1. Introduction and Anatomy
The lacrimal gland is positioned in the lacrimal fossa of the frontal bone. The levator aponeurosis separates the lacrimal gland into two portions: palpebral and orbital lobes. The larger orbital lobe has excretory ducts that pass through and join with the ducts of the palpebral lobe before eventually emptying into the superolateral conjunctiva. Sensory innervation is supplied by the lacrimal nerve which is a branch of the ophthalmic division of the trigeminal nerve. Parasympathetic innervation is contributed by the facial nerve via greater and deep petrosal nerve; this is important in the secretion of aqueous part of the precorneal tear film, which is essential to the health of the eye.
The lacrimal gland is secured in place by interwoven fibrous periosteal connection including connective tissue posteriorly, the ligament of Soemmering superiorly, Whitnall Ligament medially, and to the lateral margin of the levator aponeurosis laterally [1, 2].
The lacrimal gland arises from the ectoderm of conjunctiva, interacting with its neighboring orbital bone, soft tissues and interstructure space as it continues to develop until 3-4 years after birth. Perhaps genetic differences determine the differences in phenotypic manifestation of these structures that ultimately determine the lacrimal gland size and contours[
2,
3].
During aging processes, like many other structures in the body, due to the gravity, suspensory ligaments of the lacrimal gland can become lax, resulting in the prolapse of the lacrimal gland, most commonly the palpebral lobe [
2]. The incidence of this disorder has been reported in 15% of patients who presented for blepharoplasty evaluation; in older patient populations, with a mean age of 78, in 60% of the cases [
4].
2. Case Report
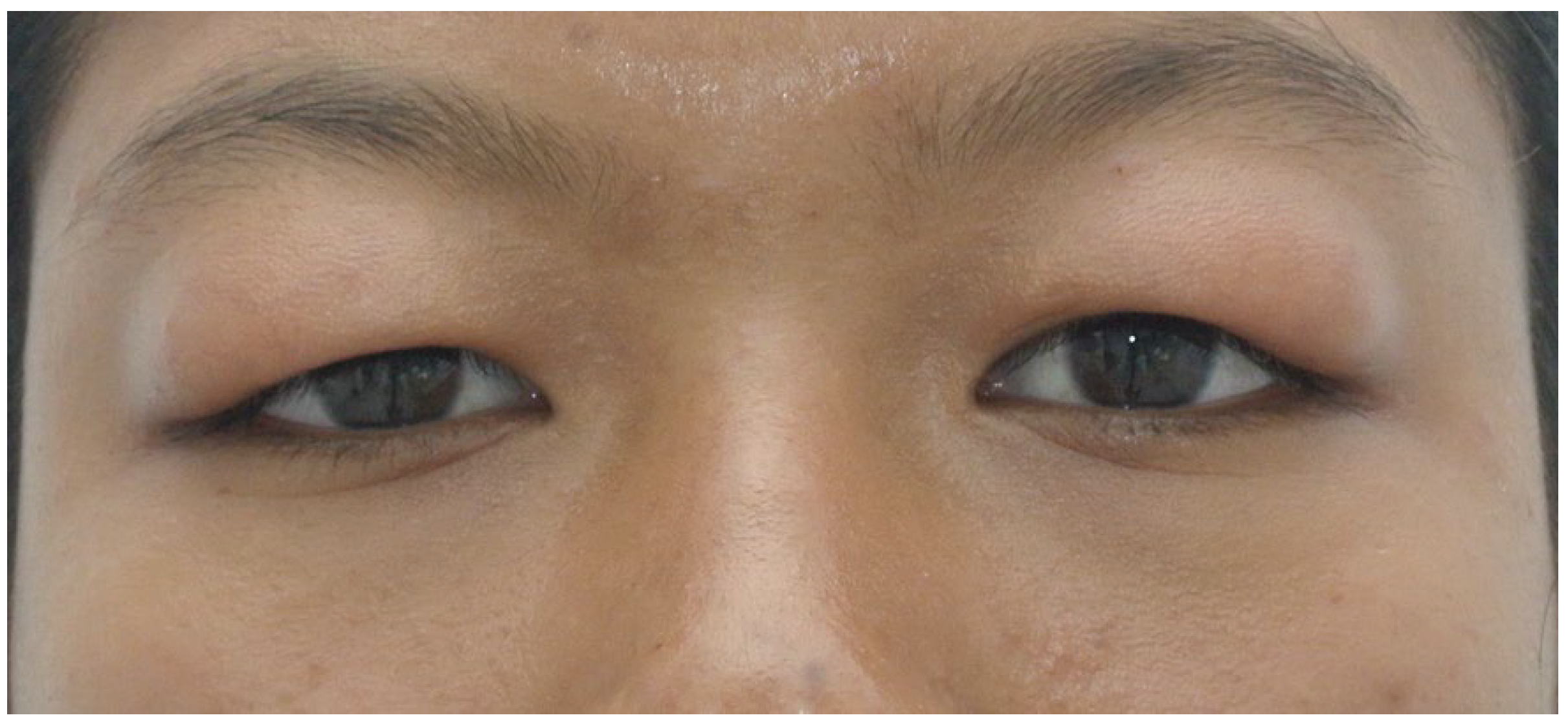
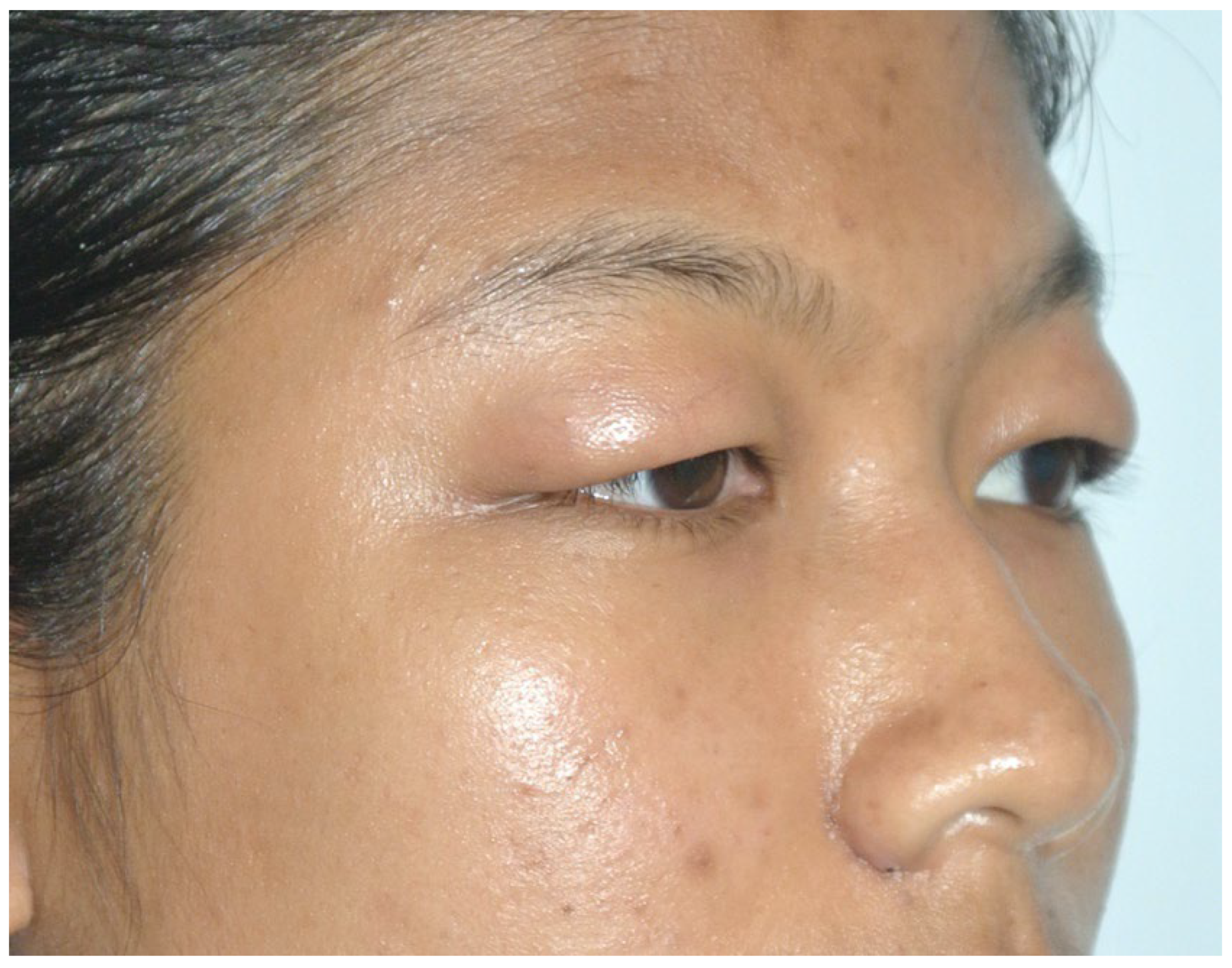
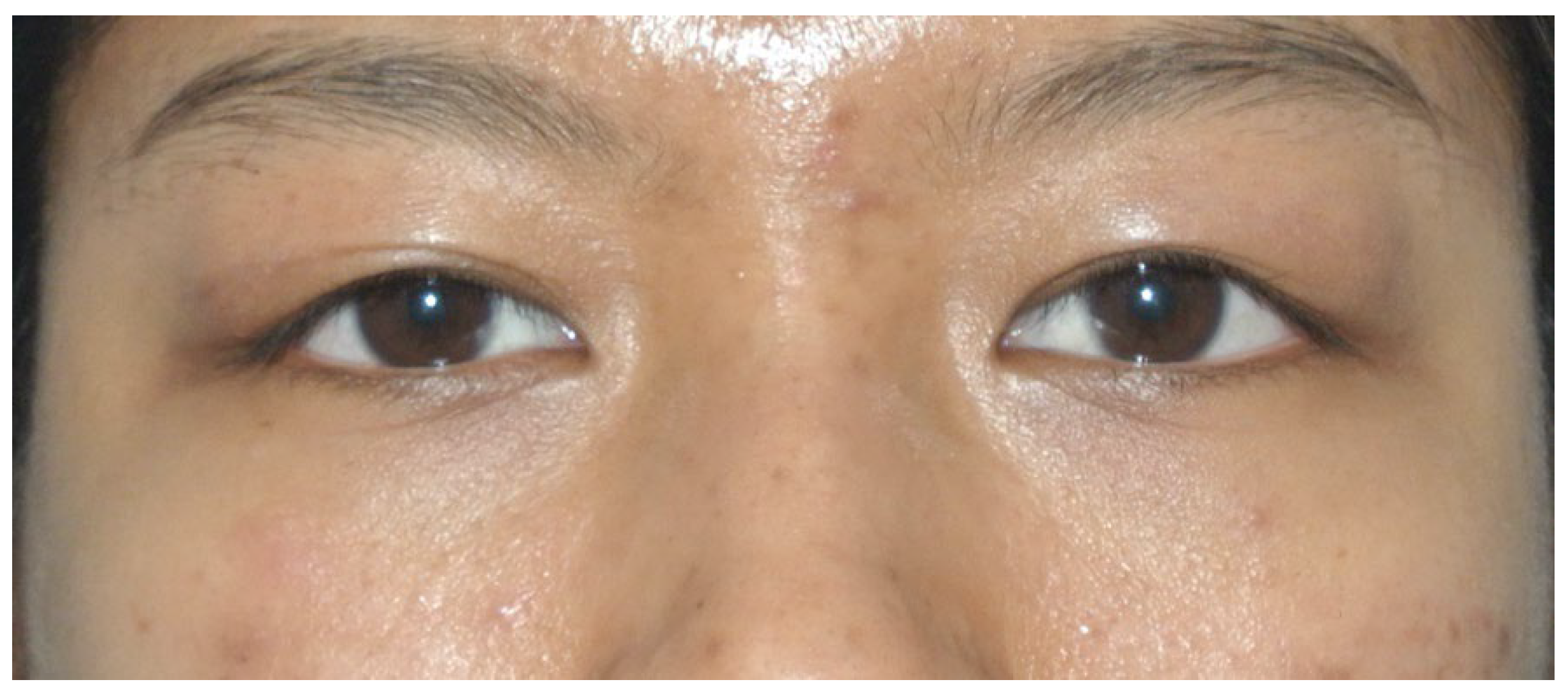
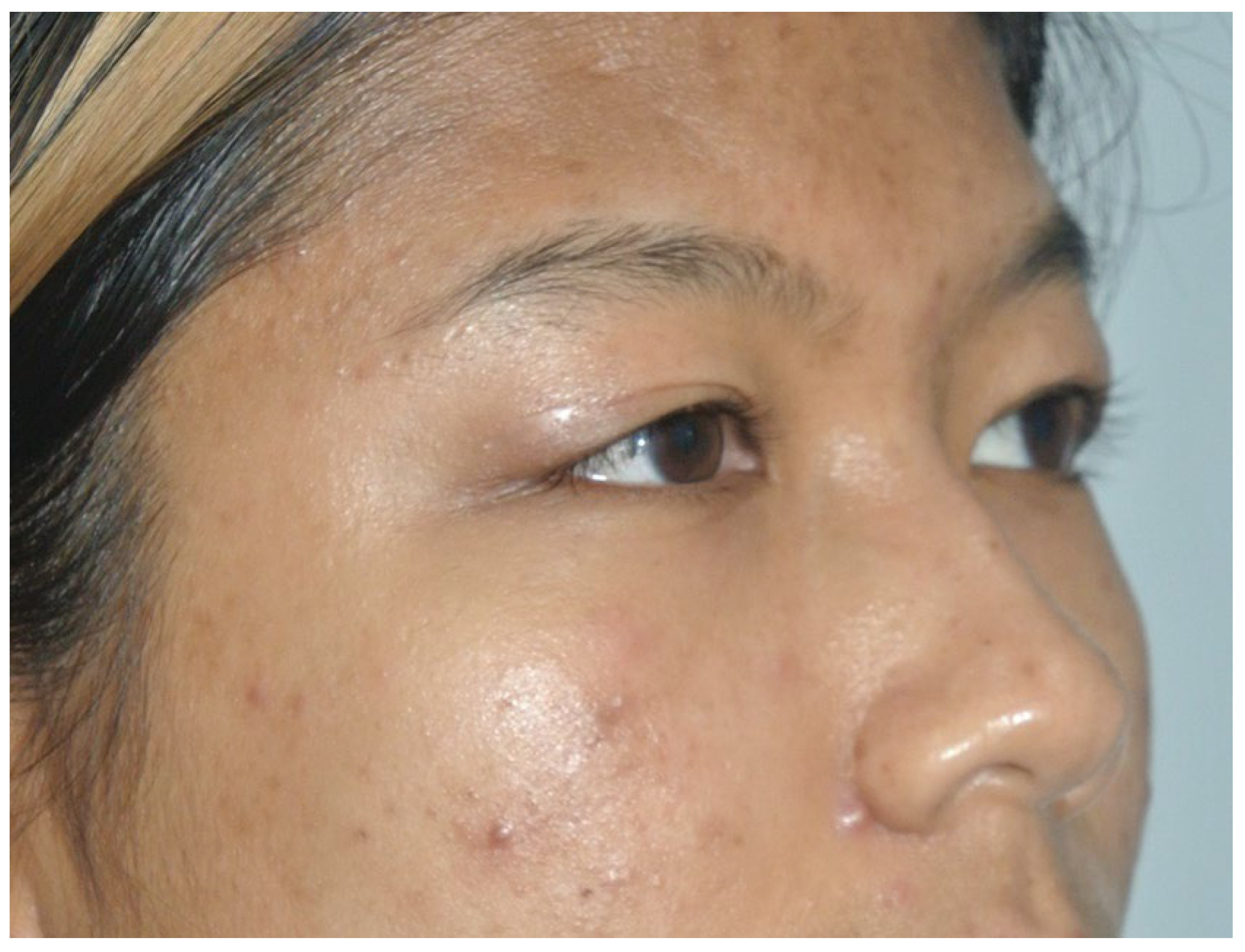
A 19 years old Asian woman was referred to our department with slow, progressive fullness in the lateral two-thirds of both upper eyelids at the age of onset at 7 years old with the eventual disappearance of upper eyelid crease and occasional mild erythema. She reported the fullness worsens after crying spells and bee stings with no identifiable relieving or associated factors. It is also reported to have sagged over the years until the symptoms stabilized at the age of 14. (
Figure 1 and
Figure 2). Patient denied pain, any visual field restriction or any other ocular irritation with no history of trauma to the orbits.
Physical examination shows redundant, non-pitting edematous upper eyelid skin with a firm, mobile mass in the lateral two-thirds of the upper eyelid with the right side being worse. These masses cannot be manually reduced.
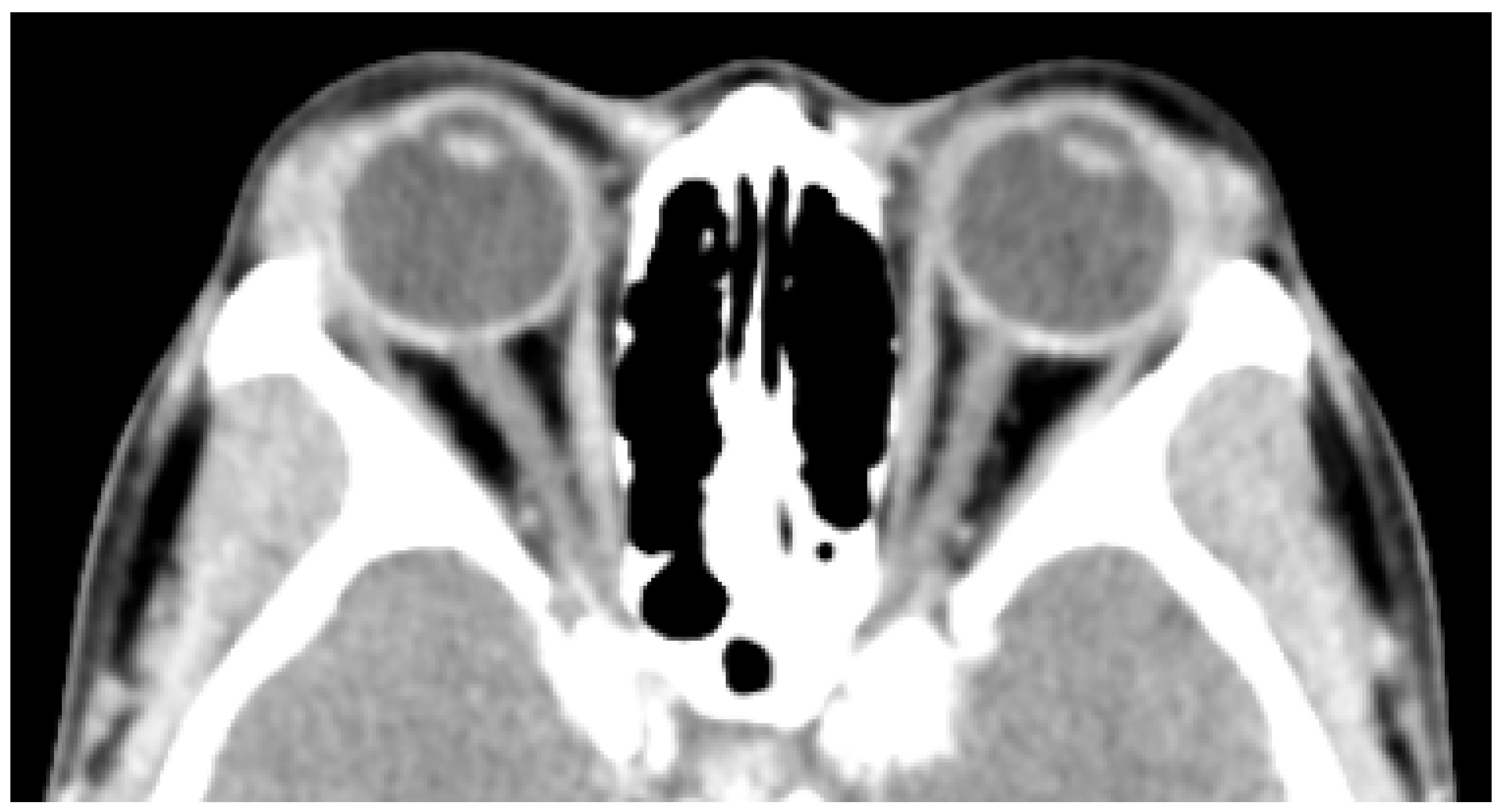
CT scan with contrast of the orbits (
Figure 3) shows bilateral symmetrical diffuse hypertrophy of lacrimal glands (arrowheads) measuring at approximately 9mm in thickness.
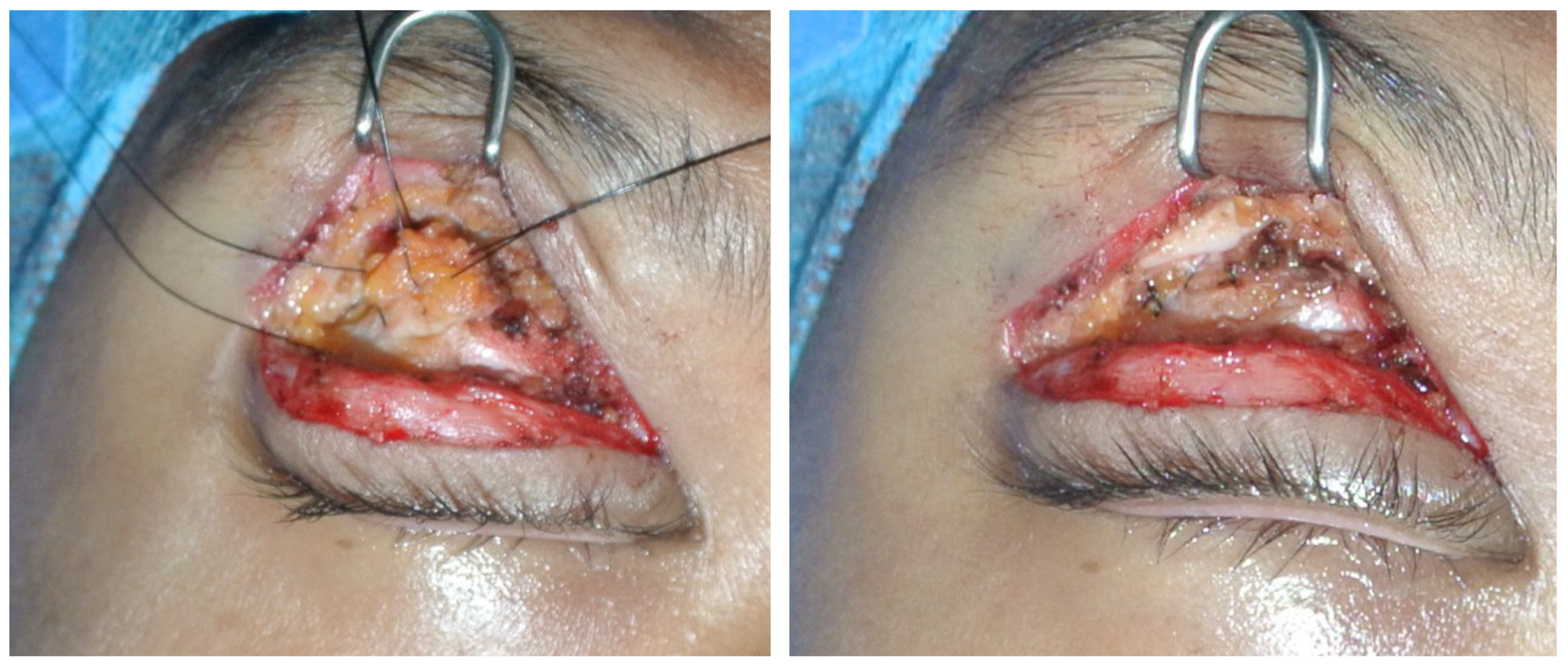
The patient underwent surgical treatment under local anesthesia. A transverse incision along the upper palpebral sulcus was made to expose the palpebral portion of the orbicularis oculi muscle. The redundant palpebral skin was excised. A blunt dissection of the orbital septum and extensive dieresis were performed to expose the central fat pad (
Figure 4). The prolapsed lacrimal gland, located laterally, was identified by its characteristics pinkish, firm, lobulated structure. The orbital lobe of the lacrimal gland was fixed to the periosteum of the lacrimal fossa using three sutures with nonabsorbable 4–0 monofilament nylon (
Figure 5 and
Figure 6). Hemostasis was ensured. The orbital septum and the orbicular oculi muscle were closed with simple interrupted sutures of 5–0 braided polyglactin. The skin was closed with continuous sutures of 6–0 monofilament polypropylene.
Suture were removed 7 days later. Postoperative three months have elapsed since the time of this report (
Figure 6 and
Figure 7).
3. Discussion
Lacrimal gland prolapse can be congenital or acquired, and can be due to various etiologies including recurrent edema (belpharochalasis syndrome), involutional changes craniofacial deformities, thyroid ophthalmopathy, sarcoidosis, post-traumatic and infectious conditions [
4]. There are a number of corrective surgical techniques varying from light cautery for mild cases to repositioning by fixation with sutures for moderate to severe cases [
4] to “lacrimoplasty”, whereby the prolapsed gland is fixed to the predrilled holes in the inner surface of the orbital rim, in recurrent cases [
5]. Postoperative recurrence can happen as late as 4 years especially in patients with blepharochalasis syndrome whose frequent swelling loosens the supporting structures of the eyelid [
5].
In our case presentation, the patient has no functional problem and correction was done for aesthetic reasons using suture repositioning technique. Although only 3 months have elapsed postoperatively, we have not observed any signs of recurrence, and the patient is satisfied with the result so far. We will continue to follow the patient on a regular basis.
4. Conclusions
Reposition of a prolapsed lacrimal gland is a safe and effective adjuvant procedure in upper blepharoplasty, with minimal complications and good postoperative outcome. Lacrimal gland reposition is a procedure that entails the separation of anatomic structures such as orbital septum, adipose tissue, and levator complex. However, failure to recognize a prolapsed lacrimal gland may cause simple excision of the gland likely by mistaking it with excess of fat pads, and this will have negative impact on the ocular lubrication.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Friedhofer H, Orel M, Saito FL, Alves HR, Ferreira MC. Lacrimal gland prolapse: management during aesthetic blepharoplasty: review of the literature and case reports. Aesthetic Plast. Surg. 2009, 33, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Lorber, M. Gross Characteristics of Normal Human Lacrimal Glands. Ocul. Surf. 2007, 5, 13–22. [Google Scholar] [CrossRef]
- Burkat CN, Wei LA. The Lacrimal System: Diagnosis, Management, and Surgery. 2nd rev. ed. Switzerland, Springer, 2015, 1.
- Massry, GG. Prevalence of Lacrimal Gland Prolapse in the Functional Blepharoplasty Population. Ophthal Plast Reconstr Surg. 2011, 27, 410–413. [Google Scholar] [CrossRef]
- Choudhary S, Khanna, S, Mantri R, Arora P, Jain R, Dutta S. Lacrimoplasty: a new bone fixation technique for recurrent lacrimal gland prolapse. Eur. J. Plast. Surg. 2018, 41, 465–470. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).