1. Introduction
Recently, pigtail catheter insertion is the preferred alternative minimally invasive treatment over the conventional large-bore chest tubes for pleural effusion drainage [
1,
2,
3]. Placing a large-bore chest tube is relatively invasive, with potential morbidities and complications [
4]. Pigtail catheters have a smaller profile, with more flexible materials causing lesser pain and injury to surrounding tissues [
5]. Fewer complications of pigtail catheters were documented in cases of simple pleural effusions compared to chest tubes [
6]. Furthermore, additional treatment, such as pleurodesis or fibrinolysis, can be performed using the pre-existing catheters [
7].
Maintaining the proper position of an indwelling catheter is important for efficient drainage. Inserted catheters can be unintentionally pulled out. Nevertheless, catheters can be securely fixated onto the skin by thoroughly educating the patients. An improper position can compromise catheter function and, occasionally, dislodge catheters completely.
To overcome these drawbacks, the novel double-pigtail catheter (DPC), which has additional pigtail coiling in the middle of the catheter, was introduced. The aim of the present study was to compare the complication and clinical success rates of conventional single-pigtail catheters (SPCs) without multiple side holes, SPCs with multiple side holes (SPC+M), and DPCs for pleural effusion drainage.
2. Materials and Methods
2.1. Study population
The requirement of obtaining informed consent from participants was waived owing to the retrospective study design. The study protocol was approved by the Institutional Review Board of Gangneung Asan Hospital (approval no.: GNAH 2020-12-006). Between July 2018 and December 2019, we retrospectively reviewed all consecutive drainage procedures for initially unloculated pleural effusion of varying etiology. Shifting pleural fluid collection was verified in the decubitus view of simple chest radiographs as baseline examination for all patients. A total of 382 pleural drainage procedures were performed in 343 patients.
Table 1 presents the baseline characteristics.
2.2. Types of percutaneous drainage pigtail catheter
Pigtail catheters available for pleural drainage were: 1) SPC: Dawson–Mueller Drainage Catheter, made of ultrathane, with a hydrophilic coated distal segment (5 cm, five side holes with pigtail formation of 10 mm), and Mac–Loc for the suture fixation system (25 cm in delivery length and 0.038” inner diameter; Cook, Bloomington, IN, USA); 2) SPC+M: Biliary Drainage Catheter, made of ultrathane, with a hydrophilic coated distal segment (12 cm, nine side holes with pigtail formation) and side-port segment (8 cm, 22 side holes), and Mac–Loc for the suture fixation system (40 cm in delivery length, 0.038” in the inner diameter; Cook, Bloomington, IN, USA); 3) DPC: Multi-purpose Drainage Catheter, made of polyurethane, double-loop pigtail, and a suture fixation system, with a total of 21 side holes (5 for each pigtail and 11 side-port segments), pigtail loop size of 2 cm with 7-cm intervals, delivery length of 30 cm, and 0.038” in the inner diameter (Sungwon Medical, Cheongju, North Chungcheong Province, Korea;
Figure 1a,b).
2.3. Procedure details
All procedures were performed by one intervention radiologist (BLINDED-FOR-REVIEW) in the intervention radiology suite with the patients in the supine position. Vital signs were monitored throughout the procedure. Combined fluoroscopy and ultrasound were used to guide the drainage catheter placement using the Seldinger technique as follows: 1) After sterilizing the skin, hypoechoic fluid collection was confirmed on ultrasonography in the intercostal space of the lower ribs, approximately at the level of the mid-axillary line. 2) For local anesthesia, 2% lidocaine was administered at the puncture site, and the location of the needle (21G Chiba needle) was continuously verified using an ultrasound probe, with the needle “walking over” the upper edge of the rib to avoid intercostal neurovascular bundles. 3) After puncturing the pleura, a metallic hair wire with a floppy tip (0.018”) was inserted through the needle, and the 6-Fr dilator sheath was inserted (3S-Percutaneous access kit, Dukwoo Medical, Hwaseong, Gyeonggi, Korea). 4) Through the sheath, a 0.035” hydrophilic guide wire (Radifocus, Terumo, Tokyo, Japan) was inserted. 5) Under fluoroscopic guidance, 10.2-Fr pigtail catheters were inserted over the guidewire, and the catheter tip was located at the T6–8 level, presumed to be the most dependent portion of fluid collection in the supine position. 6) The same anchoring technique was applied in all patients by one interventional radiologist (number of knots: five; one loop of thread around the tubing between the knots of 2-0 black silk).
2.4. Technical and clinical success and complications
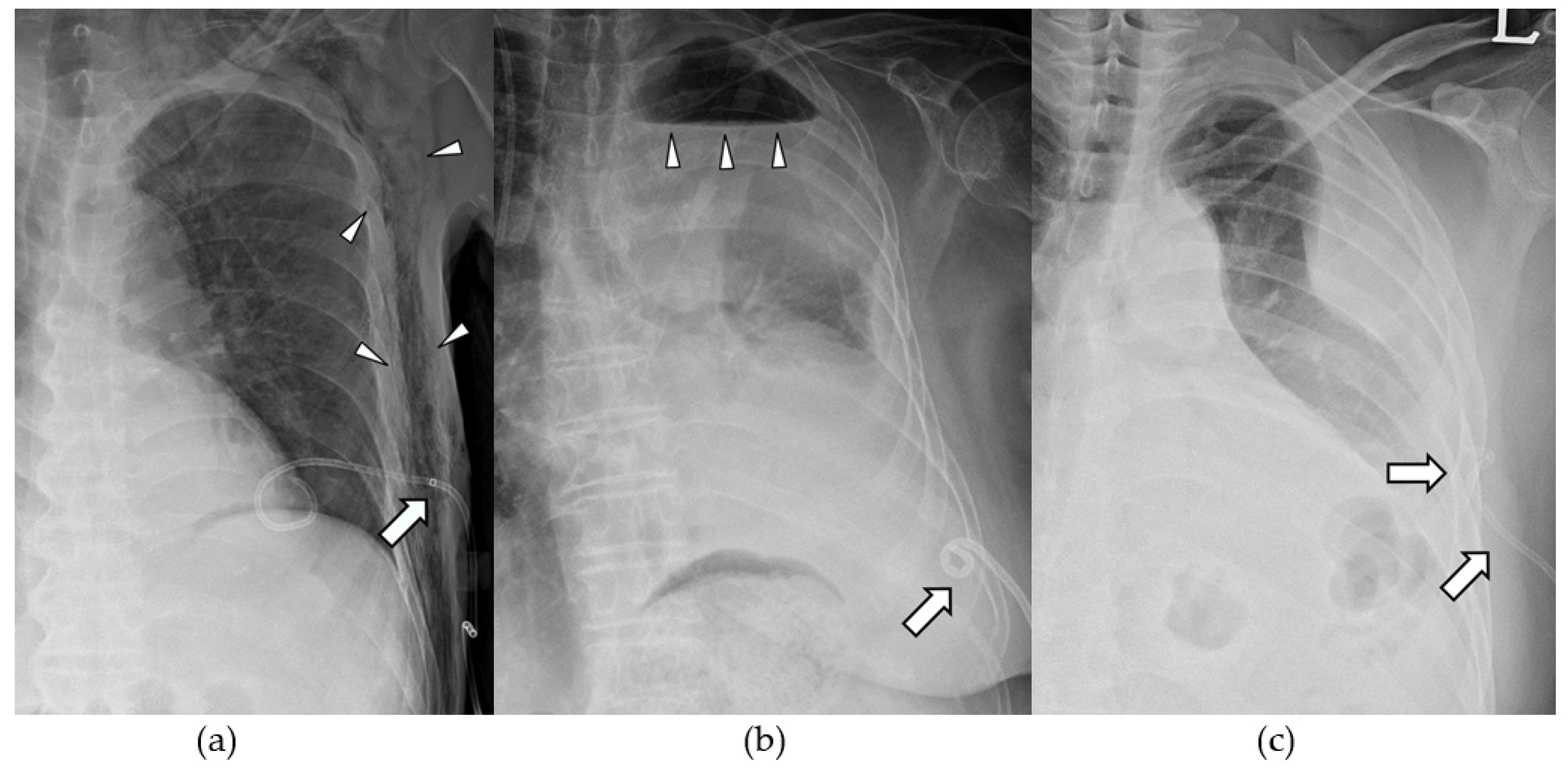
Technical success was defined as smooth drainage immediately after successful installation of the catheter in the thoracic cavity with pleural effusion. Clinical success was defined as improvement in pleural effusion on follow-up simple chest radiography within 3 days without additional procedures. Indwelling time was defined as the catheterization period, and when the catheter was removed or changed because of complications, it was treated as censored data. Major complications included dysfunctional retraction, complete dislodgement, and blockage. Dysfunctional retraction was defined as outward pulling of the distal pigtail loop of the catheter without leaving the pleural cavity, causing a dysfunction in drainage and replacement of the catheter (
Figure 2a,b). Complete dislodgement was defined as dislocation of the catheter end outside the pleural cavity where drainage fluid is located (
Figure 2c). Blockage was defined as rapid decrease in the amount of daily drainage with a significant amount of pleural effusion remaining on simple chest radiographs. Other complications, such as atraumatic pneumothorax (
Figure 2B), hemorrhage, and subcutaneous emphysema (
Figure 2a) were recorded for each catheter during the indwelling time.
2.5. Statistical analysis
Complications were compared among catheters using the chi-square and Fisher’s exact tests. A survival analysis was used for calculating the indwelling time. Statistical analyses were performed using SPSS version 25.0 (IBM, Armonk, NY, USA), and p-values < 0.05 were considered to indicate statistical significance.
3. Results
Demographic data did not differ significantly among the groups (
Table 1). All procedures were technically successful without immediate complications, The clinical success rate of SPC, SPC+M and DPC groups were 83.7%, 81.2% and 90.1%, respectively, showing significant differences (p=0.029).
Regarding complications, the rates of dysfunctional retraction in the DPC, SPC+M, and SPC groups were 4.5%, 15.5%, and 23.6%, respectively (p < 0.001), showing significant differences (
Table 2).
There were three cases of complete dislodgement in the entire study population: two in the SPC group and and one in the SPC+M group. One SPC+M catheter was continuously retracted (
Figure 2a) and eventually completely dislodged from the pleural cavity. In the other two cases, patients unconsciously pulled out their catheters at night, and the catheters were missing on follow-up radiographs. However, complete dislodgement did not occur in the DPC group.
The frequencies of blockage in the SPC+M, DPC, and SPC groups were nine (8.2%), eight (5.1%), and four (3.4%), showing no statistical significance.
As for other complications, atraumatic pneumothorax was the most common (n = 16: six in the SPC group, five in the SPC+M group, and five in the DPC group). Chest wall hemorrhage (n = 1) and subcutaneous emphysema (n = 1) were also detected in the SPC+M group (
Table 2).
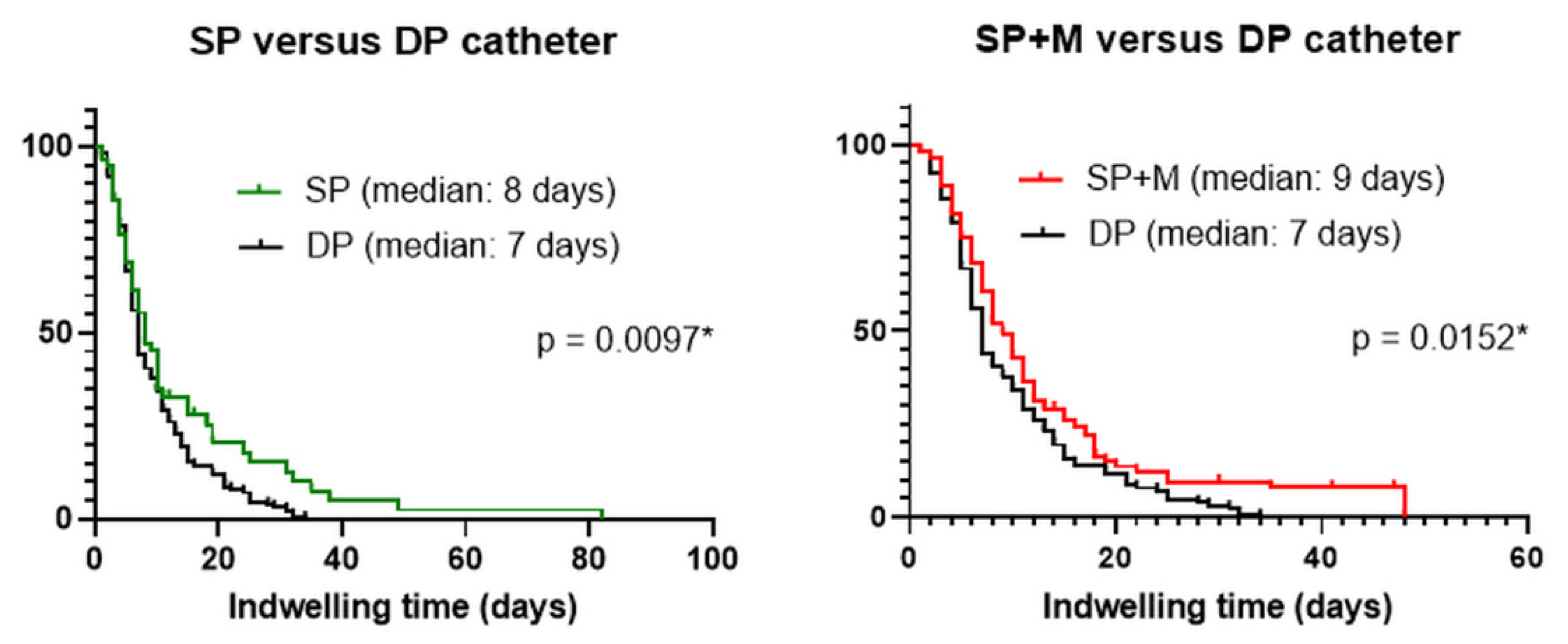
In the survival analysis, the estimated indwelling times were eight (95% confidence interval [CI]: 7.3–10.7), nine (95% CI: 6.6–9.4), and seven (95% CI: 6.3–7.7) days for SPC, SPC+M, and DPC, respectively, with DPC showing a significant difference (p < 0.05) (
Figure 3a,b).
4. Discussion
Dysfunctional retraction and complete dislodgement are relatively common complications following percutaneously inserted drainage procedures [
8]. The rates of these complications following pleural drainage procedures have been rarely reported [
1,
5,
6]. The drainage catheters may become malpositioned or gradually pull away because of respiratory motion or inappropriate management, including physical traction. Maintaining their optimal position is crucial to keep efficient draining capability during the indwelling period [
9]. It can decrease patient discomfort and reduce associated medical costs. To place the side holes of a catheter into the intended space, additional pigtail coiling was formed at the mid-shaft of the drainage pigtail catheter. These catheters’ performances in preventing retraction or dislodgement were not studied before.
Dysfunctional retraction was most frequently noted in the SPC+M group, followed by SPC and DPC groups. In cases of SPC+M, dysfunction of the catheter was more likely to occur when some of the side holes at the mid-shaft were pulled outside the pleural cavity (
Figure 2a). These pulled-out side-holes can be blocked inside the chest wall and cause dysfunction resulting in replacement. SPC can become dysfunctional when the pigtail loop is fully retracted and hangs onto the parietal pleura (
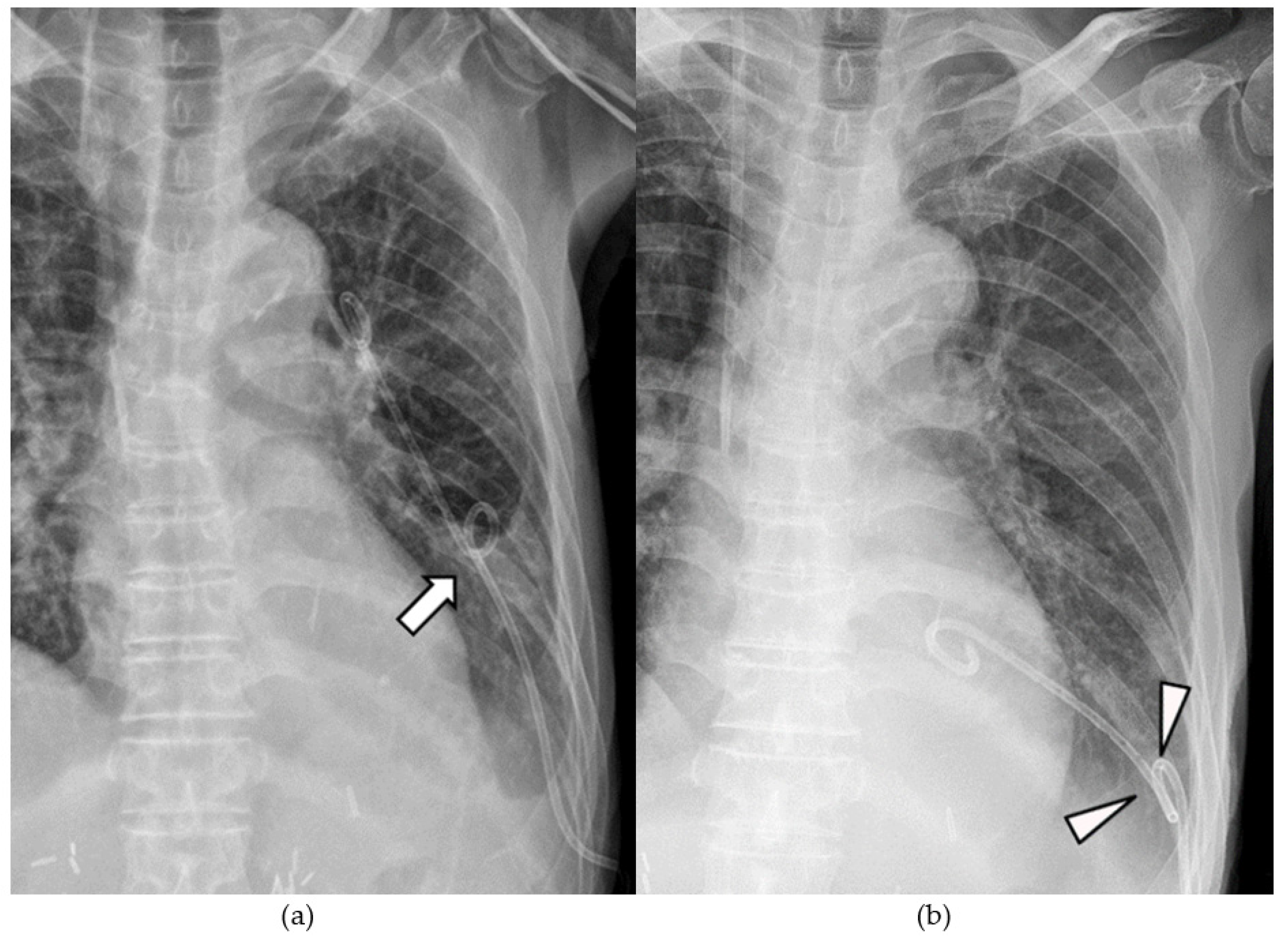
Figure 2b). In contrast, when unintended traction occurred in DPC, additional pigtail coiling at the mid-shaft of the catheter prevented further retraction. The function of DPC was preserved by limiting the range of retraction (
Figure 4a, b). Furthermore, complete dislodgement of DPC did not occur.
Pneumothorax occurred with all three types of catheters, possibly associated with intrapleural negative pressure during inspiration. It mostly occurred in the indwelling period and could be managed if the dysfunction of the catheter had not occurred. In addition, in the case of SPC+M, subcutaneous emphysema occurred. This may be because some side holes were located in the subcutaneous tissue of the chest wall with continuous intrapleural negative pressure (
Figure 2a). Since subcutaneous emphysema caused great discomfort to the patient, it is regarded as a major complication.
Effective drainage would be achieved if more side holes are well-placed in the intended position. However, paradoxically, some debris would get stuck in the side hole, which impairs catheter patency. When replacing or removing the catheter, in the case of SPC+M, a lot of debris was stuck in the multiple side holes of the linear shaft, presumed to cause blockage of the passage. Side holes inside the pigtail loop were presumed to be less vulnerable to blockage because they were faced in the centripetal direction inside the loop. Catheters with multiple side holes (SPC+M and DPC) showed a higher blockage rate compared to SPC. In addition, SPC+M showed a higher blockage rate compared to DPC, as SPC+M had more side holes on the shaft (22 vs. 11). However, these findings failed to demonstrate statistical significance.
The clinical success rates of these three types of catheter are comparable to those in a previously published study [
10]. As mentioned earlier, the SPC+M group showed the lowest clinical success rate among all types of catheters. This may be because SPC+M was more vulnerable to both retraction and blockage. DPC resisted dysfunctional retraction compared to other types of catheters and showed a comparable blockage rate as SPC.
DPC showed a significantly shorter indwelling time than other types of catheters. Longer proper positioning of the catheter seemed to decrease indwelling time. This can shorten the length of hospital stay and reduce medical costs.
This study has some limitations. First, this study had a retrospective design. Second, randomization was not performed in the catheter type selection. However, the number of procedures did not differ significantly among the three groups. Third, the amount or nature of the patients’ pleural effusion (viscosity, turbidity, amount of debris) was not constant. However, all procedures were performed by one interventional radiologist; therefore, only one anchoring technique was used. As the method of fixing the catheter to the skin was unified, comparing dysfunctional retraction or complete dislodgement under the same conditions was possible.
5. Conclusions
DPC had a lower dysfunctional retraction rate compared to the other conventional pleural drainage catheters because it limited the range of retraction. It also had a higher clinical success rate compared to SPC+M. Furthermore, it was efficient, with a shorter indwelling time, possibly resulting in shortened hospital stay and reduced costs.
Author Contributions
Conceptualization, Y.C. and J.S.; methodology, J.S.; formal analysis, J.S.; data curation, Y.C.; writing—original draft preparation, Y.C., H.N.L.; writing—review and editing, H.N.L., J.H.S., S.L., S.P.; supervision, J.S., J.H.S.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Gangneung Asan Hospital (IRB No.: GNAH 2020-12-006, date of approval 5 January 2021).
Informed Consent Statement
The requirement for informed consent was waived owing to the retrospective nature of this study.
Data Availability Statement
The dataset generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mehra, S.; Heraganahally, S.; Sajkov, D.; Morton, S.; Bowden, J. The effectiveness of small-bore intercostal catheters versus large-bore chest tubes in the management of pleural disease with the systematic review of literature. Lung India 2020, 37, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Fuhrman, B.P.; Landrum, B.G.; Ferrara, T.B.; Steinhorn, D.M.; Connell, A.P.; Smith-Wright, D.L.; Green, T.P. Pleural drainage using modified pigtail catheters. Crit. Care Med. 1986, 14, 575–576. [Google Scholar] [CrossRef] [PubMed]
- Lawless, S.; Orr, R.; Killian, A.; Egar, M.; Fuhrman, B. New pigtail catheter for pleural drainage in pediatric patients. Crit. Care Med. 1989, 17, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.S.; Bratton, S.L.; Brogan, T.V. Efficacy and Complications of Percutaneous Pigtail Catheters for Thoracostomy in Pediatric Patients. Chest 1998, 114, 1116–1121. [Google Scholar] [CrossRef] [PubMed]
- Gammie, J.S.; Banks, M.C.; Fuhrman, C.R.; Pham, S.M.; Griffith, B.P.; Keenan, R.J.; Luketich, J.D. The Pigtail Catheter for Pleural Drainage: A Less Invasive Alternative to Tube Thoracostomy. Journal of the Society of Laparoendoscopic Surgeons 1999, 3, 57–61. [Google Scholar] [PubMed]
- Elsayed, A.; Alkhalifa, R.; Alodayni, M.; Alanazi, R.; Alkhelaiwy, L.; Zalah, M.; Alnaeli, G.; Alorabi, T.; Al-Qarni, M.; Al-Otaibi, S. Implication of pigtail catheter vs chest tube drainage. Int. J. Community Med. Public Heal. 2018, 5, 3686. [Google Scholar] [CrossRef]
- Ghoneim, A.H.; Elkomy, H.A.; Elshora, A.E.; Mehrez, M. Usefulness of pigtail catheter in pleurodesis of malignant pleural effusion. Egypt. J. Chest Dis. Tuberc. 2014, 63, 107–112. [Google Scholar] [CrossRef]
- Saqib, A.; Ibrahim, U.; Maroun, R. An unusual complication of pigtail catheter insertion. J. Thorac. Dis. 2018, 10, 5964–5967. [Google Scholar] [CrossRef] [PubMed]
- Maher, M.M.; Kealey, S.; McNamara, A.; O’laoide, R.; Gibney, R.G.; Malone, D.E. Management of Visceral Interventional Radiology Catheters: A Troubleshooting Guide for Interventional Radiologists. RadioGraphics 2002, 22, 305–322. [Google Scholar] [CrossRef] [PubMed]
- Bediwy, A.S.; Amer, H.G. Pigtail Catheter Use for Draining Pleural Effusions of Various Etiologies. ISRN Pulmonol. 2012, 2012, 1–6. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).