1. Introduction
In Europe, emerging new gene and cell therapies have led to the creation of laws that regulate the products commonly known as advanced therapy medicinal products (ATMPs). The ATMPs are divided into four types:
Cell therapy medicinal products (CTMPs). Products that contain manipulated cells or tissues that are intended to be used for the different essential functions in the recipient, compared to the one they had in the donor.
Tissue-engineered products (TEPs). Engineered cells or tissues that can regenerate, repair, or replace human tissue.
Gene therapy medicinal products (GTMPs). Products directly related to diagnostic, therapeutic, or prophylactic effects that use specific recombinant nucleic acids.
Combined ATMPs (cATMPs). Integrate two or more of the products listed above [
1].
However, each regulatory agency around the world has its own product classification. Some of the regulatory agencies around the world are the European Medicines Agency (EMA) in Europe, the Food Drug Administration (FDA) in the United States of America (USA), the Ministry of Food and Drug Safety (MFDS) in South Korea, the Drug Controller General of India (DCGI) in India, the Therapeutic Goods Administration (TGA) in Australia, and the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan.
The CTMP therapies use mostly what originally were baptized as mesenchymal stem cells (commonly referred to as MSCs) and later attempted to be changed for medicinal signaling cells, and more recently for mesenchymal progenitors (Arnold I. Caplan, personal communication 2022). For convenience, the term MSCs will be used here [
2,
3,
4].
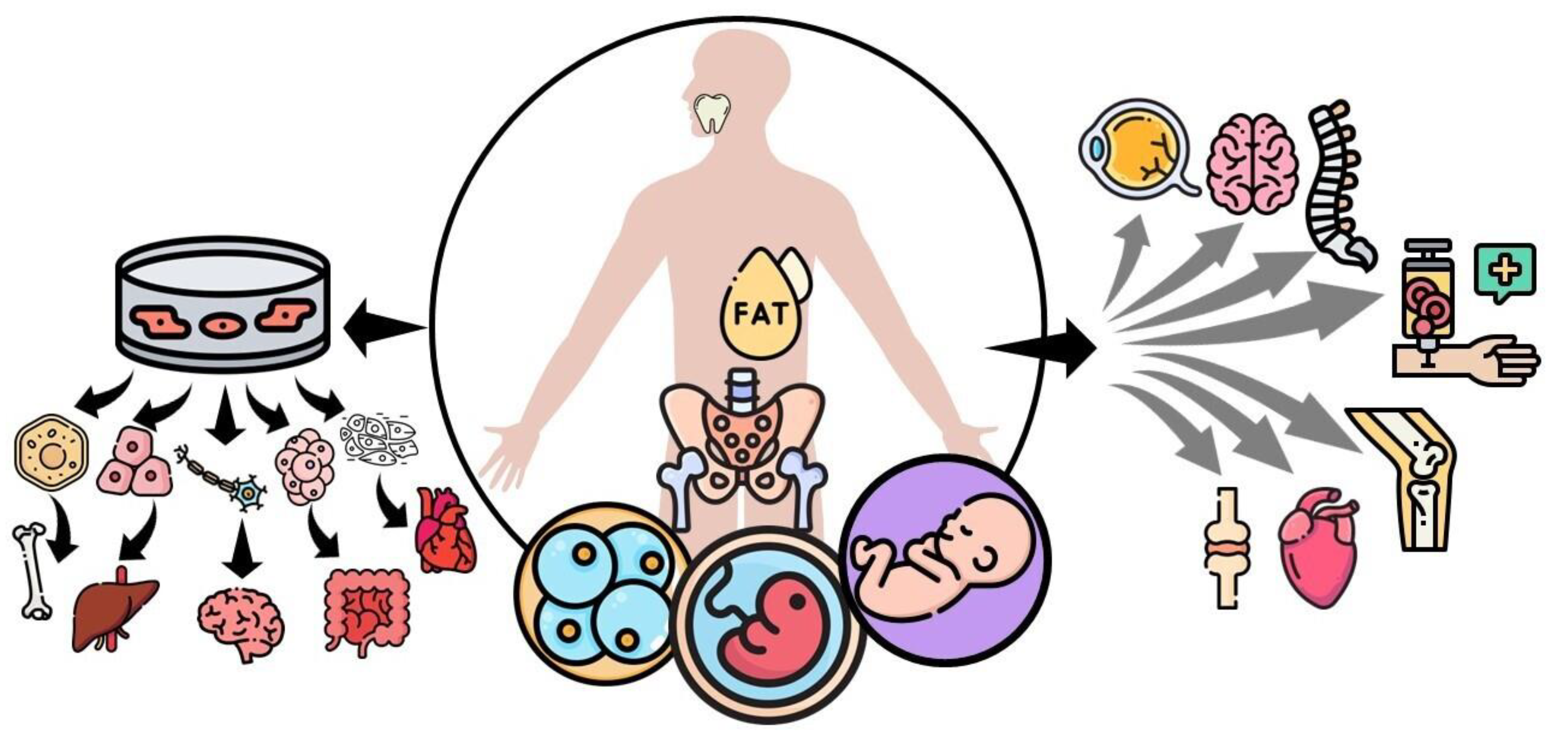
Going back to the basics, stem cells, in general, can be classified based on their differentiation capacity including totipotent, pluripotent, multipotent, and unipotent. The
totipotent stem cells have the potential to differentiate into any type of cell found in an organism, which is the case of the zygote. The
pluripotent stem cells have the potential to give rise to all the cells included in the mesoderm, endoderm, and ectoderm layers. Then these cells give rise to different types of specialized cells in the body becoming multipotent.
Multipotent stem cells can produce a variety of cells limited to the germinal layer of origin, which is the case of the MSCs, that have the potential to become muscle, bone, and cartilage, all derived from the mesoderm. Lastly, the
unipotent stem cells can create only one lineage of cells, for example, those of muscle or skin can only give rise to muscle or skin cells, respectively [
5]. In turn, stem cells can be classified based on the developmental stage in which they can be extracted, such as embryonic, fetal, infant, or adult stem cells [
5]. Embryonic stem cells are derived from the inner cells of a blastocyst, are highly undifferentiated and highly proliferative, and can comprise totipotent and pluripotent stem cells. Fetal stem cells, which include MSCs and as the name implies, can be isolated from fetal tissues such as blood, bone marrow (BM), liver, and kidney. Infant MSCs include those extracted from the cord blood, amnion, or placenta. Then, the adult MSCs comprise those isolated from adipose tissue, BM, peripheral blood, and tooth pulp [
6] (
Figure 1).
Recently, we carried out a systematic review with the aim of analyzing the different applications that MSCs have had in the different registered clinical trials around the world [
7]. Now, in this narrative review, we will synthesize the information about current MSCs therapies approved by regulatory agencies, communicate the problems that these therapies usually face, and propose solutions to overcome these problems.
2. Mesenchymal stem cells
As mentioned above, the terms medicinal signaling cells and mesenchymal progenitors have begun to be used by experts in the field with the intention of replacing previous names used to refer to MSCs [
2,
3,
4]. Nevertheless, we are going to use the latter to avoid confusion. MSCs come from cells derived from the embryonic mesoderm and they are capable of self-renewal, and under appropriate stimulation, of differentiating into various tissues types
in vitro, including bone, cartilage, muscle, BM stroma, tendon/ligament, fat, and dermis [
8,
9,
10]. On the other hand, MSCs
in vivo (or
in physio, referring to what occurs inside the body) originate as perivascular cells and do not differentiate into other cell types to repair damaged tissue, but rather, they detach from the blood vessels of the damaged tissues to generate a regenerative microenvironment through their immunomodulatory secretions and trophic bioactive factors, inducing other cells (stem cells from the damaged tissue) to regenerate the tissue [
11,
12,
13]. It was precisely for this property that they were proposed to be renamed Medicinal Signaling Cells [
4].
Adult bone marrow MSCs (BM-MSCs) are the most widely used in clinical trials; however, the MSCs from birth-associated tissues may have additional biological properties, such as high proliferative capacity, longer life span, and greater differentiation potential [
14]. Depending on their origin, these cells exhibit different immunophenotypes that explain some of the variations in their responses. Adult MSCs positively express CD44, CD90, CD105 (SH2), and CD166, and negatively express CD14, CD34, and CD45 [
15]. Birth-associated MSCs express more primitive surface markers. On the other hand, MSCs from amnion and umbilical cord MSCs lack the ability to conduct
in vitro adipogenic differentiation, while those from placenta and umbilical cord express genes for hematopoietic growth factors that give them the ability to develop into hematopoietic progenitor cells [
7].
MSCs can be administered from autologous or allogeneic sources [
7]. BM-MSCs are isolated from the BM extracted from the iliac crest, femur, or tibia. Isolation of MSCs from the BM can be performed by density gradient centrifugation or direct plating. The density gradient centrifugation method involves the use of gradient density solutions with low viscosity and low osmotic pressure that allows the separation of the different types of cells depending on their density. On the other hand, in the direct plating method, cells are seeded into a low-density culture dish, approximately 10³ to 10⁶ cells/cm², separated by adhesin, and finally subjected to expansion. The MSCs expanded in culture do not lose their differentiation potential, although their lifespan is limited to 15-50 population doublings [
8,
16]. MSCs from adipose tissue (AT-MSCs) are isolated from liposuction or lipectomy samples (visceral or subcutaneous adipose tissue from the abdomen, brachium, femoral, or gluteal areas). AT-MSCs isolation typically involves enzymatic digestion of adipose tissue samples by collagenases, followed by the removal of red blood cells (RBC) with a specific RBC lysis procedure, and filtration of the cells [
8]. MSCs from neonatal tissues can be isolated from the entire umbilical cord, including the connective tissue, the Wharton’s jelly, and the blood vessels. The cell biology methods used to isolate MSCs from the umbilical cord vary depending on which compartment of the umbilical cord is selected as the source. Typically, these methods may include enzymatic digestion of umbilical-cord tissue samples, RBC-specific lysis, cell filtration, and/or density gradient separation. The isolation/expansion procedure is similar for adult and neonatal MSCs [
8].
3. Clinical applications of MSCs
We performed a systematic review that reported that up until June 2020, there were 903 registered clinical trials at
clinicaltrials.gov using MSCs as treatments, which had complete information about their objective and current phase. The medical specialties with the largest number or registered clinical trials were orthopedics, pneumology, neurology, cardiology, and immunology (from highest to lowest). With respect to the phases in which these clinical trials were found, 278 were in phase 1, 551 were in phase 2, 68 were in phase 3, and the remaining 6 were in phase 4. Despite many registered studies, only 18 of them have published results [
7].
Regarding these published results, most of the diseases for which MSCs are being used currently do not have a cure. For example, in orthopedics, cartilage lesions and osteoarthritis stand out. Currently, the treatments for these diseases are drugs or surgical measures to reduce discomfort and pain. Two treatment strategies using MSCs have been published reporting clinical improvements in pain, stiffness, and functionality in patients with knee osteoarthritis. One of which uses an intra-articular injection of autologous or allogeneic BM-MSCs and another that replaces the defect in the cartilage with a fibrin glue combined with chondronds and allogeneic BM-MSCs [
7]. Regarding cardiology, promising results in clinical and pathophysiological outcomes have been found in diseases such as dilated cardiomyopathy and ischemic or non-ischemic heart failure. In this case, MSCs have been delivered either locally (intramyocardial, intracoronary, and transendocardial) or intravenously, with an autologous or allogeneic source, and based on BM-MSCs, showing improvements in cardiac function, functional capacity, and quality of life [
7].
In pneumology, there are two published trials, one about idiopathic pulmonary fibrosis where allogeneic MSCs coming from the placenta, related or unrelated to a human leukocyte antigen (HLA) identical or HLA mismatched donors, were used. These patients were able to walk longer distances and had an improvement in lung function. The other pathology was acute respiratory distress syndrome for which allogeneic BM-MSCs were used. Unfortunately, this trial did not show any benefits [
7]. Concerning neurology/neurosurgery, spinal cord injury was treated through intrathecal and subarachnoid autologous BM-MSCs injections. Both trials resulted in improvements in sensitivity, pain, neurophysiological parameters, functional independence, and urodynamic studies [
7]. In the rest of the areas, AT-MSCs enriched fat grafts were injected in patients that required a breast reconstruction, showing promising results with a volume persistence [
7]. On the other hand, MSCs were used to treat sickle cell disease and advanced glaucoma, without good results in the trials [
7].
4. MSCs-approved treatments
Most of the treatments usually receive approval from the regulatory agencies after phase 3, making them commercially available to continue with phase 4. Until April 2023, three years after our systematic review, the number of registered clinical trials had risen to 1,120. However, the number of approved products by regulatory agencies around the world remains the same with only twelve (Table 1). In 2010, the first product that contained MSCs was approved by the MFDS in South Korea. The product is named Queencell and it is manufactured by Anterogen. Queencell is composed of stromal vascular fraction (SVF), which is a by-product of adipose harvesting of excess fatty tissue. SVF comprises a heterogeneous mixture of AT-MSCs and other cell types such as preadipocytes, endothelial progenitor cells, mast cells, and fibroblasts; approved for the treatment of subcutaneous tissue defects [
17].
Nine of the 12 approved MSCs products are from Asia. The country in the region with the most approved products is South Korea with 5 of them. These include the previously referred Queencell, in addition to Cellgram-AMI, Cupistem, Cartistem, and Neuronata-R. Cellgram-AMI is a method to improve the left ventricular ejection fraction in patients with acute myocardial infarction (AMI) reperfused by coronary angioplasty within 72 hours after chest pain [
18]. Cupistem showed that 82% of the patients with complex Crohn’s fistula achieved complete healing in eight weeks after treatment and 81% of them sustained a positive response up to week 96 [
17]. Cartistem is used for the treatment of knee cartilage defects associated with osteoarthritis recommended by the International Cartilage Repair Society (ICRS) grade IV (the most severe stage of the classification with no visible cartilage remaining) [
19]. Finally, NeuroNata-R has a neuroprotective effect that relieves the progression of amyotrophic lateral sclerosis (ALS) through the extension of motor nerve cell survival due to its anti-inflammatory and immunomodulatory effects [
20].
The other 4 remaining products are 2 from Japan, 1 from India, and 1 more from Iran. The products in Japan are Temcell HS and Stemiral. Temcell HS is an approved therapy for acute and refractory graft versus host disease (GVHD) in children and adult patients undergoing BM transplants for hematologic malignancies [
21]. Stemirac is the first “stem-cell” treatment approved for spinal cord injuries [
22]. In India, Stempeucel was approved for the treatment of critical limb ischemia (CLI) due to Buerger’s disease and peripheral arterial disease [
23]. Lastly, in Iran, Mesestrocell is used as an osteoarthritis treatment [
24].
In Europe, EMA has approved two MSCs therapies so far. Holoclar is used in the eye to replace damaged cells in the cornea epithelium in adults to treat moderate to severe limbal stem-cell deficiency caused by burns [
25]. Alofisel was approved for the treatment of complex anal fistulas in adult patients with Crohn’s disease [
26]. Finally, in the USA, being the country with the most MSCs clinical trials conducted, the only approved MSCs therapy so far is Remestemcel-L, which is an allogeneic cell product used for the treatment of steroid-refractory acute GVHD in pediatric patients [
27].
5. Current issues and future directions
MSCs will play an important role in the treatment of many diseases and conditions that currently do not have an effective treatment or cure. Although it is theoretically possible to transfer MSCs from the bench to the bedside, significant failures in quality control and many inconsistencies (regarding immunocompatibility, stability, heterogeneity, differentiation, and migratory capacity) have been reported in several clinical trials [
34]. Even though the product has been approved, the manufacturing company continues to face the possibility of having it withdrawn from the market. This could be due to problems with the safety of the product or not applying or paying for a renewal of the marketing authorization after the agreed deadline. This problem is more common in products used to treat diseases where the incidence is very low, and the price of the treatment very high [
35]. Also, another considerable economic problem that face these therapies for their applicability is that most of the insurance companies consider the MSCs therapies as experimental and they do not cover their costs.
Currently, there are animal studies that include several strategies that have been proposed to solve part of these problems. Among them are genetic modifications or priming strategies to modify the inherent characteristics of MSCs, biomaterial strategies to modify the outside circumstances, and the usage of MSCs’ secreted proteins and peptides (secretome). The genetic modification includes viral DNA transduction with mRNA/DNA transfection, or more recently, the CRISPR-Cas9 technology with higher effectiveness and specificity [
34]. The priming of MSCs could be done with pro-inflammatory mediators (IFN-y, TNF-a, IL-1a, IL-1b, IL-17a, and LPS), with hypoxia (1 to 5% of O
2), or with biomaterials (3D cell culture in collagen-hydrogel scaffold or chitosan scaffold, high-glucose concentration culture medium, spheroid formation, and matrilin-3-primed spheroids) [
34]. In the case of biomaterials, they are used to improve the delivery of MSCs, showing benefits in their adherence and survival [
34]. Lastly, the collection of proteins and peptides of the secretome of MSCs, includes growth factors, cytokines, chemokines, and even extracellular vesicles (EVs). This secretome has been shown to improve the safety profile and the efficacy in the treatment of neurological diseases, due to the greater ability it provides to MSCs for crossing the blood-brain barrier and blood-retinal barrier [
34].
While many clinical trials are underway and the various pathologies for which its efficacy as a treatment is being explored, we come to another big concern. Many people, including medical staff, want to take advantage of the desperate situation in which patients find themselves and set up businesses of products that have not been approved, including some not even in clinical studies. A recent report, which only includes the USA, reports that there are 1,480 businesses and 2,754 clinics selling MSCs treatments. This was four times more than five years ago [
35]. Another very similar concern is the so-called medical tourism, which consists of the same situation where people fo to foreign countries, mostly underdeveloped countries, in search of treatments that are not approved or even prohibited in their country [
36]. Most of these clinics offer treatments for multiple diseases for which MSCs have not been approved yet, such as autism spectrum disorders, alopecia, anti-aging therapies, chronic pain, erectile dysfunction, and even Coronavirus Disease 2019 (COVID-19) [
37]. In addition to exploiting the suffering, hope, fear, and economy of patients, these treatments represent a potential risk to their health. There are several potential safety concerns reported, including site reactions, the ability of cells to move from the site of application and change into inappropriate cell types, tumor formation, blindness, kidney failure, and infections because of the contamination of the finished products [
38]. Also, most of these establishments offer therapies where the extraction, isolation, and application processes do not comply with the standardized protocols (good manufacturing practices of GMPs), which leads to the failure of their purpose.
To solve this problem, regulatory agencies around the world should put pressure on their governments to take more rigorous actions against these dishonest and unprincipled establishments that take advantage of the misfortune of patients and damage the clinical research carried out in this field. For this reason, the population, in general, has been exhorted to do their part in this great problem. First, to make sure that before receiving any therapy that includes MSCs, they verify that it has been approved by the corresponding regulatory agency. If not, at least check that the therapy is being tested in a registered clinical trial and ensure that the treatment is being regulated during its production and application. Finally, to report illegal establishments where unapproved therapies are being used [
39].
In conclusion, there is a long way to go regarding treatment with MSCs, as any emerging treatment requires multiple efforts from different areas of interest for the matter, including researchers at the basic and clinical level, marketing companies, regulatory agencies and even governments and international organizations to solve the problems that have arisen throughout its development. A large part of the scientific community and the general public are very enthusiastic about the results that these therapies have shown and the scope that they could achieve in the future in the treatment of a wide variety of diseases in which their effect is being studied.
Author Contributions
Conceptualization, L.E.F.G. and H.A.B.S; investigation, L.E.F.G., S.A.B.B., and H.A.B.S.; writing-original draft preparation, L.E.F.G., S.A.B.B., and H.A.B.S.; writing-review and editing, L.E.F.G. and H.A.B.S.; visualization, L.E.F.G., S.A.B.B., and H.A.B.S.; supervision, H.A.B.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
We would like to thank Arnold I. Caplan, Vijay Vad, and Antonio Madrazo-Ibarra for their critical reading of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ramezankhani R, Torabi S, Minaei N, et al. Two Decades of Global Progress in Authorized Advanced Therapy Medicinal Products: An Emerging Revolution in Therapeutic Strategies. Frontiers in Cell and Developmental Biology 2020; 8: 547653.
- Shah S, Mudigonda S, Underhill TM, et al. Prx1+ and Hic1+ Mesenchymal Progenitors Are Present Within the Epidural Fat and Dura Mater and Participate in Dural Injury Repair. Stem Cells Translational Medicine 2022; 11(2): 200-212.
- Grech L, Ebejer JP, Mazzitelli O, et al. Possible Role of Circulating Bone Marrow Mesenchymal Progenitors in Modulating Inflammation and Promoting Wound Repair. International Journal of Molecular Sciences 2022; 23(1): 78.
- Caplan AI. Mesenchymal stem cells: Time to change the name! Stem Cells Translational Medicine 2017; 6: 1445-1451.
- Rajabzadeh N, Fathi E, Farahzadi R. Stem cell-based regenerative medicine. Stem Cell Investigation 2019; 6: 19.
- O’Donoghue K, Fisk NM. Fetal stem cells. Best Practice & Research Clinical Obstetrics and Gynaecology 2004; 18(6): 853-875.
- Rodríguez-Fuentes DE, Fernández-Garza LE, Samia-Meza JA, et al. Mesenchymal Stem Cells Current Clinical Applications: A Systematic Review 2021; 52: 93-101.
- Naji A, Eitoku M, Favier B, et al. Biological functions of mesenchymal stem cells and clinical implications. Cellular and Molecular Life Sciences 2019; 76: 3323-3348.
- Caplan, AI. Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. Journal of Cellular Physiology 2007; 213: 341-347.
- Da Silva Meirelles L, Cesar Chagastelles P, Beyer Nardi N. Mesenchymal stem cells reside in virtually all post-natal organs and tissues. Journal of Cell Science 2006; 119: 2204-2213.
- Crisan M, Yap S, Casteilla L. A Perivascular Origin for Mesenchymal Stem Cells in Multiple Human Organs. Cell Stem Cell 2008; 3: 301-313.
- Guimarães-Gamboa N, Cattaneo P, Sun Y, et al. Pericytes of Multiple Organs Do Not Behave as Mesenchymal Stem Cells In Vivo. Cell Stem Cell 2017; 20: 345-359.
- Caplan AI, Correa D. The MSC: An Injury Drugstore. Cell Stem Cell 2011; 9: 11-15.
- Hass R, Kasper C, Böhm S, et al. Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue-derived MSC. Cell Communication and Signaling 2011; 9: 1-14.
- Silva-Carvalho AE, Resende Sousa MR, Alencar-Silva T, et al. Mesenchymal stem cells immunomodulation: The road to IFN-γ licensing and the path ahead. Cytokine \& Growth Factor Reviews 2019; 47: 32-42.
- Ferrin I, Beloqui I, Zabaleta L, et al. Isolation, Culture, and Expansion of Mesenchymal Stem Cells. In: Crook J, Ludwing T. Stem Cell Banking. Methods in Molecular Biology, vol 1590. Humana Press, New York, NY; 2017. p. 170-190.
- Biological Products (Cell therapy products) ANTEROGEN [Internet]. Ministry of Food and Drug Safety. [cited 2022 Jan 7]. Available from: https://www.mfds.go.kr/eng/brd/m_30/view.do?seq=71337&srchFr=&srchTo=&srchWord=&srchTp=&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&page=1.
- Business (Stem Cell drugs) Hearticellgram-AMI is the world´s first stem cell drug [Internet]. PHARMICELL. [cited 2022 Jan 11]. Available from: http://www.pharmicell.com/eng/biz/medicine_cellgram.html.
- Products (1st generation) CARTISTEM. [cited 2022 Jan 11]. Available from: https://www.medi-post.com/cartistem/.
- CORESTEM (Products) ALS (NeuroNata-R). [cited 2022 Jan 11]. Available from: http://corestem.com/en/m21.php.
- BioPharma Asia (Sections) JCR Pharma launch TEMCELL HS in Japan. [cited 2022 Jan 12]. Available from: https://biopharma-asia.com/sections/jcr-pharma-launch-temcell-hs-in-japan/.
- Cyranoski, D. Japan’s approval of stem-cell treatment for spinal-cord injury concerns scientists. Nature 2019; 565: 544-545.
- Stempeutics (Products) Stempeucel. [cited 2022 Jan 12]. Available from: https://www.stempeutics.com/stempeucel.html.
- CellTech Pharmed. Mesestrocell: Cell therapy for osteoarthritis. [cited 2022 Jan 12]. Available from: http://en.celltech.ir/.
- European Medicine Agency Sciences Medicine Health (Medicines) Holoclar. [cited 2022 Jan 12]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/holoclar#:~:text=Holoclar%20is%20a%20stem%2Dcell,iris%20(the%20coloured%20part).
- European Medicine Agency Sciences Medicine Health (Medicines) Alofisel. [cited 2022 Jan 12]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/alofisel.
- ONCOLOGY DRUGS ADVISORY COMMITTEE. REMESTEMCEL-L FOR TREATMENT OF STEROID REFRACTORY ACUTE GRAFT VERSUS HOST DISEASE IN PEDIATRIC PATIENTS. FDA Advisory Committee 2020; 1-127.
- Alliance for Regenerative Medicine. Available Products. [cited 2022 Jan 13]. Available from: https://alliancerm.org/available-products/.
- CORESTEM, First licensed stem cell therapy for ALS. Biopharma dealmarkers 2019; B24.
- NICE National Institute for Health and Care Excellence (Guidance). Holoclar for treating limbal stem cell deficiency after eye burns. [cited 2022 Jan 13]. Available from: https://www.nice.org.uk/guidance/ta467/chapter/2-the-technology.
- GlobeNewswire by notified (mesoblast). Mesoblast’s Japan Licensee Receive Pricing for TEMCELL HS Inj. for Treatment of Acute Graft Versus Host Disease. [cited 2022 Jan 13]. Available from: https://www.globenewswire.com/news-release/2015/11/27/790909/0/en/Mesoblast-s-Japan-Licensee-Receives-Pricing-for-TEMCELL-HS-Inj-for-Treatment-of-Acute-Graft-Versus-Host-Disease.html.
- Takeda (News Releases). Takeda Receives Approval to Manufacture and Market Alofisel (darvadstrocel) in Japan for Treatment of Complex Perianal Fistulas in Patients with Non-active or Mildly Active Luminal Crohn’s Disease. [cited 2022 Jan 13]. Available from: https://www.takeda.com/newsroom/newsreleases/2021/takeda-receives-approval-to-manufacture-and-market-alofisel-darvadstrocel-in-japan-for-treatment-of-complex-perianal-fistulas-in-patients-with-non-active-or-mildly-active-luminal-crohns-disease/.
- MINNEWS (Economy). Hemodialysis is the second largest in the world, with a market share of 20%. Nipro is in the field of regenerative medicine. [cited 2022 Jan 13]. Available from: https://min.news/en/economy/6bd2d26e84f61a961aeb1c00747d0d8e.html.
- Zhou T, Yuan Z, Weng J, et al. Challenges and advances in clinical applications of mesenchymal stromal cells. Journal of Hematology & Oncology 2021; 14: 24.
- LABIOTECH.eu (In depth). Why Are There Only 11 Cell and Gene Therapies in Europe? [cited 2022 Jan 14]. Available from: https://www.labiotech.eu/in-depth/atmp-cell-gene-therapy-ema/.
- Orozco-Solares TE, León-Moreno LC, Rojas-Riozo A, et al. Allogenic Mesenchymal Stem Cell-Based Treatment Legislation in Latin America: The Need for Standardization in a Medical Tourism Context.
- News wise (Articles). Businesses selling non-FDA-approved stem cell products grew four-fold in five years, UCI study says. [cited 2022 Jan 14]. Available from: https://www.newswise.com/articles/businesses-selling-non-fda-approved-stem-cell-products-grew-four-fold-in-five-years-uci-study-says.
- U. S. FOOD & DRUG ADMINISTRATION (Consumer updates). FDA Warns About Stem Cell Therapies. [cited 2022 Jan 14]. Available from: https://www.fda.gov/consumers/consumer-updates/fda-warns-about-stem-cell-therapies.
- U. S. FOOD & DRUG ADMINISTRATION (Consumer’s biologics). Important Patient and Consumer Information About Regenerative Medicine Therapies. [cited 2022 Jan 14]. Available from: https://www.fda.gov/vaccines-blood-biologics/consumers-biologics/important-patient-and-consumer-information-about-regenerative-medicine-therapies.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).