1. Introduction
Engaging patients, caregivers, and community groups in determining research priorities is increasingly acknowledged to ensure that health services research addresses genuine needs and enhances patient experiences. Methods such as the James Lind Alliance Priority Setting Partnerships and community-based participatory strategies have proven effective in formulating research questions that differ from those identified solely by researchers, often emphasizing issues such as access to care, service coordination, and self-management [
1,
2].
Regions characterized by linguistic and cultural diversity present difficulties in prioritizing. Research from places such as Ireland and Singapore, as well as other multilingual areas, indicates that traditional top-down methods might neglect the needs of minority groups. In contrast, well-managed participatory processes can reveal concerns specific to the context and enhance the legitimacy of decisions made [
3,
4].
Despite these advantages, participatory activities often face obstacles. Disparities in power between researchers and participants can restrict the impact of community contributions, and marginalized groups are frequently underrepresented, even when their inclusion is a stated objective [
5]. Additionally, resource limitations and institutional demands, such as inflexible funding structures, hinder ongoing involvement [
6].
Research has shown that involving participants in setting priorities can shift research towards topics that focus on patients and enhance stakeholder satisfaction. However, its long-term effects on healthcare quality and outcomes have not been thoroughly documented [
7]. It is crucial to evaluate these processes in various settings to create effective strategies for fair participation and determine whether the identified priorities eventually influence policy and service delivery.
Building on this evidence, the present study investigates how a structured bilingual participatory survey can inform health services research priorities in South Tyrol a culturally and linguistically diverse region [
8,
9]. The survey was distributed to non-profit organizations representing patient and social interests to identify research topics of greatest relevance for regional health services. Specifically, we ask whether engaging these stakeholders can generate priorities that reflect the patient experience, support patient-centered care, and guide improvements in the quality of healthcare.
2. Methods
2.1. Study Design and Participants
An online cross-sectional survey was conducted to determine the priorities for regional health services research from the perspectives of patients and social interest organizations (PSIOs), as well as general practitioners (GPs) in South Tyrol, Italy. On August 25, 2025, an email invitation was dispatched to all 64 member organizations of the South Tyrolean Umbrella Association for Social and Health Affairs (“Dachverband für Soziales und Gesundheit”), with a reminder sent on September 17, 2025. Five of these email addresses were invalid. Each PSIO was asked to share the invitation with its leaders, staff, and members to increase participation rates. Simultaneously, GPs employed by the South Tyrolean Public Health Service (n = 290) received direct invitations. The survey will conclude on September 25, 2025.
2.2. Questionnaire Development and Content
The questionnaire was developed by the Institute of General Practice and Public Health to address the study objectives, drawing on relevant literature on participatory priority setting and prior health services research conducted in South Tyrol. In addition, the current program activities of the institute—the only dedicated public health research institute in the region—were incorporated to ensure contextual relevance. The instrument covered organizational characteristics, respondent roles, priority ratings for a predefined set of regional health research topics, experiences with patient and public involvement in healthcare planning, perceived barriers to healthcare access, suggestions for enhancing patient influence in decision-making, and preferred modes of engagement in priority setting (e.g., online surveys, workshops, focus groups, and patient advisory boards). Open-ended items enabled respondents to raise additional health system issues and to provide free-text recommendations.
The draft questionnaire was prepared in German, translated into Italian by a native speaker, and provided in both languages. An English version is available in the Supplementary Material. It combined multiple-choice, ranking, and open-ended questions to gather information. To ensure clarity and validity, the questionnaire was piloted by a biostatistician, GP, and clinical psychologist before distribution.
2.3. Data Collection
The survey was administered using Google Forms. Responses were anonymous, and participation was voluntary and confidential. Completion of the online questionnaire was considered as implied consent. According to local regulations, formal ethics committee approval was not required because no patient-level clinical data were collected for this study.
2.4. Statistical Analysis
All analyses were prespecified as descriptive and exploratory. Categorical variables were summarized as counts and percentages, and ordinal/continuous items as mean (SD) and median (IQR), reporting the valid n for each item (no imputation). Unless stated otherwise, tests were two-sided with α = 0.05; given the study’s exploratory aims, p-values are presented unadjusted and interpreted alongside effect sizes. Analyses were conducted using IBM SPSS Statistics for Windows version 25.0 (IBM Corp., Armonk, NY, USA).
The language of free-text responses was recoded to German and Italian; blanks were left as system missing. For multi-response questions (e.g., preferred participation modes; barriers; facilitators), open answers were content coded using a directed approach into binary indicators (1 = theme mentioned; 0 = not mentioned) and summarized as proportions of all respondents.
Because priority ratings were captured on 5-point ordinal scales and group sizes were unequal, GPs versus PSIO respondents were compared using Mann–Whitney U tests for each research topic; medians and IQRs are shown per group. For associations between categorical variables, Pearson’s chi-square tests with Cramer’s V as the effect size (small ≈ 0.10–0.29, moderate ≈ 0.30–0.49, large ≥ 0.50) were used. The association between language and research interest was examined using chi-square, and Kendall’s tau-b was additionally reported as an ordinal measure of association. Missing data were excluded listwise for the variables involved in each specific test.
To explore the relationships between interest in research participation, topic priorities, and inter-topic relationships, Spearman’s rank correlations (ρ) were computed using pairwise complete observations. Correlation magnitudes were interpreted using conventional thresholds (small ≈ 0.10–0.29; moderate ≈ 0.30–0.49; large ≥ 0.50) [
10].
2.5. Use of Generative Artificial Intelligence
Generative Artificial Intelligence (AI; ChatGPT, OpenAI) was used to assist in structuring and refining the manuscript text, including the formulation of the Introduction and Methods sections. AI was also used to synthesize and cross-reference the existing literature to ensure clarity and contextualization. No generative AI was used for data collection, statistical analysis, or interpretation of the results. All content was reviewed and approved by the authors.
3. Results
3.1. Survey Participation and Respondent Characteristics
A total of 95 completed surveys were evaluated. Among the ten GPs who participated, nine (9.5%) were employed in primary care. The other respondents were affiliated with PSIOs as either members or service users (40.0%), board members or leaders (28.4%), staff (15.8%), or held other roles (6.3%). This confirms that most responses originated from the PSIO sector, with physicians contributing a smaller but distinct subgroup of respondents. As invitations were distributed both to organizational representatives and through organizations to their members, multiple responses per organization were possible. Thus, the distribution reflects individual perspectives rather than a strict one-response-per-organization approach.
Among all responses, 51 respondents (53.7%) provided a valid and identifiable organization name, while 44 (46.3%) either left the field empty or provided information that could not be linked to a specific organization. Of the organizations that could be classified, chronic disease associations were the most frequent (n = 28; 54.9%), followed by disability-related groups (n = 11; 21.6%), mental health or psychosocial support organizations (n = 7; 13.7%), child and family welfare organizations (n = 2; 3.9%), and social inclusion or poverty relief groups (n = 3; 5.9%).
These categories represent a wide range of patient and community interests. Together, chronic disease and disability organizations accounted for more than three-quarters of all identified PSIO, indicating that the survey successfully engaged the most active segments of the South Tyrolean Federation for Social and Health Affairs.
3.1.1.
Open-text responses were provided predominantly in German (n = 52; 71.2%), while a smaller group responded in Italian (n = 21; 28.8%). Twenty-two participants (23.2% of the total sample) left these fields empty and were coded as missing. It should be noted that the questionnaire was available in both German and Italian; the coding here reflects the language used in free-text answers rather than the version of the questionnaire selected. Among German-language responses, most indicated conditional interest (“maybe / more information desired,” 55.8%), followed by definite interest (34.6%) and no interest (9.6%). Italian-language responses showed a different distribution, with a higher proportion expressing definite interest (47.6%), 42.9% reporting conditional interest, and 9.5% indicating no interest. Respondents with missing entries displayed a pattern like the German-language group, with conditional interest being most frequent.
Despite these descriptive differences, a chi-square test of independence did not reveal a statistically significant association between language and research interests (χ² = 1.14, df = 2, p = 0.566). The effect size was small (Cramer’s V = 0.125), and ordinal association measures (Kendall’s tau-b = –0.12, p = 0.292) confirmed the absence of systematic trends.
3.1.2. Perceived Barriers to Healthcare Access
The open-ended survey question on perceived barriers to healthcare access among survey participants (“What barriers do your members experience in accessing health care?”) was analyzed using the same directed content approach described above.
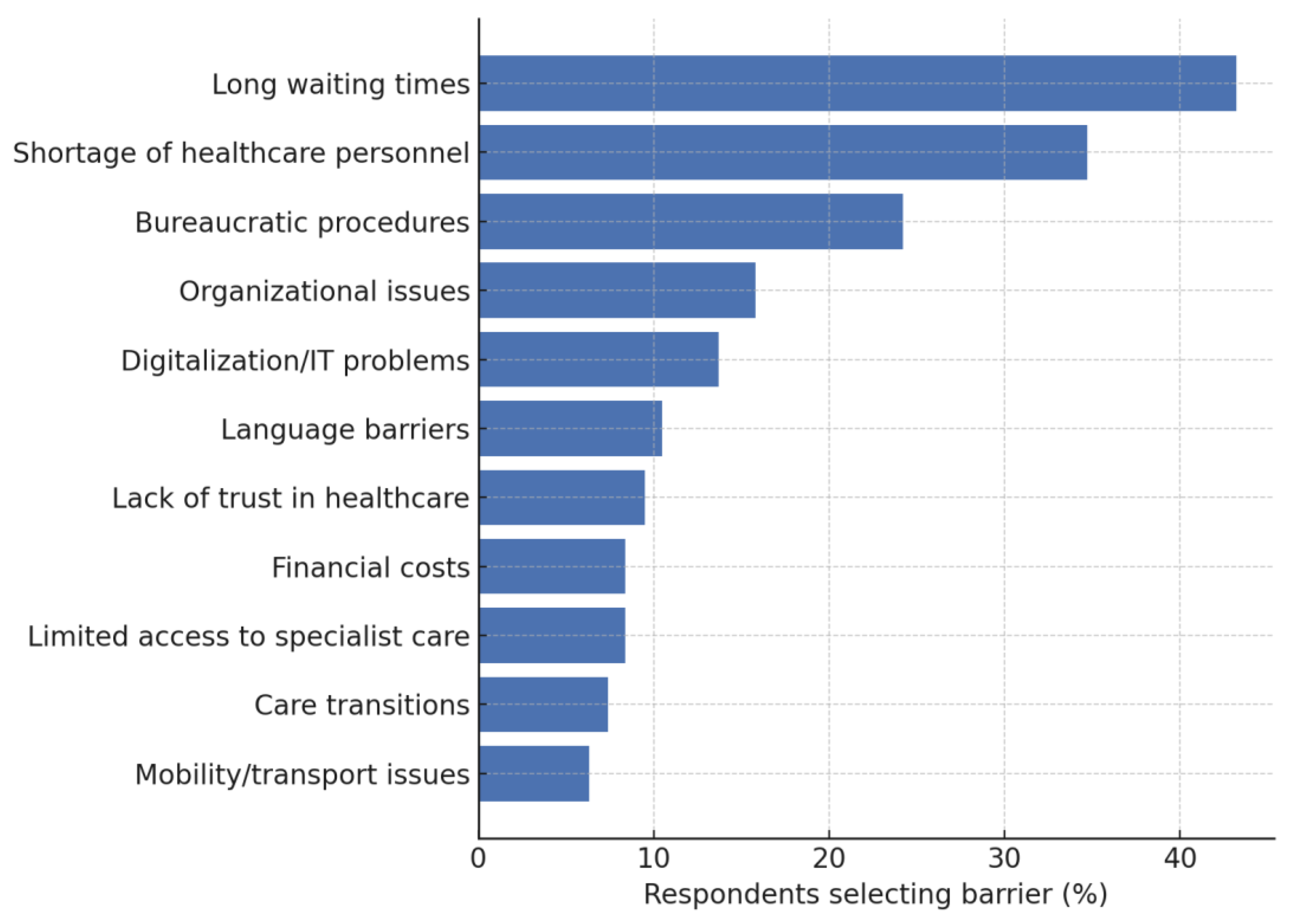
Figure 1 presents the frequency of these content-derived categories as a proportion of all 95 respondents.
Long waiting times clearly dominated the responses, mentioned by more than two-fifths of the participants. A shortage of healthcare personnel was the second most frequent barrier, followed by bureaucratic procedures. Organizational issues, digitalization/IT problems, language barriers, lack of trust in healthcare, financial costs, limited access to specialist care, care transitions, and mobility or transport limitations were reported by progressively smaller proportions of respondents. These findings indicate that, within this mixed group of GPs and PSIOs, barriers are concentrated on delays and human resources, whereas structural, financial, and mobility obstacles are far less prominent.
Respondents detailed how prolonged waits disrupted both routine care and access to specific benefits, sometimes forcing individuals to seek costly private services to avoid waiting. Financial pressures were evident in reports of out-of-pocket payments for dental treatment or essential medications, despite formal fee waivers. Several narratives described the difficulties faced by vulnerable groups, such as people with disabilities, cognitive impairments, or limited language proficiency, who encountered dismissive attitudes or practical obstacles when seeking preventive or specialized services. Structural critiques included the persistence of a hospital-centered care model, fragmented reporting and reimbursement procedures, and electronic health records used mainly as document repositories rather than tools for integrated care.
3.2. Research Priority Ratings
Participants evaluated a predetermined list of research topics using a 5-point priority scale.
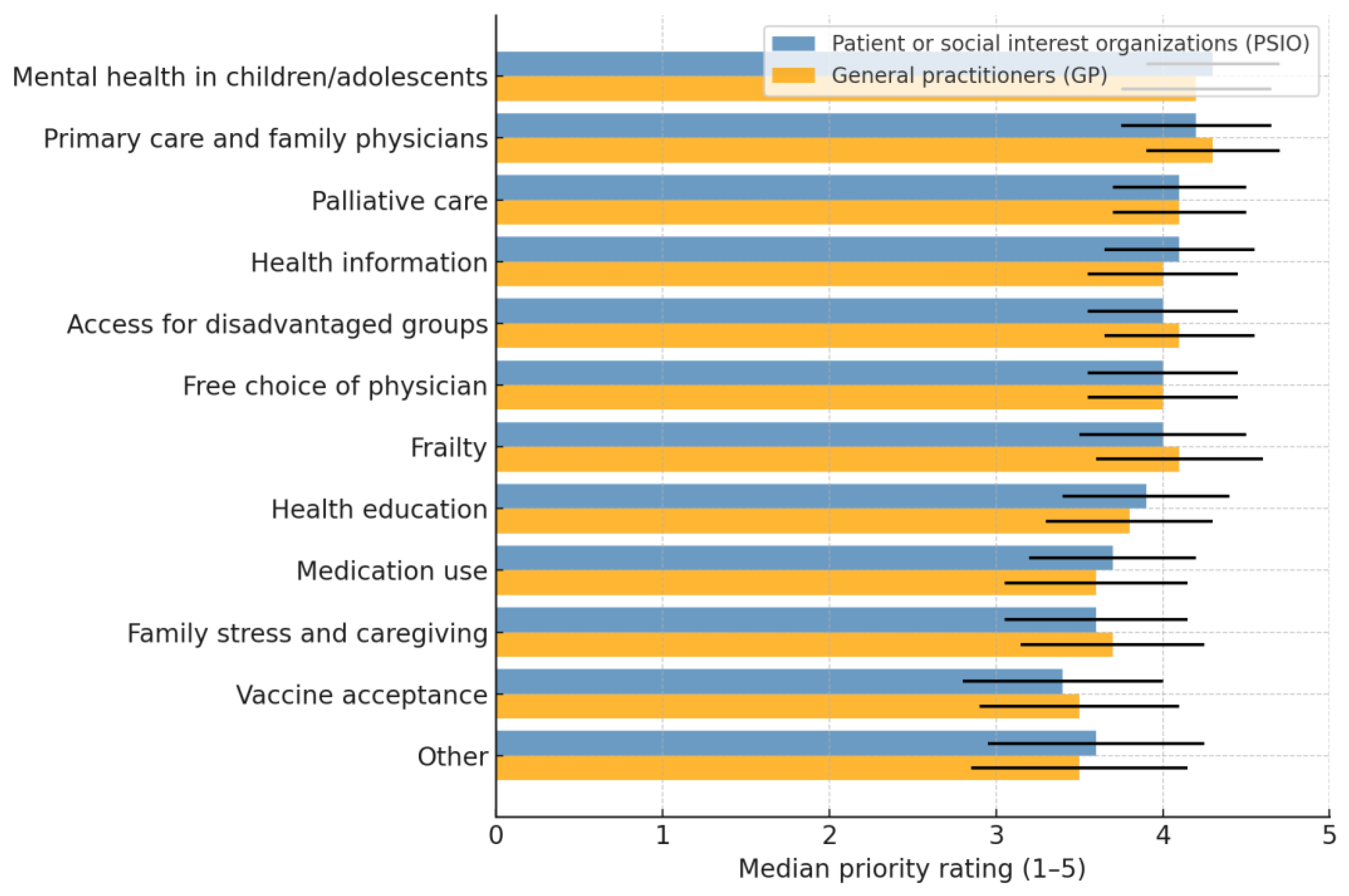
As illustrated in
Table 1, the top priorities were the mental health of children and adolescents, continuity and trust in primary care, and patient-focused palliative care and end-of-life care. These were closely followed by reliable health information, communication, and access to healthcare for disadvantaged groups. Moderate-priority topics included the freedom to choose a trusted general practitioner and its effect on waiting times for specialist appointments and diagnostic procedures, detecting frailty in older adults and appropriate care, and health education in schools. Lower priorities were given to environmentally sustainable and safe prescribing, the family impact of gender differences in stress management, and vaccine acceptance with culturally sensitive information.
Among the 95 valid survey responses, 85 respondents (89.5%) represented PSIO, and 10 respondents (10.5%) were GPs (nine in primary care and one as a PSIO member). Mann–Whitney U tests comparing the priority ratings between GPs and PSIO across all 12 research topics revealed no statistically significant differences (all
p > 0.16). The mean rank patterns suggest only minor and non-significant tendencies. GPs rated vaccine acceptance and access to disadvantaged groups as slightly higher than PSIO. The PSIO showed slightly higher rankings for frailty and free choice of physician. These differences were not significant, indicating a broad agreement between GPs and PSIO in setting research priorities (
Figure 2).
3.3. Interest in Research Participation
Among the 81 valid responses to the question, “Is your organization interested in participating in research projects (e.g., in formulating research questions, workshops, or sharing experiential knowledge)?”, 38.3% indicated yes, 9.9% responded no, and 51.9% selected maybe / more information desired, while 14 participants (14.7% of the total sample of 95) provided no answer.
When examined by organizational role, definite interest in research participation was most frequent among board or leadership members (46.2%), followed by members or service users (40.7%) and staff (21.4%); GPs showed an intermediate level (33.3%). A chi-square test of independence (χ² = 7.18, df = 12, p = 0.846) revealed no statistically significant association between organizational role and research interest, reflecting a small sample size.
Correlation Results
Spearman correlation analyses were used to examine the associations between interest in research participation and rated priority topics for health research (Tab. 2).
Interest in research participation showed small negative correlations with several priority topics, including palliative care (ρ = –0.23, p = 0.049), primary care continuity (ρ = –0.26, p = 0.022), and stress in families (ρ = –0.25, p = 0.034). These results suggest that respondents expressing a higher interest in participating in research tended to assign slightly lower priority ratings to these specific research areas. Other associations with interest in research were weak and insignificant.
Among the priority topics themselves, there was a consistent pattern of positive inter-correlations, indicating that participants who rated one topic as highly important tended to give high ratings to other topics.
The strongest relationships were observed between frailty and palliative care (ρ = 0.66, p < 0.001), health education in schools and stress in families (ρ = 0.59, p < 0.001), and primary care continuity with appropriate prescribing (ρ = 0.64, p < 0.001).
Numerous moderate associations (ρ ≈ 0.30–0.50, all p < 0.01) linked most other topic pairs, suggesting a generally coherent pattern of high concern across the research priorities.
Table 2.
Significant Spearman correlations between research participation interest and priority topics (and among the priority topics).
Table 2.
Significant Spearman correlations between research participation interest and priority topics (and among the priority topics).
| Variables |
n (pairs) |
ρ (Spearman) * |
p-value |
Effect size †
|
|
Interest in research participation × Palliative care priority |
73 |
–0.23 |
0.049 |
Small |
|
Interest in research participation × Primary care continuity |
75 |
–0.26 |
0.022 |
Small |
|
Interest in research participation × Stress in families |
73 |
–0.25 |
0.034 |
Small |
| Frailty × Palliative care |
84 |
0.66 |
<0.001 |
Large |
| Health education in schools × Stress in families |
82 |
0.59 |
<0.001 |
Large |
| Primary care continuity × Appropriate prescribing |
85 |
0.64 |
<0.001 |
Large |
| Frailty × Primary care continuity |
84 |
0.46 |
<0.001 |
Moderate |
| Frailty × Appropriate prescribing |
84 |
0.44 |
<0.001 |
Moderate |
| Palliative care × Primary care continuity |
83 |
0.48 |
<0.001 |
Moderate |
| Palliative care × Appropriate prescribing |
82 |
0.45 |
<0.001 |
Moderate |
| Health education in schools × Mental health of children |
85 |
0.42 |
<0.001 |
Moderate |
| Access for disadvantaged groups × Primary care continuity |
83 |
0.39 |
0.002 |
Moderate |
| Access for disadvantaged groups × Appropriate prescribing |
82 |
0.37 |
0.003 |
Moderate |
3.3. Recommendations for Enhancing Patient and Public Involvement
Among the 95 respondents, 15 (15.8%) reported prior involvement of their members or users in the planning or evaluation of health services, while 42 (44.2%) stated that no participation had taken place, and 38 (40.0%) were uncertain. Thirty-five respondents (36.8 %) expressed definite interest in participating in research projects, while an additional 47 (49.5 %) indicated conditional interest, requesting more detailed information before committing. Only 13 respondents (13.7 %) reported no interest in research collaboration. These findings suggest substantial openness within PSIOs and GPs to engage in research in the ways specified in the questionnaire, such as contributing to research questions, participating in workshops or focus groups, or providing feedback on research results, provided that adequate information and support are available.
3.3.1. Feeling Heard in Health Decisions and Research
The open-ended question “What would help your members feel better heard in health decisions and research?” was analyzed using a directed content approach. All narrative responses were screened for recurring themes and subsequently coded into binary variables indicating whether a respondent mentioned a specific theme.
Table 3 presents the frequency of the content-derived categories as the proportion of all 95 respondents in the study. Quantitative coding showed that clearer communication between decision-makers and the public was the most frequently mentioned facilitator (12.6%), followed by more time for participation (10.5%) and active inclusion of patients or community representatives (7.4%). Other suggestions included representation in formal governance bodies and greater recognition of general practitioners. Less commonly reported were calls for better education and information to support engagement, greater empathy from institutions, improved accessibility or barrier-free opportunities, reduced bureaucratic barriers, and increased trust in health authorities or researchers.
Requests for “communication on equal terms” and the use of clear, simple language, especially for people with intellectual disabilities or limited language proficiency, were common. As one participant put it, “General practitioners should have more time to listen to patients.’ Another emphasized that patients “should be perceived as persons, not as numbers.” Respondents highlighted the need for more time with physicians and other health professionals to allow for genuine listening and dialogue beyond routine consultations.
Several comments called for formal mechanisms that would give patients and caregivers a recognized voice in decision-making. Suggestions included the creation or revival of decision-making bodies that include “experts by experience,” systematic integration of patient organizations into planning processes, and designated contact persons within the health authority to address concerns. Some respondents asked for greater recognition of general practitioners within the regional health service and for the simplification of bureaucratic procedures, such as easier booking systems or more transparent administrative pathways.
Participants advocated for improved health education and public campaigns, such as organ donation awareness and better information on chronic diseases, to empower citizens to participate effectively. One long and detailed statement called for “systematic integration of patient organizations; transparent communication and co-design; participation in clinical research through patient advisory boards; and structured opportunities for feedback, such as patient portals or satisfaction surveys, that are taken seriously and used to achieve concrete improvements.”
3.3.2. Preferred Modes of Participation in Setting Research Priorities
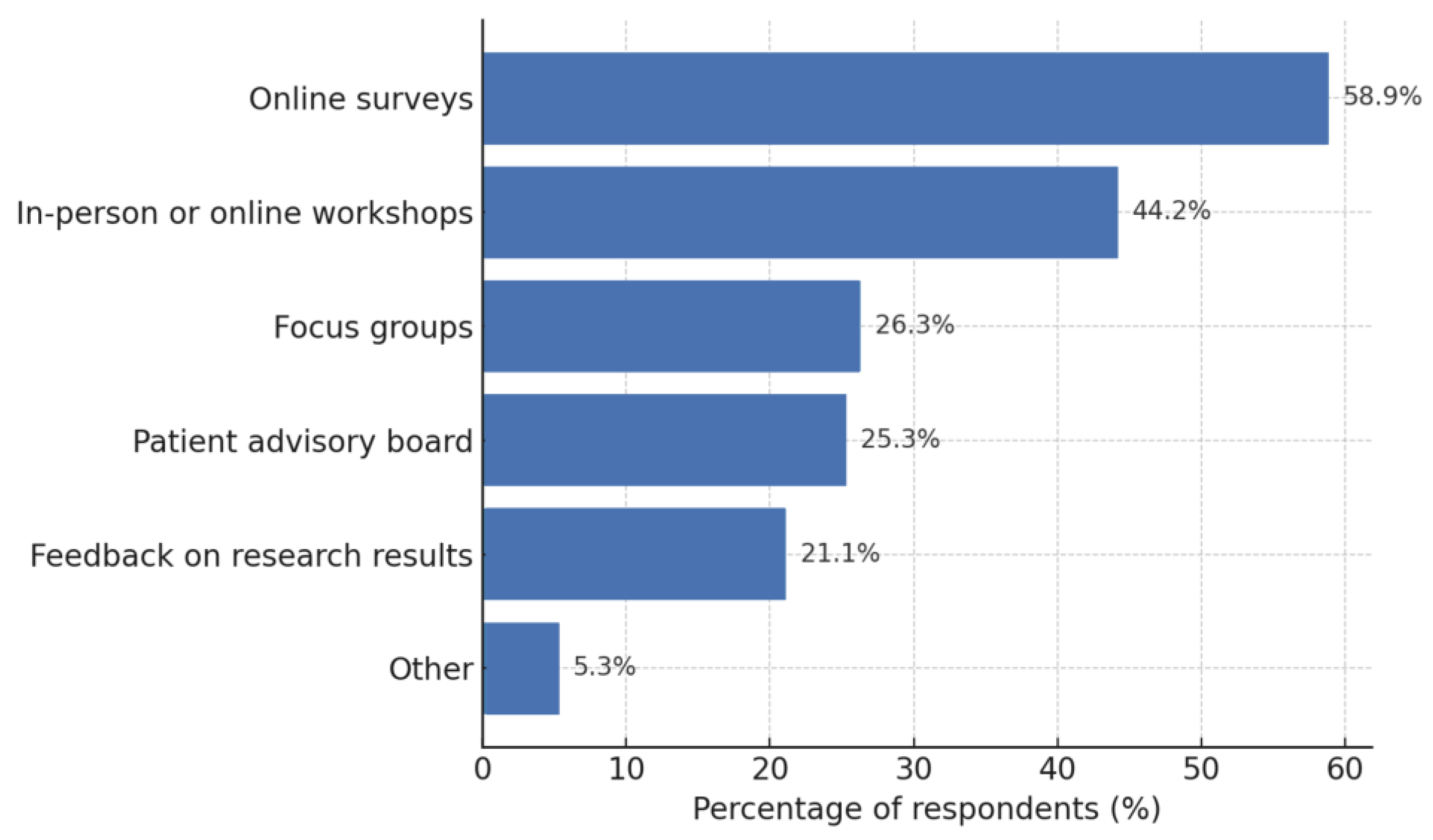
The survey asked respondents how they would prefer to participate in defining research priorities (“How would you prefer to participate in setting research priorities?). Select up to two options”). All answers were content coded into binary variables to capture the presence of each predefined option, allowing multiple selections per respondent.
Figure 3 displays the proportion of all 95 respondents who selected each participation mode. Online surveys were the most frequently chosen format, followed by participation in in-person or online workshops and involvement in patient advisory boards. Roughly one quarter indicated interest in focus groups and one fifth in providing feedback on the research results. A small minority (5.3%) provided free-text suggestions outside the predefined options, mainly calling for direct personal dialogue with researchers or hybrid formats that combine elements of surveys and workshops.
4. Discussion
This priority-setting survey demonstrated stakeholder engagement and clarity of the research agenda. Although most respondents represented PSIOs, leadership positions were well represented, providing perspectives from individuals pivotal to patient involvement and citizen science. Across this diverse group, long waiting times and shortages of healthcare personnel emerged as the most pressing barriers to healthcare access, while the highest research priorities focused on the mental health of children and adolescents, continuity and trust in primary care, and patient-centered palliative and end-of-life care. Interest in active participation in research was substantial, with nearly 40% expressing definite willingness and more than half requesting additional information, indicating potential partners for collaborative research and health-system development. These findings highlight the need for collective awareness of system bottlenecks, convergent research priorities, and readiness among PSIOs to engage in future participatory research efforts.
4.1. Respondent Characteristics
The linguistic distribution of the responses reflects South Tyrol's demographics, where approximately 68% of the population is German-speaking and 27% Italian-speaking [
11]. In our sample, 71.2% of the answers were in German and 28.8% in Italian. This indicates that the survey captured the region's two majority language groups while potentially underrepresenting linguistic minorities, possibly including participants with missing free-text responses.
Interest in participatory research did not differ between German- and Italian-speaking respondents, showing linguistic background did not affect research collaboration willingness. Evidence suggests language alone does not influence participation when engagement methods are inclusive. Successful engagement across linguistic groups depends more on quality facilitation, trust-building, and accessible materials than specific language [
12,
13,
14,
15].
Common barriers to healthcare access—long waiting times, staff shortages, and bureaucratic procedures—indicate system-level challenges affecting the population. Less frequent obstacles like language barriers, trust issues, and mobility limitations highlight burdens faced by disadvantaged groups. Long waiting times, staff shortages, and bureaucratic procedures represent system-level obstacles that disproportionately affect those with fewer resources [
16,
17]. Such barriers discourage access to care by contributing to perceptions of inaccessibility [
17]. These findings demonstrate why perceived barriers matter: they shape participation conditions and require addressing. Language barriers, trust issues, and mobility limitations particularly affect disadvantaged groups like migrants and people with disabilities, who risk underrepresentation without targeted measures [
18,
19]. Addressing these barriers through trust-building and accessible formats is essential for equitable inclusion [
17,
19].
4.2. Research Priority Ratings
The identified prioritization patterns highlight challenges for healthcare systems, with youth mental health, continuity of primary care, and palliative care receiving the highest rankings. The urgency of youth mental health reflects a global crisis exacerbated by COVID-19, with increasing psychological distress and unmet needs among adolescents and young adults [
20,
21,
22]. Evidence shows that delayed detection and care lead to worse outcomes, underscoring the need for integrated, accessible, and youth-friendly primary care models [
23,
24]. Continuity in primary care was prioritized, consistent with findings that sustained provider relationships reduce hospitalizations, improve care transitions, and strengthen patient outcomes [
25,
26]. The high priority for palliative care reflects the growing recognition of patient-centered approaches in serious illness management, particularly in improving the quality of life and aligning care with patient values, although mental health support remains insufficient [
27,
28].
Reliable health information and equitable access for disadvantaged groups have emerged as priorities, highlighting their role in reducing inequities and responding to systemic challenges. International evidence shows that socioeconomically disadvantaged, minority, rural, and older populations face barriers, including limited digital access and skills [
29,
30], low health literacy [
31,
32], and structural obstacles such as language barriers, discrimination, and limited trust in providers [
33,
34]. These findings mirror respondents' concerns and emphasize the need for culturally tailored interventions that engage affected groups in health information design and delivery [
31,
35].
Moderate priorities, such as GP choice, frailty detection, and school health education, were rated secondary to urgent issues, whereas sustainable prescribing, gender stress differences, and vaccine acceptance received lower priority. This suggests that respondents viewed the immediate challenges of mental health, care continuity, and access as more pressing than structural or long-term issues.
The absence of significant differences between GPs and PSIOs indicates a consensus across stakeholder groups rather than profession-specific agendas. Similar findings have been reported in structured priority-setting processes, where clinicians and patient stakeholders emphasize quality of care, access, and care models [
36,
37,
38]. Evidence from cancer and general practice research shows convergence, with prevention, survivorship, and care coordination being rated highly across groups [
39]. This alignment strengthens the legitimacy of the present results as a foundation for future participatory research. When priorities are shared, the resulting agendas are more inclusive, less vulnerable to claims of narrow professional bias, and more likely to attract support, funding, and implementation [
2,
36,
40]. Broad agreement across stakeholders thus enhances the credibility of identified priorities and underscores the value of participatory approaches in ensuring that health research addresses community-relevant concerns.
4.3. Interest in Research Participation
Interest in future research participation was moderate, with approximately 38% of respondents expressing willingness, 10% declining, and just over half reporting uncertainty. This distribution mirrors findings from other contexts, where many potential participants remain undecided until they receive clearer information about the study’s aims, procedures, and benefits [
41,
42,
43]. Uncertainty often reflects not a lack of interest but the need for greater trust, reassurance about ethical safeguards, and practical support to overcome perceived barriers to participation [
44,
45]. Evidence shows that transparent communication, trust-building, and reducing the logistical burden of participation can help translate moderate levels of willingness into active engagement [
41,
46,
47].
PSIO board and leadership members showed more interest in future research participation than staff, with GPs between, though differences were not statistically significant. This aligns with studies showing professional role alone does not predict research engagement [
48,
49]. GPs have been described as difficult to recruit, with willingness varying by age, gender, and practice context [
50]. Education, prior research experience, and organizational support are stronger determinants of participation, highlighting the importance of fostering a supportive research culture across professional roles in nursing.
Correlation analyses revealed minor negative associations between participation willingness and priority ratings for palliative care, continuity of care, and family stress, while strong positive correlations existed among other topics. Willingness to engage in research was largely independent of topic preferences, though those rating sensitive areas as priorities appeared less inclined to participate. This aligns with evidence that emotionally taxing research topics may reduce participation willingness [
42,
43,
50].
The correlations between topics like frailty and palliative care, school health education and family stress, and primary care continuity and prescribing, indicate their interconnected nature. This clustering reflects a systems perspective, emphasizing integrated health approaches, consistent with priority-setting studies showing related theme groupings [
51,
52]. The results support that these research areas were perceived as jointly important, underscoring the coherence of the identified agenda.
4.4. Preferred Modes of Research Participation
In this study, online surveys have emerged as the preferred mode of participation, reflecting convenience, flexibility, and privacy. This finding aligns with evidence that mode preference predicts actual participation in web-based studies [
53,
54,
55]. Workshops and patient advisory boards were frequently mentioned, suggesting participants value interactive and collaborative formats, despite greater time commitment and institutional support [
51,
56]. Focus groups and feedback on research results were less prioritized, indicating dialogic approaches appeal to a smaller subgroup [
57,
58]. Finally, only a minority preferred free-text or hybrid formats, showing that while flexibility is welcomed, most participants prefer structured modes [
51,
59].
4.5. Recommendations for Enhancing Research Participation
While few respondents had prior structured patient involvement experience, most were willing to engage in future research activities, suggesting the potential for participatory approaches with proper support. Evidence shows that effective engagement relies more on creating conditions that empower contributors and establish inclusive partnerships than on baseline familiarity [
51,
60,
61,
62,
63].
Respondents emphasized clear communication, dialogue time, and inclusion strategies, aligning with best practices for patient involvement in health research. Transparent communication about involvement in activities builds trust [
51,
63,
64]. Regular feedback and demonstration of how input shapes decisions strengthen engagement.
Sufficient time and resources enable meaningful engagement, as tokenistic processes risk limiting impact [
51,
63]. Diversity requires flexible meeting formats and support for patients, PSIOs, and GPs [
65,
66]. Recognizing each group's expertise, particularly GPs' practical knowledge, bridges professional and community perspectives [
51,
66]. Shared decision-making approaches that respect all voices lead to greater trust and research impact [
60,
64].
In line with our results, where only 15.8% reported prior involvement but most expressed definite or conditional willingness, education and training can build confidence and capacity, while empathetic engagement and accessible processes lower barriers to entry [
67,
68,
69]. Conversely, concerns about administrative burdens and institutional transparency reflect well-documented obstacles that deter participation, underscoring the need for structural solutions and feedback mechanisms to translate willingness into active involvement [
67,
68].
4.5. Strengths and Limitations
This study had several strengths. This study represents the first structured, bilingual, participatory survey on health services research priorities in South Tyrol, a region marked by linguistic and cultural diversity. The inclusion of both German- and Italian-speaking organizations ensured coverage of the region’s two main language groups, and the involvement of PSIOs provided perspectives beyond those of professionals. With 64 PSIOs active in a region of approximately 530,000 inhabitants, their numbers and participation provide a robust base for priority setting. The bilingual design, piloted by experts with clinical and methodological backgrounds, and the combination of structured items with open-ended questions enhanced contextual relevance and validity.
This study has several limitations must be acknowledged. Most importantly, the response rate among GPs was alarmingly low, with only nine of 290 invited GPs responding. This likely reflects a combination of factors, including the reliance on a single email invitation and one reminder, the risk that messages were overlooked, and the well-documented challenges of engaging GPs in research, such as limited time and the perceived low relevance of academic studies to daily practice [
50,
52]. Consequently, the GP perspective is underrepresented in the findings, reducing the generalizability of the conclusions regarding professional stakeholders. In addition, although the predefined list of research topics was informed by the literature and regional program activities, framing effects may have influenced responses, and certain topics may have been overlooked.
Given the exploratory nature of this study, no formal adjustment for multiple tests was performed. While this approach allows for the identification of potentially relevant patterns, some associations may represent chance findings. As a sensitivity consideration, applying a Benjamini–Hochberg false discovery rate (FDR) control at q = 0.10 would likely confirm strong inter-topic associations, but marginal effects should be interpreted cautiously [
70].
Finally, although the cross-sectional design provides a snapshot of current priorities, it cannot assess how these priorities evolve over time or whether they ultimately inform policy and practice.
5. Conclusions
This study provides the first systematic bilingual assessment of health service research priorities in South Tyrol, engaging both GPs and PSIOs in a participatory process. Despite the very low GP response rate, the participation of community organizations highlights the feasibility and value of including diverse stakeholders in regional priority setting.
The findings emphasize the centrality of child and adolescent mental health, continuity and trust in primary care, and palliative and end of life care as top priorities, alongside enduring concerns about equitable access and reliable health information. While participatory approaches revealed broad agreement, the study also uncovered practical barriers to engagement, including limited prior involvement and a preference for low-burden participation modes, such as online surveys.
These results demonstrate that participatory approaches can generate priorities that are context-specific, patient-centered, and relevant to health policy and service development in a culturally diverse region. Future efforts should build on this foundation by improving the recruitment of healthcare professionals, strengthening structural mechanisms for patient and public involvement, and ensuring that identified priorities are systematically linked to research funding and policy decisions.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, File: Shaping research together – questionnaire.
Author Contributions
Conceptualization, A.E., D.H., G.P. and C.J.W.; methodology, C.J.W., V.B., A.M. and C.F.; formal analysis, investigation, and data curation, C.J.W.; writing—original draft preparation, C.J.W.; writing—review and editing, D.H., G.P., V.B., A.M., and C.F.; supervision, A.E. . All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study because the survey did not involve patients, clinical interventions, or the collection of sensitive or personally identifiable health data. The Committee for Clinical Research Ethics of the South Tyrolean Health Authority confirmed in writing that no formal evaluation or authorization was required (communication dated 31 July 2025).
Informed Consent Statement
Participation in the online survey was voluntary and anonymous. Respondents were informed about the purpose of the study on the first page of the questionnaire, and completion of the survey implied consent.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI |
Artificial intelligence |
| FDR |
False discovery rate |
| GP |
General practitioner |
| IQR |
Interquartile range |
| PSIO |
Patient and social interest organization |
| SD |
Standard deviation |
References
- Boivin, A.; Lehoux, P.; Lacombe, R.; Burgers, J.; Grol, R. Involving Patients in Setting Priorities for Healthcare Improvement: A Cluster Randomized Trial. Implement Sci 2014, 9, 24.
- Manafò, E.; Petermann, L.; Vandall-Walker, V.; Mason-Lai, P. Patient and Public Engagement in Priority Setting: A Systematic Rapid Review of the Literature. PLoS One 2018, 13, e0193579.
- Thumboo, J.; Yoon, S.; Wee, S.; Yeam, C.T.; Low, E.C.T.; Lee, C.E. Developing Population Health Research Priorities in Asian City State: Results from a Multi-Step Participatory Community Engagement. PLoS One 2019, 14, e0216303. [CrossRef]
- MacFarlane, A.; Phelan, H.; Papyan, A.; Hassan, A.; Garry, F. Research Prioritization in Migrant Health in Ireland: Toward a Participatory Arts-Based Paradigm for Academic Primary Care. Ann Fam Med 2022, 20, 2727. [CrossRef]
- Pratt, B. Inclusion of Marginalized Groups and Communities in Global Health Research Priority-Setting. J Empir Res Hum Res Ethics 2019, 14, 169–181. [CrossRef]
- Tilahun, B.; Amare, G.; Endehabtu, B.F.; Atnafu, A.; Derseh, L.; Gurmu, K.K.; Delllie, E.; Nigusie, A. Explore the Practice and Barriers of Collaborative Health Policy and System Research-Priority Setting Exercise in Ethiopia. Health Res Policy Syst 2024, 22, 64. [CrossRef]
- Crowe, S.; Fenton, M.; Hall, M.; Cowan, K.; Chalmers, I. Patients’, Clinicians’ and the Research Communities’ Priorities for Treatment Research: There Is an Important Mismatch. Res Involv Engagem 2015, 1, 2. [CrossRef]
- Wiedermann, C.J.; Piccoliori, G.; Engl, A. Supporting Primary Care Communication on Vaccination in Multilingual and Culturally Diverse Settings: Lessons from South Tyrol, Italy. Epidemiologia (Basel) 2025, 6, 50. [CrossRef]
- Ausserhofer, D.; Barbieri, V.; Lombardo, S.; Gärtner, T.; Eisendle, K.; Piccoliori, G.; Engl, A.; Wiedermann, C.J. Health Literacy Gaps Across Language Groups: A Population-Based Assessment in Alto Adige/South Tyrol, Italy. Eur J Investig Health Psychol Educ 2025, 15, 153. [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates. Hillsdale, NJ 1988, 20–26.
- Ergebnisse Sprachgruppenzählung - 2024 | Publikationen und verschiedene Statistiken diverser Themen Available online: https://astat.provincia.bz.it/de/publikationen/ergebnisse-sprachgruppenzahlung-2024 (accessed on 30 September 2025).
- Quinton, S.; Treveri Gennari, D.; Dibeltulo, S. Engaging Older People through Visual Participatory Research: Insights and Reflections. Qual Res 2023, 23, 1647–1668.
- Fischer, K.; Schulz, K.; Chenais, E. “Can We Agree on That”? Plurality, Power and Language in Participatory Research. Prev Vet Med 2020, 180, 104991. [CrossRef]
- Purschke, C. Crowdscapes. Participatory Research and the Collaborative (Re) Construction of Linguistic Landscapes with Lingscape. Lingv Vanguard 2021, 7, 20190032.
- Sisenop, F.S.; Natan, M.N.; Lindert, J.L. Community-Based Participatory Research in Population-Based Health Surveys-a Case Example from East Friesland (Germany). Eur J Public Health 2020, 30, ckaa165. 954.
- Loignon, C.; Hudon, C.; Goulet, É.; Boyer, S.; De Laat, M.; Fournier, N.; Grabovschi, C.; Bush, P. Perceived Barriers to Healthcare for Persons Living in Poverty in Quebec, Canada: The EQUIhealThY Project. Int J Equity Health 2015, 14, 4. [CrossRef]
- O’Donnell, P.; Tierney, E.; O’Carroll, A.; Nurse, D.; MacFarlane, A. Exploring Levers and Barriers to Accessing Primary Care for Marginalised Groups and Identifying Their Priorities for Primary Care Provision: A Participatory Learning and Action Research Study. Int J Equity Health 2016, 15, 197. [CrossRef]
- Markey, K.; Noonan, M.; Doody, O.; Tuohy, T.; Daly, T.; Regan, C.; O’Donnell, C. Fostering Collective Approaches in Supporting Perinatal Mental Healthcare Access for Migrant Women: A Participatory Health Research Study. Int J Environ Res Public Health 2022, 19, 1124. [CrossRef]
- Turin, T.C.; Chowdhury, N.; Haque, S.; Rumana, N.; Rahman, N.; Lasker, M.A.A. Meaningful and Deep Community Engagement Efforts for Pragmatic Research and beyond: Engaging with an Immigrant/Racialised Community on Equitable Access to Care. BMJ Glob Health 2021, 6, e006370. [CrossRef]
- Colizzi, M.; Lasalvia, A.; Ruggeri, M. Prevention and Early Intervention in Youth Mental Health: Is It Time for a Multidisciplinary and Trans-Diagnostic Model for Care? Int J Ment Health Syst 2020, 14, 23. [CrossRef]
- McGorry, P.D.; Mei, C.; Chanen, A.; Hodges, C.; Alvarez-Jimenez, M.; Killackey, E. Designing and Scaling up Integrated Youth Mental Health Care. World Psychiatry 2022, 21, 61–76. [CrossRef]
- Wiedermann, C.J.; Barbieri, V.; Plagg, B.; Marino, P.; Piccoliori, G.; Engl, A. Fortifying the Foundations: A Comprehensive Approach to Enhancing Mental Health Support in Educational Policies Amidst Crises. Healthcare (Basel) 2023, 11. [CrossRef]
- Duong, M.T.; Bruns, E.J.; Lee, K.; Cox, S.; Coifman, J.; Mayworm, A.; Lyon, A.R. Rates of Mental Health Service Utilization by Children and Adolescents in Schools and Other Common Service Settings: A Systematic Review and Meta-Analysis. Adm Policy Ment Health 2021, 48, 420–439. [CrossRef]
- MacDonald, K.; Fainman-Adelman, N.; Anderson, K.K.; Iyer, S.N. Pathways to Mental Health Services for Young People: A Systematic Review. Soc Psychiatry Psychiatr Epidemiol 2018, 53, 1005–1038. [CrossRef]
- Toulany, A.; Stukel, T.A.; Kurdyak, P.; Fu, L.; Guttmann, A. Association of Primary Care Continuity With Outcomes Following Transition to Adult Care for Adolescents With Severe Mental Illness. JAMA Netw Open 2019, 2, e198415. [CrossRef]
- Khatri, R.; Endalamaw, A.; Erku, D.; Wolka, E.; Nigatu, F.; Zewdie, A.; Assefa, Y. Continuity and Care Coordination of Primary Health Care: A Scoping Review. BMC Health Serv Res 2023, 23, 750. [CrossRef]
- Block, S. Our Unrealized Imperative: Integrating Mental Health Care into Hospice and Palliative Care. J Palliat Med 2025, 28, 151–161. [CrossRef]
- Shalev, D.; Robbins-Welty, G.; Ekwebelem, M.; Moxley, J.; Riffin, C.; Reid, M.C.; Kozlov, E. Mental Health Integration and Delivery in the Hospice and Palliative Medicine Setting: A National Survey of Clinicians. J Pain Symptom Manage 2024, 67, 77–87. [CrossRef]
- Kaihlanen, A.-M.; Virtanen, L.; Buchert, U.; Safarov, N.; Valkonen, P.; Hietapakka, L.; Hörhammer, I.; Kujala, S.; Kouvonen, A.; Heponiemi, T. Towards Digital Health Equity - a Qualitative Study of the Challenges Experienced by Vulnerable Groups in Using Digital Health Services in the COVID-19 Era. BMC Health Serv Res 2022, 22, 188. [CrossRef]
- Cheng, C.; Beauchamp, A.; Elsworth, G.R.; Osborne, R.H. Applying the Electronic Health Literacy Lens: Systematic Review of Electronic Health Interventions Targeted at Socially Disadvantaged Groups. J Med Internet Res 2020, 22, e18476. [CrossRef]
- Stormacq, C.; Wosinski, J.; Boillat, E.; Van den Broucke, S. Effects of Health Literacy Interventions on Health-Related Outcomes in Socioeconomically Disadvantaged Adults Living in the Community: A Systematic Review. JBI Evid Synth 2020, 18, 1389. [CrossRef]
- Stormacq, C.; Oulevey Bachmann, A.; Van den Broucke, S.; Bodenmann, P. How Socioeconomically Disadvantaged People Access, Understand, Appraise, and Apply Health Information: A Qualitative Study Exploring Health Literacy Skills. PLoS One 2023, 18, e0288381. [CrossRef]
- Ford, J.A.; Wong, G.; Jones, A.P.; Steel, N. Access to Primary Care for Socioeconomically Disadvantaged Older People in Rural Areas: A Realist Review. BMJ Open 2016, 6, e010652. [CrossRef]
- McFadden, A.; Siebelt, L.; Gavine, A.; Atkin, K.; Bell, K.; Innes, N.; Jones, H.; Jackson, C.; Haggi, H.; MacGillivray, S. Gypsy, Roma and Traveller Access to and Engagement with Health Services: A Systematic Review. Eur J Public Health 2018, 28, 74–81. [CrossRef]
- O’Mara-Eves, A.; Brunton, G.; Oliver, S.; Kavanagh, J.; Jamal, F.; Thomas, J. The Effectiveness of Community Engagement in Public Health Interventions for Disadvantaged Groups: A Meta-Analysis. BMC Public Health 2015, 15, 129. [CrossRef]
- Zarin, W.; Sreetharan, S.; Doherty-Kirby, A.; Scott, M.; Zibrowski, E.; Soobiah, C.; Elliott, M.; Chaudhry, S.; Al-Khateeb, S.; Tam, C.; et al. Patient- and Public-Driven Health Research: A Model of Co-Leadership and Partnership in Research Priority Setting Using a Modified James Lind Alliance Approach. J Clin Epidemiol 2025, 181, 111731. [CrossRef]
- Heal, C.; Roberts, G. General Practice Research Priority Setting in Australia: Informing a Research Agenda to Deliver Best Patient Care. Aust J Gen Pract 2019, 48, 789–795. [CrossRef]
- Abrams, R.; Blake, S. UK General Practice Service Delivery Research Priorities: An Adapted James Lind Alliance Approach. Br J Gen Pract 2024, 74, e9–e16. [CrossRef]
- Milley, K.; Druce, P.; McNamara, M.; Bergin, R.J.; Chan, R.J.; Cust, A.E.; Davis, N.; Fishman, G.; Jefford, M.; Rankin, N.; et al. Cancer in General Practice Research Priorities in Australia. Aust J Gen Pract 2024, 53, 227–234. [CrossRef]
- Howard, A.F.; Warner, L.; Cuthbertson, L.; Sawatzky, R. Patient-Driven Research Priorities for Patient-Centered Measurement. BMC Health Serv Res 2024, 24, 735. [CrossRef]
- Liang, J.-E.; Liang, M.-Y.; Zhang, E.-E.; Peng, Y.-Y.; Chen, L.-L.; Deng, J.-Y.; Lin, T.; Fu, J.; Zhang, J.-N.; Li, S.-L.; et al. Factors Influencing Willingness to Participate in Ophthalmic Clinical Trials and Strategies for Effective Recruitment. Int J Ophthalmol 2024, 17, 157–163. [CrossRef]
- Glass, D.C.; Kelsall, H.L.; Slegers, C.; Forbes, A.B.; Loff, B.; Zion, D.; Fritschi, L. A Telephone Survey of Factors Affecting Willingness to Participate in Health Research Surveys. BMC Public Health 2015, 15, 1017. [CrossRef]
- Gayet-Ageron, A.; Rudaz, S.; Perneger, T. Study Design Factors Influencing Patients’ Willingness to Participate in Clinical Research: A Randomised Vignette-Based Study. BMC Med Res Methodol 2020, 20, 93. [CrossRef]
- Raimundo-Silva, V.; Marques, C.T.; Fonseca, J.R.; Martínez-Silveira, M.S.; Reis, M.G. Factors Related to Willingness to Participate in Biomedical Research on Neglected Tropical Diseases: A Systematic Review. PLoS Negl Trop Dis 2024, 18, e0011996. [CrossRef]
- Liu, H.-E.; Li, M.-C. Factors Influencing the Willingness to Participate in Medical Research: A Nationwide Survey in Taiwan. PeerJ 2018, 6, e4874. [CrossRef]
- Smyth, J.M.; Jones, D.R.; Wen, C.K.F.; Materia, F.T.; Schneider, S.; Stone, A. Influence of Ecological Momentary Assessment Study Design Features on Reported Willingness to Participate and Perceptions of Potential Research Studies: An Experimental Study. BMJ Open 2021, 11, e049154. [CrossRef]
- Kelly, B.; Margolis, M.; McCormack, L.; LeBaron, P.A.; Chowdhury, D. What Affects People’s Willingness to Participate in Qualitative Research? An Experimental Comparison of Five Incentives. Field Methods 2017, 29, 333–350.
- Amicucci, M.; Dall’Oglio, I.; Biagioli, V.; Gawronski, O.; Piga, S.; Ricci, R.; Angelaccio, A.; Elia, D.; Fiorito, M.E.; Marotta, L.; et al. Participation of Nurses and Allied Health Professionals in Research Activities: A Survey in an Academic Tertiary Pediatric Hospital. BMC Nurs 2022, 21, 159. [CrossRef]
- Wenke, R.; Mickan, S. The Role and Impact of Research Positions within Health Care Settings in Allied Health: A Systematic Review. BMC Health Serv Res 2016, 16, 355. [CrossRef]
- Tawo, S.; Gasser, S.; Gemperli, A.; Merlo, C.; Essig, S. General Practitioners’ Willingness to Participate in Research: A Survey in Central Switzerland. PLoS One 2019, 14, e0213358. [CrossRef]
- Burke, N.N.; Stewart, D.; Tierney, T.; Worrall, A.; Smith, M.; Elliott, J.; Beecher, C.; Devane, D.; Biesty, L. Sharing Space at the Research Table: Exploring Public and Patient Involvement in a Methodology Priority Setting Partnership. Res Involv Engagem 2023, 9, 29. [CrossRef]
- Virnau, L.; Braesigk, A.; Deutsch, T.; Bauer, A.; Kroeber, E.S.; Bleckwenn, M.; Frese, T.; Lingner, H. General Practitioners’ Willingness to Participate in Research Networks in Germany. Scand J Prim Health Care 2022, 40, 237–245. [CrossRef]
- Olson, K.; Smyth, J.D.; Wood, H.M. Does Giving People Their Preferred Survey Mode Actually Increase Survey Participation Rates? An Experimental Examination. Public Opin Q 2012, 76, 611–635. [CrossRef]
- Mulder, J.; De Bruijne, M. Willingness of Online Respondents to Participate in Alternative Modes of Data Collection. Surv Pract 2019, 12. [CrossRef]
- Nkyekyer, J.; Clifford, S.A.; Mensah, F.K.; Wang, Y.; Chiu, L.; Wake, M. Maximizing Participant Engagement, Participation, and Retention in Cohort Studies Using Digital Methods: Rapid Review to Inform the Next Generation of Very Large Birth Cohorts. J Med Internet Res 2021, 23, e23499. [CrossRef]
- Romsland, G.I.; Milosavljevic, K.L.; Andreassen, T.A. Facilitating Non-Tokenistic User Involvement in Research. Res Involv Engagem 2019, 5, 18. [CrossRef]
- Cook, S.; Mayers, S.; Goggins, K.; Schlundt, D.; Bonnet, K.; Williams, N.; Alcendor, D.; Barkin, S. Assessing Research Participant Preferences for Receiving Study Results. J Clin Transl Sci 2019, 4, 243–249. [CrossRef]
- Urry, K.; Chur-Hansen, A.; Scholz, B. From Member Checking to Collaborative Reflection: A Novel Way to Use a Familiar Method for Engaging Participants in Qualitative Research. Qual Res Psychol 2024, 21, 357–374. [CrossRef]
- Staley, K.; Barron, D. Learning as an Outcome of Involvement in Research: What Are the Implications for Practice, Reporting and Evaluation? Res Involv Engagem 2019, 5, 14. [CrossRef]
- Price, A.; Clarke, M.; Staniszewska, S.; Chu, L.; Tembo, D.; Kirkpatrick, M.; Nelken, Y. Patient and Public Involvement in Research: A Journey to Co-Production. Patient Educ Couns 2022, 105, 1041–1047. [CrossRef]
- Summers, B.; Farmer, L.; Cooper, S.; von Wagner, C.; Friedrich, B.; Abel, G.A.; Spencer, A.; Cockcroft, E. Patient Bridge Role: A New Approach for Patient and Public Involvement in Healthcare Research Programmes. BMJ Open 2025, 15, e094521. [CrossRef]
- Smits, D.-W.; van Meeteren, K.; Klem, M.; Alsem, M.; Ketelaar, M. Designing a Tool to Support Patient and Public Involvement in Research Projects: The Involvement Matrix. Res Involv Engagem 2020, 6, 30. [CrossRef]
- Liabo, K.; Boddy, K.; Bortoli, S.; Irvine, J.; Boult, H.; Fredlund, M.; Joseph, N.; Bjornstad, G.; Morris, C. Public Involvement in Health Research: What Does “good” Look like in Practice? Res Involv Engagem 2020, 6, 11. [CrossRef]
- Hoddinott, P.; Pollock, A.; O’Cathain, A.; Boyer, I.; Taylor, J.; MacDonald, C.; Oliver, S.; Donovan, J.L. How to Incorporate Patient and Public Perspectives into the Design and Conduct of Research. F1000Res 2018, 7, 752. [CrossRef]
- Cook, N.; Siddiqi, N.; Twiddy, M.; Kenyon, R. Patient and Public Involvement in Health Research in Low and Middle-Income Countries: A Systematic Review. BMJ Open 2019, 9, e026514. [CrossRef]
- Hatch, S.; Fitzgibbon, J.; Tonks, A.J.; Forty, L. Diversity in Patient and Public Involvement in Healthcare Research and Education-Realising the Potential. Health Expect 2024, 27, e13896. [CrossRef]
- Matheson, M.; Skinner, I.W.; Vehagen, A.; Auliffe, S.M.; Malliaras, P. Barriers and Enablers of Primary Healthcare Professionals in Health Research Engagement: A Systematic Review of Qualitative Studies. Nurs Health Sci 2025, 27, e70022. [CrossRef]
- Staniszewska, S.; Denegri, S.; Matthews, R.; Minogue, V. Reviewing Progress in Public Involvement in NIHR Research: Developing and Implementing a New Vision for the Future. BMJ Open 2018, 8, e017124. [CrossRef]
- Sheridan, R.; Martin-Kerry, J.; Hudson, J.; Parker, A.; Bower, P.; Knapp, P. Why Do Patients Take Part in Research? An Overview of Systematic Reviews of Psychosocial Barriers and Facilitators. Trials 2020, 21, 259. [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc B 1995, 57, 289–300. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).