Submitted:
27 February 2023
Posted:
28 February 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
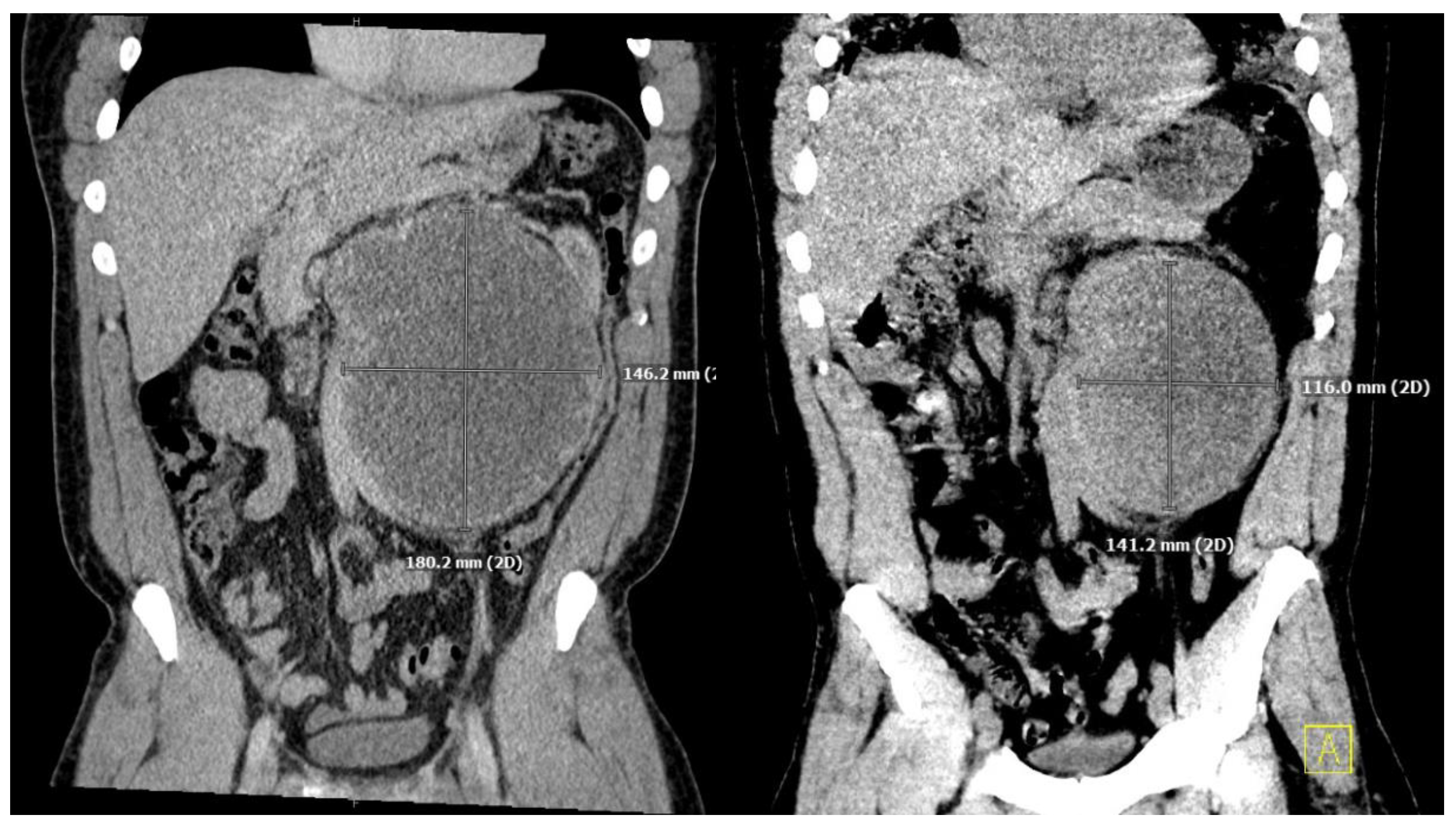
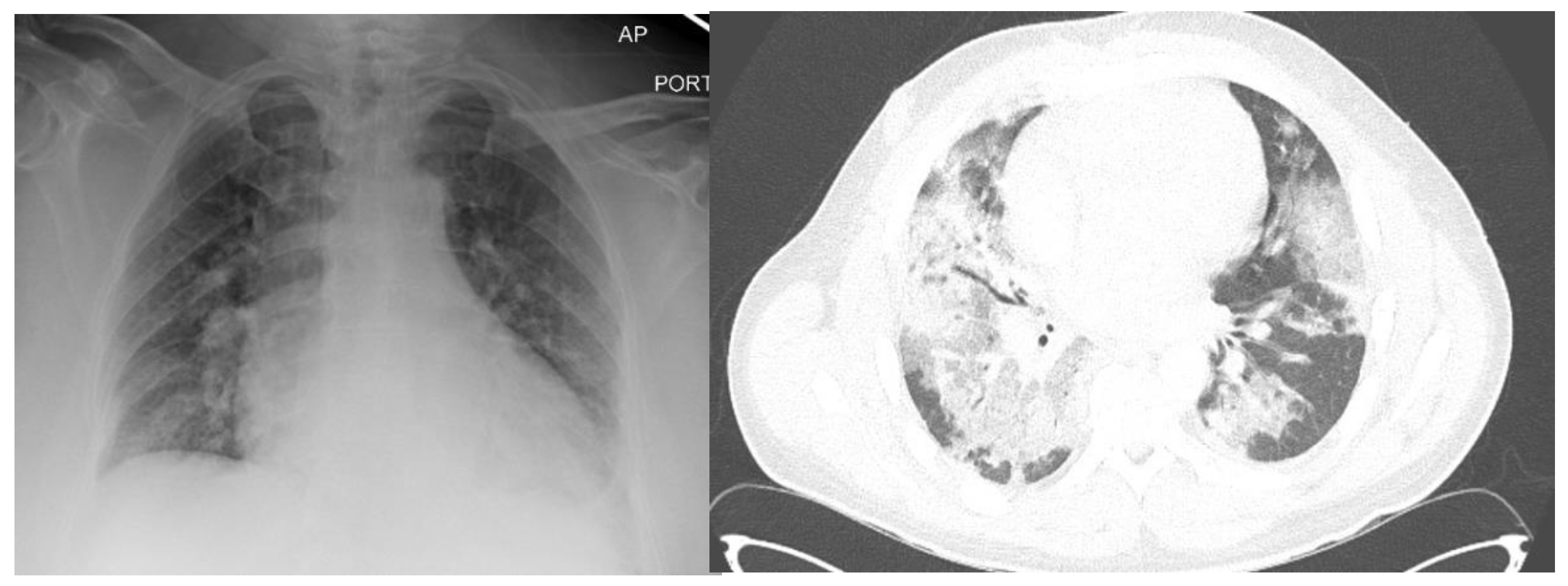
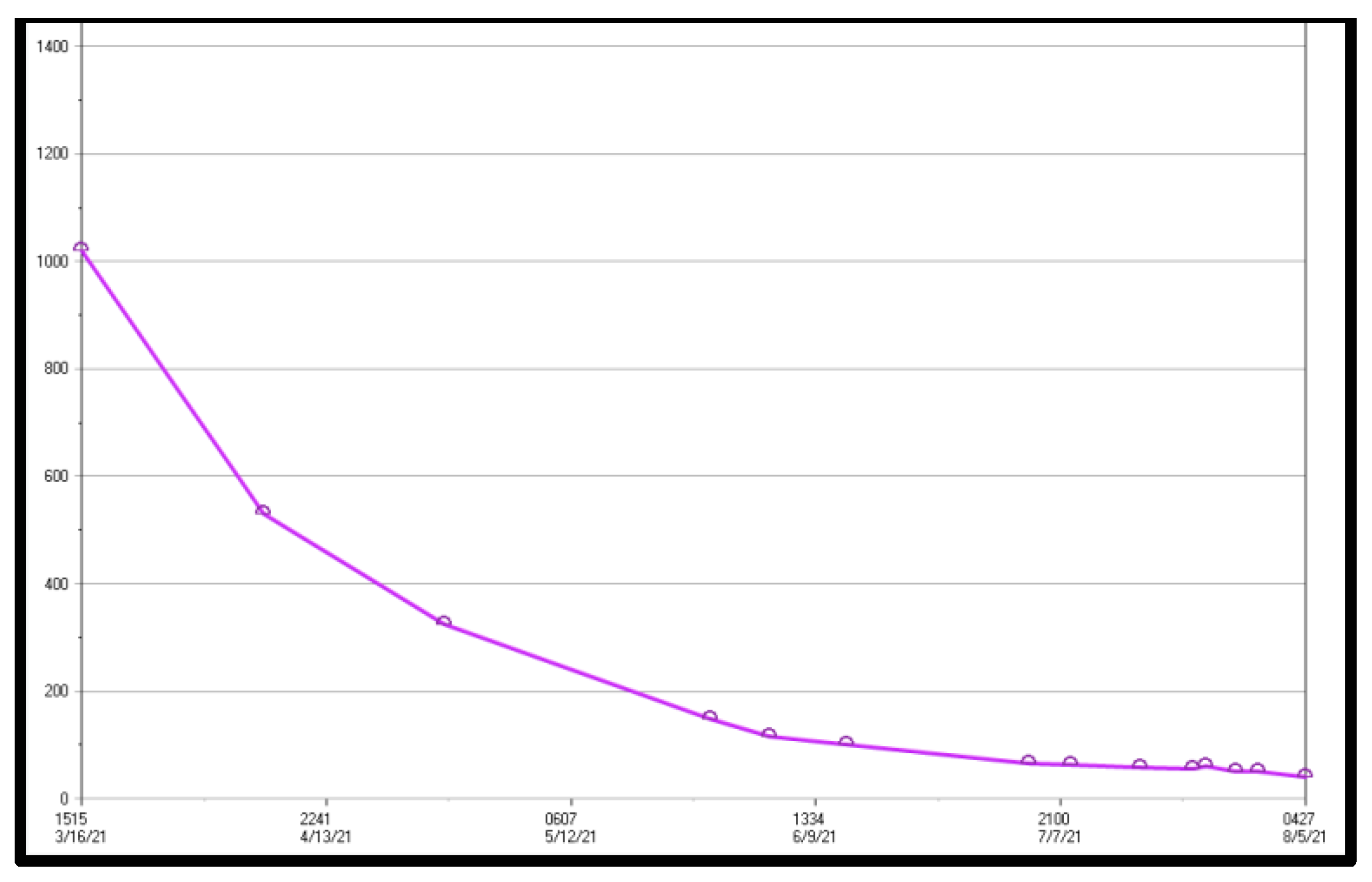
2. Case Presentation Section
3. Discussion
3.1. Testicular Cancer
3.2. Belomycin Toxicity
3.3. Lung Transplant in the Setting of Recent Neoplasm
3.4. ECMO Withdrawal and Ethical Considerations
3.5. Resolution
4. Conclusions
Funding
Conflicts of Interest
References
- Narayan, V.; Deshpande, C.; Bermudez, C.A.; Golato, J.M.; Lee, J.C.; Diamond, J.; Vaughn, D.J. Bilateral lung transplantation for bleomycin-associated lung injury. Oncologist 2017, 22, 620–622. [Google Scholar] [CrossRef] [PubMed]
- Fukawa, T.; Kanayama, H.O. Current knowledge of risk factors for testicular germ cell tumors. Int. J. Urol. 2018, 25, 337–344. [Google Scholar] [CrossRef]
- Batool, A.; Karimi, N.; Wu, X.N.; Chen, S.R.; Liu, Y.X. Testicular germ cell tumor: a comprehensive review. Cell Mol. Life Sci. 2019, 76, 1713–1727. [Google Scholar] [CrossRef] [PubMed]
- Chahoud, J.; Zhang, M.; Shah, A.; Lin, S.H.; Pisters, L.L.; Tu, S.M. Managing seminomatous and nonseminomatous germ cell tumors. Curr. Opin. Oncol. 2018, 30, 181–188. [Google Scholar] [CrossRef]
- Dorr, R.T. Bleomycin pharmacology: mechanism of action and resistance, and clinical pharmacokinetics. Semin. Oncol. 1992, 19 (Suppl 5), 3–8. [Google Scholar]
- Hay, J.; Shahzeidi, S.; Laurent, G. Mechanisms of bleomycin-induced lung damage. Arch. Toxicol. 1991, 65, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Della Latta, V.; Cecchettini, A.; Del Ry, S.; Morales, M.A. Bleomycin in the setting of lung fibrosis induction: From biological mechanisms to counteractions. Pharmacol. Res. 2015, 97, 122–130. [Google Scholar] [CrossRef]
- Rossi, S.; Erasmus, J.; McAdams, P.; Sporn, T.; Goodman, P. Pulmonary drug toxicity: Radiologic and pathologic manifestations. Radiographics 2000, 20, 1245–1259. [Google Scholar] [CrossRef] [PubMed]
- Sabino, G.; Cao, K.N. Blast from the past: Concern for a delayed presentation of bleomycin induced pulmonary toxicity. Am. J. Respir. Crit. Care Med. 2020, 201, A3118. [Google Scholar]
- Reinert, T.; Serodio da Rocha Baldotta, C.; Pereira Nunes, F.A.; Alves de Souza Scheliga, A. Bleomycin-induced lung injury. J. Cancer Res. 2013, 2013, 1–9. [Google Scholar] [CrossRef]
- Liu, Y.; Lu, F.; Kang, L.; Wang, Z.; Wang, Y. Pirfenidone attenuates bleomycin-induced pulmonary fibrosis in mice by regulating Nrf2/Bach1 equilibrium. BMC Pulm. Med. 2017, 17, 63. [Google Scholar] [CrossRef] [PubMed]
- Odish, M.F.; McGuire, W.C.; Thistlethwaite, P.; Crotty Alexander, L.E. Bleomycin-induced lung injury treated with venovenous extracorporeal membrane oxygenation (ECMO) and ultra-protective ventilator settings. BMJ Case Rep. 2020, 13, e236474. [Google Scholar] [CrossRef] [PubMed]
- Penn, I.; Starzl, T.E. Immunosuppression and cancer. Transplant. Proc. 1973, 5, 943–947. [Google Scholar] [PubMed]
- Triplette, M.; Crothers, K.; Mahale, P.; et al. Risk of lung cancer in lung transplant recipients in the United States. Am. J. Transplant. 2019, 19, 1478–1490. [Google Scholar] [CrossRef] [PubMed]
- Al-Adra, D.; Hammel, L.; Roberts, J.; Woodle, S.; Levine, D.; Mandelbrot, D.; Verna, E.; Locke, J.; D’Cunha, J.; Farr, M.; et al. Pretransplant solid organ malignancy and organ transplant candidacy: A consensus expert opinion statement. Am. J. Transplantat. 2020, 21, 460–474. [Google Scholar] [CrossRef]
- Penn, I. The effect of immunosuppression on pre-existing cancers. Transplantation 1993, 55, 742–747. [Google Scholar] [CrossRef]
- ELSO. Guidelines for Cardiopulmonary Extracorporeal Life Support Extracorporeal Life Support Organization, Version 1; Ann Arbor, MI, USA, 2017. [Google Scholar]
- Murray, J.F.; Matthay, M.A.; Luce, J.M.; Flick, M.R. An expanded definition of the adult respiratory distress syndrome. Am. Rev. Respir. Dis. 1988, 138, 720–723, Erratum in: Am. Rev. Respir. Dis. 1989, 139, 1065. [Google Scholar] [CrossRef]
- Mulaikal, T.A.; Nakagawa, S.; Prager, K.M. Extracorporeal membrane oxygenation bridge to no recovery. Circulation 2019, 139, 428–430. [Google Scholar] [CrossRef]
- Beauchamp, T.L.; Childress, J.F. Principles of Biomedical Ethics, 6th ed.; Oxford University Press: New York, 2009. [Google Scholar]
- Davidson, J.E.; Jones, C.; Bienvenu, O.J. Family response to critical illness: postintensive care syndrome-family. Crit. Care. Med. 2012, 40, 618–624. [Google Scholar] [CrossRef]
- Smith, S.; Rahman, O. Post Intensive Care Syndrome. [Updated 2021 Jul 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available online: https://www.ncbi.nlm.nih.gov/books/NBK558964/.
- Zante, B.; Camenisch, S.A.; Schefold, J.C. Interventions in post-intensive care syndrome-family: A systematic literature review. Crit. Care Med. 2020, 48, e835–e840. [Google Scholar] [CrossRef]
- Nakagawa, S.; Masahiko, A.; Takayama, H.; Takeda, K.; Garan, A.; Yuill, L.; Rosen, A.; Topkara, V.; Yuzefpolskaya, M.; Colombo, P.; et al. Withdrawal of left ventricular assist devices: A retrospective analysis from a single institution. J. Palliat. Med. 2019, 23, 368–374. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




