Introduction
Hidradenitis suppurativa (HS), also known as acne inversa or “maladie de Verneuil” (described by Aristide Auguste Stanislas Verneuil, a French anatomist and surgeon from paris in 1854) is a debilitating, chronic inflammatory skin condition characterized by recurrent, painful nodules, abscesses, draining sinus tracts, and subsequent scarring [
1,
2,
3]. It’s a chronic inflammatory disease caused by obstruction of the ducts of apocrine glands. Its prevalence ranges between 0.05% to 4.1% with incidence estimated at around 6/100 000 person-year [
4]. This disease impairs patients quality of life due to persistent pain, purulent discharge, and associated social isolation. Obstruction may be attributed to genetic, hormonal, immunological, and mechanical factors, such as the use of antiperspirants or hair shaving. Additional contributing factors include constitutional elements like obesity, as well as excessive exposure to heat and smoking [
3]. Following the obstruction of the ducts from keratinous material, the glands dilate and rupture then secondary infection occurs leading to abscess and fistulas. Chronic inflammation leads to fibrosis. The anatomic regions most affected are those with rich apocrine glands like axilla, submammary, groin and anogenital regions. However, the clinical presentation of HS can be remarkably heterogenous, with unusual, documented occurrences that challenge conventional diagnostic paradigms. Previous case reports have described HS affecting anterior chest wall, jawline and neck for exemple [
6]. The diagnostic of HS is clinical but its varied presentations in atypical sites, frequently lead to misdiagnosis leading to further challenge. HS can be associated with other conditions, such as inflammatory bowel disease, acne tetrad, behçet disease, acne conglobate, severe acne, squamous cell carcinoma, pilonidal cyst [
7]. Health care providers tend to treat HS condition with a wide variety of methods including general and topical antibiotics, immunosuppressive treatment, surgery and adjuvant therapy like botulinum toxin, cryotherapy, depilation, oxygen therapy.
Case Presentation
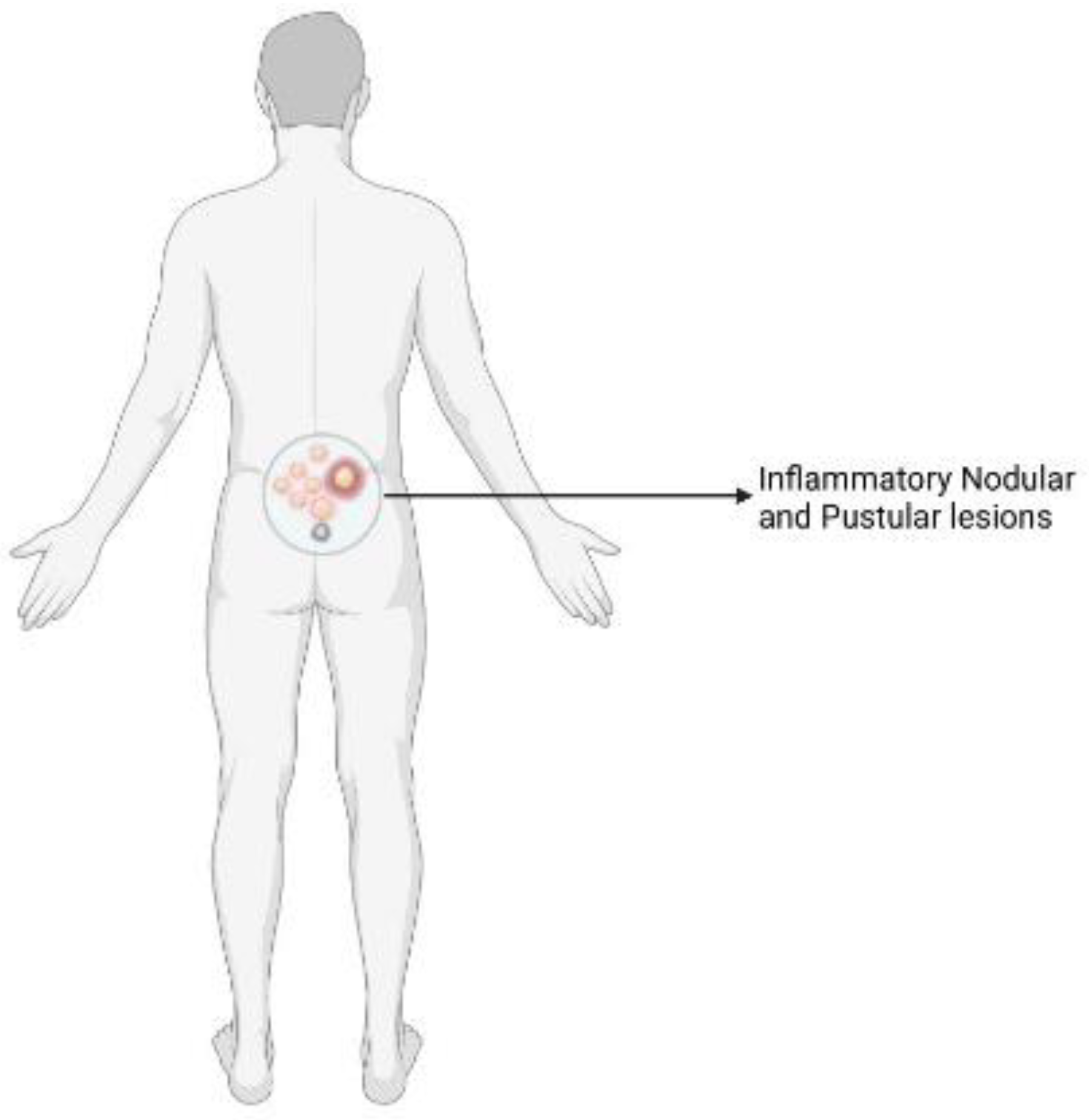
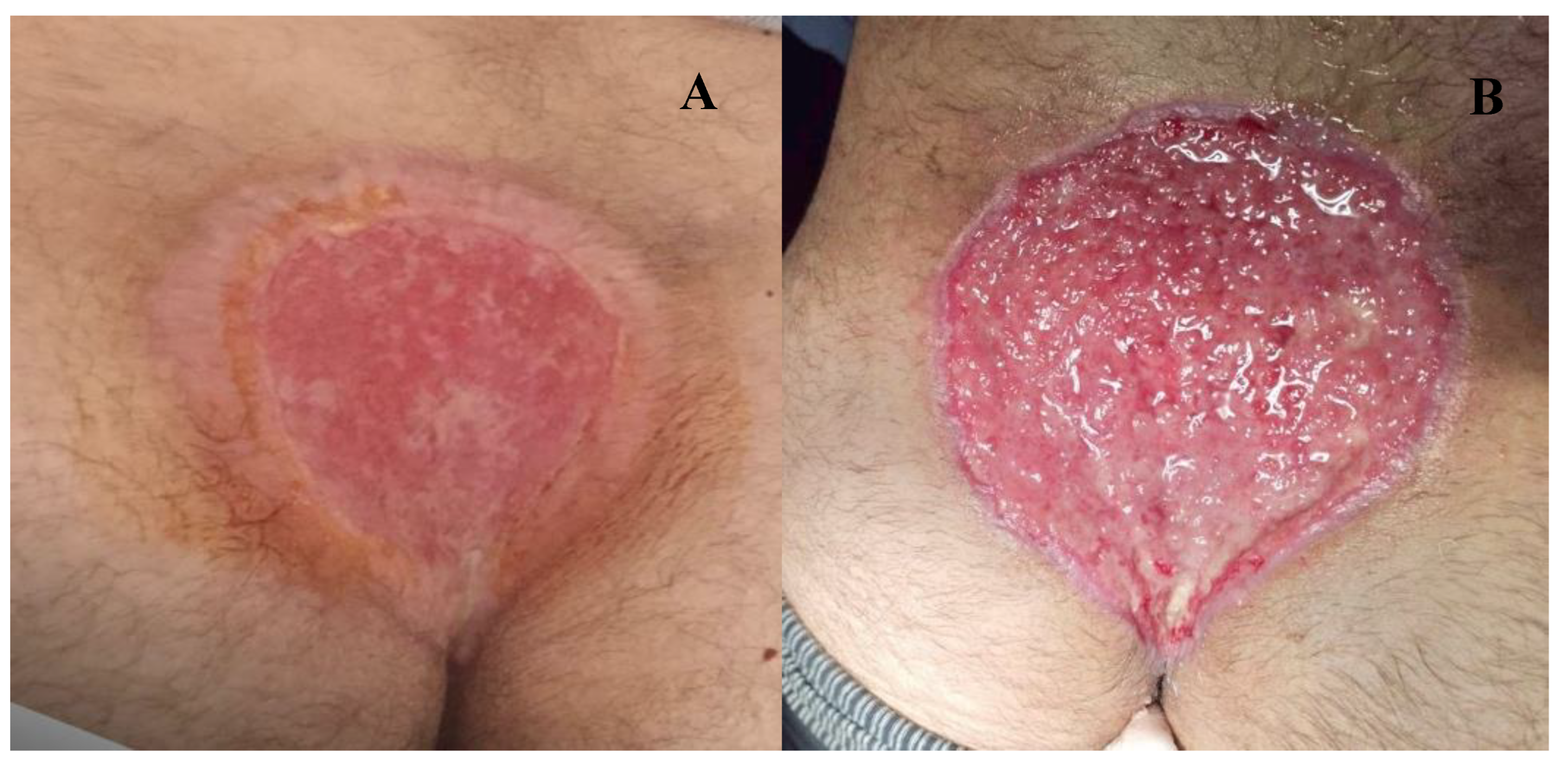
A 34 year old North-African military male, smoker with no past medical or surgery history. With normal BMI of 23. He presented to day-consultation clinic with a good general status, no fever, no jaundice. As the patient reports, the first symptoms appeared 01 year before, through the apparition of lumbar nodule with no other lesion in the arm pits, groin or perineum. The nodule were painful, expanding in volume and number turning to fistulous abscesses over time with purulent discharge causing social disconfort (
Figure 1 and
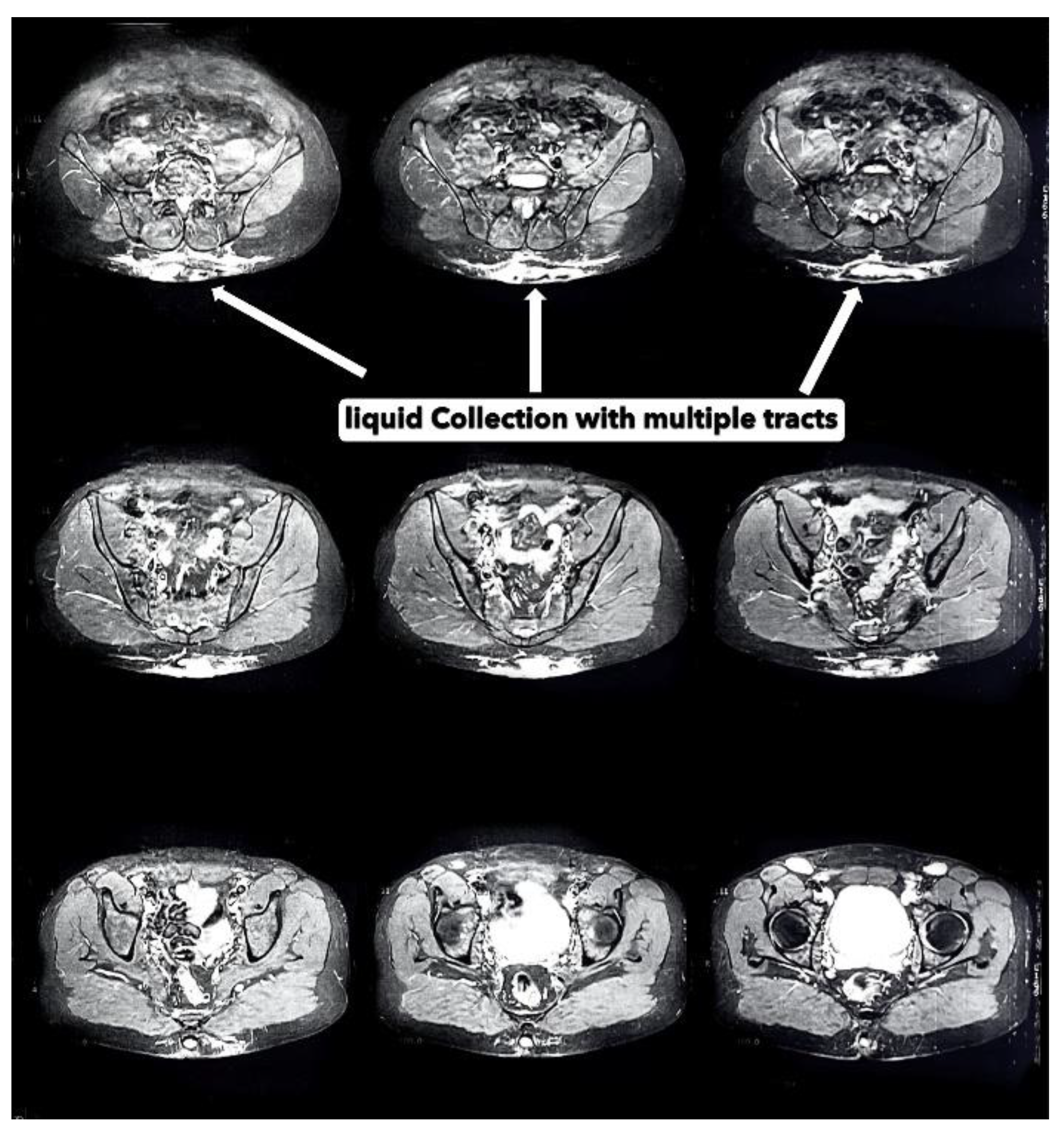
Figure 2). Prior to consultation with us, the patient took oral antibiobiotics and some topic antiseptics. The evolution of the lesions motivated a consultation. A clinical evaluation revealed skin ulcers, hyperpigmentation, hardened thick skin folds with orifices discharging pus in the lumbosacral region. Serologic testing for human immunodeficiency virus (HIV), syphilis, chronic infection with hepatitis viruses B and V, as well as chlamydia trachomatis were negative. A computer tomography (CT) imaging concluded with highlighting a polylobed collection associated with multiple fistulous tracts in the subcutaneous soft tissues of the sacrococcygeal region with liquid content showing significant hypersignal on T2 and with a thick wall enhanced after gadolinium injection measuring 20X95X130 mm (
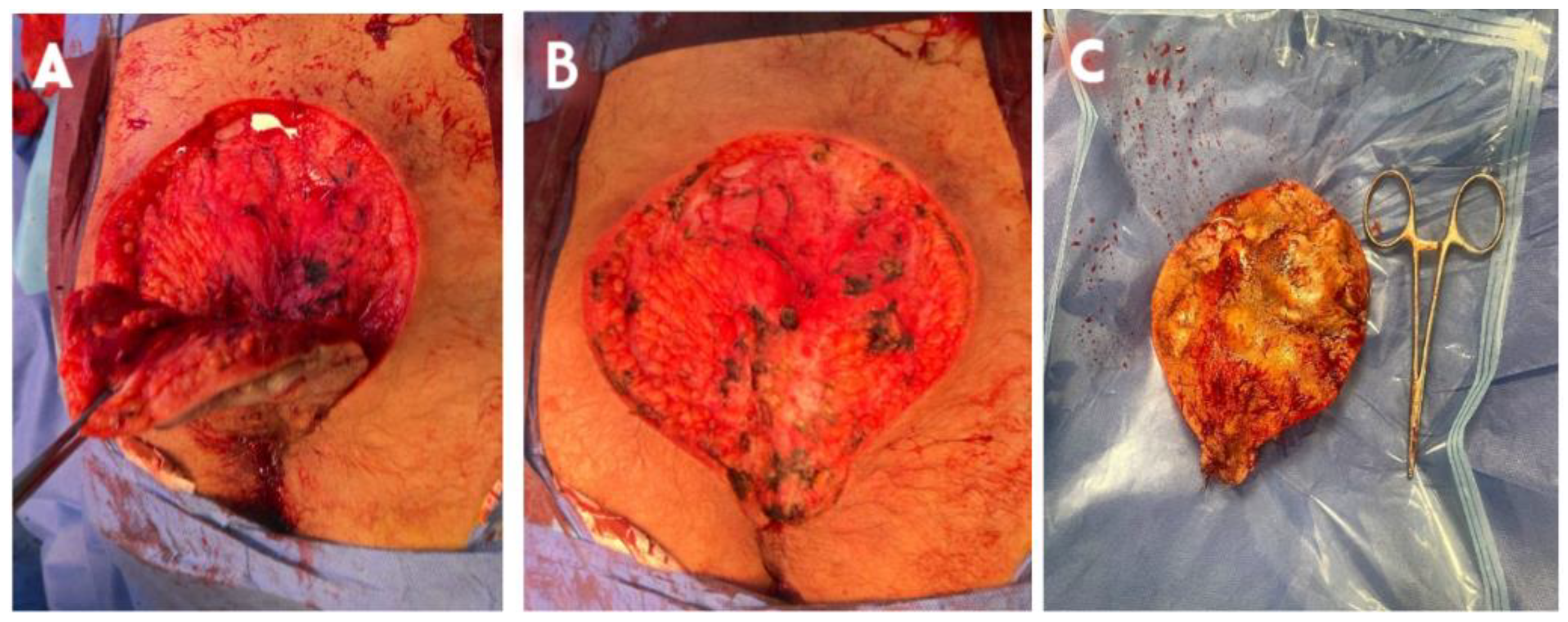
Figure 3). There was also soft tissue edema infiltration around the lesion. After the preanesthetic labtest, surgical treatment began. He was placed in ventral decubitus with rachianesthesia. We proceeded with extensive excision of the lesion until presacral fascia in deep with thin (05 mm) normal tissue margin (
Figure 4). After careful hemostasis, a sterile dressing was made. The patient was discharged with change of the dressing every 02 days and seen for routine follow-up. Following the procedure, the patient’s recovery was monitored closely, with particular attention to wound healing and any signs of infection. The surgical specimen revealed in pathology lab suppurative hidradenitis with sinus tracts opening with a brisk surrounding inflammatory infiltrate within the dermis (
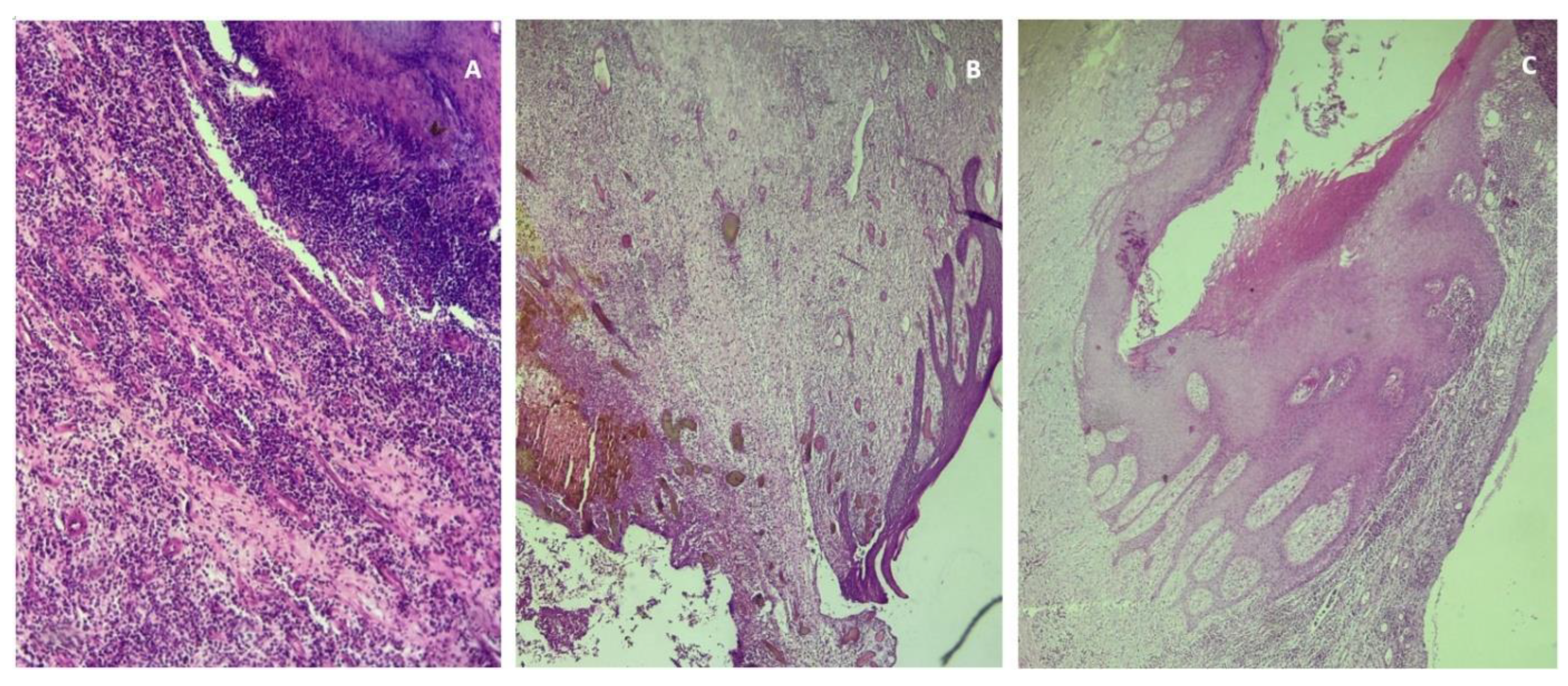
Figure 5). The patient experienced significant improvement in symptoms, and follow-up visits confirmed the effective resolution of the lesion with no immediate recurrence (
Figure 6).
Discussion
This case highlights a rare but significant localization of HS which is known to be commonly found in rich apocrine glands zones such arm pits, groin. HS is diagnosed clinically by its characteristic lesions, typical distribution, chronic nature, and lack of contagion without tendency to heal. Epidemiology is 0.05 to 4.1% of the world population but not well documented here in Africa [
4,
8]. The pathogenesis remains incompletely understood, but it has similar patterns as pilonidal sinus involving follicular occlusion and inflammation. They share also similar risk factors like hyperpilosity, obesity. Our patient was not obese but presented hyper pilosity. The chronicity tends to be specific to HS. However, in atypical locations, clinicians must maintain suspicion and consider other potential diagnoses. Initially, we aimed to rule out a tumoral lesion such as cutaneous squamous cell carcinoma, but the CT scan showing localized soft tissue infiltration provided reassurance. Differential diagnoses for dorsolumbar lesions include furuncles, carbuncles, pilonidal cyst, and extra sphincteric fistula-in-ano (since we are in a proctology unit). Notably, pilonidal sinuses, while histologically similar can also occur unexpected locations such as penis, scalp, abdomen, neck, groin further complicating the diagnostic picture. In our case the anatomopathology department concluded (
Figure 5). The evolution is appraised by several scores including the Hurley severity score for routine clinical practice and sartorius score [
10,
11]. A valid, accurate as well as easy to use scoring system for the assessment of HS severity is needed. Our patient presented a hurley III lesion (
Table 1) justifying our extensive excision of cutaneous, subcutaneous tissue sparing the fascia as directed by some authors. The treatment of t of HS patients include lifestyle change obesity smoking cessation, topical antiseptics associated with oral antibiotics such as tetracyclines, rifampicin, clindamycin that anti inflammatory effects. Further adjunction of anti-TNF-alpha antibody adalimumab and anti-IL-17 secukinumab approved by US Food and Drug Admnistration [
3]. Surgical excision y remains the most radicaly and effective curative treatment [
12,
13]. Surgical techniques include Deroofing, large excision with reconstructive techniques and local wound care. In our case we excised with wide lateral margins. The deep margin included skin, its appendages and subcutaneous tissue as advised by manfredini et al.[
12]. Reconstructive modalities have been described with wound healing adjunct to surgery like negative wound treatment, carbon laser treatment, sometimes with hyperbaric oxygenotherapy were mentioned [
13].
Conclusion
The management of hidradenitis suppurative in atypical locations requires a multidisciplinary approach, integrating medical, surgical and supportive care. The atypical presentation of HS in dorsolumbar region mimicks numerous diagnosis of chronic skin lesions. The description of the best combinations and timing of surgery, wound care and medical therapies, is a matter of future research for the definition of the optimal management of HS patient.
Author Contributions
SA collected the clinical data and drafted the manuscript. RC, MA, LB collection of clinical and pathology data, HL and TT read and supervised the manuscript. All authors contributed to the article and approved the submitted and final version the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent
The patient’s consent was obtained for publication of this case report
Data Availability Statement
No data was used for the research described in the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
IL-17: Interleukin 17
H&E: Hematoxylin and Eosin staining
HS: Hidradenitis suppurativa
PNNs: Polynuclear neutrophils
TNF-alpha: Tumor Necrosis Factor alpha
References
- Zouboulis Cc Desai, N.; Emtestam, L.; Hunger Re Ioannides, D.; Juhász, I.; et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol [Internet]. 2015, 29, 619–644. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/jdv.12966 [cited 4 June 2025]. [CrossRef] [PubMed]
- Verneuil, A. Etudes sur les tumeurs de la peau; de quelques maladies des glandules sudoripares. Arch Gen Med. 1854, 447–468. [Google Scholar]
- McCarthy, S. Hidradenitis Suppurativa. Annu Rev Med [Internet]. 2025, 76, 69–80. Available from: https://www.annualreviews.org/content/journals/10.1146/annurev-med-051223-031234 [cited 8 June 2025]. [CrossRef] [PubMed]
- Ingram, J.R. The epidemiology of hidradenitis suppurativa. Br J Dermatol [Internet]. 2020, 183, 990–998. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/bjd.19435 [cited 9 July 2025]. [CrossRef] [PubMed]
- Poli, F.; Wolkenstein, P.; Revuz, J. Back and Face Involvement in Hidradenitis Suppurativa. Dermatology [Internet]. 2010, 221, 137–141, [cited 2025 Jun 8]. [Google Scholar] [CrossRef] [PubMed]
- Harvey LM, Fortson JK. Hidradenitis Suppurativa at an Uncommon Site: A Review of Its Clinical Features, Diagnostic Difficulties, and Management. Cureus [Internet]. [cited 2025 Jun 23];13(10):e18704. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8584235/. [CrossRef]
- Fabbrocini G, De Vita V. Comorbidities and Complex Syndromes. In: Hidradenitis Suppurativa [Internet]. John Wiley & Sons, Ltd.; 2017 [cited 2025 Jul 9]. p. 55–64. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/9781119424291.ch7.
- Bettoli V, Ruina G. Epidemiology and pathogenesis. In: Hidradenitis Suppurativa [Internet]. 2017 [cited 2025 Jun 26]. p. 3–5. Available from: https://login.research4life.org/tacsgr1onlinelibrary_wiley_com/doi/10.1002/9781119424291.ch2.
- Canoui-Poitrine, F.; Revuz, J.E.; Wolkenstein, P.; Viallette, C.; Gabison, G.; Pouget, F.; et al. Clinical characteristics of a series of 302 French patients with hidradenitis suppurativa, with an analysis of factors associated with disease severity. J Am Acad Dermatol. 2009, 61, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Hurley H. Axiillairy hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign 41. pemphigus: surgical approach. Dermatol Surg. :729–39.
- Sartorius, K.; Emtestam, L.; Jemec, G.B.E.; Lapins, J. Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol [Internet]. 2009, 161, 831–839, [cited 2025 Jul 9]. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, M.; Garbarino, F.; Bigi, L.; Pellacani, G.; Magnoni, C. Surgical and postsurgical wound care in hidradenitis suppurativa. Dermatol Ther [Internet]. 2020, 33, e13282. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/dth.13282 [cited 8 June 2025]. [CrossRef] [PubMed]
- Ezanno, A.C.; Guillem, P.; Gorin, C.; Gabison, G.; Malgras, B.; Fougerousse, A.C. What should a surgeon know about hidradenitis suppurativa? J Visc Surg [Internet]. 2023, 160, 444–455. Available from: https://www.sciencedirect.com/science/article/pii/S187878862300142X [cited 8 June 2025]. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).