or taking care of one. | Berntzen et al., 2023; Forsberg et al., 2023; Ghezeljeh et al., 2023; Apostol-Nicodemus et al., 2022; Galazzi et al., 2022; Mawaddah et al., 2022; Nohesara et al., 2022; Robinson-Lane et al., 2022; Picardi et al., 2021; Rahimi et al., 2021.; Selman et al., 2021. |
| Responsibility/caring for COVID-19 patient: Being responsible for taking care of COVID-19 patient or overseeing the family due to the absence of patient. Feeling unprepared. | Berntzen et al., 2023; Forsberg et al., 2023; Ghezeljeh et al., 2023; Mawaddah et al., 2022; Robinson-Lane et al., 2022; Chen et al., 2021; Nakhae et al., 2021; Picardi et al., 2021; Rahimi et al., 2021; Mirzaei et al., 2020; Rizvi Jafree et al., 2020. |
| Visiting restrictions & isolation: Issues with restrictions to visiting patients in healthcare facilities. Feelings of isolation from infected loved one and society. | Berntzen et al., 2023; Forsberg et al., 2023; Ghezeljeh et al., 2023; Galazzi et al., 2022; Greenberg et al., 2022; Kentish-Barnes et al. 2021; Nakhae et al., 2021; Selman et al., 2021. |
| Guilt feelings or emotional impact: Feelings of guilt or emotional distress of having a loved one with COVID-19. | Berntzen et al., 2023; Nohesara et al., 2022; Robinson-Lane et al., 2022; Bartoli et al., 2021; Chen et al., 2021; Selman et al., 2021; Mohammadi et al., 2020. |
| Funeral services or mourning restrictions: Due to COVID-19 protocols, funeral or other mourning practices were modified or restricted. | Galazzi et al., 2022; Nohesara et al., 2022; Borghi et al., 2021; Kentish-Barnes et al., 2021; Mohammadi et al., 2020. |
| Needing peace and solitude: Alone time. Meditation time. Spirituality. | Onrust et al., 2023; Mawaddah et al., 2022; Borghi et al., 2021; Rahimi et al., 2021; Rizvi Jafree et al., 2020. |
| Worrying about self or others/Neglect: Worrying over family health, neglecting care for self or others. | Berntzen et al., 2023; Ghezeljeh et al., 2023; Robinson-Lane et al., 2022; Borghi et al., 2021; Rahimi et al., 2021. |
| Feelings of stigma: Being or feeling stigmatized for having a COVID-19 infected patient. | Ghezeljeh et al., 2023; Mawaddah et al., 2022; Mohammadi et al., 2020; Rizvi Jafree et al., 2020. |
| Category | Studies |
| Healthcare system being helpful: The healthcare system was perceived to have assisted in several ways. | Ghezeljeh et al., 2023; Onrust et al., 2023; Chen et al., 2021; Kentish-Barnes et al., 2021. |
| Media: How the media (e.g., social, print, TV) either is perceived helpful or harmful on covering or reporting information on COVID-19. | Robinson-Lane et al., 2022; Bartoli et al., 2021; Nakhae et al., 2021; Rizvi Jafree et al., 2020 |
| Being the point of contact: Having to contact other members of family about patient’s health or difficulty in contacting them. | Forsberg et al., 2023; Galazzi et al., 2022; Borghi et al., 2021. |
| Fear of death of or grief of losing a COVID-19 infected loved one. | Onrust et al., 2023; Nakhae et al., 2021; Mohammadi et al., 2020. |
| Perceived inadequate closure at end of life: Not having the proper farewell with victim. | Chen et al., 2021; Selman et al., 2021; Mohammadi et al., 2020. |
| PPE and other safety measures: The Importance of using personal protective equipment and social distancing. | Mawaddahi et al., 2022; Robinson-Lane et al., 2022; Selman et al., 2021. |
| Types of Study |
| Quantitative= 17 Studies Qualitative= 17 studiesMixed= 3 studies |
| Most Common Type of Quantitative Study |
| Questionnaire/Survey =17 |
| Most Common Type of Qualitative Study |
| Interview= 14 |
| The Top Three Countries with the Most Studies |
| Iran= 10 |
| Italy= 5 |
| United States= 4 |
| Number of Participants in the Study Populations |
| 1-100=19 |
| 101-1,000=11 |
| 1,001+=7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





