1. Introduction
As the global population ages, the number of people living with dementia has rapidly increased. Alzheimer’s disease is the most common ailment, accounting for the majority of cases worldwide. Dementia causes profound physical, psychological, social, and economic effects, not only on the patients, but also on their caregivers, families, and society [
1,
2]. Consequently, dementia has emerged as a major global public health issue and an important national policy priority in many countries.
Dementia should not be viewed solely as a medical disease; rather, it is a complex condition requiring a holistic approach that considers an individual’s life context, personal relationships, and broader social environment [
2]. Thus, dementia care cannot be confined to symptom management or pharmacological treatment alone. It requires comprehensive, person-centered care that respects the individuality, dignity, and life stories of the patient [
2].
The Japanese Medical Specialty Board formally designated “general medicine (GM)” as the nineteenth basic medical specialty in 2014. Training under the new board certification program began in 2018 [
3,
4,
5]. Physicians involved in this emerging specialty are responsible for providing comprehensive, cross-cutting care that spans multiple settings and patient conditions. GM in Japan consists of two subspecialties: family medicine (FM) [
6] and hospital general medicine (HGM) [
7]. FM focuses on community-based primary care, whereas HGM emphasizes leadership, acute care coordination, and governance within a hospital setting [
4,
5,
6,
7].
As the system is in its formative stage, the role of GM physicians, including FM and HGM, has not been firmly established, and their professional identities continue to evolve [
4,
5,
8]. This ambiguity extends to dementia care, although GM physicians are increasingly involved; however, there is no standardized, nationwide role for them in dementia diagnosis or management. Despite these limitations, there is growing recognition of their potential to serve as versatile, community-anchored providers, to ensure continuity of care across outpatient and inpatient settings [
5].
Unlike organ-specific specialists, GM physicians care for the whole person. They not only address physical symptoms, but also psychological, social, and environmental problems. Thus, they treat individuals, not just diseases [
3]. Their approach focuses on longitudinal, relationship-based management that integrates medical, psychological, and social aspects of health [
3,
4,
5]. Moreover, their training includes ambulatory and hospital care, which ideally positions them to provide seamless support throughout the course of chronic conditions, such as dementia [
3,
4,
5,
6,
7].
Although the role of the GM physician in dementia care continues to evolve, their contribution to early detection, continuity of care, and community integration has been increasingly recognized. As Japan’s population continues to age [
9], incorporating GM physicians into dementia care frameworks represents an important innovation.
This review focuses on dementia as a representative condition to determine how GM physicians, while still developing their professional identity within Japan’s healthcare system, can uniquely embody the principles of person-centered care and support the evolving community-based integrated care framework.
2. Methods
2.1. Literature Search Strategy
This review includes literature published between January 2010 and July 2025, which captures the evolution and institutionalization of modern dementia care strategies worldwide. This is reflected in the growing emphasis on integrated, community-centered care models highlighted in the World Alzheimer Reports 2010 [
10] and 2013 [
11]. It also encompasses the development of key domestic frameworks in Japan, including the launch of the Community-Based Integrated Care System (CBICS) in 2012 [
12] and the introduction of board-certified GM physician training in 2018 [
3]. These milestones have contributed to modern primary care and dementia care infrastructure.
English-language, peer-reviewed articles were identified from the PubMed, Scopus, Web of Science, CiNii and J-Stage databases using combinations of the following keywords: “dementia,” “general medicine,” “primary care,” “family medicine,” “hospitalist,” “generalist physician,” “integrated care,” “Japan,” “United States,” “United Kingdom,” “Canada,” “community-based care,” and “early diagnosis.” These terms were used to capture literature relevant to dementia care delivery in generalist and primary care settings in Japan and other countries.
Japanese-language materials were also sourced from official websites and government databases, including the Ministry of Health, Labour and Welfare [
9,
12,
13], the Japanese Medical Specialty Board [
3], Japan Primary Care Association [
6], and Japanese Society of Hospital General Medicine [
7]. These sites provide insight into domestic policy frameworks, including the CBICS [
12] and GM physician (FM and HGM) training programs [
3,
6,
7]. In addition, studies were included based on their relevance to dementia care models, GM physician roles, care integration strategies, and healthcare system-level comparisons. Empirical and conceptual or policy-oriented literature was reviewed to enable a comprehensive analysis.
2.2. Terminology and Abbreviations
To ensure clarity and consistency, the following terminology is used when referring to primary care providers and generalist physicians in the different healthcare systems:
United States (US): Primary Care Physicians (PCPs) - generalist physicians responsible for both first-contact and continuous care [
14].
United Kingdom (UK): General Practitioners (GPs) - primary care physicians and gatekeepers within the National Health Service [
15].
Canada: Family Physicians (FPs) - generalists who deliver comprehensive primary care across all age groups [
16].
Japan: Kakaritsuke Physicians (Kakaritsuke-I) - physicians who provide routine community-based care. This is a functional role rather than a standardized certification or a formal gatekeeping function [
17,
18].
In this review, “GM physicians” refers to board-certified generalist physicians, who were trained to provide care in outpatient and inpatient settings [
3,
4,
5]. These include:
FM physicians who are primarily engaged in longitudinal, community-based outpatient care [
6].
HGM physicians who are based in hospital settings manage acute conditions, multimorbidity, and care transitions [
7].
3. Global Perspectives on Dementia Care in Primary Care
Dementia care systems vary widely worldwide, which reflects differences in healthcare infrastructure, population needs, and policy priorities. To contextualize Japan’s GM model, the US, the UK, and Canada, three countries with established primary care infrastructures, national dementia strategies, and influence on global community-based dementia care, are compared. These countries have different healthcare financing systems: the UK’s National Health Service and Canada’s Medicare are publicly funded, single-payer systems that primarily provide free care at the point of use [
19,
20], whereas the US operates a predominantly private, multi-payer system that is supplemented by public programs, including Medicare and Medicaid [
21].
3.1. US
In the US, dementia care is managed within the primary care system, in which PCPs are the first point of contact for most patients and their families [
22,
23]. A national survey conducted by the Alzheimer’s Association indicated that approximately 82% of PCPs perceive themselves as frontline providers for dementia, which highlights their central role in diagnosis and ongoing management [
24,
25]. In clinical practice, initial assessments are frequently integrated within routine primary care visits, during which brief cognitive screening tools may be utilized. Patients with suspected cognitive impairment may be referred to neurologists, geriatric psychiatrists, or memory clinics for further evaluation [
22,
25].
Hospital-based dementia care in the US is usually provided by hospitalists [
26]. This division of labor, in which PCPs manage outpatient care and hospitalists oversee inpatient care, has created a structural separation between the two sectors. This may hinder the flow of information and contribute to fragmented management over the course of the disease [
26].
Although national guidelines emphasize the importance of early and accurate diagnosis, there are several limitations to effective implementation. PCPs often report insufficient dementia-specific training, limited consultation times, and restricted access to specialists, which reduces their ability to diagnose dementia [
22,
25]. In fact, only 39% of PCPs report feeling “very comfortable” making a diagnosis [
24]. In addition, the prevailing reimbursement structures rarely incentivize comprehensive cognitive assessments, which further discourages dementia detection [
22,
25].
Service availability is also inconsistent based on geography. While urban centers with large academic hospitals have multidisciplinary memory clinics that offer specialized diagnostic and management services [
27], rural communities often lack such resources. This contributes to inequities in diagnosis and caregiver support [
27]. Federal initiatives, such as the National Plan to Address Alzheimer’s Disease, aim to enhance coordination and expand training opportunities for PCPs; however, implementation has been inconsistent across regions, leaving significant gaps in practice [
28].
3.2. UK
In the UK, dementia care is provided through the National Health Service, which has established structured diagnostic pathways that begin with GPs [
29]. GPs typically conduct a preliminary screening. If dementia is suspected, patients are referred to specialized memory clinics for formal diagnostic evaluation [
30,
31]. These clinics included multidisciplinary teams, including neurologists, geriatricians, and mental health professionals, which ensures a more comprehensive approach to diagnosis and care planning.
To improve primary care engagement, the UK has implemented national frameworks, such as the Quality and Outcomes Framework, which provide financial incentives for practices to maintain accurate dementia registries and conduct regular patient reviews [
32,
33]. These measures have led to increases in dementia prevalence, improved follow-up, and a modest reduction in length of hospital stay. In addition, the Quality and Outcomes Framework has indirectly encouraged GP practices to adopt standardized documentation and regular communication with memory clinics, which has gradually improved the transparency of care pathways.
Significant challenges remain. Although early diagnosis rates have improved, coordination between the GPs and hospitals remains a limitation, with delays often occurring from incomplete integration of diagnostic records across care settings [
34]. Community-based care is supported by dementia-friendly initiatives that involve social workers, occupational therapists, and community nurses [
35]. These programs, combined with local campaigns to improve awareness and reduce stigma [
36], are important steps toward building a supportive environment. They also highlight the use of mobilizing nonmedical resources, such as volunteer networks and local charities, to support formal healthcare efforts.
Despite these efforts, ensuring care continuity, particularly during hospital admissions and discharges, remains problematic. Transitional care often depends on region-specific resources, resulting in a considerable variation in patient experiences. Addressing these gaps is considered a priority for the National Dementia Strategy [
37], reflecting ongoing concerns regarding the fragmentation of care pathways, despite system-wide reforms.
3.3. Canada
In Canada, the responsibility for dementia care rests primarily with FPs, who provide outpatient care for the majority of patients [
38]. This system has struggled historically, from a shortage of specialists and the absence of a unified national dementia strategy. These issues have hindered timely diagnoses and effective care coordination [
39]. The adoption of a national dementia strategy in 2019 was a turning point that standardized approaches across provinces and strengthened system capacity [
40].
Surveys suggest that while over 86% of FPs provide care for individuals with dementia, only 41% consider themselves adequately prepared to do so, reflecting persistent training gaps and a need for additional educational opportunities [
41]. To address this, several models have emerged, including Primary Care Memory Clinics, which focus on interdisciplinary assessment, collaborative management, and the integration of support services [
38,
41]. Diagnosis typically begins in the primary care setting, with referrals to memory clinics or specialists, such as neurologists or geriatricians, if necessary [
42].
Hospital care is usually provided by hospitalists or geriatric teams [
43]; however, as in many health systems, coordination between primary and hospital-based services is inconsistent, particularly in rural and remote regions, where access to specialists is limited [
39,
43,
44]. Innovative programs, such as rural memory clinics, have been established to mitigate geographic disparities and ensure equitable access to services [
44].
The national strategy, known as A Dementia Strategy for Canada: Together We Aspire, strives for timely diagnosis, caregiver support, and stigma reduction as key priorities [
40]. High-quality dementia care has been increasingly linked to interdisciplinary teamwork, integration with community-based services, and strong physician leadership [
45,
46]. Despite these improvements, achieving seamless transitions across community, hospital, and long-term care settings remains a challenge, and highlights the need for further system-level reforms [
39,
44].
Table 1 compares the dementia care systems in Japan, the US, the UK, and Canada across domains, such as primary care providers, diagnostic pathways, care continuity, community integration, and unique features. Although Japan is included for reference, its unique elements, particularly the emerging role of GM physicians in bridging outpatient and inpatient care, are further explored in
Section 4.
Overall, dementia care in the US, the UK, and Canada exhibits diverse approaches shaped by primary care structures, diagnostic pathways, and community integration. Japan’s CBICS (
Table 1), provides a formal framework to coordinate between Kakaritsuke physicians and hospitals. While this structure allows seamless integration compared with other countries, its implementation shows regional variation and limited authority for primary care providers; thus, continuity has not been fully realized. The emerging role of board-certified GM physicians, who practice in outpatient and inpatient settings, offers the potential to strengthen these links and further enhance seamless, community-integrated care. These distinctive features of Japan’s system, and the impact of GM physicians, are summarized in detail in
Section 4.
4. The Japanese GM Model: Integrating Outpatient and Inpatient Roles in Dementia Care
4.1. Current Landscape of Dementia Diagnosis and Care in Japan
Japan’s healthcare system is based on universal health insurance and free access. It allows patients to seek care at any facility regardless of disease severity or referral status [
47,
48]. Although this system ensures equity, it also fosters specialist-oriented care pathways, which are reinforced by the lack of a gatekeeping system [
47]. Modest surcharges for direct hospital visits have had little effect, and cultural preference for specialist credentials as a marker of trust and quality further sustains this tendency [
48].
With respect to dementia, Kakaritsuke physicians provide longitudinal care in the community, but have variable training and expertise. Many began as organ-specific specialists and transitioned to community practice without formal education in primary care or dementia [
49,
50]. Two groups may be distinguished: certified generalists (GM, FM, HGM) [
3,
6,
7] and hybrid subspecialists-generalist physicians [
49,
50]. Although the former are capable of high-quality primary care, their numbers remain limited [
48]. As a result, >70% of general practitioners still refer suspected dementia cases to specialists [
51]. Despite national efforts to emphasize the role of primary care, integration remains limited because of the absence of gatekeeping and the lack of a certification system for Kakaritsuke physicians [
47].
A dementia diagnosis is primarily made by dementia specialists or organ-based experts, such as neurologists, geriatricians, psychiatrists, and neurosurgeons, often working in memory clinics or in Medical Centers for Dementia established nationwide in 2008 [
52,
53,
54]. Hospital-based dementia care is usually provided by specialists in acute hospitals, where patients with comorbidities, such as pneumonia, are often admitted directly, often through Kakaritsuke referrals [
12,
53,
55]. This structure promotes fragmentation between outpatient and inpatient care.
To address these limitations, Japan established the CBICS, which coordinates medical, long-term care, welfare, housing, and preventive services for dementia care patients [
12,
55]. Key personnel include Kakaritsuke physicians, dementia specialists, Dementia Support Physicians, Intensive Support Teams, Clinical Support Teams, municipal agencies, and trained community Dementia Supporters, along with acute care hospitals and long-term care providers. Nevertheless, engagement of Kakaritsuke physicians in dementia care remains inconsistent, as only approximately 30% have dementia-specific training [
9].
Overall, GM physicians are expected to have a central role. With expertise spanning outpatient and inpatient care and formal dementia training, GM physicians represent an evolved form of Kakaritsuke practice, bridging community and hospital settings to enhance early detection, continuity, and quality of dementia care [
3,
6,
7]. The next section describes their roles within this emerging framework.
4.2. Current and Anticipated Roles of GM Physicians
Once GM became a board-certified specialty in 2018 [
3], GM physicians, including those trained in FM and HGM [
3,
6,
7], gradually expanded their involvement in dementia care, particularly in regions lacking specialists.
In community settings, FM physicians serve as the primary contact for cognitive concerns [
56]. Many utilize standardized tools, such as the Mini-Mental State Examination, Hasegawa Dementia Scale-Revised, or Montreal Cognitive Assessment [
49,
53]. Although some refer all suspected cases for confirmation, others independently conduct differential diagnoses, rule out treatable causes, and conduct imaging before making a final diagnosis [
49]. They also play an important role in advance care planning and preparing families for the disease trajectory [
57]. Collaboration with the Initial-phase Intensive Support Team enables timely specialist access for patients without an established Kakaritsuke physician [
53].
In hospital settings, HGM physicians manage acute conditions that frequently occur in dementia patients, such as aspiration pneumonia or delirium. They lead inpatient diagnostic reasoning, acute management, and safe discharge planning, which include coordinating multidisciplinary teams to ensure a smooth transition to home or long-term care [
58,
59,
60,
61]. This includes addressing cognitive status, caregiver capacity, and available community resources.
Currently, FM and HGM physicians primarily operate within their respective domains, community-based and hospital-based care, which results in fragmented continuity for some patients. This is similar to the occasional disconnect between Kakaritsuke physicians and hospital care during acute illnesses. However, GM physicians, combining FM and HGM competencies, can follow patients across outpatient and inpatient settings, bridging these sectors and reducing care fragmentation. Although full integration remains limited, team-based collaboration within the GM model can approximate seamless care, laying the foundation for an expanded, continuous role [
8,
12,
55].
In the future, the dual capacities of GM physicians will enable them to contribute across the dementia care continuum by detecting early cognitive decline through long-standing patient relationships, managing acute comorbidities in the hospital, and ensuring smooth reintegration into community life. This integrated role not only supports patient-centered care, but also improves capacity for comprehensive dementia management, particularly in under-resourced regions in Japan.
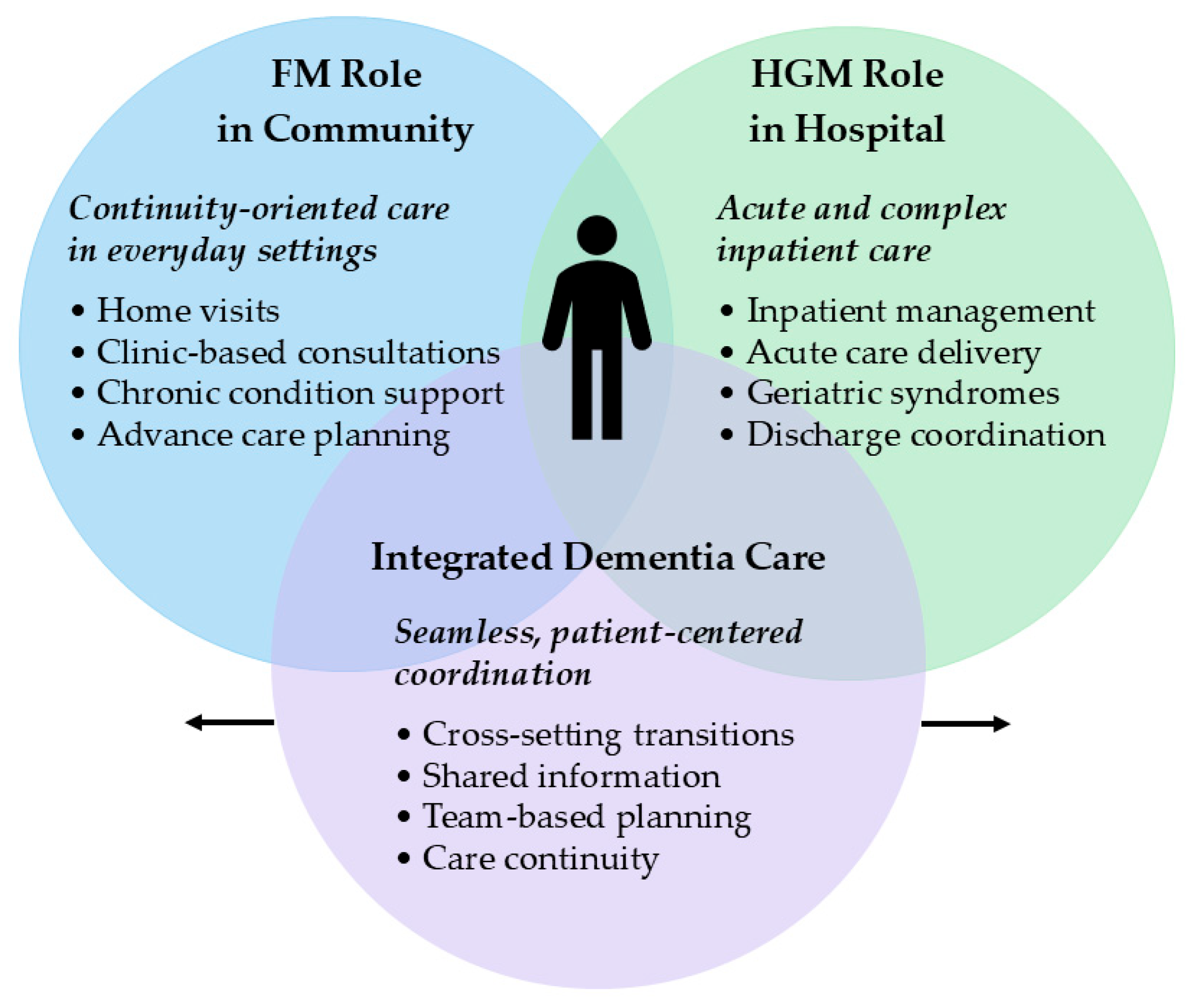
The complementary functions of FM physicians in community-based primary care and HGM physicians in hospital-based inpatient care, as well as their integration within the GM model, are presented in
Figure 1. This conceptual framework visually illustrates how these roles overlap to provide seamless dementia care. A comparative summary of these contributions across primary, hospital, and integrated care settings is listed in
Table 2.
4.3. Integrated Role of GM Physicians: Strengths and Challenges
Japan’s GM-based dementia care model, which integrates the complementary roles of FM physicians and HGM physicians, offers a unique framework for addressing the complex needs of individuals with dementia [
49,
62]. Traditionally, the continuity of care between Kakaritsuke physicians and hospitals has been fragmented, particularly during acute illnesses. GM physicians are uniquely positioned to bridge this gap by effectively combining community-based primary care and hospital-based inpatient management within a single, integrated role. Thus, GM physicians may be considered an evolved form of Kakaritsuke practice, formalizing and expanding core functions through structured training in FM and HGM. As central players within the CBICS, GM physicians facilitate seamless, person-centered care across outpatient and inpatient settings, ensuring continuity from early detection to end-of-life care [
12,
55].
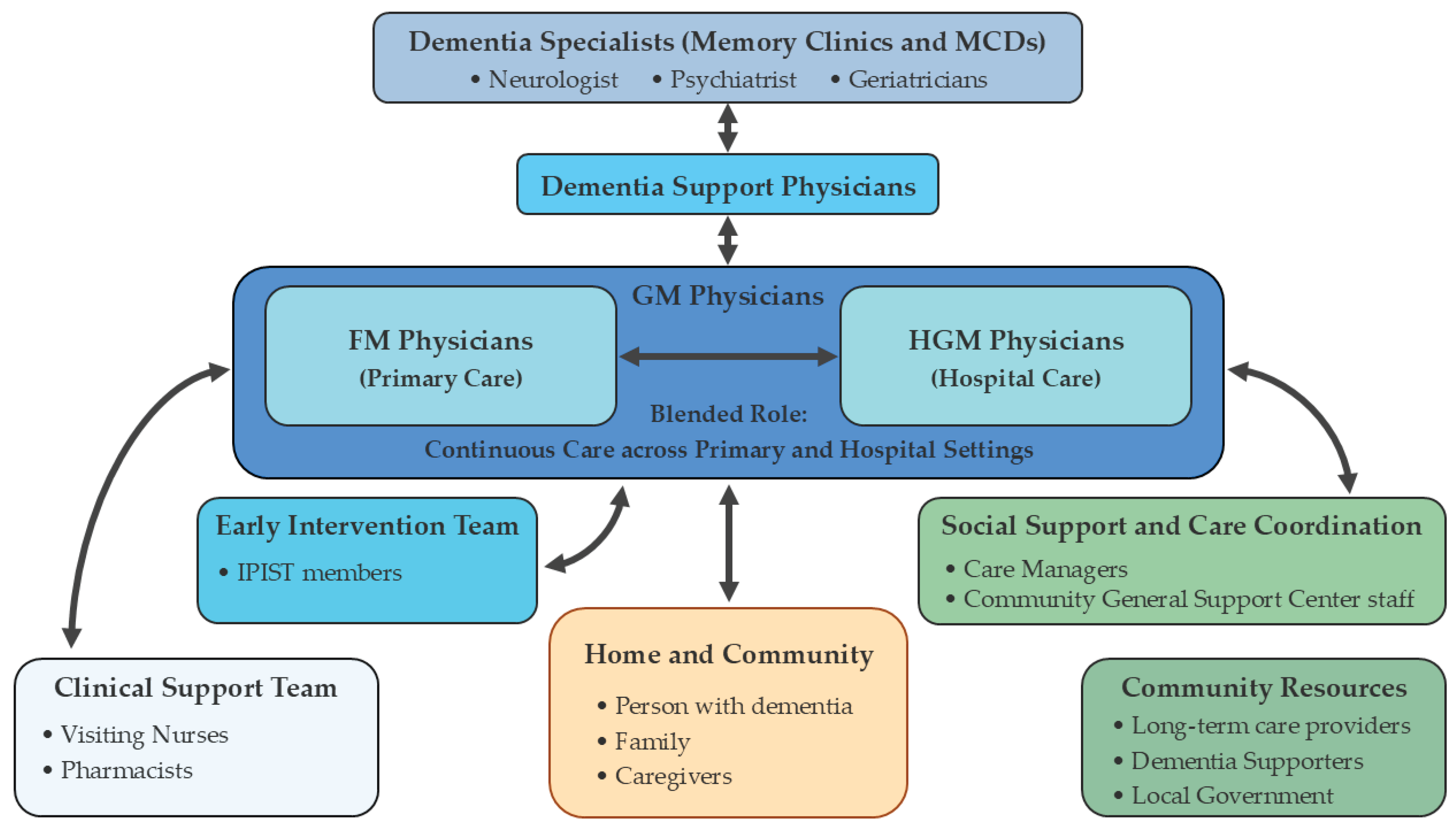
Their dual capacities facilitate collaboration with local actors, such as Initial-phase Intensive Support Teams and Community-based Comprehensive Support Centers, thereby integrating medical, social, and long-term care resources [
12,
55].
Figure 2 illustrates the conceptual framework of the roles of GM physicians across care settings and their interactions with key CBICS stakeholders. This fosters long-term therapeutic relationships, proactive disease management, timely response to complications, and consistent care planning [
3,
4,
5,
6,
7]. These features are valuable in dementia care, in which evolving cognitive, psychological, and social needs must be holistically addressed [
49,
52,
58,
62,
63].
Despite these strengths, several challenges remain for the GM-based model. Although GM physicians receive formal training in dementia care, which surpasses that of typical Kakaritsuke physicians, the depth and consistency of hands-on experience and advanced skill development vary, particularly in rural or resource-limited settings where they often serve as frontline providers [
8,
64]. Personnel numbers do not meet the increasing demand for dementia care, and integration into local care systems remains uneven [
65]. Some areas lack the structural support required for collaborative and cross-sectoral roles [
47].
Systemic constraints further limit adoption. These include unclear definitions in dementia diagnosis and care coordination, and broader ambiguity regarding the GM physician’s position within the healthcare system [
3,
4,
9,
66]. This uncertainty results from the relatively recent formalization of GM as a board-certified specialty [
3], and the lack of explicit integration into existing healthcare hierarchies. Other barriers include fragmented care protocols and reimbursement structures that disincentivize cross-sectoral collaboration.
Although Japan has enacted a national dementia strategy, which includes the 2019 National Framework for Promotion of Dementia Policies [
13,
67] and the 2023 Basic Act on Dementia to Promote an Inclusive Society [
13,
68], to promote inclusive and evidence-based care, the GM-based model has yet to be formally positioned within international frameworks, such as those advanced by the World Health Organization [
69] and the Organization for Economic Cooperation and Development [
70]. This lack of explicit alignment may limit the model’s direct transferability; however, it also emphasizes the importance of contextual adaptation and comparative validation. Addressing these challenges will require standardized dementia-specific curricula, strategic workforce planning, role clarification, aligned incentives, and enhanced interprofessional collaboration.
5. Limitations and Future Directions
This narrative review primarily compares Japan’s GM-based dementia care model with those of the US, UK, and Canada. Although these systems provide valuable points of contrast, the exclusion of other aging societies, particularly in Asia, limits the generalizability of our findings. Future studies should explore how other aging societies with similar demographic and cultural contexts, such as South Korea, Taiwan, and China, are addressing dementia care, and determine whether the Japanese model can be adapted to these contexts.
Although this review is conceptual, primarily descriptive, and model-based, it lacks empirical data on health outcomes, cost-effectiveness, and caregiver satisfaction. To validate and refine the GM-based model, future mixed-methods studies are needed to examine patient and caregiver experiences under GM-based care, comparative outcomes versus specialist-driven models, regional variations in implementation and access, and cost–benefit analyses in diverse healthcare settings. Generating this data will be important to inform policy decisions and clinical guidelines, ultimately advancing the role of GM physicians in dementia care.
6. Conclusions
As dementia will continue to be a public health challenge for the 21st century, sustainable and person-centered care models are needed. Japan’s GM physician model, which integrates FM and HGM roles within the CBICS, offers a distinctive and promising response.
By bridging the historical gap between Kakaritsuke physicians and hospitals, ensuring continuity across care settings, and promoting interdisciplinary collaboration aligned with patient life and community resources, GM physicians are positioned to facilitate integrated dementia care. Despite some limitations, such as the variability in training pathways, limited workforce capacity, and systemic fragmentation, the potential advantages of this model warrant greater investment, structured evaluation, and scholarly attention.
Japan’s experience offers insight for other aging societies attempting to restructure dementia care around the principles of continuity, coordination, and community integration. Moving forward, international dialogue, empirical validation, and targeted policy innovation, such as workforce development, reimbursement reform, and role standardization, are essential for realizing the full potential of this evolving model.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Dementia. Available online: https://www.who.int/en/news-room/fact-sheets/detail/dementia (accessed on 25 July 2025).
- Alzheimer’s Association. 2025 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2025, 21, e70235. [Google Scholar] [CrossRef]
- Japanese Board of General Medicine, Japanese Medical Specialty Board. Available online: https://jbgm.org/ (accessed on 25 July 2025).
- Tago, M.; Hirata, R.; Takahashi, H.; Yamashita, S.; Nogi, M.; Shikino, K.; Sasaki, Y.; Watari, T.; Shimizu, T. How Do We Establish the Utility and Evidence of General Medicine in Japan? Int. J. Gen. Med. 2024, 17, 635–638. [Google Scholar] [CrossRef]
- Tago, M.; Watari, T.; Shikino, K.; Sasaki, Y.; Takahashi, H.; Shimizu, T. Five Tips for Becoming an Ideal General Hospitalist. Int. J. Gen. Med. 2021, 14, 10417–10421. [Google Scholar] [CrossRef]
- Japan Primary Care Association. Available online: https://www.primarycare-japan.com/ (accessed on 25 July 2025).
- Japanese Society of Hospital General Medicine. Available online: https://hgm-japan.com/ (accessed on 25 July 2025).
- Suzuki, T.; Katayama, K.; Houchens, N.; Hartley, S.; Tokuda, Y.; Watari, T. The Future of Hospital Medicine in Japan: Lessons From the United States Hospital Medicine System. Int. J. Gen. Med. 2025, 18, 2379–2390. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Dementia. Available online: https://www.mhlw.go.jp/content/12404000/001172378.pdf (accessed on 25 July 2025).
- Wimo, A.; Prince, M. World Alzheimer Report 2010: The Global Economic Impact of Dementia; London: Alzheimer’s Disease International, 2010. [Google Scholar]
- Prince, M.; Prina, M.; Guerchet, M. World Alzheimer Report 2013: Journey of Caring: An analysis of long-term care for dementia; London: Alzheimer’s Disease International. 2013.
- Ministry of Health, Labour and Welfare. The Community-based Integrated Care System. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/chiiki-houkatsu/ (accessed on 25 July 2025).
- Ministry of Health, Labour and Welfare. Measures for Dementia. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/ninchi/index.html (accessed on 25 July 2025).
- American Academy of Family Physicians. Primary care. Available online: https://www.aafp.org/about/policies/all/primary-care.html (accessed on 25 July 2025).
- Greenfield, G.; Foley, K.; Majeed, A. Rethinking primary care’s gatekeeper role. BMJ 2016, 354, i4803. [Google Scholar] [CrossRef]
- Shahaed, H.; Glazier, R.H.; Anderson, M.; Barbazza, E. : Bos, V.L.L.C.; Saunes, I.S.; Auvinen, J.; Daneshvarfard, M.; Kiran, T. Primary care for all: lessons for Canada from peer countries with high primary care attachment. CMAJ 2023, 195, E1628–E1636. [Google Scholar] [CrossRef] [PubMed]
- Japan Medical Association. Primary Care. 2023 CMAAO General Assembly, Dhaka, 2023.
- Sugiyama, K.; Oshio, T.; Kuwahara, S.; Kimura, H. Association between having a primary care physician and health behavioral intention in Japan: results from a nationwide survey. BMC Prim. Care 2023, 24, 280. [Google Scholar] [CrossRef]
- Cylus, J.; Richardson, E.; Findley, L.; Longley, M.; O’Neill, C.; Steel, D. United Kingdom: Health System Review. Health Syst. Transit. 2015, 17, 1–126. [Google Scholar]
- Marchildon, G.P.; Allin, S.; Merkur, S. Canada: Health System Review. Health Syst. Transit. 2020, 22, 1–194. [Google Scholar]
- Rice, T.; Rosenau, P.; Unruh, L.Y.; Barnes, A.J. United States: Health System Review. Health Syst. Transit. 2020, 22, 1–441. [Google Scholar] [PubMed]
- de Levante Raphael, D. The Knowledge and Attitudes of Primary Care and the Barriers to Early Detection and Diagnosis of Alzheimer’s Disease. Medicina (Kaunas) 2022, 58, 906. [Google Scholar] [CrossRef]
- Sideman, A.B.; Hernandez de Jesus, A.; Brooks-Smith-Lowe, S.; Razon, N.; Filippi, M.K.; Wood, J.; Borson, S. Family physicians’ perspectives on outcomes, processes, and policies in dementia care. Health Aff. Sch. 2025, 3, qxae167. [Google Scholar]
- Alzheimer’s Association. 2020 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2020, 16, 391–460. [Google Scholar] [CrossRef]
- Sideman, A.B.; Ma, M.; Hernandez de Jesus, A.; Alagappan, C.; Razon, N.; Dohan, D.; Chodos, A.; Al-Rousan, T.; Alving, L.I.; Segal-Gidan, F.; Rosen, H.; Rankin, K.P.; Possin, K.L.; Borson, S. Primary Care Practitioner Perspectives on the Role of Primary Care in Dementia Diagnosis and Care. JAMA Netw. Open. 2023, 6, e2336030. [Google Scholar] [CrossRef] [PubMed]
- Nothelle, S.; Kelley, A.S.; Zhang, T.; Roth, D.L.; Wolff, J.L.; Boyd, C. Fragmentation of care in the last year of life: Does dementia status matter? J. Am. Geriatr. Soc. 2022, 70, 2320–2329. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.L.; Baker, L.; Chen, A.Y.; Wang, J.J. Geographic variation in shortfalls of dementia specialists in the United States. Health Aff. Sch. 2024, 2, qxae088. [Google Scholar] [CrossRef] [PubMed]
- National Plan to Address Alzheimer’s Disease. Available online: https://aspe.hhs.gov/collaborations-committees-advisory-groups/napa/napa-documents/napa-national-plan?utm_source=chatgpt.com (accessed on 25 July 2025).
- National Health Service. How to get a dementia diagnosis. Available online: https://www.nhs.uk/conditions/dementia/symptoms-and-diagnosis/diagnosis/ (accessed on 25 July 2025).
- Wells, C.E.; Smith, S.J. Diagnostic Care Pathways in Dementia. J. Prim. Care Community Health 2017, 8, 103–111. [Google Scholar] [CrossRef]
- Hayhoe, B.; Majeed, A.; Perneczky, R. General practitioner referrals to memory clinics: are referral criteria delaying the diagnosis of dementia? J. R. Soc. Med. 2016, 109, 410–415. [Google Scholar] [CrossRef]
- Russell, P.; Banerjee, S.; Watt, J.; Adleman, R.; Agoe, B.; Burnie, N.; Carefull, A.; Chandan, K.; Constable, D.; Daniels, M.; Davies, D.; Deshmukh, S.; Huddart, M.; Jabin, A.; Jarrett, P.; King, J.; Koch, T.; Kumar, S.; Lees, S.; Mir, S.; Naidoo, D.; Nyame, S.; Sasae, R.; Sharma, T.; Thormod, C.; Vedavanam, K.; Wilton, A.; Flaherty, B. Improving the identification of people with dementia in primary care: evaluation of the impact of primary care dementia coding guidance on identified prevalence. BMJ Open 2013, 3, e004023. [Google Scholar] [CrossRef]
- University of York. GP health checks offer modest but important benefits for dementia patients. Available online: https://www.york.ac.uk/research/themes/dementia-gp-health-check-benefit/?utm_source=chatgpt.com (accessed on 25 July 2025).
- Burn, A.M.; Fleming, J.; Brayne, C.; Fox, C.; Bunn, F. Dementia case-finding in hospitals: a qualitative study exploring the views of healthcare professionals in English primary care and secondary care. BMJ Open 2018, 8, e020521. [Google Scholar] [CrossRef]
- Moniz-Cook, E.; Mountain, G. The memory clinic and psychosocial intervention: Translating past promise into current practices. Front. Rehabil. Sci. 2023, 4, 1052244. [Google Scholar] [CrossRef]
- Wheatley, A.; Bamford, C.; Brunskill, G.; Booi, L.; Dening, K.H.; Robinson, L. Implementing post-diagnostic support for people living with dementia in England: a qualitative study of barriers and strategies used to address these in practice. Age Ageing 2021, 50, 2230–2237. [Google Scholar] [CrossRef]
- Department of Health. Living well with dementia: A National Dementia Strategy. London, 2009.
- Moore, A.; Frank, C.; Chambers, L.W. Role of the family physician in dementia care. Can. Fam. Physician 2018, 64, 717–719. [Google Scholar] [PubMed]
- Ismail, Z.; Black, S.E.; Camicioli, R.; Chertkow, H.; Herrmann, N.; Laforce, R., Jr.; Montero-Odasso, M.; Rockwood, K.; Rosa-Neto, P.; Seitz, D.; Sivananthan, S.; Smith, E.E.; Soucy, J.P.; Vedel, I.; Gauthier, S. CCCDTD5 participants. Recommendations of the 5th Canadian Consensus Conference on the diagnosis and treatment of dementia. Alzheimer’s Dement. 2020, 16, 1182–1195. [Google Scholar] [CrossRef]
- Public Health Agency of Canada. A Dementia Strategy for Canada: Together We Aspire. Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-strategy.html (accessed on 25 July 2025).
- The Canadian Institute for Health Information. Family doctor preparedness. Available online: https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/family-doctor-preparedness?utm_source=chatgpt.com (accessed on 25 July 2025).
- Lee, L.; Hillier, L.M.; Locklin, J.; Lumley-Leger, K.; Molnar, F. Specialist and family physician collaboration: Insights from primary care-based memory clinics. Heal. Soc. Care Community 2019, 27, e522–e533. [Google Scholar] [CrossRef] [PubMed]
- The Canadian Institute for Health Information. Dementia in hospitals. Available online: https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-hospitals?utm_source=chatgpt.com (accessed on 25 July 2025).
- Morgan, D.G.; Crossley, M.; Kirk, A.; D’Arcy, C.; Stewart, N.; Biem, J.; Forbes, D.; Harder, S.; Basran, J.; Dal Bello-Haas, V.; McBain, L. Improving access to dementia care: development and evaluation of a rural and remote memory clinic. Aging Ment. Health 2009, 13, 17–30. [Google Scholar] [CrossRef]
- Henein, M.; Arsenault-Lapierre, G.; Sourial, N.; Godard-Sebillotte, C.; Bergman, H.; Vedel, I.; Research on Organization of Healthcare Services for Alzheimer’s (ROSA) Team. Description of organizational and clinician characteristics of primary dementia care in Canada: a multi-method study. BMC Prim. Care 2022, 23, 121. [Google Scholar] [CrossRef]
- Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Available online: https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf (accessed on 25 July 2025).
- Kato, D.; Ryu, H.; Matsumoto, T.; Abe, K.; Kaneko, M.; Ko, M.; Irving, G.; Ramsay, R.; Kondo, M. Building primary care in Japan: Literature review. J. Gen. Fam. Med. 2019, 20, 170–179. [Google Scholar] [CrossRef]
- Sato, R.; Jakobsson, U.; Midlöv, P. A proposed medical system change in Japan inspired by Swedish primary health care: Important role of general practitioners and specialist nurses at primary health care centers. J. Gen. Fam. Med. 2024, 25, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Tsunawaki, S.; Dejonckheere, M.; Cigolle, C.T.; Phillips, K.; Rubinstein, E.B.; Matsuda, M.; Fetters, M.D.; Inoue, M. Practices and perspectives of primary care physicians in Japan and the United States about diagnosing dementia: a qualitative study. BMC Geriatr. 2021, 21, 540. [Google Scholar] [CrossRef]
- Saigal, P.; Takemura, Y.; Nishiue, T.; Fetters, M.D. Factors considered by medical students when formulating their specialty preferences in Japan: findings from a qualitative study. BMC Med. Educ. 2007, 7, 31. [Google Scholar] [CrossRef]
- Umegaki, H.; Suzuki, Y.; Kuzuya, M.; Iguchi, A. Attitudes of Japanese general practitioners towards referrals of demented patients. Nippon Ronen Igakkai Zasshi 2007, 44, 102–106. [Google Scholar] [CrossRef]
- Awata, S. Current activities of medical centers for dementia in Japan. Geriatr. Gerontol. Int. 2014, 14, 23–27. [Google Scholar] [CrossRef] [PubMed]
-
Dementia Clinical Practice Guideline Development Committee, Clinical Practice Guideline for Dementia 2017; Igaku-Shoin: Tokyo, Japan, 2017.
- National Center for Geriatrics and Gerontology. Available online: https://www.ncgg.go.jp/english/hospital/memorycenter/ (accessed on 25 July 2025).
- Mizutani, A.; Shindo, A.; Tabei, K.I.; Yoshimaru, K.; Satoh, M.; Tomimoto, H. Identifying and Characterizing People with Dementia Not Accessing the Japanese Community-Based Integrated Care System Using Health Insurance Claims Data. Intern. Med. 2023, 62, 345–353. [Google Scholar] [CrossRef]
- Noda, H.; Yamagishi, K.; Ikeda, A.; Asada, T.; Iso, H. Identification of dementia using standard clinical assessments by primary care physicians in Japan. Geriatr. Gerontol. Int. 2018, 18, 738–744. [Google Scholar] [CrossRef]
- McMahan, R.D.; Hickman, S.E.; Sudore, R.L. What Clinicians and Researchers Should Know About the Evolving Field of Advance Care Planning: a Narrative Review. J. Gen. Intern. Med. 2024, 39, 652–660. [Google Scholar] [CrossRef]
- Miyagami, T.; Shimizu, T.; Kosugi, S.; Kanzawa, Y.; Nagasaki, K.; Nagano, H.; Yamada, T.; Fujibayashi, K.; Deshpande, G.A.; Flora Kisuule, Tazuma, S. ; Naito, T. Roles considered important for hospitalist and non-hospitalist generalist practice in Japan: a survey study. BMC Prim. Care 2023, 24, 139. [Google Scholar] [CrossRef] [PubMed]
- Kurihara, M.; Kamata, K.; Tokuda, Y. Impact of the hospitalist system on inpatient mortality and length of hospital stay in a teaching hospital in Japan: a retrospective observational study. BMJ Open 2022, 12, e054246. [Google Scholar] [CrossRef]
- Hamada, O.; Tsutsumi, T.; Tsunemitsu, A.; Fukui, T.; Shimokawa, T. Imanaka, Y. Impact of the Hospitalist System in Japan on the Quality of Care and Healthcare Economics. Intern. Med. 2019, 58, 3385–3391. [Google Scholar] [CrossRef]
- Hamada, O.; Tsutsumi, T.; Imanaka, Y. Efficiency of the Japanese Hospitalist System for Patients with Urinary Tract Infection: A Propensity-matched Analysis. Intern. Med. 2023, 62, 1131–1138. [Google Scholar] [CrossRef] [PubMed]
- Tsunawaki, S.; Abe, M.; DeJonckheere, M.; Cigolle, C.T.; Philips, K.K.; Rubinstein, E.B.; Matsuda, M.; Fetters, M.D.; Inoue, M. Primary care physicians’ perspectives and challenges on managing multimorbidity for patients with dementia: a Japan-Michigan qualitative comparative study. BMC Prim. Care 2023, 24, 132. [Google Scholar] [CrossRef] [PubMed]
- Maki, Y. ; Yamaguchi, H. Early detection of dementia in the community under a community-based integrated care system. Geriatr. Gerontol. Int. 2014, 14, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Ryu, Y.; Sano, C. Family Medicine Education at a Rural Hospital in Japan: Impact on Institution and Trainees. Int. J. Environ. Res. Public Health 2021, 18, 6122. [Google Scholar] [CrossRef]
- Iwata, H.; Matsushima, M.; Watanabe, T.; Sugiyama, Y.; Yokobayashi, K.; Son, D.; Satoi, Y.; Yoshida, E.; Satake, S.; Hinata, Y.; Fujinuma, Y. The need for home care physicians in Japan - 2020 to 2060. BMC Health Serv. Res. 2020, 20, 752. [Google Scholar] [CrossRef]
- Miyagami, T.; Yamada, T.; Kanzawa, Y.; Kosugi, S.; Nagasaki, K.; Nagano, H.; Shimizu, T.; Fujibayashi, K.; Deshpande, G.A.; Naito, T. Large-Scale Observational Study on the Current Status and Challenges of General Medicine in Japan: Job Description and Required Skills. Int. J. Gen. Med. 2022, 15, 975–984. [Google Scholar] [CrossRef]
- Ishihara, M.; Matsunaga, S.; Islam, R.; Shibata, O.; Chung, U.I. A policy overview of Japan’s progress on dementia care in a super-aged society and future challenges. Glob. Health Med. 2024, 6, 13–18. [Google Scholar] [CrossRef] [PubMed]
- The Basic Act on Dementia to Promote an Inclusive Society. Available online: https://www.japaneselawtranslation.go.jp/outline/92/905R510.pdf (accessed on 25 July 2025).
- World Health Organization. Global action plan on the public health response to dementia 2017-2025; World Health Organization: Geneva, 2017. [Google Scholar]
- Anderson, G.; Oderkirk, J. Dementia Research and Care: Can Big Data Help?; OECD Publishing, Paris, 2015.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).