Figure 1.
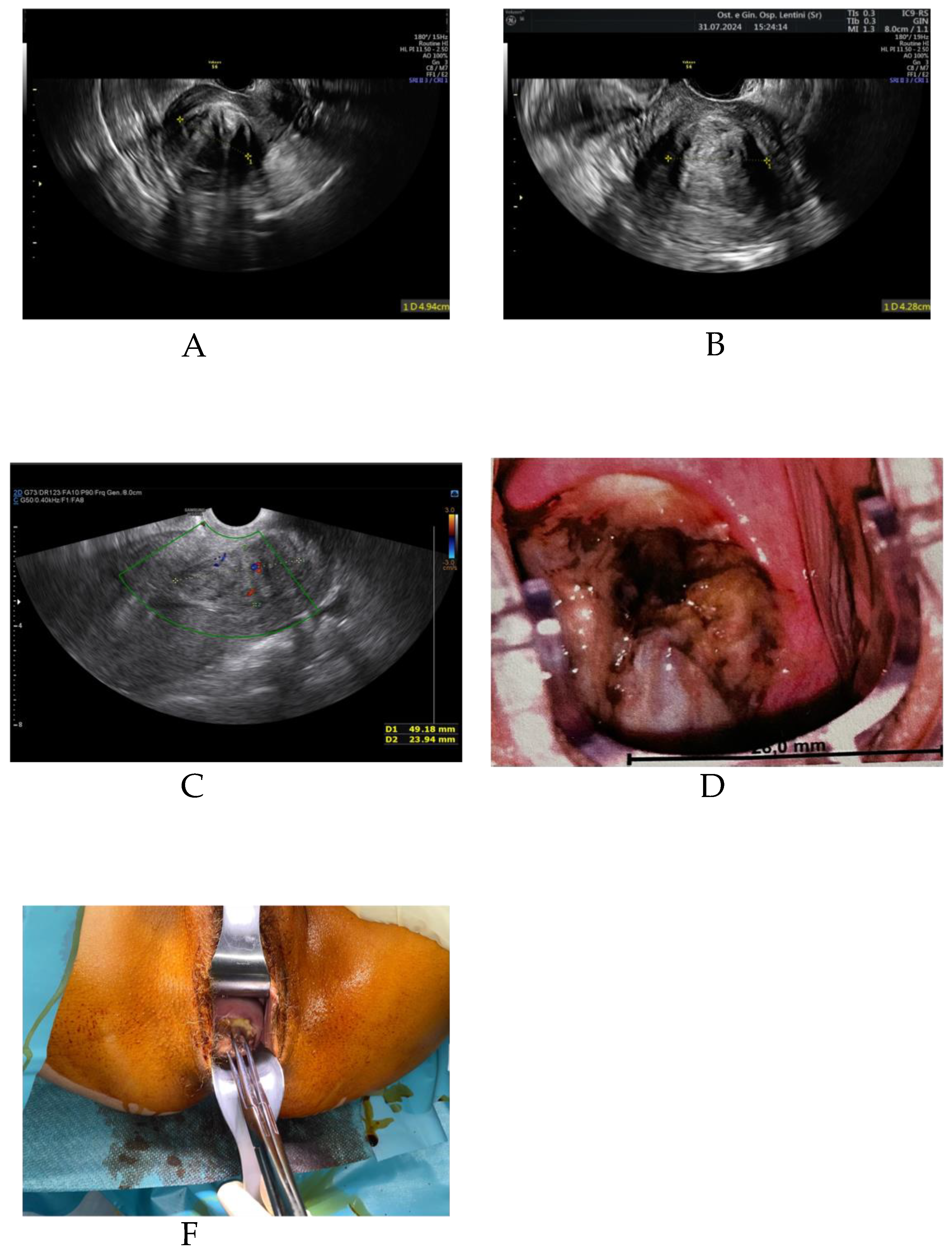
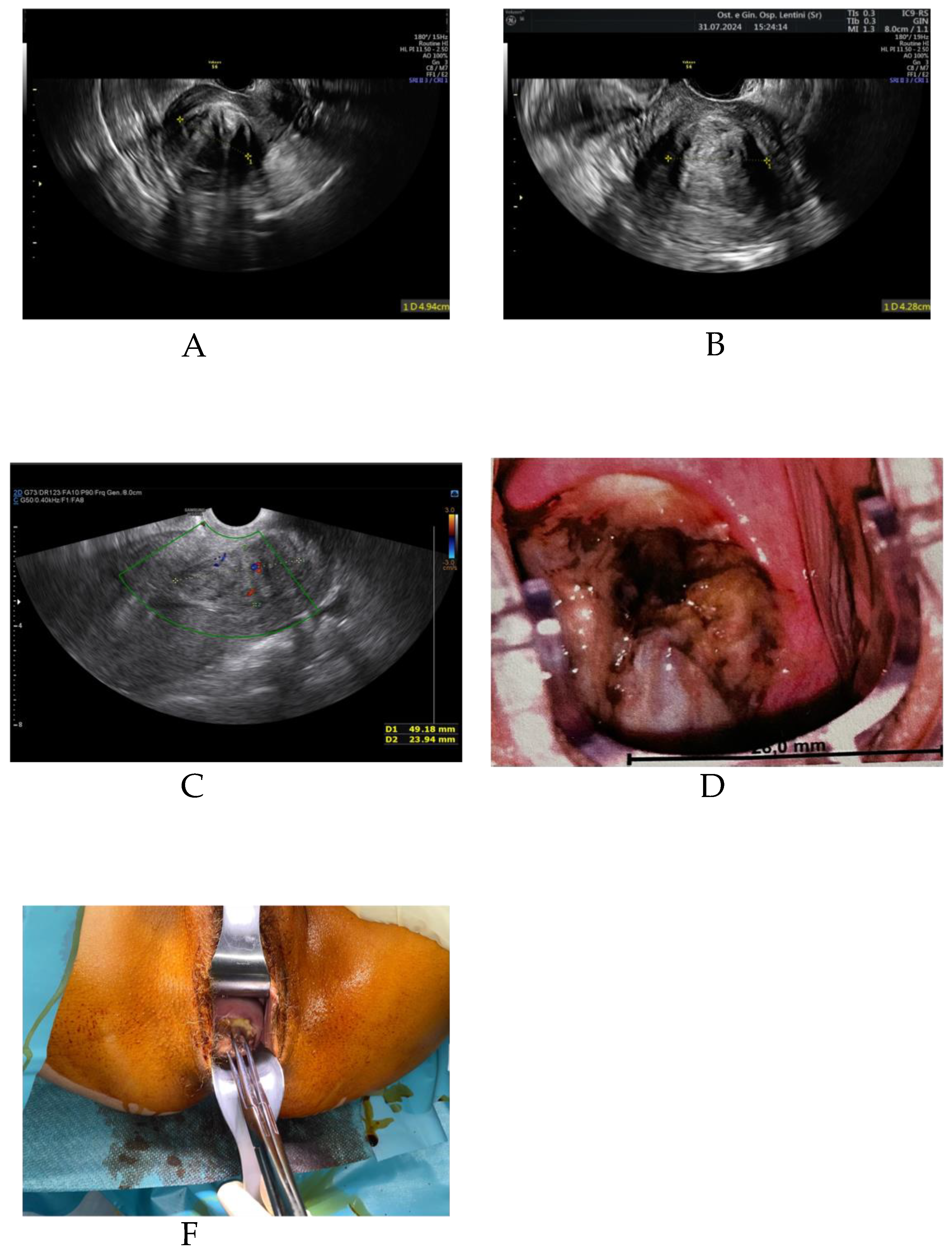
Uterine fibroids, also known as leiomyomas or myomas, are common gynaecological tumors that affect 20% to 40% of women aged 30 and over. In about one-third of cases, they cause symptoms such as heavy menstrual bleeding (hypermenorrhea), dysmenorrhea, dyspareunia, and pelvic pain. The choice of treatment depends on the number, size, and location of the fibroids, as well as the patient’s symptoms and reproductive goals. Historically, hysterectomy was the standard treatment for symptomatic fibroids, particularly for types 3, 5, 6, and 2–5 according to the FIGO classification. More recently, less invasive alternatives have become available. Transvaginal radiofrequency ablation (RFA) is a technique that allows fibroid treatment without surgical incision. The method uses an ultrasound-guided electrode inserted via the vaginal route into the fibroid tissue. The high-frequency alternating current produces localised heating (60–80 °C), leading to coagulative necrosis, cell death, ischemia, and loss of hormone receptor activity in the treated tissue. The patient, C.E., is a 41-year-old woman with a history of one spontaneous delivery and prior laparoscopic surgery for endometriosis. She presented to our gynaecology unit complaining of hypermenorrhea, pelvic pain, and fatigue due to anaemia. A transvaginal ultrasound identified a 5 cm uterine fibroid (FIGO type 2–5).In June 2024, she underwent transvaginal RFA. The procedure was completed without intraoperative or postoperative complications. One month later, the patient reported improvement in pelvic pain but continued to experience heavy menstrual bleeding. Follow-up ultrasound showed the fibroid had decreased by approximately 1 cm. Two months after the procedure, she returned with complaints of excessive hypermenorrhea, spotting, smelly vaginal discharge, and pelvic pain. Transvaginal ultrasound revealed the fibroid had migrated into the cervix with a vascular pedicle. Vaginal surgical removal was performed under general anesthesia. The procedure lasted 10 minutes and was completed without complications. The patient was discharged in good health. Histopathological analysis is pending. Uterine fibroids are benign tumors common in reproductive and perimenopausal women. They typically require treatment only when symptomatic, such as when causing heavy bleeding, anemia, or pain. Hysterectomy was historically the primary surgical option, but many minimally and non-invasive techniques are now available. Transvaginal RFA is a minimally invasive, incision-free method performed under ultrasound guidance. It allows for targeted fibroid ablation with minimal downtime and low complication rates. Fibroid expulsion is a rare post-RFA event. To date, only one similar case has been reported, from a hospital in Germany in 2023. Common symptoms of fibroid expulsion include vaginal bleeding, smelly discharge, and the sensation of a mass passing through the vagina. Fibroid removal via the vaginal route is safe and effective, even for large fibroids. In our case, we considered the expulsion beneficial, as the fibroid was completely removed without complications. However, this outcome could also represent a complication, especially if associated with infection, significant blood loss, or surgical risks. The estimated risk of fibroid expulsion after RFA is approximately 1%–1.5%. In cases where expulsion occurs, timely vaginal removal can lead to a favorable outcome. It remains unclear whether this rare event should be classified as a complication or a potential therapeutic benefit. (A) Transvaginal ultrasound showing a 5 cm FIGO type 2–5 fibroid prior to RFA. (B) One month post-RFA, showing a reduction in fibroid size. (C) Two months post-RFA, Doppler ultrasound revealing fibroid descent into the cervical canal.(D) Cervical fibroid visualized during colposcopic examination (E) Intraoperative image showing the removal of the expelled fibroid.
Figure 1.
Uterine fibroids, also known as leiomyomas or myomas, are common gynaecological tumors that affect 20% to 40% of women aged 30 and over. In about one-third of cases, they cause symptoms such as heavy menstrual bleeding (hypermenorrhea), dysmenorrhea, dyspareunia, and pelvic pain. The choice of treatment depends on the number, size, and location of the fibroids, as well as the patient’s symptoms and reproductive goals. Historically, hysterectomy was the standard treatment for symptomatic fibroids, particularly for types 3, 5, 6, and 2–5 according to the FIGO classification. More recently, less invasive alternatives have become available. Transvaginal radiofrequency ablation (RFA) is a technique that allows fibroid treatment without surgical incision. The method uses an ultrasound-guided electrode inserted via the vaginal route into the fibroid tissue. The high-frequency alternating current produces localised heating (60–80 °C), leading to coagulative necrosis, cell death, ischemia, and loss of hormone receptor activity in the treated tissue. The patient, C.E., is a 41-year-old woman with a history of one spontaneous delivery and prior laparoscopic surgery for endometriosis. She presented to our gynaecology unit complaining of hypermenorrhea, pelvic pain, and fatigue due to anaemia. A transvaginal ultrasound identified a 5 cm uterine fibroid (FIGO type 2–5).In June 2024, she underwent transvaginal RFA. The procedure was completed without intraoperative or postoperative complications. One month later, the patient reported improvement in pelvic pain but continued to experience heavy menstrual bleeding. Follow-up ultrasound showed the fibroid had decreased by approximately 1 cm. Two months after the procedure, she returned with complaints of excessive hypermenorrhea, spotting, smelly vaginal discharge, and pelvic pain. Transvaginal ultrasound revealed the fibroid had migrated into the cervix with a vascular pedicle. Vaginal surgical removal was performed under general anesthesia. The procedure lasted 10 minutes and was completed without complications. The patient was discharged in good health. Histopathological analysis is pending. Uterine fibroids are benign tumors common in reproductive and perimenopausal women. They typically require treatment only when symptomatic, such as when causing heavy bleeding, anemia, or pain. Hysterectomy was historically the primary surgical option, but many minimally and non-invasive techniques are now available. Transvaginal RFA is a minimally invasive, incision-free method performed under ultrasound guidance. It allows for targeted fibroid ablation with minimal downtime and low complication rates. Fibroid expulsion is a rare post-RFA event. To date, only one similar case has been reported, from a hospital in Germany in 2023. Common symptoms of fibroid expulsion include vaginal bleeding, smelly discharge, and the sensation of a mass passing through the vagina. Fibroid removal via the vaginal route is safe and effective, even for large fibroids. In our case, we considered the expulsion beneficial, as the fibroid was completely removed without complications. However, this outcome could also represent a complication, especially if associated with infection, significant blood loss, or surgical risks. The estimated risk of fibroid expulsion after RFA is approximately 1%–1.5%. In cases where expulsion occurs, timely vaginal removal can lead to a favorable outcome. It remains unclear whether this rare event should be classified as a complication or a potential therapeutic benefit. (A) Transvaginal ultrasound showing a 5 cm FIGO type 2–5 fibroid prior to RFA. (B) One month post-RFA, showing a reduction in fibroid size. (C) Two months post-RFA, Doppler ultrasound revealing fibroid descent into the cervical canal.(D) Cervical fibroid visualized during colposcopic examination (E) Intraoperative image showing the removal of the expelled fibroid.
Author Contributions
Conceptualization, Martina Billeci; investigation, Gianfranco Morreale; resources, Martina Billeci; data curation, Ferdinando Antonio Gulino; writing—original draft preparation, Martina Billeci; writing—review and editing, Francesco Cannone. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study; the ASP Siracusa Ethics Committee on Scientific Ethics waived the need for IRB approval for the case report, wherein the patient had signed informed consent.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The original contributions presented in this work are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Stewart EA: Cookson CL, Gandolfo RA, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501–1512. [CrossRef]
- Foth D, Röhl FW, Friedrich C, Tylkoski H, Rabe T, Römer T, et al. Symptoms of uterine myomas: data of an epidemiological study in Germany. Arch Gynecol Obstet. 2017;295(2):415–426. [CrossRef]
- Bradley LD, Pasic RP, Miller LE. Clinical performance of radiofrequency ablation for uterine fibroids: systematic review. J Laparoendosc Adv Surg Tech A. 2019;29(12):1507–1517. [CrossRef]
- Iversen H, Dueholm M. Radiofrequency thermal ablation for uterine myomas: long-term outcomes. J Minim Invasive Gynecol. 2017;24(6):1020–1028. [CrossRef]
- Piriyev E, Bends R, Schiermeier S, Romer T. RFA in high-risk patients with bleeding disorder. Ginekol Pol. 2022;93(8):614–619.
- Piriyev E, Schiermeier S, Bends R, Römer T. RFA of fibroids ≥5 cm with abnormal bleeding. J Gynecol Obstet Hum Reprod. 2022;51(2).
- Chudnoff S, Guido R, Roy K, et al. Ultrasound-guided transcervical ablation of fibroids. Obstet Gynecol. 2019;133(1):13–22. [CrossRef]
- Römer T, Bends R, Christoffel L, et al. Expert consensus on RFA in symptomatic fibroids. Arch Gynecol Obstet. 2022;306(1):1–6.
- Borah BJ, Nicholson WK, Bradley L, Stewart EA. Impact of fibroids: a national survey. Am J Obstet Gynecol. 2013;209:319.e1.
- Amaral VF, Yochiy FY, Furlanetto ML Jr, Payão SLM. Myoma expulsion after UAE. Case Rep Surg. 2021;2021:6644229. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).