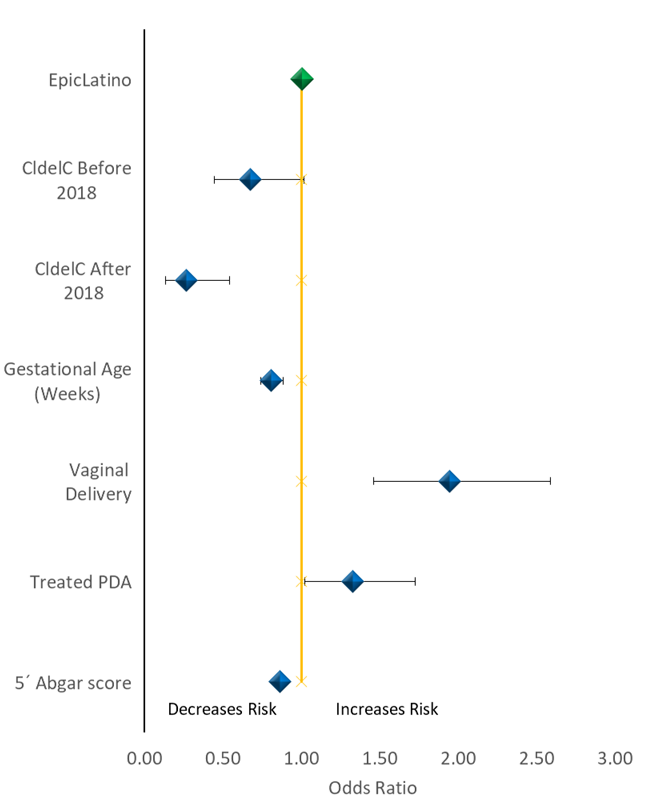
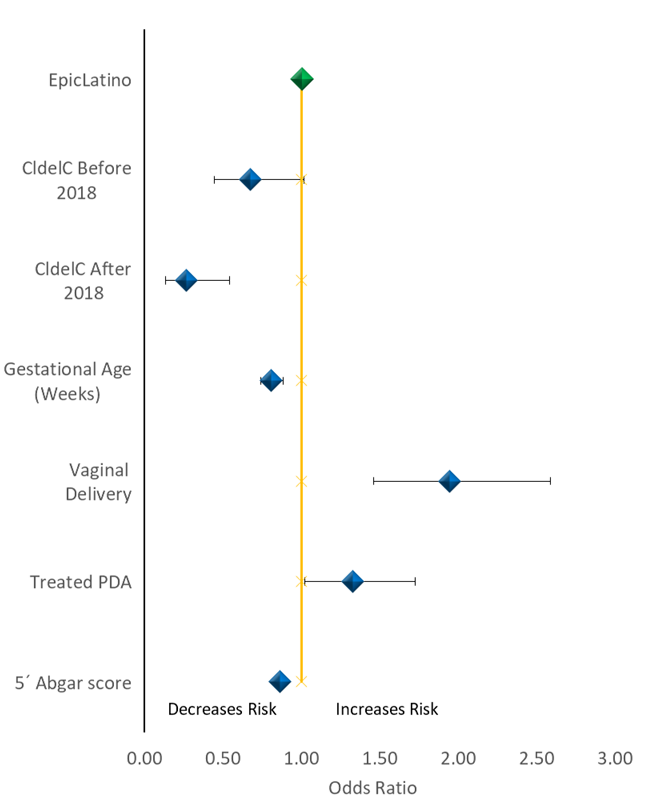
Introduction: Intraventricular Hemorrhage (IVH) is a devastating condition mostly in preterm infants at < 30 weeks GA with large morbidities and mortality usually in the first 72 hours after birth. Prevention seems to be the only way to completely deal with this problem. The IVH prevention in this age group has been studied and includes some strategies such as prenatal corticosteroids, cesarean delivery, careful extraction among others, but still, it has an unacceptably high incidence in this population. A protocol with the name Drive to Zero IVH Prevention Project that was presented in one of EpicLatino conferences some years ago. As with any quality improvement in practices, we adapted this project to our unit. Objective: To compare the IVH incidence in our unit after the protocol implementation with and historic cohort from the same unit and with all other units un the epilactino network. Material and method: In October 2017 we begun to implement a neuro protection protocol. For this analysis we include every patient born <30 weeks of GA, inborn or outborn but less than 2 days old, that survived at least three days and had a neuroimaging preformed. We include cases until July 2022, and we use the EpicLatino, a Latin-American database, from 2018 to 2020 excluding our own unit for comparison as well as an historical cohort from our unit from 2010-2017. The protocol consists of: Minimal manipulation, low volume ventilation, one routine fiscal exam a day, neutral head position, one blood pressure measured per shift, no keel stick measurements, continuous dim light and low noise level, minimal touch, no vasoactive therapy except in extreme cases, temperature and humidity at 80%, catheters, when possible, fluid restriction followed with diuresis, no PDA therapy or Echo if possible and routine therapy with hydrocortisone, erythropoietin, caffeine, parenteral nutrition, and trophic feeding. e performed a univariate analysis for IVH and groups and a logistic regression model with variables that had statistical significance in the univariate analysis. Results: The study group included 64 cases, the historic cohort 123 and the EpicLatino 1029. Demographic characteristics were similar with few statistically significant differences. We found four grade 1-2 and six grade 3-4 IVH in the study group (some caused by very traumatic delivery with multiples hematomas in head, body, and extremities), all significantly lower that the other two groups. The logistic regression model confirmed the independent statistically significant result in the study group. Conclusion: The hemorrhage during delivery must be prevented by the obstetric team. Afterwards, a set of interventions like very gentle handling with minimal manipulation and unnecessary strict lab managing seams to decrease the incidence of IVH.