1. Introduction
Multiple sclerosis (MS) is a chronic, immune-mediated neurological disease characterized by demyelination and progressive disability, affecting more than 2.8 million people worldwide [
1]. Individuals living with MS face a wide spectrum of physical, cognitive, and psychosocial challenges that may compromise daily functioning and work capacity. Occupational participation is therefore a significant component of quality of life in this population, yet it is frequently threatened by disease progression, fatigue, heat sensitivity, and workplace-related stressors [
2,
3].
The emergence of the coronavirus disease 2019 (COVID-19) pandemic introduced additional layers of vulnerability for people with MS: concerns rapidly developed around susceptibility to SARS-CoV-2 infection, severity of COVID-19 in MS patients (especially those on disease-modifying therapies), and disruptions in healthcare access [
4,
5]. Alongside clinical risks, the pandemic also reshaped working conditions globally, with frontline occupations, essential services, and remote-work transitions exerting varied and sometimes unequal effects on individuals with chronic illnesses [
6,
7,
8,
9].
Occupational hazards during the COVID-19 era encompass both biological risks (exposure to SARS-CoV-2), and non-biological stressors, including intensified workloads, psychosocial strain, inadequate workplace accommodations, and disparities in occupational protection [
10]. For individuals with MS, such hazards may interact with pre-existing disease-related vulnerabilities, potentially influencing relapse rates, symptom burden, mental health, and employment stability. Despite growing attention to these challenges, evidence remains fragmented and has not been comprehensively synthesized across epidemiological, clinical, and occupational research [
11,
12,
13].
Understanding the intersection of MS, COVID-19, and occupational hazards is essential for informing workplace policies, guiding clinical decision-making, and identifying risk mitigation strategies tailored to vulnerable populations. While previous reviews have focused on clinical outcomes of COVID-19 in MS patients or on general employment barriers in MS, no scoping review has specifically integrated these domains [
13,
14,
15].
Previous works on occupational outcomes in people with MS during COVID-19 offers useful employment-related estimates but remains limited by its narrow scope, exclusion of qualitative and mixed-methods studies. They focus mainly on employment status and remote work, without addressing broader occupational hazards such as psychological stress, workplace safety, infection risk, or post-pandemic trajectories, and lacks an integrative clinical–occupational perspective. To fill these gaps, this scoping review maps the wider evidence across clinical, psychosocial, and occupational domains, including post-pandemic outcomes and diverse study designs.
Therefore, the aim of this scoping review is to synthesize and map the full range of occupational exposures, workplace experiences, and employment outcomes among individuals with MS during and beyond the COVID-19 era. By integrating qualitative and quantitative evidence across multiple disciplines, this review seeks to identify key risk patterns, highlight research gaps, and inform future policy and clinical decision-making.
2. Methods
2.1. Data Sources and Search Strategy
A review is conducted following the (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines [
16], to systematically map the literature on MS in the context of the COVID-19 pandemic, with a focus on occupational hazards, including infection exposure, workplace conditions, psychological stressors, and employment outcomes.
A literature search was conducted using electronic academic databases including PubMed, Scopus, and Web of Science to retrieve peer-reviewed articles published from January 2020 to the present. The following search terms were employed: (“occupation”, “Employ”, “work”, “vocation”, “workplace”, “workforce”, “labour force”, “labor force”, “Career”, “Job”, “worker”, “fitness for work”, “Multiple sclerosis”, “Demyelinating Autoimmune Diseases”, “Demyelinating Autoimmune Disorders”, “Clinically Isolated Syndrome”, “Demyelinating”, “SARS-CoV-2”, “COVID-19”, “Coronavirus disease 2019” using AND/OR Boolean operators.
Reference lists of the included publications were reviewed to identify any additional studies not captured in the database searches, and duplicates or irrelevant records were removed. Two reviewers independently screened the titles and abstracts of all retrieved articles and conducted full-text assessments to determine eligibility.
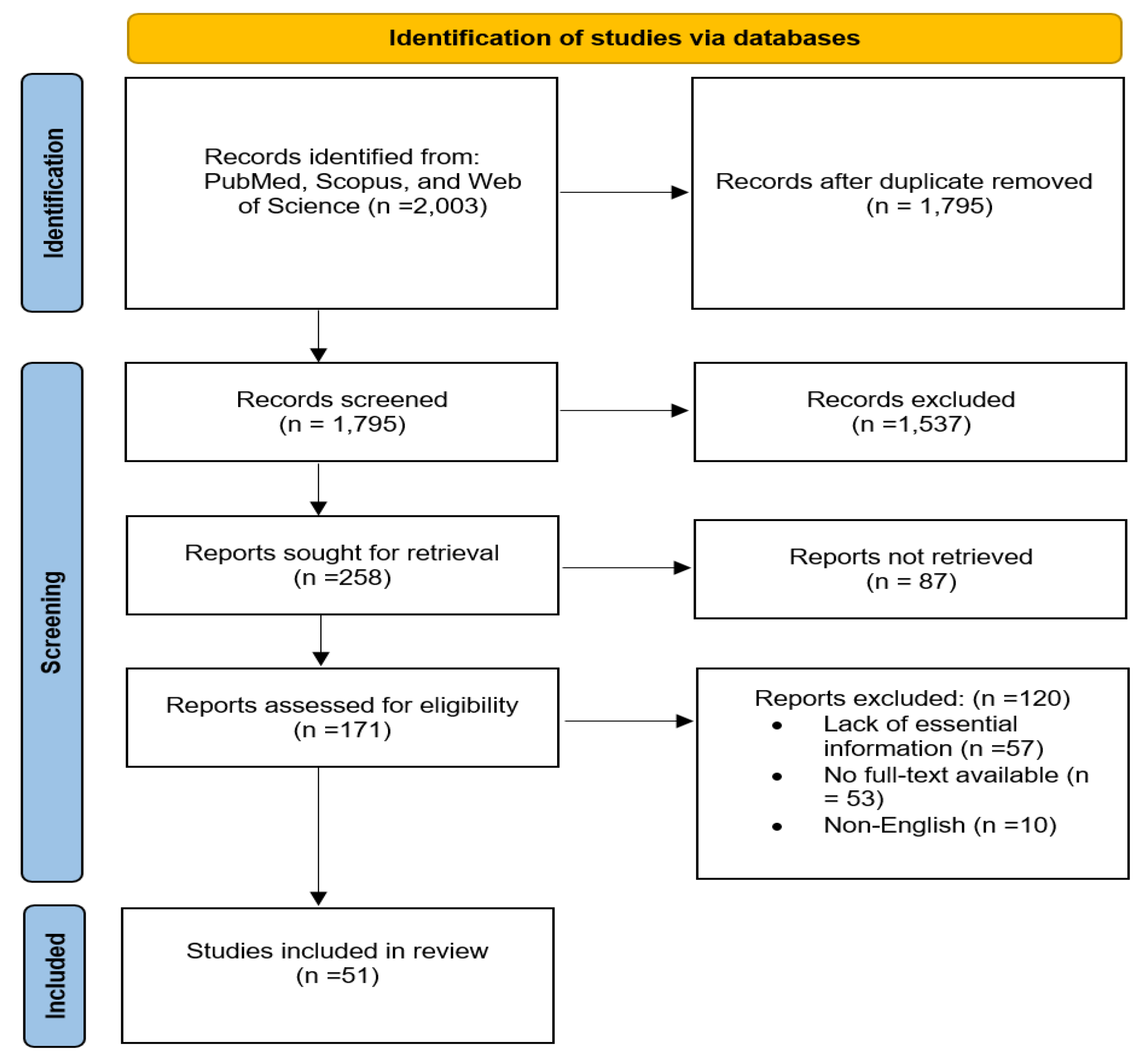
Figure 1.
PRISMA flow diagram of the study design process.
Figure 1.
PRISMA flow diagram of the study design process.
2.2. Eligibility Criteria
Studies were included if they: 1) involved individuals diagnosed with MS; 2) reported on occupational outcomes or workplace-related exposures during the COVID-19 pandemic; and 3) were published in English. We excluded editorials, conference abstracts without full data, animal studies, and studies not addressing occupational or work-related outcomes.
2.3. Screening and Data Extraction
Two reviewers independently screened titles and abstracts, followed by full-text assessment for eligibility. Discrepancies were resolved through discussion or consultation with a third reviewer. A standardized data extraction form was used to collect study characteristics (author, year, country, study design, sample size), MS-related variables (disease type, disability), occupational outcomes (employment status, workplace accommodations, psychosocial stressors), and COVID-19-related exposures or outcomes.
3. Results
3.1. Study Selection and Characteristics
A total of 51 studies, encompassing 18,379 patients with multiple sclerosis (PwMS), were included in this review. The studies varied widely in design, including cross-sectional surveys, retrospective analyses, and a few longitudinal cohorts, and spanned multiple countries and healthcare contexts. Most studies focused on psychological outcomes, social/environmental triggers, and occupational or work-related consequences during the COVID-19 pandemic.
3.2. Psychological Outcomes and Work-Related Implications
The included studies consistently reported that PwMS experienced substantial psychological burden during the pandemic. Depressive symptoms remained prevalent or increased compared with pre-pandemic estimates, stress levels generally escalated, and anxiety outcomes were mixed some studies showed increased anxiety, while others suggested reductions, likely reflecting variations in measurement instruments or pandemic phases. These mental health impacts have direct occupational relevance, as depression, stress, and anxiety are known to impair work performance, increase absenteeism, and reduce overall employment participation in MS populations. Several studies also suggested that changes in workplace conditions, including shifts to remote work, altered workloads, or reduced on-site support, interacted with psychological strain to exacerbate occupational challenges. Collectively, the evidence indicates that pandemic-related employment effects were likely mediated by both increased psychosocial burden and structural workplace changes.
3.3. Social, Environmental, and Socioeconomic Factors
Stressful life events, including economic insecurity, job loss, and other pandemic-related social disruptions, were commonly reported as triggers affecting both disease trajectories and occupational stability. While some studies focused on triggers for MS onset, the findings underscore the interplay between broader socioeconomic context and employment outcomes. In particular, financial strain and job insecurity during the pandemic may have amplified clinical vulnerability, reduced return-to-work capacity, and heightened occupational instability. This emphasizes that pandemic effects on work cannot be considered in isolation from macro-level social and economic conditions.
3.4. Heterogeneity, Study Designs, and Quality Considerations
Several limitations were recurrent across studies. First, cross-sectional designs predominated, limiting causal inference about the direct effects of pandemic exposures on occupational outcomes. Pre-existing factors such as disease severity, comorbidities, and socioeconomic status may have influenced both psychological strain and employment changes. Second, there was substantial heterogeneity in study outcomes, measurement instruments, and timing (early versus later pandemic stages), complicating synthesis and limiting generalizability. Some studies reported wide variability in psychological effect sizes, while others highlighted the influence of local socioeconomic factors that may not be generalizable internationally.
3.5. Synthesis: Implications for Occupational Hazards and Research Gaps
Overall, the evidence indicates that PwMS faced significant employment disruption during the COVID-19 pandemic, with high prevalence of job loss, retirement, or other changes in work status. Psychological stress and mental health challenges were common and likely contributed to reduced occupational functioning. Pandemic-related socioeconomic stressors acted both as triggers for clinical deterioration in susceptible individuals and as drivers of workplace instability. Notably, the current literature largely neglects workplace-level hazards, including occupation-specific infection risk, adequacy of employer accommodations, and effectiveness of return-to-work programs. There is also limited integration of qualitative evidence on the lived experiences of PwMS in the workplace. These gaps justify further scoping research that combines clinical, psychosocial, occupational-exposure, policy, and qualitative evidence to comprehensively understand occupational hazards and resilience among PwMS during pandemic conditions.
Table 1 summarizes the main psychological, occupational, and social outcomes reported across the included studies. The table highlights the prevalence of mental health impacts, work-related disruptions, and socioeconomic stressors experienced by PwMS during the pandemic. The summary table illustrates the interconnectedness of psychological burden, occupational disruption, and socioeconomic stressors for PwMS during the COVID-19 pandemic. Mental health deterioration and employment changes frequently co-occurred, highlighting the need for workplace policies and interventions that address both psychosocial support and occupational safety. Importantly, very few studies examined occupation-specific hazards or the lived experiences of patients, underscoring critical gaps in current research.
4. Discussion
The findings of this scoping review highlight a complex, multi-layered impact of the COVID-19 pandemic on people with multiple sclerosis (PwMS), particularly with respect to mental health and occupational outcomes. Several themes emerge: psychological burden, shifts in work conditions (both positive and negative), socioeconomic stressors, and important gaps in workplace-level data.
4.1. Psychological Burden and Mental-Health Trajectories
A prominent pattern across reviewed studies is a high prevalence of mental-health symptoms among PwMS during the pandemic, especially depression, stress, and anxiety [
17]. In some studies, depressive symptoms remained similar or increased compared with pre-pandemic baselines; stress levels often rose, while anxiety findings were more heterogeneous [
18]. This psychological burden is significant because mental health is deeply intertwined with functional and occupational outcomes in MS. Depression, stress, and anxiety are known to impair concentration, energy, motivation, and overall work participation contributing to absenteeism, presenteeism, and possibly premature exit from the workforce. In the broader population, pandemic-related economic distress and disruptions have been linked to elevated mental distress, suggesting that macro-level stressors likely amplified pre-existing vulnerabilities in chronically ill groups [
19]. Therefore, our review’s observation of elevated psychological burden among PwMS during COVID-19 likely represents more than short-term distress: it signals a risk for long-term deterioration in quality of life, work ability, and disease management.
4.2. Occupational Disruption: A Double-Edged Sword
Similarly, important is the impact on employment and work conditions. Meta-analytic evidence indicates that during the pandemic about 47% of PwMS were unemployed or retired, and roughly 43% reported changes in employment status [
15].
Work-from-home arrangements emerged as a notable adaptation: in at least one multiple-methods study, PwMS reported that remote work improved their ability to manage MS symptoms and enhanced self-perceived productivity [
20]. These observations suggest that, for a subset of PwMS, pandemic-induced flexibility (remote work, reduced commuting, adjusted working hours) may have offered previously unavailable accommodations improving work capacity and disease management. This aligns with literature on chronic illness more broadly, which shows that remote work can buffer against some disability-related barriers and enable better alignment of work demands with health needs. However, this “benefit” must be contextualized: many PwMS may not have equitable access to remote work, or may face compounding stressors social isolation, reduced support, increased uncertainty, which may offset benefits. For example, in the same study, participants reported heightened feelings of anxiety and loneliness despite flexible work arrangements [
20]. Moreover, in another study, a sizeable proportion of PwMS reported that the pandemic directly impacted their occupation in ways characterized by uncertainty, job instability, or broader life-course worries [
21]. Hence, pandemic-era occupational disruption appears as a double-edged sword: potentially beneficial (through flexibility), but also risky, especially when combined with mental-health strain and socioeconomic instability.
4.3. Socioeconomic Stressors and Broader Context
Our results also underscore how socioeconomic stressors financial strain, job loss, reduced workplace supports, and economic uncertainty may have compounded the challenges for PwMS. Several studies report increased unemployment or underemployment, decreased access to medical follow-up, and disruptions in care (e.g., cancelled clinical appointments, delayed treatments), especially during lockdowns [
22]. This broader context matters: for chronic illnesses such as MS, stable employment often supports health through income, social inclusion, access to insurance or disability benefits, and routine care. This scenario echoes findings in other chronic-disease populations, where pandemic-induced social and economic disruption has been linked to increased psychological distress and long-term adverse outcomes [
23].
4.4. Heterogeneity, Limitations, and Gaps in Evidence
When interpreting these findings, important limitations must be acknowledged. As in your Results section, many studies relied on cross-sectional designs, which constrain causal inference. Pre-existing vulnerabilities (severity of MS, comorbidities, socioeconomic status) may drive both psychological distress and employment changes, rather than the pandemic alone. Moreover, there is high heterogeneity across studies in terms of measurement instruments, timing (early vs. later pandemic), national context, and definitions of work outcomes (remote vs. in-person work, temporary vs. permanent job loss, part-time vs. full-time work). This variation complicates attempts to generalize results or draw robust conclusions.
Critically, Our Review Like Much of the Literature Reveals Significant Gaps
Few studies systematically evaluated workplace-level hazards or accommodations (e.g., access to ergonomic setup at home, employer support, infection risk mitigation, employer flexibility). There is limited use of qualitative data exploring lived experiences of PwMS in the workplace — including stigma, disclosure of MS status, social support, or discrimination. Longitudinal data remain scarce; thus it is unclear whether the observed changes in employment and mental health will translate into long-term occupational disability, dropout, or recovery post-pandemic. Intersectional factors (e.g., socioeconomic status, gender, job type, severity of MS) are underexplored, limiting understanding of who is most vulnerable or resilient.
4.5. Implications for Policy, Practice, and Future Research
The Findings of This Scoping Review Carry Several Important Implications
Employers and policymakers should recognize remote work and flexible arrangements as potentially effective, lasting accommodations for PwMS not only during a pandemic but as part of disability-inclusive employment policy. Formalizing such accommodations may support long-term workforce participation, reduce absenteeism/presenteeism, and enhance quality-of-life. Social and mental-health support must be prioritized for PwMS during widespread crises. Given the elevated psychological burden, strategies such as tele-counseling, peer support, social-support networks, and proactive outreach could mitigate exacerbation of mental-health symptoms. There is a critical need for longitudinal, mixed-methods research combining quantitative occupational and clinical outcomes with qualitative lived-experience data. Such studies would help to understand not only “what changed,” but “how and why” — exploring themes such as accommodation adequacy, disclosure, stigma, employer attitudes, and individual adaptation. Research should also examine inequalities within the PwMS population for example based on disease severity, job type (manual vs. desk work), socioeconomic background, gender to identify subgroups at particular risk and tailor interventions accordingly. Finally, for future health crises or pandemics, disability-inclusive emergency planning should integrate employment stability, access to care, and psychosocial support to protect vulnerable populations such as PwMS.
5. Limitations
While this scoping review offers a broad synthesis, it is constrained by limitations of the underlying studies (as discussed above). Another limitation is potential publication bias: studies demonstrating significant negative outcomes (job loss, severe psychological distress) may have been more likely to be published. Additionally, our synthesis may under-represent the experiences of PwMS in low-resource settings or non-Western countries, given that many studies were conducted in Europe or high-income countries.
6. Conclusions
The COVID-19 pandemic has had substantial and multifaceted effects on PwMS not only in terms of mental health but also employment, work conditions, and socioeconomic stability. While remote work and flexible arrangements offered a silver lining for some, many experienced increased stress, economic strain, and job insecurity. The existing literature though informative remains limited by heterogeneity, methodological constraints, and major gaps around workplace-level experiences and long-term outcomes. Given the ongoing global challenges (e.g., pandemic recurrences, economic instability), future research and policy should prioritize disability-inclusive employment practices, longitudinal monitoring, and holistic support systems for PwMS and other chronic-disease populations.
Author Contributions
Conceptualization, I.A. and A.V.E; methodology, I.A. and A.V.E; software, I.A.; validation, I.A., and N.S.; investigation, I.A., A.V.E, and N.S.; resources, I.A.; data curation, I.A.; writing—original draft preparation, I.A., A.V.E., N.S., M.M.M., and P.T.; writing—review and editing, I.A., A.V.E., N.S., M.M.M., and P.T.; visualization, I.A.; supervision, I.A. , and A.V.E., project administration, I.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated or analyzed in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We are grateful for the administrative and technical support provided by our colleagues during the literature search and data extraction processes.
Conflicts of Interest
The authors declare no conflicts of interest
References
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; van Der Mei, I.; et al. Rising Prevalence of Multiple Sclerosis Worldwide: Insights from the Atlas of MS. Mult. Scler. J. 2020, 26, 1816–1821. [Google Scholar] [CrossRef]
- Kowalec, K.; McKay, K.A.; Patten, S.B.; Fisk, J.D.; Evans, C.; Tremlett, H.; Marrie, R.A.; in Epidemiology, C.T.; of Comorbidity on Multiple Sclerosis (ECoMS), I.; in Epidemiology, C.T.; et al. Comorbidity Increases the Risk of Relapse in Multiple Sclerosis: A Prospective Study. Neurology 2017, 89, 2455–2461. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.M.; Arnett, P.A. Factors Related to Employment Status Changes in Individuals with Multiple Sclerosis. Mult. Scler. J. 2005, 11, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Torres, I.; Meca Lallana, V.; Costa-Frossard, L.; Oreja-Guevara, C.; Aguirre, C.; Alba Suarez, E.M.; Gomez Moreno, M.; Borrega Canelo, L.; Sabin Munoz, J.; Aladro, Y.; et al. Risk and Outcomes of COVID-19 in Patients with Multiple Sclerosis. Eur. J. Neurol. 2021, 28, 3712–3721. [Google Scholar] [CrossRef] [PubMed]
- Zabalza, A.; Cárdenas-Robledo, S.; Tagliani, P.; Arrambide, G.; Otero-Romero, S.; Carbonell-Mirabent, P.; Rodriguez-Barranco, M.; Rodriguez-Acevedo, B.; Restrepo Vera, J.L.; Resina-Salles, M.; et al. COVID-19 in Multiple Sclerosis Patients: Susceptibility, Severity Risk Factors and Serological Response. Eur. J. Neurol. 2021, 28, 3384–3395. [Google Scholar] [CrossRef]
- Tengilimouglu, D.; Gönüllü, U.; Icsik, O.; Tosun, N.; Zekiouglu, A.; Tengilimouglu, O.; Younis, M. The Problems Experienced by Employees with Chronic Disease during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 578. [Google Scholar] [CrossRef]
- Ducas, J.; Daneau, C.; Bouqartacha, S.; Lecours, A.; Abboud, J.; Marchand, A. A.; Descarreaux, M. The Impact of Telework on Absenteeism, Presenteeism, and Return to Work among Workers with Health Conditions: A Scoping Review. Front. Public Heal. 2025, 13, 1655200. [Google Scholar] [CrossRef]
- Scarpetta, S.; Carcillo, S.; Salvatori, A. The Unequal Impact of COVID-19: A Spotlight on Frontline Workers, Migrants and Racial/Ethnic Minorities [Internet] 2022.
- Parent-Thirion, A.; Mackova, B.; Ivaškait-Tamoši, V.; Cabrita, J. Job Quality of COVID-19 Pandemic Essential Workers; Eurofound, 2023.
- Fronteira, I.; Mathews, V.; Dos Santos, R.L.B.; Matsumoto, K.; Amde, W.; Pereira, A.; de Oliveira, A.P.C.; Craveiro, I.; Chança, R.; Boniol, M.; et al. Impacts for Health and Care Workers of Covid-19 and Other Public Health Emergencies of International Concern: Living Systematic Review, Meta-Analysis and Policy Recommendations. Hum. Resour. Health 2024, 22, 10. [Google Scholar] [CrossRef]
- Glanz, B.I.; Dégano, I.R.; Rintell, D.J.; Chitnis, T.; Weiner, H.L.; Healy, B.C. Work Productivity in Relapsing Multiple Sclerosis: Associations with Disability, Depression, Fatigue, Anxiety, Cognition, and Health-Related Quality of Life. Value Heal. 2012, 15, 1029–1035. [Google Scholar] [CrossRef]
- von Drathen, S.; Gold, S.M.; Peper, J.; Rahn, A.C.; Ramien, C.; Magyari, M.; Hansen, H. C.; Friede, T.; Heesen, C. Stress and Multiple Sclerosis--Systematic Review and Meta-Analysis of the Association with Disease Onset, Relapse Risk and Disability Progression. Brain. Behav. Immun. 2024, 120, 620–629. [Google Scholar] [CrossRef]
- Ponzio, M.; Podda, J.; Pignattelli, E.; Verri, A.; Persechino, B.; Vitturi, B.K.; Bandiera, P.; Manacorda, T.; Inglese, M.; Durando, P.; et al. Work Difficulties in People with Multiple Sclerosis. J. Occup. Rehabil. 2024, 34, 606–617. [Google Scholar] [CrossRef]
- Maurino, J.; Martinez-Ginés, M.L.; Garcia-Dominguez, J.M.; Solar, M.D.; Carcelén-Gadea, M.; Ares-Luque, A.; Ballabriga, J.; Navarro-Cantó, L.; Medrano, N.; Honan, C.A.; et al. Workplace Difficulties, Health-Related Quality of Life, and Perception of Stigma from the Perspective of Patients with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2020, 41, 102046. [Google Scholar] [CrossRef]
- Vitturi, B.K.; Rahmani, A.; Montecucco, A.; Dini, G.; Durando, P. Occupational Outcomes of People with Multiple Sclerosis during the COVID-19 Pandemic: A Systematic Review with Meta-Analysis. Front. Public Heal. 2023, 11, 1217843. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRI-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Zarghami, A.; Hussain, M.A.; Campbell, J.A.; Ezegbe, C.; van der Mei, I.; Taylor, B. V; Claflin, S.B. Psychological Impacts of COVID-19 Pandemic on Individuals Living with Multiple Sclerosis: A Rapid Systematic Review. Mult. Scler. Relat. Disord. 2022, 59, 103562. [Google Scholar] [CrossRef]
- Vacaras, V.; Nistor, C.; Schiopu, A.M.; Vacaras, C.; Marin, G.-E.; Muresanu, D.F. The Psychological Impact of the COVID-19 Pandemic on People with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2023, 76, 104825. [Google Scholar] [CrossRef] [PubMed]
- Sundaram-Stukel, R.; Davidson, R.J. Associational and Plausible Causal Effects of COVID-19 Public Health Policies on Economic and Mental Distress. arXiv Prepr. arXiv2112.11564 2021. [Google Scholar]
- De Dios Perez, B.; Pritchard, C.; Powers, K.; das Nair, R.; Evangelou, N.; Ford, H.; Tallantyre, E.; Dobson, R.; Radford, K. The Impact of COVID-19 on the Employment of People With M. Sclerosis: A M. Methods Study. Int. J. MS Care 2024, 26, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Murley, C.; Dervish, J.; Machado, A.; Svärd, V.; Wennman-Larsen, A.; Hillert, J.; Friberg, E. Exploring the Working Life of People with Multiple Sclerosis during the COVID-19 Pandemic in Sweden. BMC Public Health 2024, 24, 1389. [Google Scholar] [CrossRef]
- Vogel, A.C.; Schmidt, H.; Loud, S.; McBurney, R.; Mateen, F.J. Impact of the COVID-19 Pandemic on the Health Care Of> 1,000 People Living with Multiple Sclerosis: A Cross-Sectional Study. Mult. Scler. Relat. Disord. 2020, 46, 102512. [Google Scholar] [CrossRef]
- Aksoy, O.; Wu, A.F.-W.; Aksoy, S.; Rivas, C. A. Social support and mental well-being among people with and without chronic illness during the Covid-19 pandemic: evidence from the longitudinal UCL covid survey. BMC Psychol. 2024, 12, 136. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).