Submitted:
01 September 2025
Posted:
02 September 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Study Design and Data Selection
Statistical Analysis
3. Results
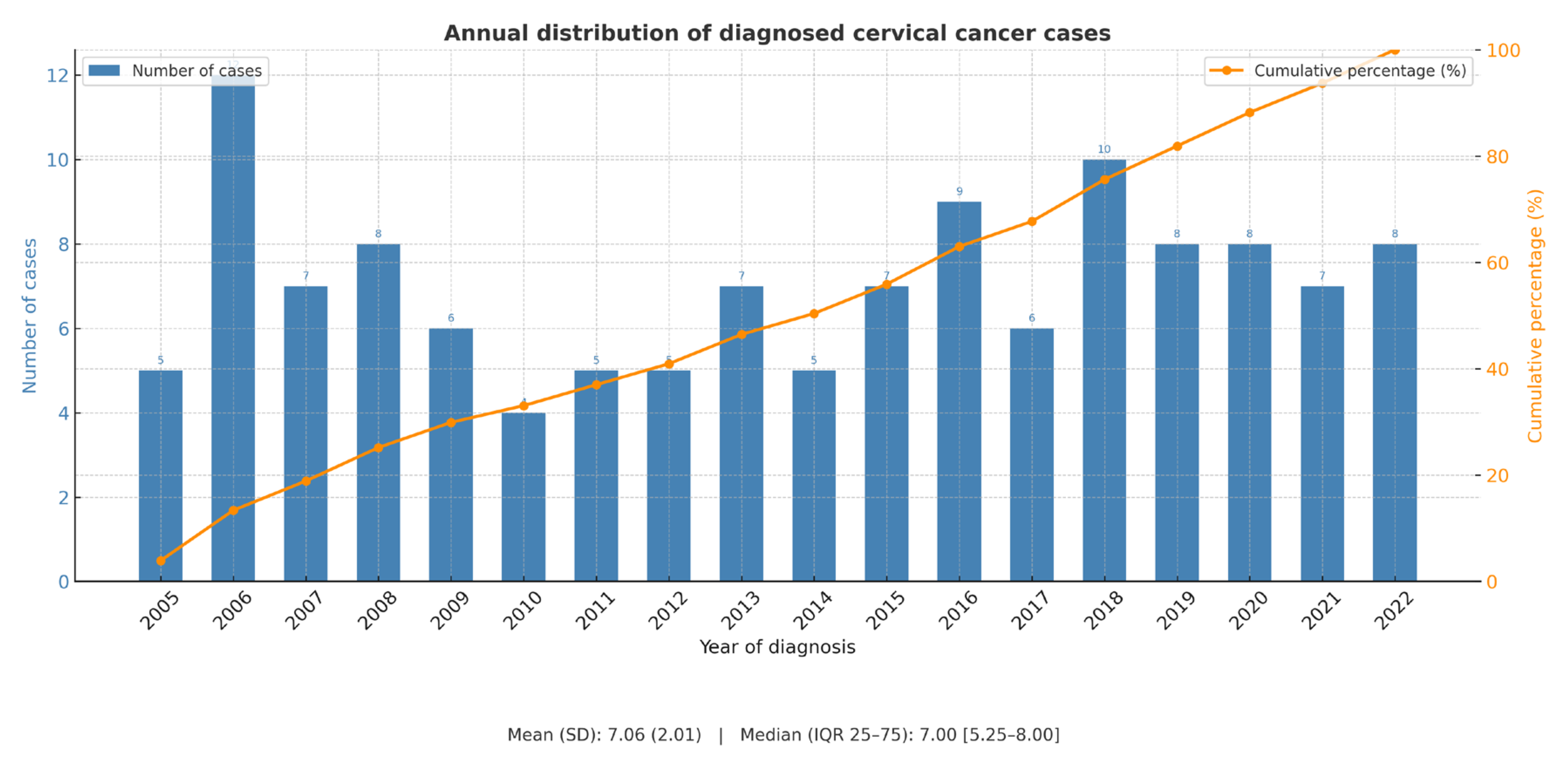
3.1. Evaluation of ESGO QIs at Our Center
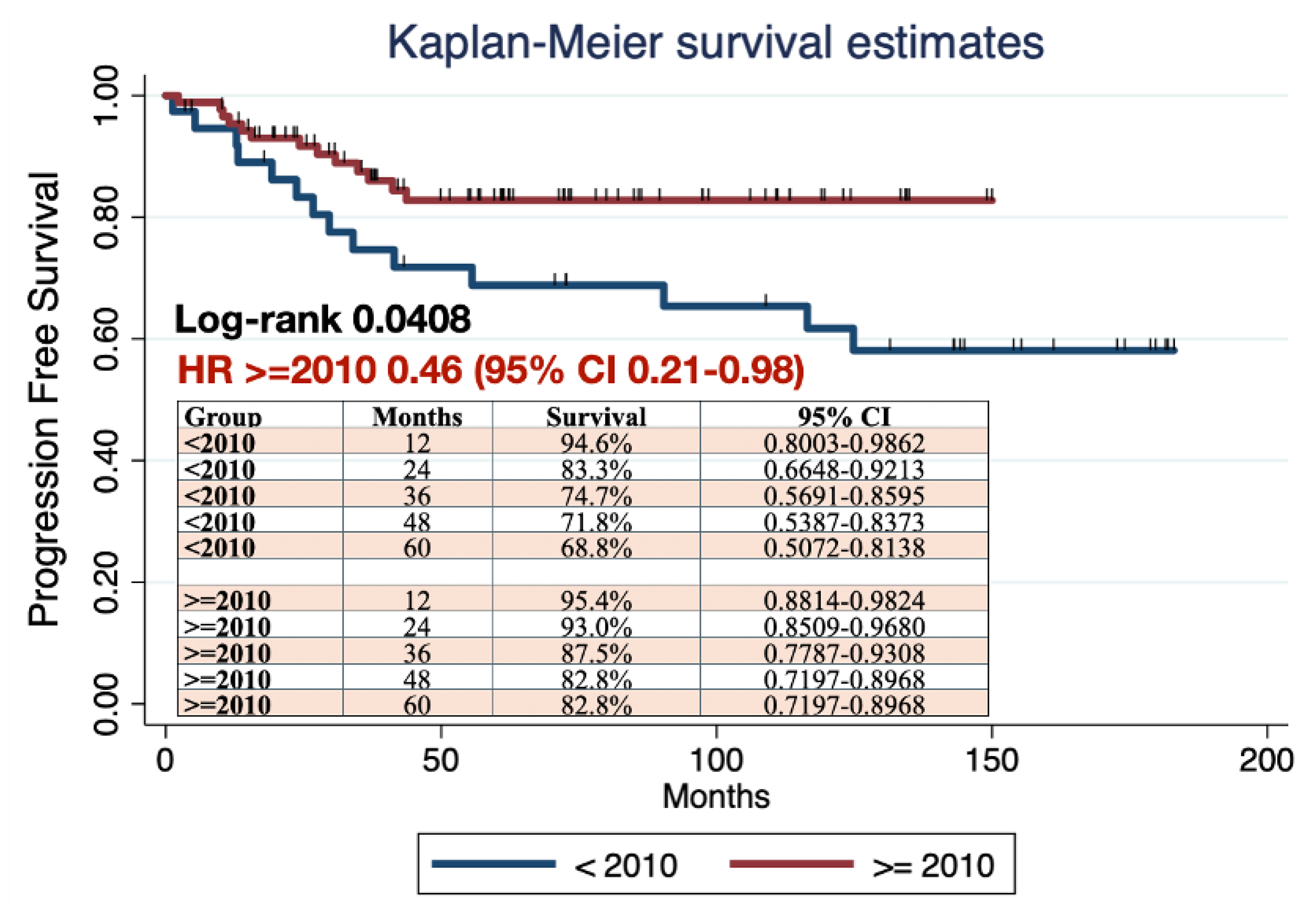
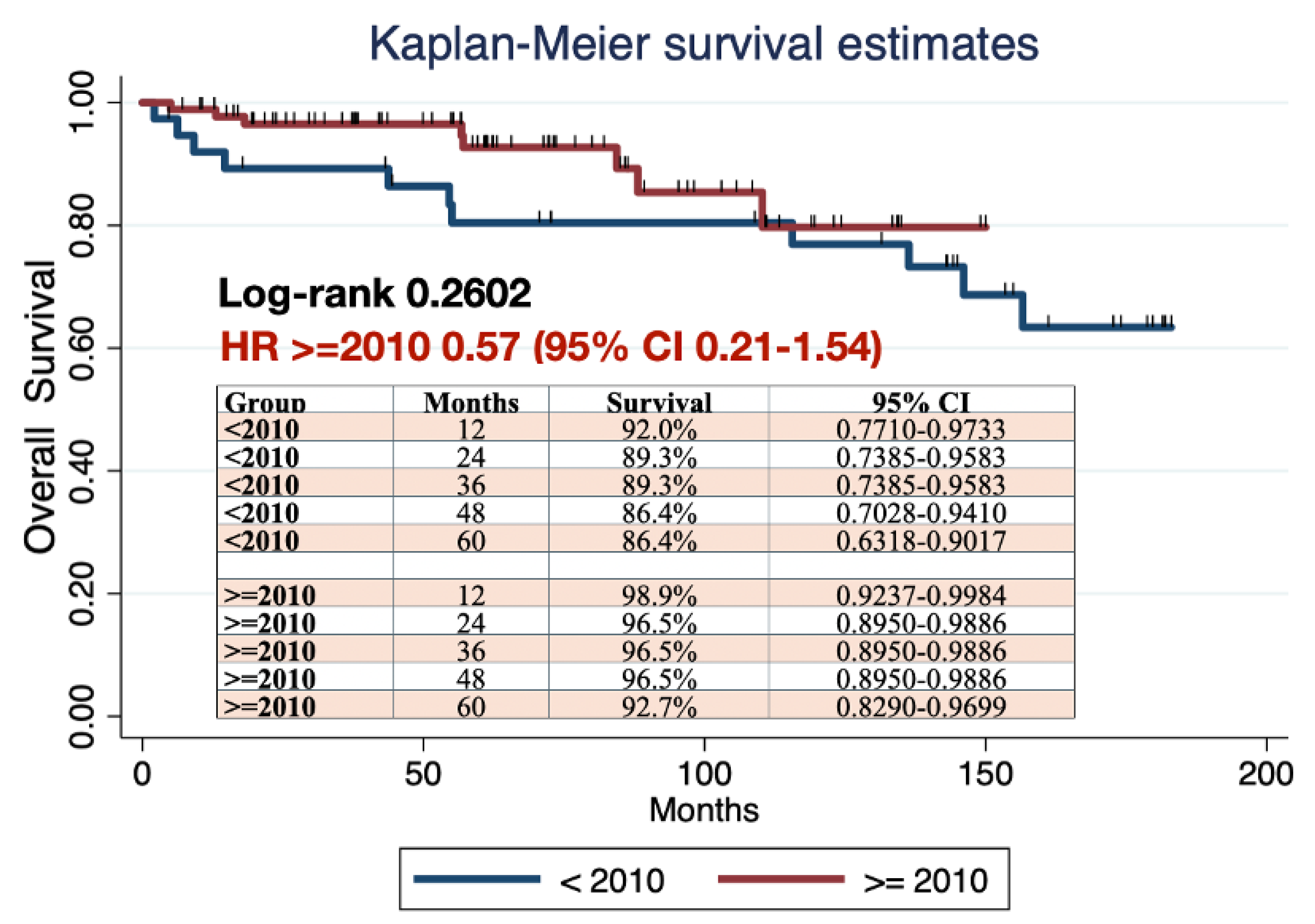
3.2. Comparative Analysis by Study Groups (Before 2010 vs. 2010 and Beyond)
3.3. Analysis of Factors Associated with Recurrence in Patients Who Underwent Radical Surgery for Early-Stage Cervical Cancer
4. Discussion
Results in the Context of Published Literature
Limitations and Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ESGO | European Society of Gynaecological Oncology |
| QI | Quality Indicators |
| PFS | Progression Free Survival |
| HPV | Human papillomavirus |
| PL | Pelvic lymphadenectomy |
| SLNB | Sentinel lymph node biopsy |
| MRI | Magnetic resonance imaging |
| SD | Standard deviation |
| IQR | Interquartile range |
| EBR | External beam radiation |
| BT | Vaginal brachytherapy |
| CRT | Chemoradiotherapy |
| MDT | Multidisciplinary team |
References
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229-263. [CrossRef]
- Sant M, Chirlaque Lopez MD, Agresti R, et al. Survival of women with cancers of breast and genital organs in Europe 1999-2007: Results of the EUROCARE-5 study. Eur J Cancer. 2015;51(15):2191-2205. [CrossRef]
- Cibula D, Planchamp F, Fischerova D, et al. European Society of Gynaecological Oncology quality indicators for surgical treatment of cervical cancer. Int J Gynecol Cancer. 2020;30(1):3-14. [CrossRef]
- Cibula D, Raspollini MR, Planchamp F, et al. ESGO/ESTRO/ESP Guidelines for the management of patients with cervical cancer - Update 2023. Int J Gynecol Cancer. 2023;33(5):649-666. Published 2023 May 1. [CrossRef]
- Fotopoulou C, Concin N, Planchamp F, et al. Quality indicators for advanced ovarian cancer surgery from the European Society of Gynaecological Oncology (ESGO): 2020 update. Int J Gynecol Cancer. 2020;30(4):436-440. [CrossRef]
- Jochum F, De Rozario T, Lecointre L, et al. Adherence to European ovarian cancer guidelines and impact on survival: a French multicenter study (FRANCOGYN). Int J Gynecol Cancer. 2021;31(11):1443-1452. [CrossRef]
- Boria F, Chiva L, Zanagnolo V, et al. Radical hysterectomy in early cervical cancer in Europe: characteristics, outcomes and evaluation of ESGO quality indicators. Int J Gynecol Cancer. 2021;31(9):1212-1219. [CrossRef]
- Ding Y, Zhang X, Qiu J, Zhang J, Hua K. Assessment of ESGO Quality Indicators in Cervical Cancer Surgery: A Real-World Study in a High-Volume Chinese Hospital. Front Oncol. 2022;12:802433. Published 2022 Jan 25. [CrossRef]
- Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri. Int J Gynaecol Obstet. 2018;143 Suppl 2:22-36. [CrossRef]
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med. 2018;379(20):1895-1904. [CrossRef]
- Peters WA, Liu PY, Barrett RJ, Stock RJ, Monk BJ, Berek JS, Souhami L, Grigsby P, Gordon W Jr, Alberts DS. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after.
- radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000 Apr;18(8):1606-13.
- Lee B, Kim K, Park Y, Lim MC, Bristow RE. Impact of hospital care volume on clinical outcomes of laparoscopic radical hysterectomy for cervical cancer: A systematic review and meta-analysis. Medicine (Baltimore). 2018;97(49):e13445. [CrossRef]
- Li LY, Wen LY, Park SH, et al. Impact of the Learning Curve on the Survival of Abdominal or Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. Cancer Res Treat. 2021;53(1):243-251. [CrossRef]
- Matsuo K, Shimada M, Yamaguchi S, et al. Association of Radical Hysterectomy Surgical Volume and Survival for Early-Stage Cervical Cancer. Obstet Gynecol. 2019;133(6):1086-1098. [CrossRef]
- Thomas V, Chandy RG, Sebastian A, et al. Treatment Outcomes of Early Carcinoma Cervix Before and After Sub-specialization. Indian J Surg Oncol. 2021;12(1):78-85. [CrossRef]
- Pedone Anchora L, Bizzarri N, Gallotta V, et al. Impact of surgeon learning curve in minimally invasive radical hysterectomy on early-stage cervical cancer patient survival. Facts Views Vis Obgyn. 2021;13(3):231-239. [CrossRef]
- Concin N, Planchamp F, Abu-Rustum NR, et al. European Society of Gynaecological Oncology quality indicators for the surgical treatment of endometrial carcinoma. Int J Gynecol Cancer. 2021;31(12):1508-1529. [CrossRef]
- Fernandez-Gonzalez S, Ponce J, Martínez-Maestre MÁ, Barahona M, Gómez-Hidalgo NR, Díaz-Feijoo B, Casajuana A, Gracia M, Frias-Gomez J, Benavente Y, et al. The Impact of Surgical Practice on Oncological Outcomes in Robot-Assisted Radical Hysterectomy for Early-Stage Cervical Cancer, Spanish National Registry. Cancers. 2022; 14(3):698. [CrossRef]
- Hardt JL, Merkow RP, Reissfelder C, Rahbari NN. Quality assurance and quality control in surgical oncology. J Surg Oncol. 2022;126(8):1560-1572. [CrossRef]
- Benoit L, Koual M, Nguyen-Xuan HT, et al. Does a pre-operative conization improve disease-free survival in early-stage cervical cancer?. Arch Gynecol Obstet. 2021;303(1):231-239. [CrossRef]
- Casarin J, Buda A, Bogani G, et al. Predictors of recurrence following laparoscopic radical hysterectomy for early-stage cervical cancer: A multi-institutional study. Gynecol Oncol. 2020;159(1):164-170. [CrossRef]
- Casarin J, Bogani G, Papadia A, et al. Preoperative Conization and Risk of Recurrence in Patients Undergoing Laparoscopic Radical Hysterectomy for Early Stage Cervical Cancer: A Multicenter Study. J Minim Invasive Gynecol. 2021;28(1):117-123. [CrossRef]
- Bizzarri N, Pedone Anchora L, Kucukmetin A, et al. Protective Role of Conization Before Radical Hysterectomy in Early-Stage Cervical Cancer: A Propensity-Score Matching Study. Ann Surg Oncol. 2021;28(7):3585-3594. [CrossRef]
- Chacon E, Manzour N, Zanagnolo V, et al. SUCCOR cone study: conization before radical hysterectomy. Int J Gynecol Cancer. 2022;32(2):117-124. [CrossRef]
- Manzour N, Chiva L, Chacón E, et al. SUCCOR Risk: Design and Validation of a Recurrence Prediction Index for Early-Stage Cervical Cancer. Ann Surg Oncol. 2022;29(8):4819-4829. [CrossRef]
| No | ESGO QI | Target required | Value in our cohort | Achieved |
|---|---|---|---|---|
| 1 | Number of radical procedures in cervical cancer performed per center per year | ≥15 | 7.1 (mean) | No |
| 2 | Surgery performed or supervised by a certified gynecologic oncologist or trained surgeon dedicated to gynecologic cancer | 100% | 100% | Yes |
| 3 | Center participating in ongoing clinical trials in gynecologic cancer | ≥1 | Not reported before 2010 100% since 2010 |
Yes (from 2010) |
| 4 | Treatment discussed at a multidisciplinary team meeting | 100% | 0% before 2010 100% since 2010 |
Yes (from 2010) |
| 5 | Required pre-operative investigation (pelvic MRI) | 100% | 79% overall 100% since 2010 |
No Yes (from 2010) |
| 6 | Minimum required elements in surgical reports | 100% | 57% | No |
| 7 | Minimum required elements in pathology and pathology reports | ≥90% | 0% (1 parameter never reported) | No |
| 8 | Structured prospective reporting of follow-up and 30-day post-operative morbidity | ≥90% | 0% | No |
| 9 | Urological fistula rate within 30 days after radical parametrectomy | ≤3% | 2.38% | Yes |
| 10 | Proportion of patients with clear vaginal and parametrial margins | ≥97% | 95.3% overall 98.9% after 2010 |
No overall Yes (from 2010) |
| 11 | Proportion of patients with stage T1b disease upstaged after surgery | <10% | 12.5% overall 4.4% since 2010 |
No overall Yes (from 2010) |
| 12 | Recurrence rate at 2 years in stage pT1b1N0 patients | <10% | 9.97% | Yes |
| 13 | Proportion of patients with stage T1 disease undergoing lymph node staging | ≥98% | 100% | Yes |
| 14 | Counseling about the possibility of fertility-sparing treatment (FST) | 100% | 100% | Yes |
| 15 | Proportion of patients receiving adjuvant chemoradiotherapy after pT1b1pN0 disease | <15% | 3.13% | Yes |
| N (N=128) |
Before 2010 (n=38) |
2010 or after (n=90) |
p-value | |
|---|---|---|---|---|
| Age (years) | 128 | 46.0 ± 9.8 | 48.1 ± 12.3 | 0.3684 |
| BMI (kg/m2) | 121 | 25.9 ± 7.2 | 26.5 ± 4.7 | 0.5751 |
| FIGO Stage (2018) | ||||
|
3 (2.3%) | 2 (5.3%) | 1 (1.1%) | 0.057 |
|
6 (4.7%) | 3 (7.9%) | 3 (3.3%) | |
|
46 (35.9%) | 9 (23.7%) | 37 (41.1%) | |
|
5 (3.9%) | 0 (0.0%) | 5 (5.6%) | |
|
68 (53.1%) | 24 (63.2%) | 44 (48.9%) | |
| Maximum size per image (mm) | 90 | 24 ± 17.7 | 14.4 ± 12.7 | 0.0495 |
| Previous Conization | ||||
|
66 (51.6%) | 24 (63.2%) | 38 (42.2%) |
0.035 |
|
62 (48.4%) | 14 (36.8%) | 52 (48%) | |
| Type of procedure | ||||
|
114 (89.1%) | 36 (4.7%) | 78 (86.7%) | 0.183 |
|
12 (9.4%) | 1 (2.6%) | 11 (12.2%) | |
|
2 (1.6%) | 1 (2.6%) | 1 (2.6%) | |
| Type of parametrial resection | ||||
|
2 (1.5%) | 2 (5.3%) | 0 (0%) | <0.001 |
|
43 (33.6%) | 1 (2.6%) | 42 (46.7%) | |
|
81 (63.3%) | 35 (92.1%) | 46 (51.1%) | |
|
2 (1.5%) | 0(0%) | 2 (2.2%) | |
| Surgical approach | ||||
|
21 (16.4%) | 8 (21.1%) | 13 (14.4%) | 0.603 |
|
106 (82.8%) | 30 (79.0%) | 76 (84.4%) | |
|
1 (0.8%) | 0 (0%) | 1 (1.1%) | |
| Intraoperative complications | ||||
|
11 (8.6%) | 6 (15.8%) | 5 (5.6%) | 0.047 |
| Early postoperative complications (<30 days) | ||||
|
42 (32.8%) | 11 (29.0%) | 31 (34.4%) | 0.575 |
| Histological Subtype | ||||
|
81 (63.3%) | 23 (60.5%) | 58 (64.4%) | 0.605 |
|
25 (19.5%) | 7 (18.4%) | 18 (20.1%) | |
|
22 (17.2%) | 8 (21.1%) | 14 (15.5%) | |
| Grade | ||||
|
32 (25.0%) | 11 (29.0%) | 21 (23.3%9 | 0.660 |
|
64 (50.0%) | 16 (42.1%) | 48 (53.3%) | |
|
30 (23.4%) | 10 (26.3%) | 20 (22.2%) | |
|
2 (1.6%) | 1 (2.6%) | 1 (1.1%) | |
| LVSI | ||||
|
35 (27.3%) | 17 (44.7%) | 18 (20.0%) | 0.005 |
|
91 (71.2%) | 20 (52.7%) | 71 (78.9%) | |
|
2 (1.5%) | 1 (2.6%) | 1 (1.1%) |
| PFS | |||
|---|---|---|---|
| HR | IC 95% | p value | |
| Age (years) | 0.97 | 0.92-1.03 | 0.300 |
| BMI (Kg/m2) | 0.96 | 0.84-1.09 | 0.525 |
| Maximum tumor diameter | 1.03 | 0.93-1.14 | 0.597 |
Tumoral Grade (Ref. 1)
|
0.40 1.52 |
0.06-2.52 0.27-8.72 |
0.328 0.635 |
FIGO 2018 histological stage (Ref. IA2)
|
- - 0.05 0.03 0.002 0.04 |
- - 0.001-2.63 <0.001-16.43 <0.001-0.38 <0.001-4.15 |
1.000 1.000 0.140 0.275 0.200 0.177 |
| LVSI | 3.38 | 0.92-12.38 | 0.066 |
Stromal invasion (Ref. superficial)
|
1.47 2.09 |
0.11-19.85 0.20-22.30 |
0.771 0.541 |
| Positive margins | 5.81 | 0.14-234.10 | 0.351 |
| Parametrial invasion | 9.00 | 0.23-358.98 | 0.243 |
| Previous conization | 0.12 | 0.02-0.73 | 0.021 |
| Positive lymph nodes | 0.48 | - | - |
| Diagnostic group (Ref. <2010) | 1.13 | 0.30-4.28 | 0.859 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





