Submitted:
31 December 2022
Posted:
04 January 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
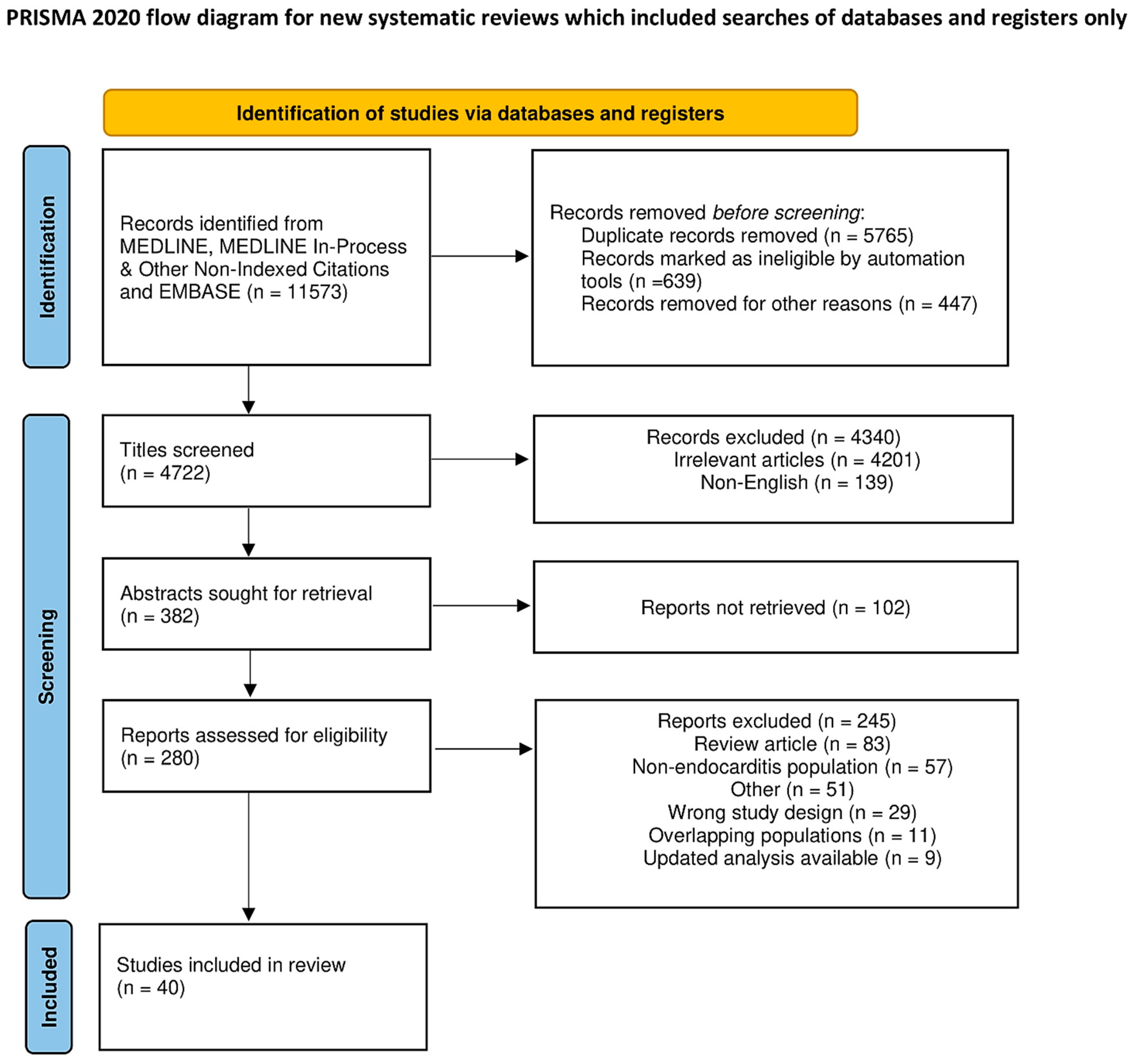
2. Methods
2.1. Search Strategy
2.2. Study Selection and Data Extraction
2.3. Endpoints and Effect Summary
3. Results
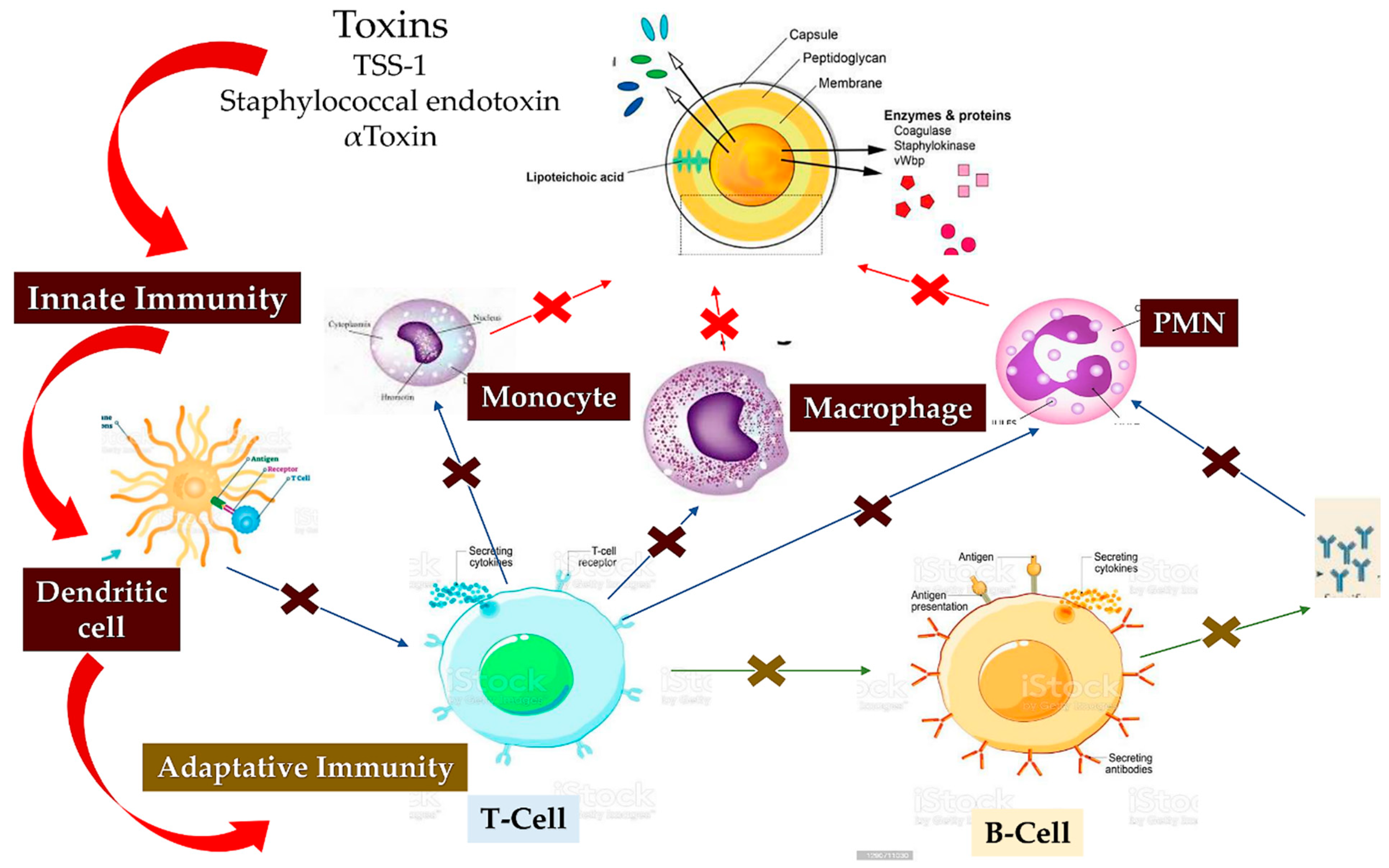
3.1. Staphylococcus aureus immunity
3.1.1. Staphylococcus aureus and host innate immunity
3.1.2. Staphylo-cytotoxins: A Trojan horse for excellent immune modulating.
3.1.3. Inconsistent cooperation between B and T lymphocytes due to cumulative effects of B lymphocyte deletion. Lack of help from T lymphocytes exacerbates infection
3.1.4. Immuno-Response and Vaccine
| First Author/Year Ref | Type of Study | Cohort | Aims | Finding |
|---|---|---|---|---|
| Lockhart et al (2008) Circulation [46] |
Human RCT Single Center (USA) |
290 pts Brushing Gro 98 Vs Extraction-Amoxicillin 96 Vs Extraction-Placebo 96 |
To compare the incidence, duration, nature, and magnitude of IE related bacteremia from single-tooth extraction and toothbrushing. To determine the impact of amoxicillin prophylaxis on single-tooth extraction. |
Amoxicillin has a significant impact on bacteremia resulting from a single-tooth extraction. Toothbrushing may be a greater threat for individuals at risk for infective endocarditis. |
| Mancini et al (2018) Virulence [49] |
Animal (Switzerland pilot) |
Rat with catheter-induced aortic vegetations | To investigate the role of Coa and vWbp in IE initiation | Coa does not support the initial colonization of IE (in L. lactis). vWbp contributes to initiation of IE (in L. lactis) however is marginal in the present of ClfA. |
| Reguiero et al (2019) Circ Cardiovasc Interv [51] |
Human Comparative Multicenter (Canada pilot) |
245 pts SEV 115 Vs BEV 130 |
To determine the incidence, clinical characteristics, and outcomes of patients with IE post-TAVR | IE post-TAVR did not reveal early or late mortality |
| Rodríguez-Vidigal et al (2019) Enferm Infecc Microbiol Clin [52] |
Human Observational Retrospective (Spain) |
200 pts with TAVI | To evaluate single-centre experience of incidence, mortality and associated factors of IE after TAVI. | Incidence of IE post TAVI greater than other series. |
| Di Carluccio et al (2021) RSC Chem Biol. [20] |
Human Multicenter (Italy pilot) |
Collected anatomical specimen | To evaluate the mechanism of interaction of SLBR-B and SLBR-H from S. gordonii in causing IE | Streptococcal Siglec-like adhesins sparks the development of tailored synthetic inhibitors and therapeutics specific for Streptococcal adhesins to counteract IE. No impairment the interplay between Siglecs and glycans. |
| Manukumar et al (2017) Sci Rep [56] |
Human Single Center (India) |
Collected blood draws | To characterize MRSA strain using MALDI-Biotyper multiplex PCR to distinguish between MRSA and MSSA. To screen PCR-SSCP | PCR-SSCP technique for rapid detection of MSSA and MRSA strains was developed |
| Mempel et al (2002) Br J Dermatol. [57] |
Human Single Center (Germany) |
†S. aureus DU 5720 Vs S. aureus DU 8325-4 Vs S. aureus DU 5883 |
To investigate haemolysin-independent virulence to human keratinocytes. | Staphylococcal invasion of human keratinocytes independently of alpha- and beta-hemolysins, leads to necrotic and apoptotic cell damage. |
| Nakagawa et al (2017) Cell Host Microbe J [58] |
Animal Multicenter Center (Japan pilot) |
Murine epicutaneous infection model | To evaluate how S. aureus trigger inflammation | Increased production of IL-1α, IL-36α and Il 17 via IL-1R and IL-36R. Increased γδ T cells, ILC3 and neutrophil. Keratinocyte* Myd88 signaling in response to S. aureus PSMα drives an IL-17-mediated skin inflammatory response to epicutaneous S. aureus infection. |
| Schwarz et al (2021) Virulence [63] |
Human in vitro and in vivo Multicenter (Germany) |
34 S. aureus Pts with S. aureus endocarditis Vs healthy individuals |
To evaluate pathomechanisms in the induction of IE | in vitro assays did not correlate with the severity of IE. i S. aureus isolates differed in the activation and inhibition of pathways connected to the extracellular matrix and inflammatory response |
| Malachowa et al (2011) PLoS One [64] |
Human/Animal Single center (USA) |
S. aureus LAC Vs S. aureus LACΔhlgABC |
To study the S. aureus USA300 transcriptome | Limited contribution of any single two-component leukotoxin lukS-PV and lukF-PV to USA300 immune evasion and virulence. |
| Alonso et al (2013) Nature [65] |
Animal Single center (USA) |
CCR5-deficient mice | To study activity of S. aureus leukotoxin ED (LukED) | CCR5-deficient mice are resistant to lethal S. aureus infection |
| Kim et al (2010) J Exp Med. [71] |
Animal Single center (USA) |
ℷ Mice with SpA (KKAA) | To study S. aureus protective immunity. | SpA (KKAA) immunization enabled MRSA-challenged mice to organize antibody responses to many different staphylococcal antigens. |
| Becker et al (2014) Proc Natl Acad Sci U S A. [72] |
In vitro Single center (USA) |
S. aureus Newman cultures | To demonstrate that SpA is released with murein tetrapeptide-tetraglycyl [L-Ala-D-iGln-(SpA-Gly5) L-Lys-D-Ala-Gly4] linked to its C-terminal threonyl | SpA, a B cell superantigen, is released with peptidoglycan linked to its C terminus. Murein hydrolases cleave the anchor structure of released SpA to modify host immune responses. |
| Zhang et al (2015) Infect Immun. [74] |
Animal Single center (China) |
Mice SaEsxA and SaEsxB Vs Mice rSaEsxA and rSaEsxB |
To investigate SaEsxA and SaEsxB, as possible targets for a vaccine. | SaEsxA and SaEsxB are effective toward Th1 and Th17 candidate antigens. |
| Brady et al (2013) PLoS One [75] |
Animal Single center (USA) |
Mice HlaH35L Vs Control Vs Prosthetic implant model of chronic biofilm |
To evaluate the ability of one S. aureus vaccine antigen to protect in three mouse models of infection | Vaccines may confer protection against one form of S. aureus disease without conferring protection against other disease presentations |
| Zhang et al (2018) mBio [76] |
Animal Multicenter (USA pilot) |
C57BL/6 mice | To study the role of adaptive immunity induced by an S. aureus vaccine in protection against S. aureus bacteremia | Multipronged humoral and cellular (B-cell, Th1, Th17) responses to S. aureus antigens may be critical to achieve effective and comprehensive immune defense |
| Yu et al (2018) Sci Rep [77] |
Animal Single center (China) |
Mouse peritonitis model | To evaluate the humoral immune response and CD4+ T cell-mediated immune responses | The MntC-specific antibodies and MntC-specific Th17 cells play cooperative roles in the prevention of S. aureus infection. |
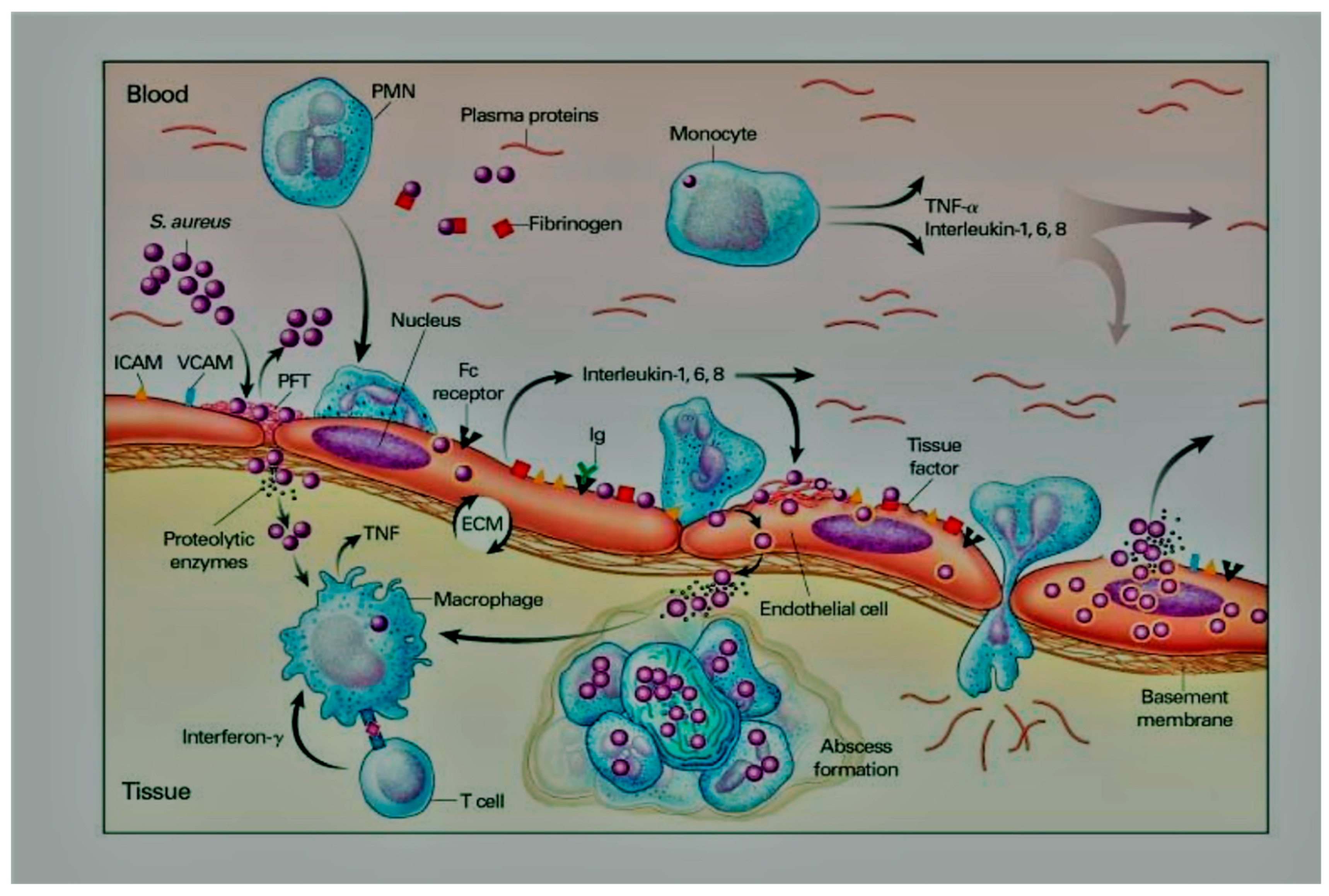
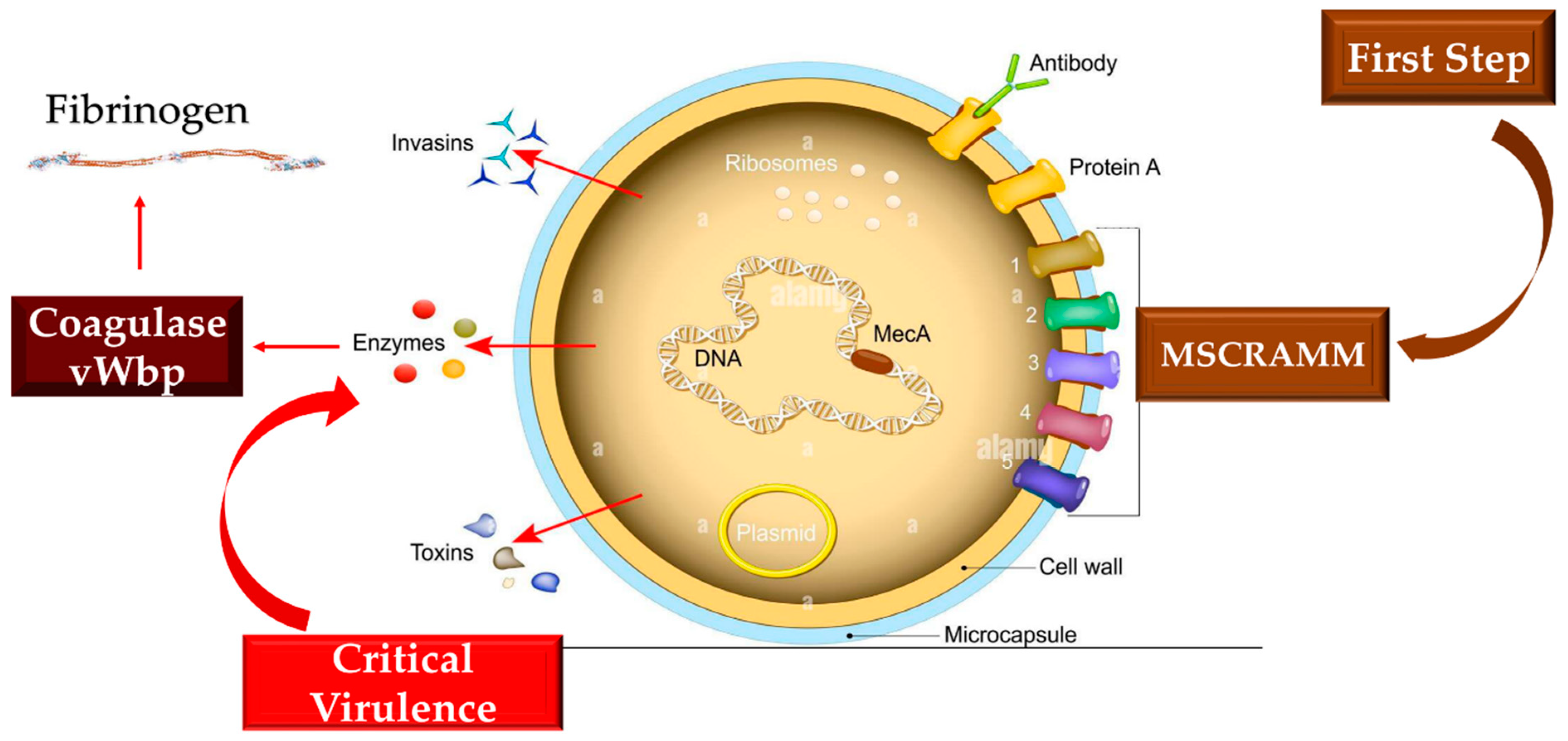
4. New evidence from the infectious array of Staphylococcus aureus. Involvement of the protective shield and host protection functions
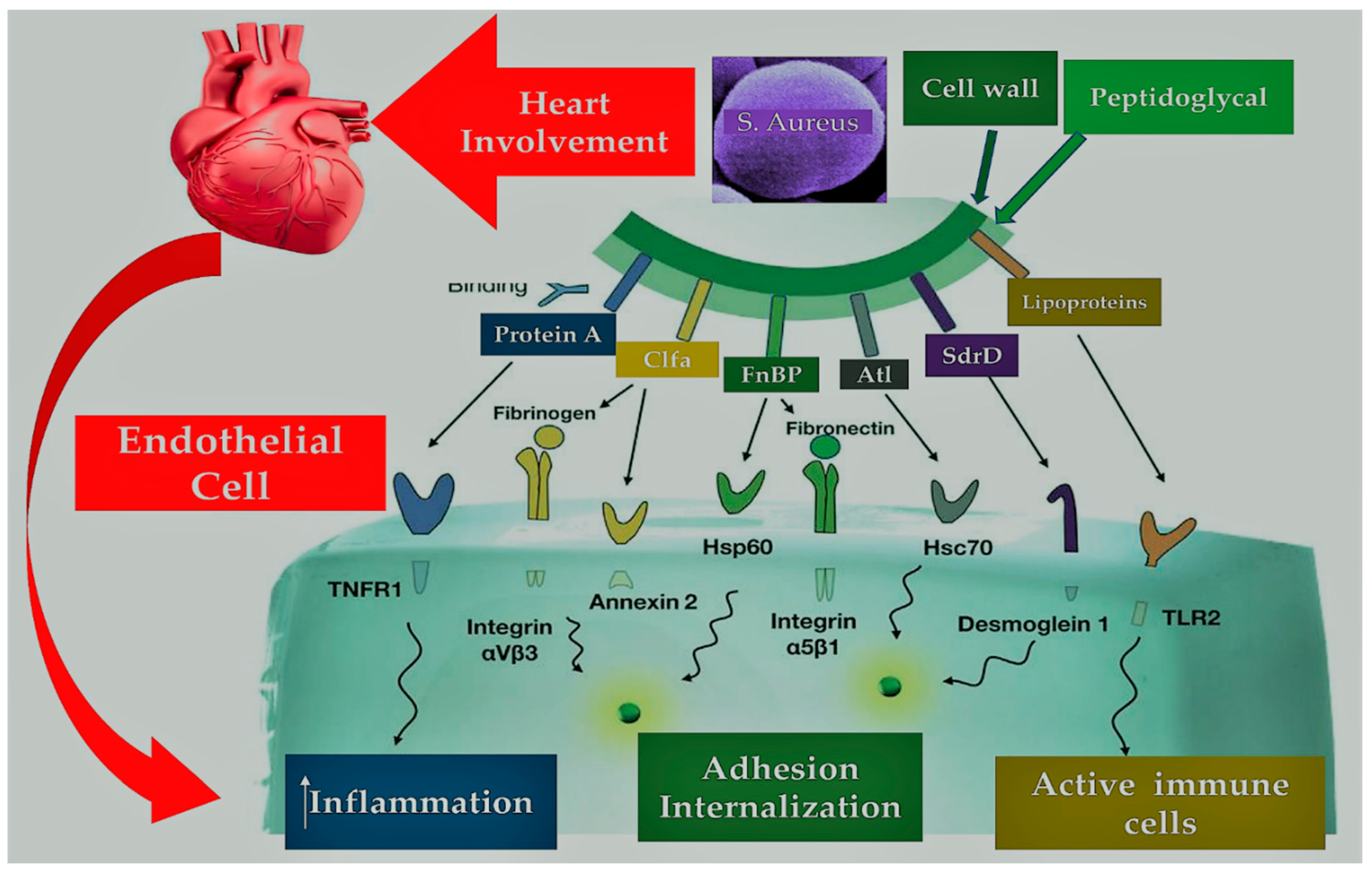
4.1. Pathogen-Host Interaction in Determining Inflammation
5. Interaction between infective endocarditis pathogens, vascular endothelium, and blood constituents
5.1. Infective Endocarditis and Platelets
| First Author/Year Ref | Type of Study | Cohort | Aims | Finding |
|---|---|---|---|---|
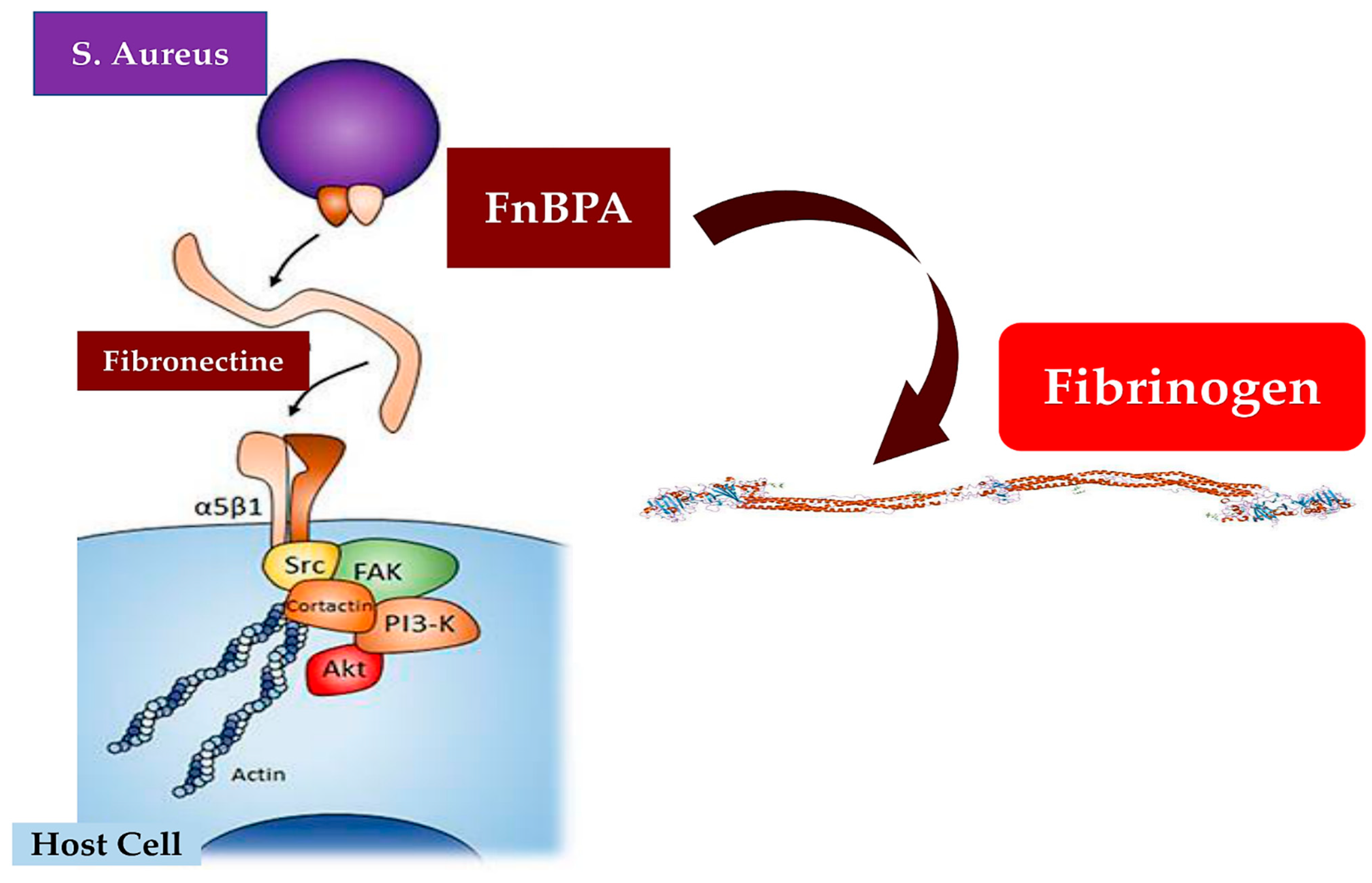
| Que et al (2005) J Exp Med [78] |
Animal model Single Center (Switzerland) |
Rat model of IE induced | To study valve colonization with experimental endocarditis. To evaluate the role of ClfA and FnBPA positive lactococci | Fibrinogen and fibronectin binding could cooperate for S. aureus valve colonization and endothelial invasion in vivo |
| Edwards et al (2012) PLoS One [79] |
Human Single Center (UK) |
Blood sample | To study in vivo role of Eap to interact with host glyco-proteins | Eap expressing strains cause a more severe infection, demonstrating its role in invasive disease. Increased level of TNFα and gC1qR/p33 expression |
| Veloso et al (2013) Infect Immun [81] |
Animal model Single Center (Switzerland) |
Rat model of IE induced 10(6) CFU L. lactis pIL253 Vs Recombinant L. lactis (ClfA, FnbpA, BCD, or SdrE) |
To explore the contributions of S. aureus virulence factors to the initiation of IE. | Fibrinogen binding in the initiation of S. aureus IE. Activation of platelet aggregation or an inflammatory response may contribute to or promote the development of EI |
| Thomas et al (2021) mBio [82] |
Animal model Single Center (USA) |
Rat model of IE induced | To identify proteins with significant amino acid identities to vWbp | Protein homologous to the C-terminal of vWbp was identified. Its role in Fg shield assembly and binds. |
| Hussain et al (2002) Infect Immun [83] |
In vitro Single center (Germany) |
S. aureus Newman cultures Vs Control mutant |
To investigate the role of Eap by constructing a stable eap::ermB deletion | Eap may contribute to pathogenicity by promoting adhesion of whole staphylococcal cells to complex eukaryotic substrates |
| Palankar et al (2018) Int J Med Microbiol. [84] |
In vitro Single center (Germany |
S. aureus Mu50 | To investigate Eap subdomain and interaction with platelet | Eap subdomain Eap D3D4 specifically interacts and rapidly activates human platelets |
| Hussain et al (2008) Infect Immun [85] |
In vitro Single center (Germany |
S. aureus Newman cultures Vs S. aureus Wood 46 |
To investigated the interactions of full-length Eap and five recombinant tandem repeat domains with host proteins. | More than one Eap tandem repeat domain is required for S. aureus agglutination, adherence, and cellular invasion but not for the stimulation of PBMC proliferation. |
| Heying et al (2007) Thromb Haemost. [88] |
Human Single Center (Germany) |
S. aureus L. lactis culture cultured human EC |
To investigate the role of FnBPA, FnBPB ClfA to promote bacterial adherence to cultured human ECs. | S. aureus FnBPs, but not ClfA, lead pathogenicity to non-pathogenic L. lactis. Adhesins (ICAM-1 and VCAM-1) evokes inflammation (interleukin-8) as well as procoagulant activity. |
| Piroth et al (2008) Infect Immun [89] |
Animal model Single Center (Switzerland) |
S. aureus L. lactis culture In vitro and in vivo |
To study subdomain of FnBPA responsible for fibrinogen and fibronectin binding, cell invasion, and in vivo endocarditis | Fb binding combined with fibronectin binding to synergize the invasion of cultured cell lines is correlate with IE severity |
| Pappelbaum et al (2013) Circulation. [91] |
Human/Animal Single center (Germany) |
6 WT mice with VWF vs 5 knockout mice vs Cultured human EC |
Whether ULVWF mediates bacterial adherence. | ULVWF contributes to the initial pathogenic step of S aureus-induced endocarditis in patients with an apparently intact endothelium. Heparin or ADAMTS13 intervenes in decreasing ULVWF adherence |
| Claes et al (2018) Thromb Haemost [93] |
Human/Animal Multicenter (Belgium pilot) |
L. lactis-clfA Vs L. lactis-fnbpA Vs Cultured human EC |
To study the influence of shear flow and plasma on the binding of ClfA and FnbpA | Pharmacological inhibition of ClfA-Fg interactions may constitute a valuable additive treatment in infective endocarditis. |
| Ko et al (2016) mBio [94] |
Animal model Single Center (USA) |
Rat model of IE induced | To identify variants of a linear Fg binding motif, present in Coa and Efb which are responsible for the Fg binding activities of these proteins | S. aureus coagulase can induce the formation of a fibrinogen shield in experimental abscess models which surrounds and protects bacteria in the microcolony from clearance. |
| Niemann et al (2021) mBio. [99] |
Animal Multicenter (Germany) |
Rat model of IE induced in osteoblasts vs epithelial cells |
To demonstrate that S. aureus was less engulfed in osteoblasts than in epithelial cells. | Large differences of S. aureus uptake efficacy in different host cell types. In vivo differences between courses of bacterial infections and the localization of bacteria in different clinical settings mediated by α5β1-integrin |
| Pietrocola et al (2020) J Biol Chem. [100] |
Animal Multicenter center (Italy pilot) |
Rat model of IE induced | To evaluate a variety of virulence factors that promote infection by S. aureus | Adherence to and invasion of epithelial and ECs by IsdB-expressing S. aureus cells was promoted by Vn, and an αvβ3 integrin-blocking mAb |
| Alfeo et al (2021) Sci Rep [101] |
Animal Multicenter center (Italy pilot |
Rat model of IE induced | To study IsdB protein and Vn binding Interacts with vWF. | Importance of IsdB in adherence of S. aureus to the endothelium colonization and as potential therapeutic target. |
| Ditkowski et al (2021) J Thorac Cardiovasc Surg [103] |
Human Multicenter (Belgium pilot) |
5 graft tissues | To investigate contributions by platelets and plasma fibrinogen to IE initiation on various grafts used for valve replacement | Binding of plasma Fg to especially BJV grafts enables adhesion of single platelets via αIIbβ3. S aureus attaches from blood to activated bound platelet αIIbβ3 via plasma fibrinogen. |
6. Biofilm formation
| First Author/Year Ref | Type of Study | Cohort | Aims | Finding |
|---|---|---|---|---|
| Schwartz et al (2021) APMIS [106] |
In vitro patch enriched with platelet and leucocyte-rich fibrin Multicenter (Danemark) |
IE organoid-like model by colonization with IE-associated bacterial isolates S. aureus, S. mitis and Enterococcus faecalis (IE vegetation (IEV) | To establish an in vitro vegetation simulation IE model for fast screening of novel treatment strategies | The surface-associated bacteria displayed increased tolerance to antibiotics compared to planktonic bacteria. IE simulation model with the relevant pathogens S. aureus, S. mitis group, and E. faecalis was established and IE model mirrors the natural IE process. |
| Di Domenico et al (2019) BMC Microbiol [107] |
Human Multicenter (IT) |
Samples of infected heart tissue. S. s aureus 50%, Enterococcus faecalis 25% and Streptococcus gallolyticus 25% | To assess a rapid biofilm identification assay and a targeted antimicrobial susceptibility profile of biofilm-growing bacteria in patients with IE, which were unresponsive to antibiotic therapy. | Biofilm-producing bacteria, from surgically treated IE, display a high tolerance to antibiotics, which is undetected by conventional antibiograms. |
| Schwartz et al (2012) APMIS [108] |
Animal model Multicenter (Danemark) |
IE organoid-like model by colonization with IE-associated bacterial isolates S. aureus, S. mitis and Enterococcus faecalis (IEV) | To evaluate the time course of biofilm formation and the impact on antibiotic tolerance development. | The antibiotic effect was significantly higher than when treatment was started after the biofilm was allowed to mature. |
| Kim et al (2016) JTCVS [113] |
Human Single Center (USA) |
86 pts Homografts Vs 139 pts Xenograft prostheses Vs 79 pts Mechanical prostheses |
To evaluate resistance to infection | Homografts were more used in PVE (P = .002) and methicillin-resistant Staphylococcus (P = .002), compared with conventional prostheses. No significant benefit to use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE. |
| Nappi et al (2018) JTCVS [120] |
Human Single center (France) |
210 pts | To evaluate long-term results of aortic allografts and to identify factors influencing long-term durability. | The use of allograft is a valid option in complex infective endocarditis and in women of childbearing age |
| Steffen et al (2016) JTCVS. [131] |
In vitro Single center (Germany) |
10 cryopreserved human allografts | To evaluate the in vitro antimicrobial activity of 3 antibiotic regimens | Allograft antibacterial activity despite long-term storage over 5 years. Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance. Ascending aortic tissue shows a significantly enhanced bacterial resistance against staphylococcal bacteria compared with aortic valves. |
7. Conclusion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Selton-Suty C, Celard M, Le Moing V, Doco-Lecompte T, Chirouze C, Iung B, Strady C, Revest M, Vandenesch F, Bouvet A, Delahaye F, Alla F, Duval X, Hoen B; AEPEI Study Group. Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis 2012; 54: 1230–39. [CrossRef]
- Chen H, Zhan Y, Zhang K, Chen H, Zhan Y, Zhang K, Gao Y, Chen L, Zhan J, Chen Z, Zeng Z. The Global, Regional, and National Burden and Trends of Infective Endocarditis From 1990 to 2019: Results from the Global Burden of Disease Study 2019.Front Med (Lausanne). 2022 Mar 9 ;9 :774224. [CrossRef]
- Resende P Jr, Fortes CQ, do Nascimento EM, Sousa C, Querido Fortes NR, Thomaz DC, de Bragança Pereira B, Pinto FJ, de Oliveira GMM. In-hospital Outcomes of Infective Endocarditis from 1978 to 2015: Analysis Through Machine-Learning Techniques. CJC Open. 2021 Sep 11 ;4(2) :164-172. [CrossRef]
- Allegranzi B, Bagheri Nejad S, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D.. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 2011 ; 377 : 228–41. [CrossRef]
- Bagheri Nejad S, Allegranzi B, Syed SB, Ellis B, Pittet D. Health-care-associated infection in Africa: a systematic review. Bull World Health Organ. 2011 Oct 1 ;89(10):757-65. [CrossRef]
- Joubert D, Cullati S, Briot P, Righi L, Grauser D, Ourahmoune A, Chopard P. How to improve hospital admission screening for patients at risk of multidrug-resistant organism carriage: a before-and-after interventional study and cost-effectiveness analysis. BMJ Open Qual. 2022 Apr ;11(2): e001699. [CrossRef]
- Blair JMA, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJV. Molecular mechanisms of antibiotic resistance. Nat Rev Microbiol 2015 ; 13 : 42–51.
- Martínez JL Antibiotics and antibiotic resistance genes in natural environments. Science. 2008 Jul 18 ;321(5887) :365-7.
- Yang M, Zhang J, Wei Y, Zhang J, Tao C Recent advances in metal-organic framework-based materials for anti-staphylococcus aureus infection. Nano Res. 2022 May 11 :1-23.
- McAdow M, Missiakas DM, Schneewind O. Staphylococcus aureus secretes coagulase and von Willebrand factor binding protein to modify the coagulation cascade and establish host infections. J Innate Immun. 2012 ;4(2) :141-8. [CrossRef]
- Thomer L, Schneewind O, Missiakas D. Multiple ligands of von Willebrand factor-binding protein (vWbp) promote Staphylococcus aureus clot formation in human plasma. J Biol Chem. 2013 Sep 27 ;288(39) :28283-92. [CrossRef]
- Nappi F, Martuscelli G, Bellomo F, Avtaar Singh SS, Moon MR Infective Endocarditis in High-Income Countries. Metabolites. 2022 Jul 25 ;12(8) :682. [CrossRef]
- Thomas S, Liu W, Arora S, Ganesh V, Ko YP, Höök. The Complex Fibrinogen Interactions of the Staphylococcus aureus Coagulases. Front Cell Infect Microbiol. 2019 Apr 16 ;9 :106. [CrossRef]
- Sinha B, Herrmann M. Mechanism and consequences of invasion of endothelial cells by Staphylococcus aureus. Thromb Haemost. 2005 Aug ;94(2) :266-77. [CrossRef]
- Thuny F, Di Salvo G, Belliard O, Avierinos JF, Pergola V, Rosenberg V, Casalta JP, Gouvernet J, Derumeaux G, Iarussi D, Ambrosi P, Calabró R, Riberi A, Collart F, Metras D, Lepidi H, Raoult D, Harle JR, Weiller PJ, Cohen A, Habib G.. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation 2005 ;112 :69-75. [Erratum, Circulation 2005 ;112(9) : e125.
- Di Salvo G, Habib G, Pergola V, Avierinos JF, Philip E, Casalta JP, Vailloud JM, Derumeaux G, Gouvernet J, Ambrosi P, Lambert M, Ferracci A, Raoult D, Luccioni R. Echocardiography predicts embolic events in infective endocarditis. J Am Coll Cardiol 2001 ;37 :1069-76. [CrossRef]
- Vilacosta I, Graupner C, San Román JA, Sarriá C, Ronderos R, Fernández C, Mancini L, Sanz O, Sanmartín JV, Stoermann W. Risk of embolization after institution of antibiotic therapy for infective endocarditis. J Am Coll Cardiol. 2002 May 1 ;39(9) :1489-95. [CrossRef]
- Nappi F, Spadaccio C, Dreyfus J, Attias D, Acar C, Bando K. Mitral endocarditis: A new management framework. J Thorac Cardiovasc Surg. 2018 Oct ;156(4) :1486-1495.e4. [CrossRef]
- Avtaar Singh SS, Costantino MF, D'Addeo G, Cardinale D, Fiorilli R, Nappi F. A narrative review of diagnosis of infective endocarditis-imaging methods and comparison. Ann Transl Med. 2020 Dec ;8(23) :1621. [CrossRef]
- Duval X, Iung B, Klein I, Thabut G, Arnoult F, Lepage L, Laissy JP, Wolff M, Leport C; IMAGE (Resonance Magnetic Imaging at the Acute Phase of Endocarditis) Study Group.. Effect of early cerebral magnetic resonance imaging on clinical decisions in infective endocarditis: a prospective study. Ann Intern Med 2010 ;152 :497-504.
- Béraud G, Tubiana S, Erpelding ML, Le Moing V, Chirouze C, Gorenne I, Manchon P, Tattevin P, Vernet V, Varon E, Hoen B, Duval X; AEPEI study group; COMBAT study group. . Combined Bacterial Meningitis and Infective Endocarditis: When Should We Search for the Other When Either One is Diagnosed? Infect Dis Ther. 2022 May 26.
- Vitali P, Savoldi F, Segati F, Melazzini L, et al. MRI versus CT in the detection of brain lesions in patients with infective endocarditis before or after cardiac surgery. Neuroradiology. 2022 May ;64(5) :905-913. [CrossRef]
- Corr P, Wright M, Handler LC. Endocarditis- related cerebral aneurysms: radiologic changes with treatment. AJNR Am J Neuroradiol 1995 ;16 :745-8.
- 24. Champey J, Pavese P, Bouvaist H, Maillet M, Kastler A, Boussat B, Francois P; and the investigator groups. Is brain angio-MRI useful in infective endocarditis management ? Eur J Clin Microbiol Infect Dis. 2016 Dec ;35(12) :2053-2058.
- Peters PJ, Harrison T, Lennox JL. A dangerous dilemma: management of infectious intracranial aneurysms complicating endocarditis. Lancet Infect Dis 2006 ;6 :742-8. [CrossRef]
- Serrano F, Guédon A, Saint-Maurice JP, et al. Endovascular treatment of infectious intracranial aneurysms complicating infective endocarditis: a series of 31 patients with 55 aneurysms. Neuroradiology. 2022 Feb ;64(2) :353-360. [CrossRef]
- Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falcó V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH ; International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. . Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009; 169: 463–73.
- Liaqat W, Palaiodimos L, Li W, Karamanis D, Tahir A, Tzoumas A, Nagraj S, Tiwari N, Grushko M, Kokkinidis D, Gashi E, Leider J, Coyle C, Faillace RT. Epidemiologic and clinical characteristics of infective endocarditis: a single-center retrospective study in the Bronx, New York. Infection. 2022 Oct ;50(5):1349-1361. [CrossRef]
- Paul G, Ochs L, Hohmann C, Baldus S, Michels G, Meyer-Schwickerath C, Fätkenheuer G, Mader N, Wahlers T, Weber C, Jung N.. Surgical Procedure Time and Mortality in Patients with Infective Endocarditis Caused by Staphylococcus aureus or Streptococcus Species Clin Med. 2022 Apr 30 ;11(9):2538.
- Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev 2014; 27: 870–926.
- López J, Revilla A, Vilacosta I, Villacorta E, González-Juanatey C, Gómez I, Rollán MJ, San Román JA.. Definition, clinical profile, microbiological spectrum, and prognostic factors of early-onset prosthetic valve endocarditis. Eur Heart J 2007; 28: 760–65. [CrossRef]
- Alonso-Valle H, Fariñas-Alvarez C, García-Palomo JD, et al. Clinical course and predictors of death in prosthetic valve endocarditis over a 20-year period. J Thorac Cardiovasc Surg 2010; 139: 887–93. [CrossRef]
- Xu Z, Chen L, Chen X, Tang A, Huang D, Pan Q, Fang Z. Prevalence and Molecular Characterization of Methicillin-Resistant Staphylococci Recovered from Public Shared Bicycles in China. Int J Environ Res Public Health. 2022 Apr 8 ;19(8) :4492. [CrossRef]
- Argemi X, Hansmann Y, Prola K, Prévost G. Coagulase-Negative Staphylococci Pathogenomics. Int J Mol Sci. 2019 Mar 11;20(5):1215. [CrossRef]
- Chu VH, Woods CW, Miro JM, Hoen B, Cabell CH, Pappas PA, Federspiel J, Athan E, Stryjewski ME, Nacinovich F, Marco F, Levine DP, Elliott TS, Fortes CQ, Tornos P, Gordon DL, Utili R, Delahaye F, Corey GR, Fowler VG Jr; International Collaboration on Endocarditis-Prospective Cohort Study Group. the International Collaboration on Endocarditis-Prospective Cohort Study Group. Emergence of coagulase-negative staphylococci as a cause of native valve endocarditis. Clin Infect Dis 2008; 46: 232–42.
- Chu VH, Miro JM, Hoen B, Cabell CH, Pappas PA, Jones P, Stryjewski ME, Anguera I, Braun S, Muñoz P, Commerford P, Tornos P, Francis J, Oyonarte M, Selton-Suty C, Morris AJ, Habib G, Almirante B, Sexton DJ, Corey GR, Fowler VG Jr. International Collaboration on Endocarditis-Prospective Cohort Study Group. Coagulase-negative staphylococcal prosthetic valve endocarditis--a contemporary update based on the International Collaboration on Endocarditis: prospective cohort study. Heart. 2009 Apr ;95(7) :570-6. [CrossRef]
- Alawad MJ, Ali GA, Goravey W. Underrecognized pathogen; Staphylococcus warneri-associated native mitral valve endocarditis in an immunocompetent host: A case report and literature review. Clin Case Rep. 2022 Apr 22 ;10(4): e05591. [CrossRef]
- Voigt A, Shalaby A, Saba S. Rising rates of cardiac rhythm management device infections in the United States: 1996 through 2003. J Am Coll Cardiol 2006 ;48 :590–1. [CrossRef]
- Traykov V, Blomström-Lundqvist C. Antibiotic-Eluting Envelopes for the Prevention of Cardiac Implantable Electronic Device Infections: Rationale, Efficacy, and Cost-Effectiveness. Front Cardiovasc Med. 2022 Mar 28 ;9 :855233. [CrossRef]
- Elad B, Perl L, Hamdan A, Yahav D, Atamna A, Shaked H, Rubchevsky V, Sharony R, Bernstine H, Shapira Y, Vaturi M, Ofek H, Sagie A, Kornowski R, Orvin K. The clinical value of the endocarditis team: insights from before and after guidelines implementation strategy. Infection. 2022 Feb ;50(1) :57-64. [CrossRef]
- Han HC, Hawkins NM, Pearman CM, Birnie DH, Krahn AD. Epidemiology of cardiac implantable electronic device infections: incidence and risk factors. Europace. 2021 Jun 23 ;23(23 Suppl 4): iv3-iv10. [CrossRef]
- Durante-Mangoni E, Bradley S, Selton-Suty C, et al, and the International Collaboration on Endocarditis Prospective Cohort Study Group. Current features of infective endocarditis in elderly patients: results of the International Collaboration on Endocarditis Prospective Cohort Study. Arch Intern Med 2008; 168: 2095–103.
- Zampino R, Iossa D, Ursi MP, Bertolino L, Karruli A, Molaro R, Esposito G, Vitrone M, D'Amico F, Albisinni R, Durante-Mangoni E, On Behalf Of The Monaldi Hospital CardiovascularInfection Group. Clinical Significance and Prognostic Value of Hemostasis Parameters in 337 Patients with Acute Infective Endocarditis. J Clin Med. 2021 Nov 18 ;10(22) :5386. [CrossRef]
- Molton JS, Tambyah PA, Ang BSP, Ling ML, Fisher DA. The global spread of healthcare-associated multidrug-resistant bacteria: a perspective from Asia. Clin Infect Dis 2013; 56: 1310–18. [CrossRef]
- Çaǧlayan Ç, Barnes SL, Pineles LL, Harris AD, Klein EY. A Data-Driven Framework for Identifying Intensive Care Unit Admissions Colonized With Multidrug-Resistant Organisms. Front Public Health. 2022 Mar 17; 10:853757. [CrossRef]
- Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK. Bacteremia associated with toothbrushing and dental extraction. Circulation 2008; 117: 3118–25.
- Widmer E, Que YA, Entenza JM, Moreillon P. New concepts in the pathophysiology of infective endocarditis. Curr Infect Dis Rep 2006; 8: 271–79. [CrossRef]
- Moreillon P, Que YA, Bayer AS. Pathogenesis of streptococcal and staphylococcal endocarditis. Infect Dis Clin North Am. 2002 Jun ;16(2) :297-318. [CrossRef]
- Mancini S, Oechslin F, Menzi C, Que YA, Claes J, Heying R, Veloso TR, Vanassche T, Missiakas D, Schneewind O, Moreillon P, Entenza JM . Marginal role of von Willebrand factor-binding protein and coagulase in the initiation of endocarditis in rats with catheter-induced aortic vegetations. Virulence. 2018 ;9(1) :1615-1624. [CrossRef]
- Werdan K, Dietz S, Löffl B, Niemann S, Bushnaq H, Silber RE, Peters G, Müller-Werdan U.. Mechanisms of infective Endocarditis: pathogen-host interaction and risk states. Nat Rev Cardiol 2014; 11: 35–50. [CrossRef]
- Regueiro A, Linke A, Latib A, Urena M, Walther T, Husser O, Herrmann C, Nombela-Franco L, Cheema A, Le Breton H, Stortecky S, Kapadia S, Bartorelli L, Sinning JM, Amat-Santos I, Munoz-Garcia J, Lerakis S, Gutíerrez-Ibanes E, Abdel-Wahab M, Tchetche D, Testa L, Eltchaninoff H, et al. Infective Endocarditis Following Transcatheter Aortic Valve Replacement: Comparison of Balloon- Versus Self-Expandable Valves. Circ Cardiovasc Interv. 2019 Nov ;12(11): e007938.
- Rodríguez-Vidigal FF, Nogales-Asensio JM, Calvo-Cano A, et al. Infective endocarditis after transcatheter aortic valve implantation: Contributions of a single-centre experience on incidence and associated factors. Enferm Infecc Microbiol Clin (Engl Ed). 2019 Aug-Sep ;37(7):428-434. [CrossRef]
- Ciofu O, Moser C, Jensen PØ, Høiby N Tolerance and resistance of microbial biofilms. Nat Rev Microbiol. 2022 Feb 3.
- Annappah D, Saling M, Prodafikas J, Badie AN. Device-associated aortic valve endocarditis due to a complicated Enterobacter cloacae urinary tract infection. ID Cases. 2021 Dec 16 ;27: e01365. [CrossRef]
- Di Carluccio C, Forgione RE, Bosso A, et al.. Molecular recognition of sialoglycans by streptococcal Siglec-like adhesins: toward the shape of specific inhibitors. RSC Chem Biol. 2021 Oct 18 ;2(6) :1618-1630. [CrossRef]
- Manukumar H.M., Umesha S. MALDI-TOF-MS based identification and molecular characterization of food associated methicillin-resistant Staphylococcus aureus. Sci Rep. 2017 Sep 12 ;7(1) :11414. [CrossRef]
- Mempel M., Schnopp C., Hojka M, et al. Invasion of human keratinocytes by Staphylococcus aureus and intracellular bacterial persistence represent haemolysin-independent virulence mechanisms that are followed by features of necrotic and apoptotic keratinocyte cell death. Br J Dermatol. 2002 Jun ;146(6) :943-51. [CrossRef]
- Nakagawa S, Matsumoto M., Katayama, Y, et al. Staphylococcus aureus virulent PSMα peptides induce keratinocyte alarmin release to orchestrate IL-17-dependent skin inflammation. Cell Host Microbe 22, 667–677. 2017 Nov 8 ;22(5) :667-677.e5. [CrossRef]
- Fournier, B., Philpott, D.J. Recognition of Staphylococcus aureus by the innate immune system. Clin. Microbiol. Rev. 2005 Jul ;18(3) :521-40.
- Kawa T, Akira S. The role of pattern-recognition receptors in innate immunity: update on toll-like receptors. Nat. Immunol. 2010 May ;11(5) :373-84.
- Kupper T.S, Fuhlbrigge R.C. Immune surveillance in the skin: mechanisms and clinical consequences. Nat. Rev. Immunol. 2004 Mar ;4(3) :211-22. [CrossRef]
- Nestle F.O, Di M.P, Qin, J.Z., Nickoloff, B.J. Skin immune sentinels in health and disease. Nat. Rev. Immunol. 2009 Oct ;9(10) :679-91. [CrossRef]
- Schwarz C, Töre Y, Hoesker V, et al. Host-pathogen interactions of clinical S. aureus isolates to induce infective endocarditis. Virulence. 2021 Dec ;12(1) :2073-2087.
- 64. Malachowa N, Whitney A.R., Kobayashi S.D, et al. Global changes in Staphylococcus aureus gene expression in human blood. PLoS One 6, e18617. 2011 Apr 15 ;6(4) : e18617. [CrossRef]
- Alonzo 3rd F, Kozhaya, L., Rawlings S.A, et al. CCR5 is a receptor for Staphylococcus aureus leukotoxin ED. Nature 2013 Jan 3 ;493(7430):51-5.
- Alonzo 3rd F, Torres V.J. Bacterial survival amidst an immune onslaught: the contribution of the Staphylococcus aureus leukotoxins. PLoS Pathog. 2013 Feb ;9(2) : e1003143.
- Cheung G.Y, Joo H.S, Chatterjee S.S. et al. Phenol-soluble modulins–critical determinants of staphylococcal virulence. FEMS Microbiol. Rev. 2014 Jul ;38(4) :698-719. [CrossRef]
- Berube BJ, Bubeck Wardenburg J. Staphylococcus aureus α-toxin: nearly a century of intrigue. Toxins (Basel). 2013 Jun ;5(6) :1140-66. [CrossRef]
- Foster TJ. Immune evasion by staphylococci. Nat Rev Microbiol. 2005 Dec ;3(12) :948-58. [CrossRef]
- Silverman GJ, Goodyear CS. Confounding B-cell defences: lessons from a staphylococcal superantigen. Nat Rev Immunol. 2006 Jun ;6(6) :465-75. [CrossRef]
- Kim HK, Cheng AG, Kim HY, Missiakas DM, Schneewind O. Nontoxigenic protein A vaccine for methicillin-resistant Staphylococcus aureus infections in mice. J Exp Med. 2010 Aug 30 ;207(9) :1863-70. [CrossRef]
- Becker S, Frankel MB, Schneewind O, Missiakas D. Release of protein A from the cell wall of Staphylococcus aureus. Proc Natl Acad Sci U S A. 2014 Jan 28 ;111(4) :1574-9. [CrossRef]
- Zhang X, Marichannegowda MH, Rakesh KP, Qin HL. Master mechanisms of Staphylococcus aureus: consider its excellent protective mechanisms hindering vaccine development! Microbiol Res. 2018 Jul-Aug ;212-213 :59-66.
- Zhang BZ, Hua YH, Yu B, Cai JP, Zheng SY, Yam WC, Kao RY, Sze KH, Zheng BJ, Yuen KY, Huang JD. Recombinant ESAT-6-like proteins provoke protective immune responses against invasive Staphylococcus aureus disease in a murine model. Infect Immun. 2015 Jan ;83(1) :339-45. [CrossRef]
- Brady RA, Mocca CP, Prabhakara R, Plaut RD, Shirtliff ME, Merkel TJ, Burns DL. Evaluation of genetically inactivated alpha toxin for protection in multiple mouse models of Staphylococcus aureus infection. PLoS One. 2013 Apr 29 ;8(4): e63040. [CrossRef]
- Zhang F, Ledue O, Jun M, Goulart C, Malley R, Lu YJ. Protection against Staphylococcus aureus Colonization and Infection by B- and T-Cell-Mediated Mechanisms. mBio. 2018 Oct 16 ;9(5): e01949-18. [CrossRef]
- Yu W, Yao D, Yu S, Wang X, Li X, Wang M, Liu S, Feng Z, Chen X, Li W, Wang L, Liu W, Ma J, Yu L, Tong C, Song B, Cui Y. Protective humoral and CD4+ T cellular immune responses of Staphylococcus aureus vaccine MntC in a murine peritonitis model. Sci Rep. 2018 Feb 26 ;8(1) :3580. [CrossRef]
- Que Y-A, Haefliger J-A, Piroth L, François P, Widmer E, Entenza JM, Sinha B, Herrmann M, Francioli P, Vaudaux P, Moreillon P. Fibrinogen and fibronectin binding cooperate for valve infection and invasion in Staphylococcus aureus experimental endocarditis. J Exp Med 2005; 201: 1627–35. [CrossRef]
- Edwards AM, Bowden MG, Brown EL, Laabei M, Massey RC. Staphylococcus aureus extracellular adherence protein triggers TNFα release, promoting attachment to endothelial cells via protein A. PLoS One 2012; 7: e43046.
- Fitzgerald JR, Foster TJ, Cox D. The interaction of bacterial pathogens with platelets. Nat Rev Microbiol 2006; 4: 445–57.
- Veloso TR, Chaouch A, Roger T, Giddey M, Vouillamoz J, Majcherczyk P, Que YA, Rousson V, Moreillon P, Entenza JM. Use of a human-like low-grade bacteremia model of experimental endocarditis to study the role of Staphylococcus aureus adhesins and platelet aggregation in early endocarditis. Infect Immun 2013; 81: 697–703. [CrossRef]
- Thomas S, Arora S, Liu W, Churion K, Wu Y, Höök M. vhp Is a Fibrinogen-Binding Protein Related to vWbp in Staphylococcus aureus. mBio. 2021 Aug 31 ;12(4): e0116721. [CrossRef]
- Hussain M, Haggar A, Heilmann C, et al. Insertional inactivation of Eap in Staphylococcus aureus strain Newman confers reduced staphylococcal binding to fibroblasts. Infect Immun. 2002 Jun ;70(6) :2933-40. [CrossRef]
- Palankar R, Binsker U, Haracska B, et al. Interaction between the Staphylococcus aureus extracellular adherence protein Eap and its subdomains with platelets. Int J Med Microbiol. 2018 Aug ;308(6):683-691. [CrossRef]
- Hussain M, Haggar A, Peters G, et al. More than one tandem repeat domain of the extracellular adherence protein of Staphylococcus aureus is required for aggregation, adherence, and host cell invasion but not for leukocyte activation. Infect Immun. 2008 Dec ;76(12) :5615-23.
- Harraghy N, Hussain M, Haggar A, et al. The adhesive and immunomodulating properties of the multifunctional Staphylococcus aureus protein Eap. Microbiology (Reading). 2003 Oct ;149(Pt 10):2701-2707. [CrossRef]
- Flemming H-C, Wingender J. The biofilm matrix. Nat Rev Microbiol 2010; 8: 623–33.
- Heying R, van de Gevel J, Que YA, Moreillon P, Beekhuizen H Fibronectin-binding proteins and clumping factor A in Staphylococcus aureus experimental endocarditis: FnBPA is sufficient to activate human endothelial cells. Thromb Haemost. 2007 Apr ;97(4) :617-26.
- Piroth L, Que YA, Widmer E, et al. The fibrinogen- and fibronectin-binding domains of Staphylococcus aureus fibronectin-binding protein A synergistically promote endothelial invasion and experimental endocarditis. Infect Immun. 2008 Aug ;76(8) :3824-31. [CrossRef]
- Claes J, Vanassche T, Peetermans M, et al. Adhesion of Staphylococcus aureus to the vessel wall under flow is mediated by von Willebrand factor-binding protein. Blood. 2014 Sep 4 ;124(10) :1669-76. [CrossRef]
- Pappelbaum KI, Gorzelanny C, Grässle S, et al. Ultralarge von Willebrand factor fibers mediate luminal Staphylococcus aureus adhesion to an intact endothelial cell layer under shear stress. Circulation. 2013 Jul 2 ;128(1):50-9. [CrossRef]
- Claes J, Liesenborghs L, Peetermans M, et al. Clumping factor, A, von Willebrand factor-binding protein and von Willebrand factor anchor Staphylococcus aureus to the vessel wall. J Thromb Haemost. 2017 May ;15(5) :1009-1019.
- Claes J, Ditkowski B, Liesenborghs L, et al. Assessment of the Dual Role of Clumping Factor A in S. Aureus Adhesion to Endothelium in Absence and Presence of Plasma. Thromb Haemost. 2018 Jul ;118(7) :1230-1241. [CrossRef]
- Ko YP, Kang M, Ganesh VK, Ravirajan D, Li B, Höök M. Coagulase and Efb of Staphylococcus aureus Have a Common Fibrinogen Binding Motif. mBio. 2016 Jan 5 ;7(1) : e01885-15. [CrossRef]
- Foster TJ. The remarkably multifunctional fibronectin binding proteins of Staphylococcus aureus. Eur J Clin Microbiol Infect Dis. 2016 Dec ;35(12) :1923-1931. [CrossRef]
- Ahmed S, Meghji S, Williams RJ, Henderson B, Brock JH, Nair SP. Staphylococcus aureus fibronectin binding proteins are essential for internalization by osteoblasts but do not account for differences in intracellular levels of bacteria. Infect Immun. 2001 May ;69(5) :2872-7. [CrossRef]
- Massey RC, Kantzanou MN, Fowler T, Day NP, Schofield K, Wann ER, Berendt AR, Höök M, Peacock SJ.. Fibronectin-binding protein A of Staphylococcus aureus has multiple, substituting, binding regions that mediate adherence to fibronectin and invasion of endothelial cells. Cell Microbiol. 2001 Dec ;3(12) :839-51. [CrossRef]
- Ridley RA, Douglas I, Whawell SA. Differential adhesion and invasion by Staphylococcus aureus of epithelial cells derived from different anatomical sites. J Med Microbiol. 2012 Dec ;61(Pt 12) :1654-1661. [CrossRef]
- Niemann S, Nguyen MT, Eble JA, Chasan AI, Mrakovcic M, Böttcher RT, Preissner KT, Roßlenbroich S, Peters G, Herrmann M. More Is Not Always Better-the Double-Headed Role of Fibronectin in Staphylococcus aureus Host Cell Invasion. mBio. 2021 Oct 26 ;12(5): e0106221. [CrossRef]
- Pietrocola G, Pellegrini A, Alfeo MJ, Marchese L, Foster TJ, Speziale P.. The iron-regulated surface determinant B (IsdB) protein from Staphylococcus aureus acts as a receptor for the host protein vitronectin. J Biol Chem. 2020 Jul 17 ;295(29) :10008-10022. [CrossRef]
- Alfeo MJ, Pagotto A, Barbieri G, Foster TJ, Vanhoorelbeke K, De Filippis V, Speziale P, Pietrocola G. Staphylococcus aureus iron-regulated surface determinant B (IsdB) protein interacts with von Willebrand factor and promotes adherence to endothelial cells. Sci Rep. 2021 Nov 23 ;11(1) :22799. [CrossRef]
- Leeten K, Jacques N, Lancellotti P, Oury C Aspirin or Ticagrelor in Staphylococcus aureus Infective Endocarditis: Where Do We Stand? Front Cell Dev Biol. 2021 Oct 7 ;9 :716302.
- Ditkowski B, Bezulska-Ditkowska M, Jashari R, et al Antiplatelet therapy abrogates platelet-assisted Staphylococcus aureus infectivity of biological heart valve conduits. Congenital Cardiology and Cardiac Surgery Group. J Thorac Cardiovasc Surg. 2021 Jun ;161(6): e457-e472.
- Hannachi N, Habib G, Camoin-Jau L Aspirin Effect on Staphylococcus aureus-Platelet Interactions During Infectious Endocarditis. Front Med (Lausanne). 2019 Oct 15 ;6 :217.
- Park, E. Na HS, Song YR, Shin SY, Kim YM, Chung J. Activation of NLRP3 and AIM2 inflammasomes by Porphyromonas gingivalis infection. Infect Immun. 2014 Jan ;82(1):112-23. [CrossRef]
- Schwartz FA, Christophersen L, Laulund AS, Lundquist R, Lerche C, Rude Nielsen P, Bundgaard H, Høiby N, Moser C. Novel human in vitro vegetation simulation model for infective endocarditis. APMIS. 2021 Nov ;129(11) :653-662. [CrossRef]
- Di Domenico EG, Rimoldi SG, Cavallo I et al. Microbial biofilm correlates with an increased antibiotic tolerance and poor therapeutic outcome in infective endocarditis. BMC Microbiol. 2019 Oct 21 ;19(1) :228. [CrossRef]
- Schwartz FA, Nielsen L, Struve Andersen J, Bock M, Christophersen L, Sunnerhagen T, Lerche CJ, Bay L, Bundgaard H, Høiby N, Moser C. Dynamics of a Staphylococcus aureus infective endocarditis simulation model. APMIS. 2022 Apr 23. [CrossRef]
- Nappi F, Avtaar Singh SS, Timofeeva I. Learning From Controversy: Contemporary Surgical Management of Aortic Valve Endocarditis. Clin Med Insights Cardiol. 2020 Sep 28 ;14 :1179546820960729. [CrossRef]
- Nappi F, Singh SSA, Nappi P, Spadaccio C, Nenna A, Gentile F, Chello M. Heart Valve Endocarditis. Surg Technol Int. 2020 Nov 28 ;37 :203-215.
- Nappi F, Singh SSA, Spadaccio C, Acar C. Revisiting the guidelines and choice the ideal substitute for aortic valve endocarditis. Ann Transl Med. 2020 Aug;8(15):952. [CrossRef]
- Nappi F, Iervolino A, Singh SSA. The New Challenge for Heart Endocarditis: From Conventional Prosthesis to New Devices and Platforms for the Treatment of Structural Heart Disease. Biomed Res Int. 2021 Jun 14; 2021:7302165. doi: 10.1155/2021/7302165. eCollection 2021. [CrossRef]
- Kim JB, Ejiofor JI, Yammine M, Camuso JM, Walsh CW, Ando M, et al. The Journal of Thoracic and Cardiovascular Surgery. 2016;151(5):1239-48. e2. [CrossRef]
- Perrotta S, Jeppsson A, Fröjd V, Svensson G. Surgical Treatment of Aortic Prosthetic Valve Endocarditis: A 20-Year Single-Center Experience. The Annals of Thoracic Surgery. 2016;101(4):1426-32. [CrossRef]
- David TE, Gavra G, Feindel CM, Regesta T, Armstrong S, Maganti MD. Surgical treatment of active infective endocarditis: a continued challenge. J Thorac Cardiovasc Surg. 2007;133(1):144-9.
- Nappi F, Spadaccio C, Acar C. Use of allogeneic tissue to treat infective valvular disease: Has everything been said? J Thorac Cardiovasc Surg. 2017;153(4):824-8.
- Brouqui P, Raoult D. Endocarditis due to rare and fastidious bacteria. Clin Microbiol Rev. 2001;14(1):177-207.
- Kim JB, Ejiofor JI, Yammine M, Ando M, Camuso JM, Youngster I, et al. Surgical outcomes of infective endocarditis among intravenous drug users. The Journal of Thoracic and Cardiovascular Surgery. 2016;152(3):832-41. e1. [CrossRef]
- Nappi F, Spadaccio C. Simplest solutions are not always the cleverest: Can we stitch in an infected annulus? Should we rethink the current guidelines? J Thorac Cardiovasc Surg. 2017;154(6):1899-900.
- Nappi F, Nenna A, Petitti T, Spadaccio C, Gambardella I, Lusini M, et al. Long-term outcome of cryopreserved allograft for aortic valve replacement. J Thorac Cardiovasc Surg. 2018 ;156(4) :1357-65 e6. [CrossRef]
- Arabkhani B, Bekkers JA, Andrinopoulou E-R, Roos-Hesselink JW, Takkenberg JJM, Bogers AJJC. Allografts in aortic position: Insights from a 27-year, single-center prospective study. The Journal of Thoracic and Cardiovascular Surgery. 2016;152(6):1572-9. e3. [CrossRef]
- Nappi F. CRT-721 The Cryopreserved Mitral Homograft Valve: 19 Years’ Experience. JACC: Cardiovascular Interventions. 2014;7(2 Supplement): S58. [CrossRef]
- Fukushima S, Tesar PJ, Pearse B, Jalali H, Sparks L, Fraser JF, et al. Long-term clinical outcomes after aortic valve replacement using cryopreserved aortic allograft. J Thorac Cardiovasc Surg. 2014;148(1):65-72. e2. [CrossRef]
- O'Brien MF, Harrocks S, Stafford EG, Gardner MA, Pohlner PG, Tesar PJ, et al. The homograft aortic valve: a 29-year, 99.3% follow up of 1,022 valve replacements. J Heart Valve Dis. 2001;10(3):334-44; discussion 5.
- Olivito S, Lalande S, Nappi F, Hammoudi N, D'Alessandro C, Fouret P, et al. Structural deterioration of the cryopreserved mitral homograft valve. J Thorac Cardiovasc Surg. 2012;144(2):313-20, 20.e1. [CrossRef]
- Nappi F, Singh SSA, Lusini M, Nenna A, Gambardella I, Chello M. The use of allogenic and autologous tissue to treat aortic valve endocarditis. Annals of Translational Medicine. 2019;7(18):68. [CrossRef]
- Nappi F, Acar C. Monobloc or Separate Aortic and Mitral Homografts for Endocarditis of the Intervalvular Fibrosa? Ann Thorac Surg. 2021 Oct;112(4):1382-1383. [CrossRef]
- Nappi F, Spadaccio C, Moon MR A management framework for left sided endocarditis: a narrative review. Ann Transl Med. 2020 Dec;8(23):1627. [CrossRef]
- Benedetto U, Spadaccio C, Gentile F, Moon MR, Nappi F. A narrative review of early surgery versus conventional treatment for infective endocarditis: do we have an answer? Ann Transl Med. 2020 Dec;8(23):1626. [CrossRef]
- Pollari F, Spadaccio C, Cuomo M, Chello M, Nenna A, Fischlein T, Nappi F. Sharing of decision-making for infective endocarditis surgery: a narrative review of clinical and ethical implications. Ann Transl Med. 2020 Dec;8(23):1624. [CrossRef]
- Steffen V, Marsch G, Burgwitz K, Kuehn C, Teebken OE. Resistance to infection of long-term cryopreserved human aortic valve allografts. J Thorac Cardiovasc Surg. 2016;151(5):1251-9. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





