Submitted:
07 August 2025
Posted:
11 August 2025
You are already at the latest version
Abstract
Keywords:
1. From Direct to Indirect Laryngoscopy
2. The Quest for the Holy Grail in the DA Management
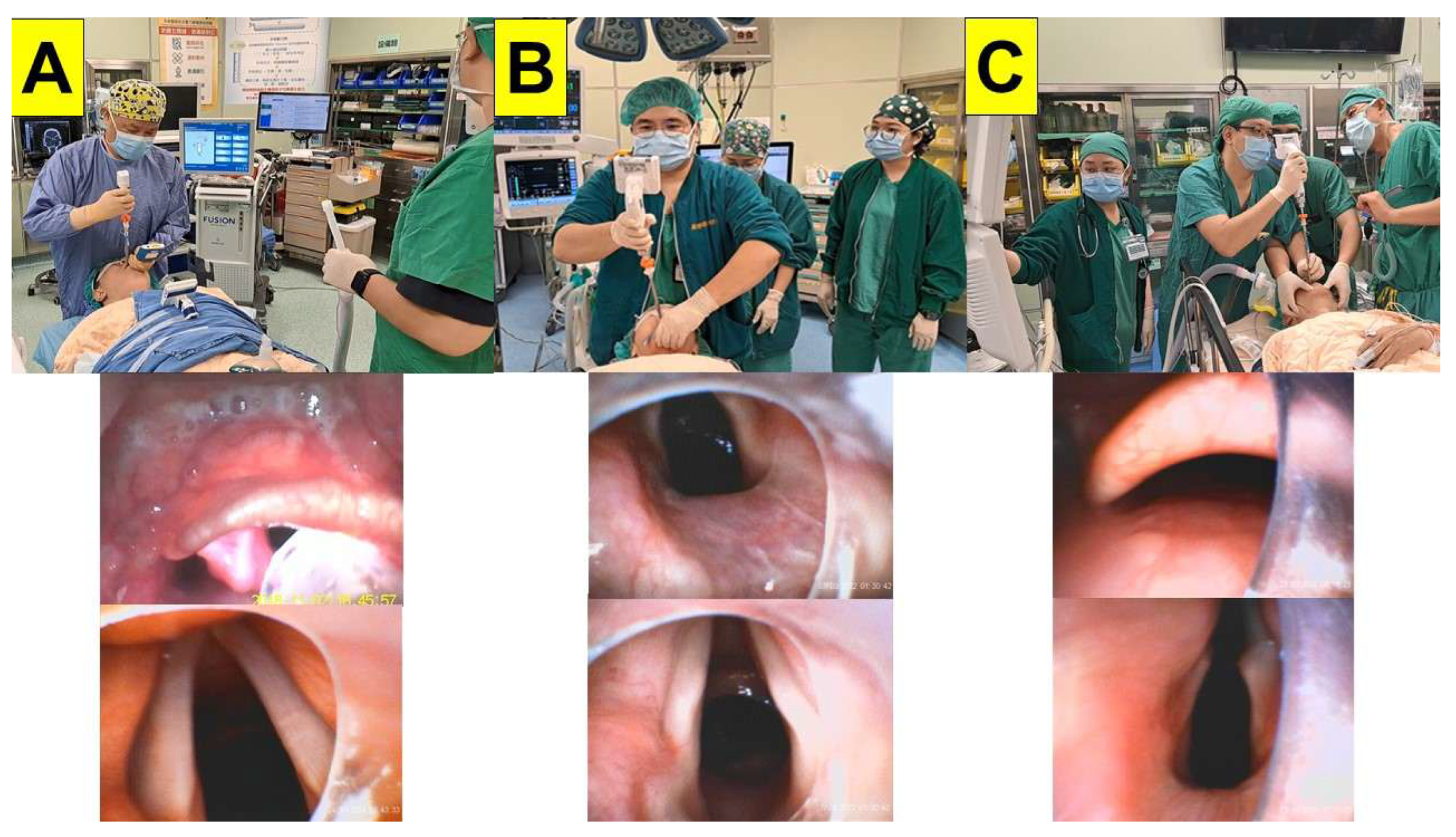
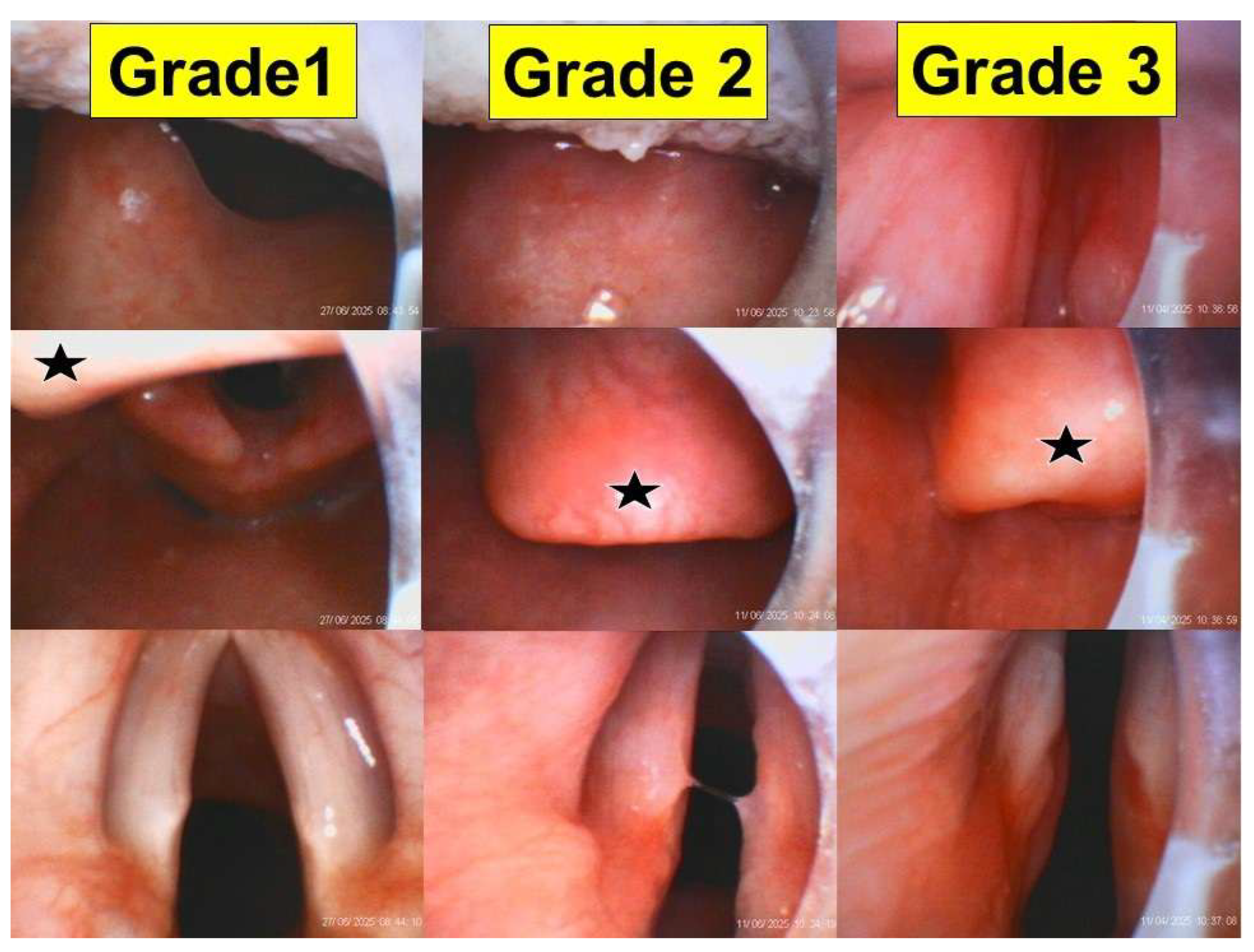
3. Technical Evolution of Styletubation
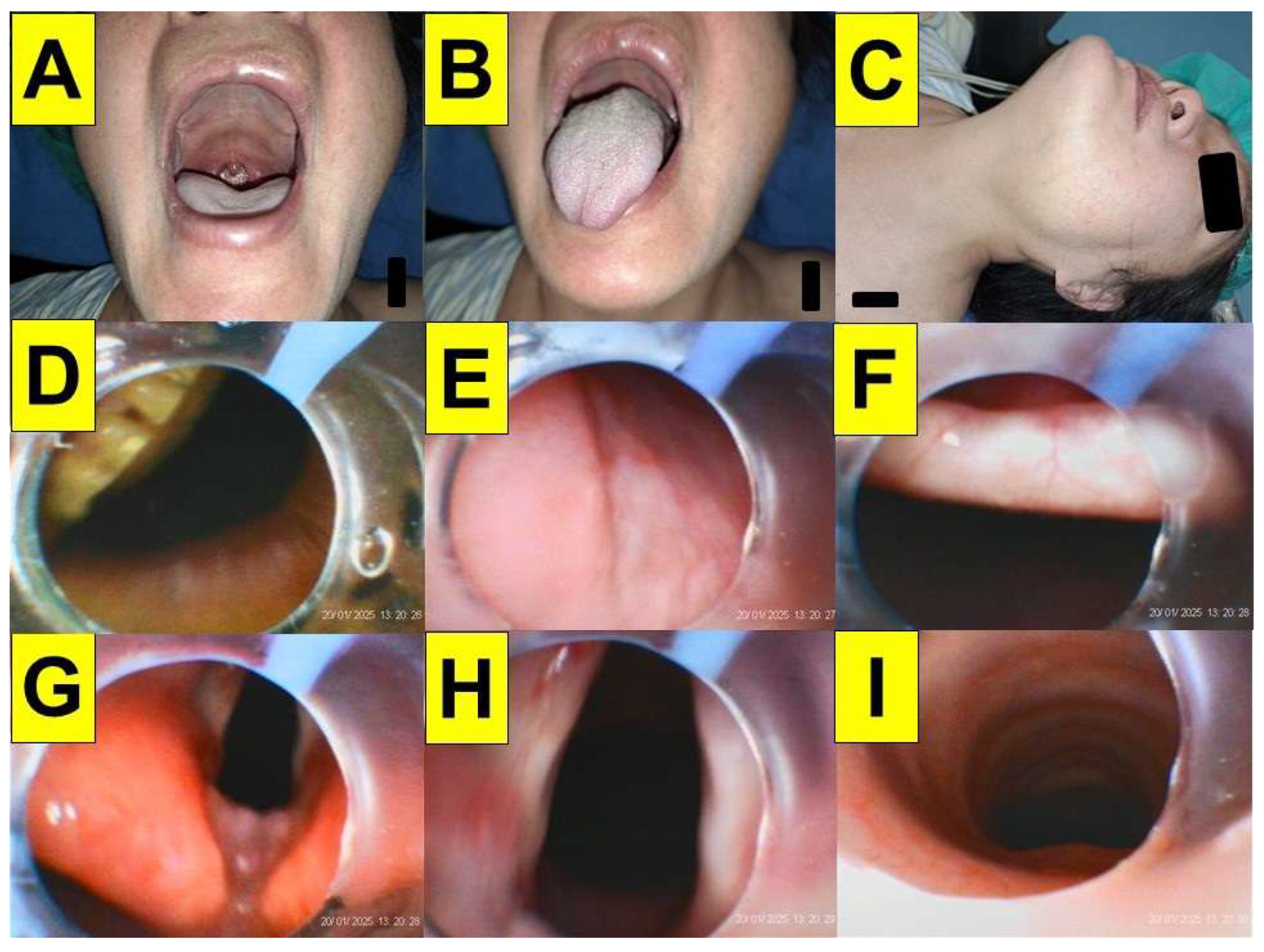
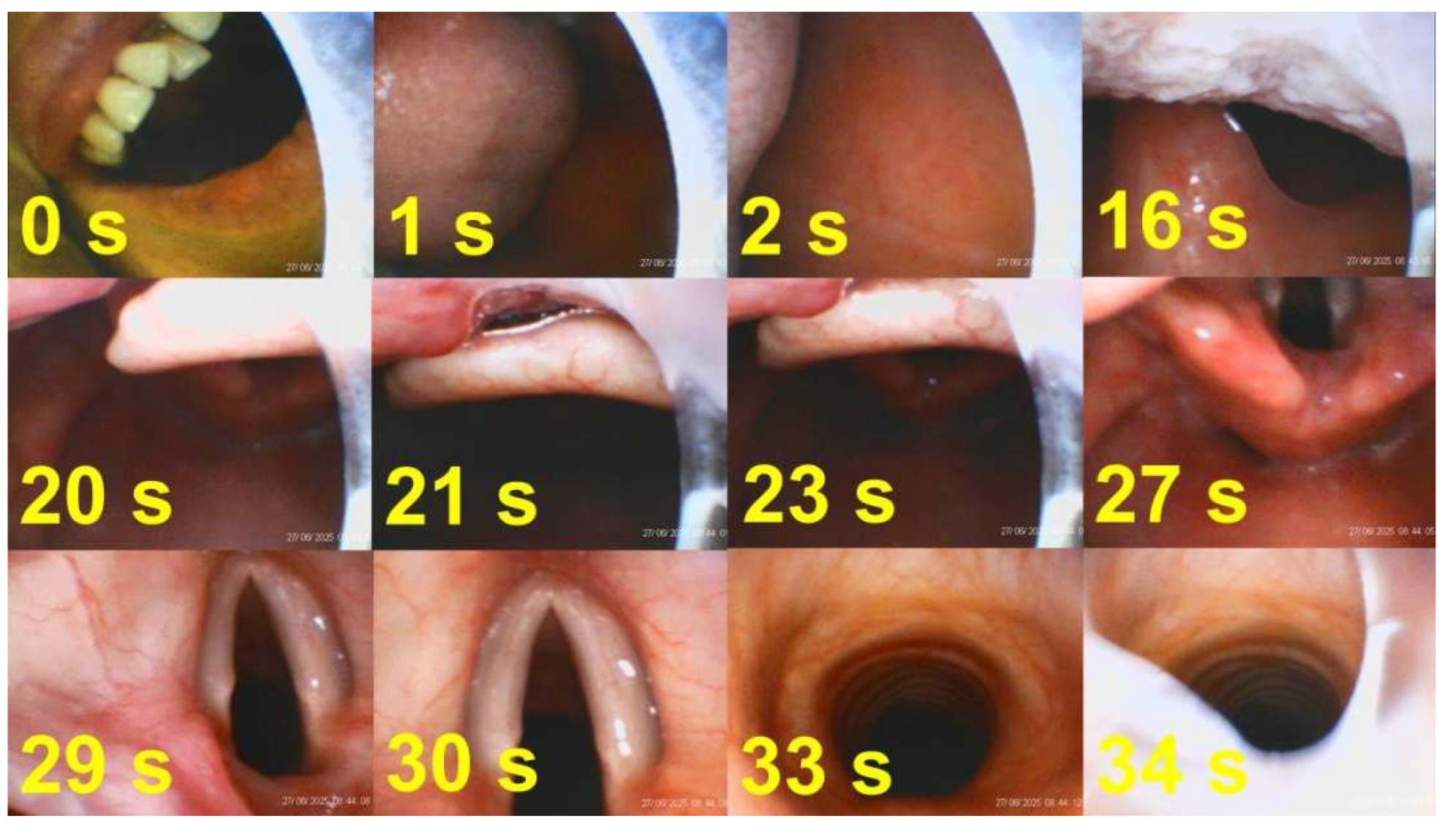
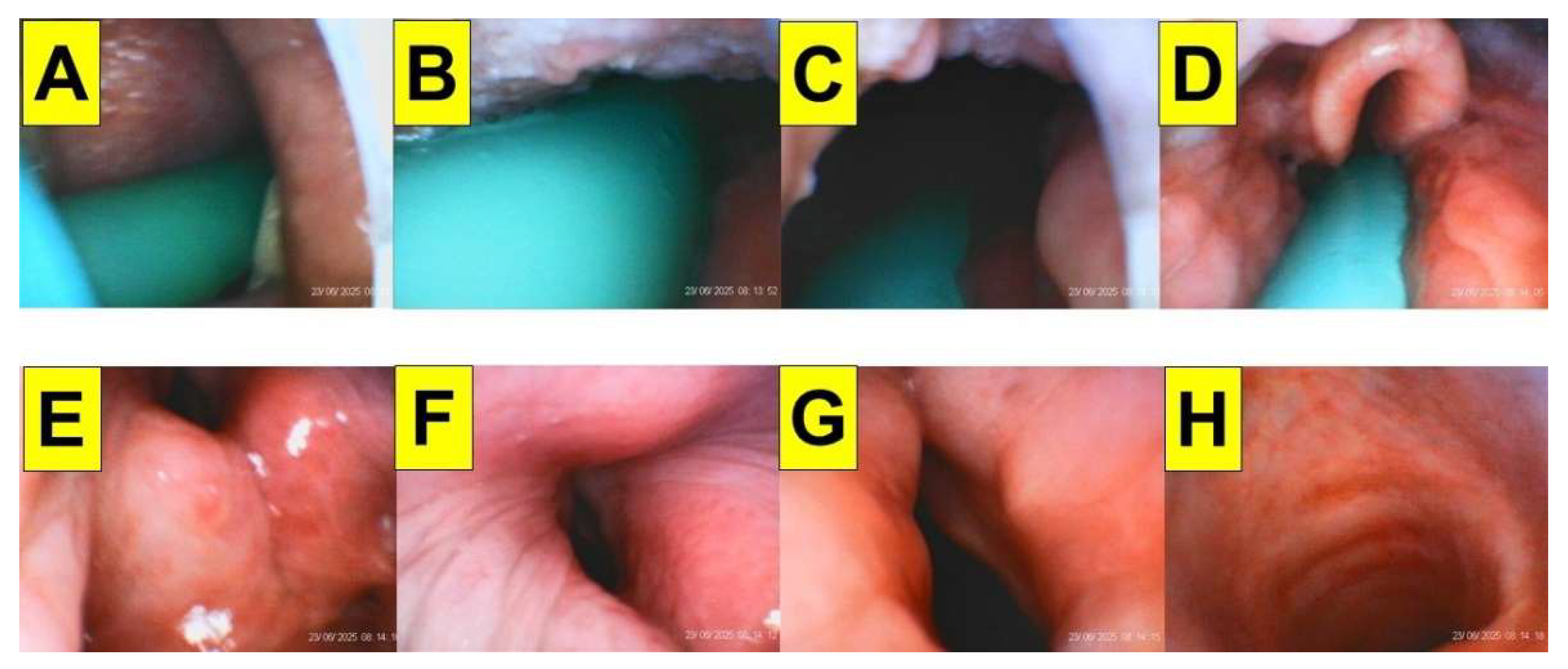
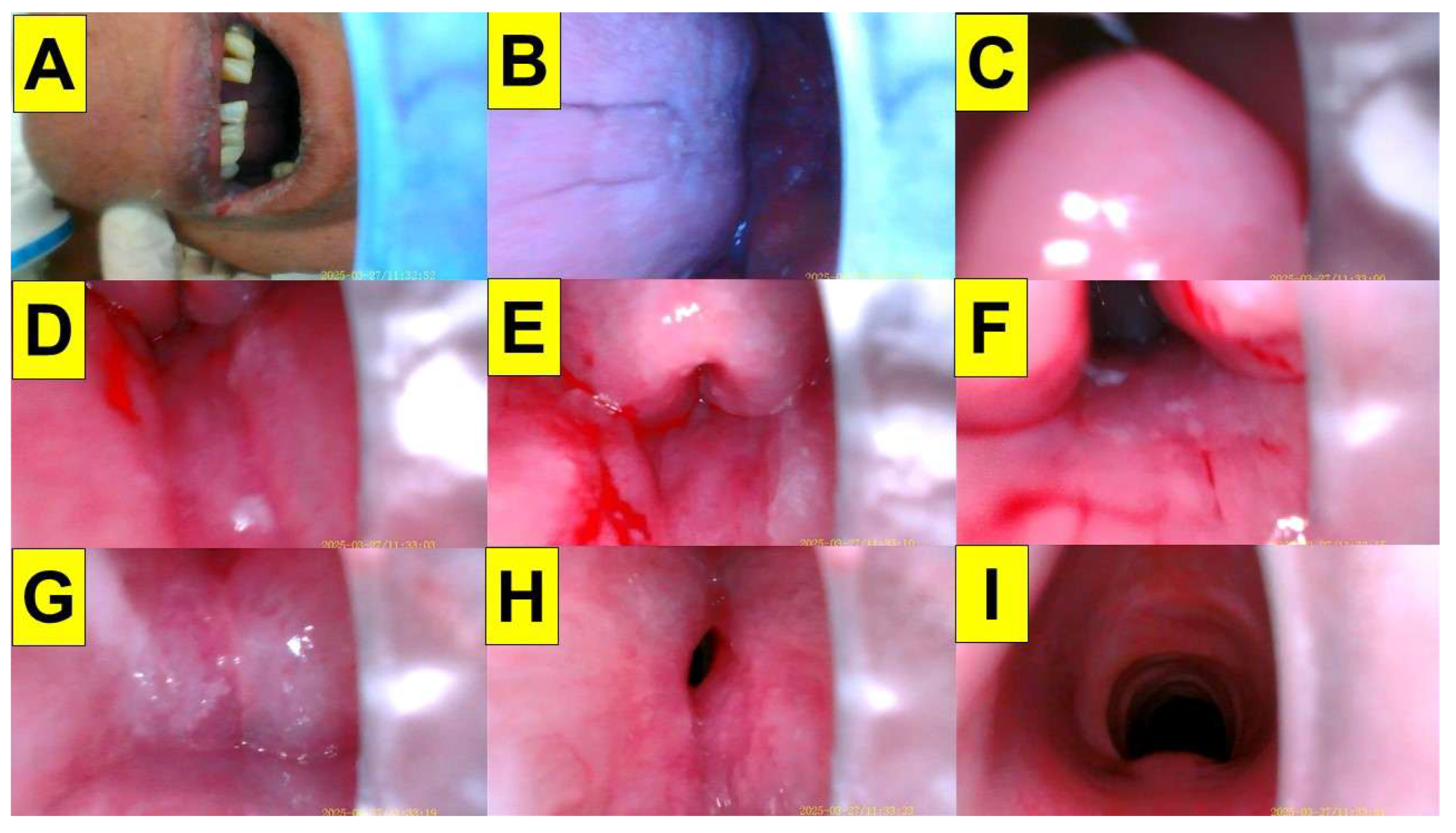
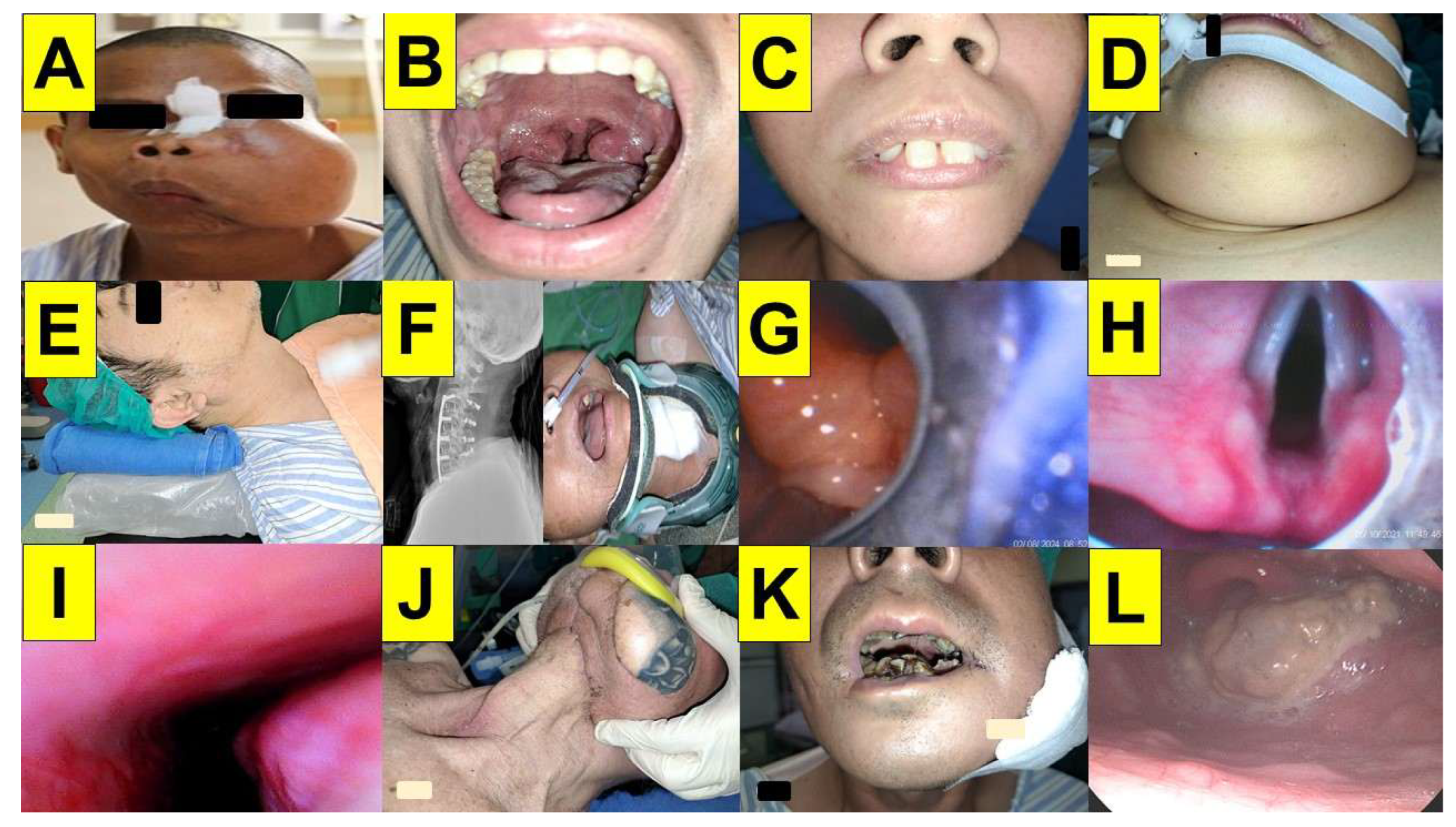
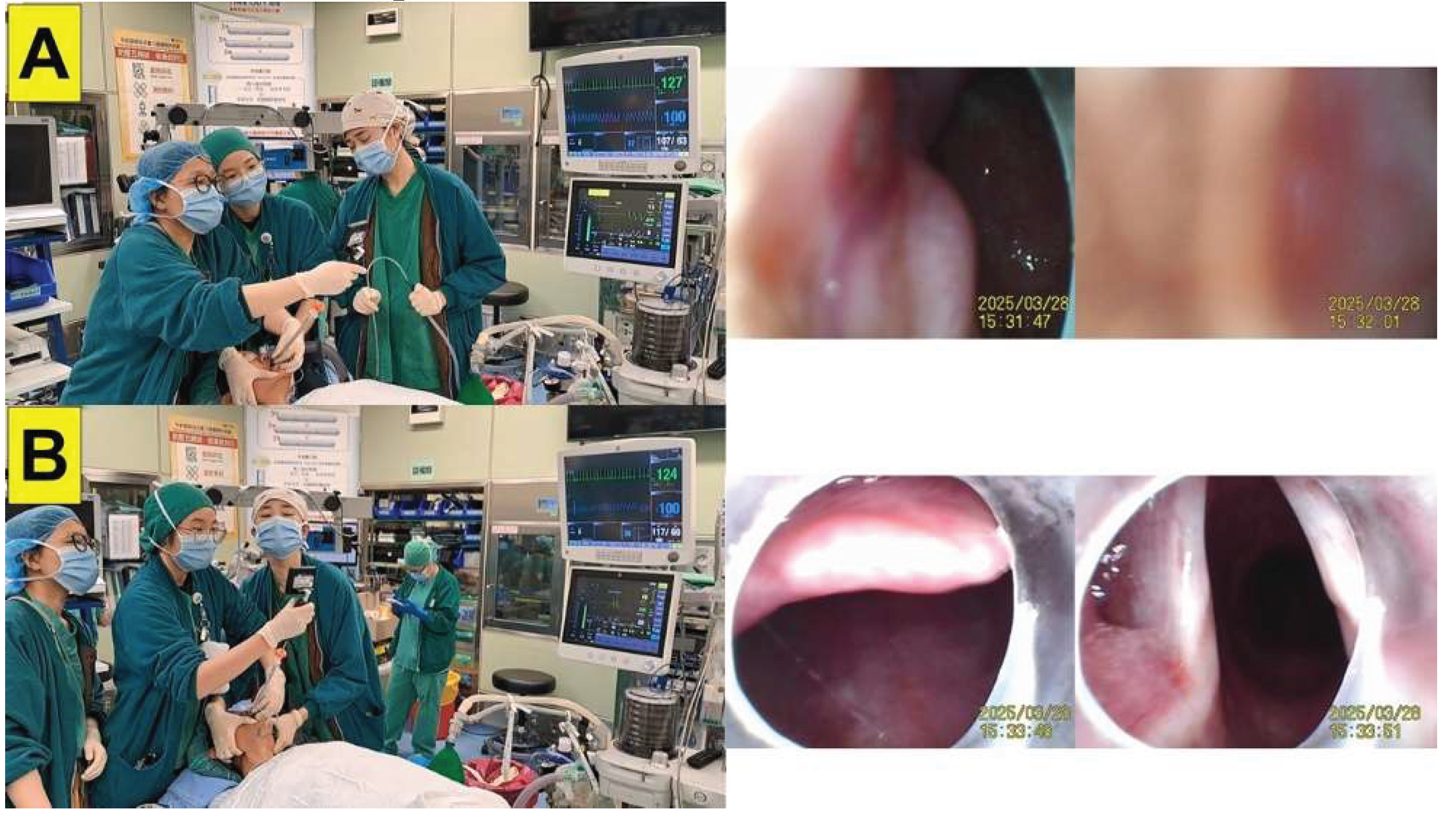
4. Pearls and Pitfalls of Styletubation
5. Discussion
| Laryngoscopy | FOB | Styletubation | |
|---|---|---|---|
| Require wide enough mouth-opening | +++ | - | + |
| Require displacing the tongue to expose glottis | +++ | + | + |
| Require high-grade Cormack-Lehane score | +++ | - | - |
| Need a blade | Yes | No | No |
| Need a stylet | Sometimes | No | No |
| Good POGO score | Sometimes | Always | Always |
| External laryngeal maneuvers are helpful | Often | No | Occasionally |
| Maneuverability along the airway path | Limited | High | High |
| First-pass success rate | Moderate to high | Excellent | Excellent |
| Overall success rate | Moderate to high | High | High |
| Time to intubate | Moderate | Long | Swift |
| Subjective feeling of easiness to operate | Acceptable | Varied | Excellent |
| Impinge on arytenoid / vocal cords | Sometimes | Often | Rare |
| Dental damage/soft tissue injuries | Sometimes | Seldom | Rare |
| Impacted by secretions/blood/vomitus | Yes | Yes | Yes |
| Over-stimulation on airway | Often | Less | Much less |
| Require an adjunctive tool | Sometimes | Sometimes | Seldom |
| Learning curve | Reasonable | Slow | Steep |
| Affordability | Yes | Expensive | Yes |
| Availability | Yes | Limited | Yes |
| Speedy preparedness, easy maintenance | Yes | No | Yes |
| Applicability to awake or asleep intubation | Yes | Yes | Yes |
| Real time imaging/video recording/documenting | Yes | Yes | Yes |
| Easy Airway | Difficult Airway | |
|---|---|---|
| Laryngeal view | Always excellent | Could be difficult |
| First-pass success rate | Near 100% | Acceptable |
| Overall success rate | Near 100% | Acceptable |
| Intubating time (routine operation) | 3 sec to 10 sec | 30 sec to 120 sec |
| Intubating time (for demonstration purpose) | 30 sec to 60 sec | NA |
| Hypoxemia | Very rare | Depends |
| Airway injuries | Very rare | Acceptable |
| Learning curve | 20% to 90% | - |
| Awake/asleep intubation | NA | Applicable |
| Combined with laryngoscopy | NA | Applicable |
6. The Future Perspective
7. Conclusions
References
- Burkle, C.M.; Zepeda, F.A.; Bacon, D.R.; Rose, S.H. A historical perspective on use of the laryngoscope as a tool in anesthesiology. Anesthesiology 2004, 100, 1003–1006. [Google Scholar] [CrossRef]
- Szmuk, P.; Ezri, T.; Evron, S.; Roth, Y.; Katz, J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the Space Age. Intensive Care Med. 2008, 34, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Pieters, B.M.; Eindhoven, G.B.; Acott, C.; van Zundert, A.A. Pioneers of laryngoscopy: indirect, direct and video laryngoscopy. Anaesth. Intensive Care 2015, 43, Suppl–4. [Google Scholar] [CrossRef] [PubMed]
- Pepe, P.E.; Copass, M.K.; Joyce, T.H. Prehospital endotracheal intubation: rationale for training emergency medical personnel. Ann. Emerg. Med. 1985, 14, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.E.; Yealy, D.M. Out-of-hospital endotracheal intubation: where are we? Ann. Emerg. Med. 2006, 47, 532–541. [Google Scholar] [CrossRef]
- Savino, P.B.; Reichelderfer, S.; Mercer, M.P.; Wang, R.C.; Sporer, K.A. Direct versus video laryngoscopy for prehospital intubation: A systematic review and meta-analysis. Acad. Emerg. Med. 2017, 24, 1018–1026. [Google Scholar] [CrossRef]
- Benger, J.R.; Kirby, K.; Black, S.; Brett, S.J.; Clout, M.; Lazaroo, M.J.; Nolan, J.P.; Reeves, B.C.; Robinson, M.; Scott, L.J.; Smartt, H.; South, A.; Stokes, E.A.; Taylor, J.; Thomas, M.; Voss, S.; Wordsworth, S.; Rogers, C.A. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome: The AIRWAYS-2 Randomized Clinical Trial. JAMA. 2018, 320, 779–791. [Google Scholar] [CrossRef]
- Lee, A.F.; Chien, Y.C.; Lee, B.C.; Yang, W.S.; Wang, Y.C.; Lin, H.Y.; Huang, E.P.; Chong, K.M.; Sun, J.T.; Huei-Ming, M.; Hsieh, M.J.; Chiang, W.C. Effect of placement of a supraglottic airway device vs endotracheal intubation on return of spontaneous circulation in adults with out-of-hospital cardiac arrest in Taipei, Taiwan: A cluster randomized clinical trial. JAMA. Netw. Open. 2022, 5, e2148871. [Google Scholar] [CrossRef]
- Magill, I.W. Endotracheal anesthesia. Am. J. Surg. 1936, 34, 450–455. [Google Scholar] [CrossRef]
- Macintosh, R.R. A new laryngoscope. Lancet 1943, 241, 205. [Google Scholar] [CrossRef]
- Bannister, F.B.; Macbeth, R.G. Direct laryngoscopy and tracheal intubation. Lancet 1944, 244, 651–654. [Google Scholar] [CrossRef]
- Mulcaster, J.T.; Mills, J.; Hung, O.R.; MacQuarrie, K.; Law, J.A.; Pytka, S.; Imrie, D.; Field, C. Laryngoscopic intubation: learning and performance. Anesthesiology 2003, 98, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Hindman, B.J.; Santoni, B.G.; Puttlitz, C.M.; From, R.P.; Todd, M.M. Intubation biomechanics: laryngoscope force and cervical spine motion during intubation with Macintosh and Airtraq laryngoscopes. Anesthesiology 2014, 121, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Schmutz, A.; Breddin, I.; Draxler, R.; Schumann, S.; Spaeth, J. Comparison of force distribution during laryngoscopy with the C-MAC D-blade and Macintosh-style blades: A randomised controlled clinical trial. J. Clin. Med. 2024, 13, 2623. [Google Scholar] [CrossRef]
- Nørskov, A.K.; Rosenstock, C.V.; Wetterslev, J.; Astrup, G.; Afshari, A.; Lundstrøm, L.H. Diagnostic accuracy of anaesthesiologists' prediction of difficult airway management in daily clinical practice: a cohort study of 188064 patients registered in the Danish Anaesthesia Database. Anaesthesia 2015, 70, 272–281. [Google Scholar] [CrossRef]
- Endlich, Y.; Lee, J.; Culwick, M.D. Difficult and failed intubation in the first 4000 incidents reported on webAIRS. Anaesth. Intensive Care 2020, 48, 477–487. [Google Scholar] [CrossRef]
- Yuan, J.; Ye, H.; Tan, X.; Zhang, H.; Sun, J. Determinants of difficult laryngoscopy based on upper airway indicators: a prospective observational study. BMC Anesthesiol. 2024, 24, 157. [Google Scholar] [CrossRef]
- Schnittker, R.; Marshall, S.D.; Berecki-Gisolf, J. Patient and surgery factors associated with the incidence of failed and difficult intubation. Anaesthesia 2020, 75, 756–766. [Google Scholar] [CrossRef]
- Ruderman, B.T.; Mali, M.; Kaji, A.H.; Kilgo, R.; Watts, S.; Wells, R.; Limkakeng, A.T.; Borawski, J.B.; Fantegrossi, A.E.; Walls, R.M.; Brown, C.A. 3rd.; National Emergency Airway Registry investigators. Direct vs video laryngoscopy for difficult airway patients in the emergency department: A National Emergency Airway Registry Study. West. J. Emerg. Med. 2022, 23, 706–715. [Google Scholar] [CrossRef]
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of difficult tracheal intubation: A closed claims analysis. Anesthesiology 2019, 131, 818–829. [Google Scholar] [CrossRef]
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; Myatra, S.N.; O'Sullivan, E.P.; Rosenblatt, W.H.; Sorbello, M.; Tung, A. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology 2022, 136, 31–81. [Google Scholar] [CrossRef] [PubMed]
- Paolini, J.B.; Donati, F.; Drolet, P. Review article: video-laryngoscopy: another tool for difficult intubation or a new paradigm in airway management? Can. J. Anaesth. 2013, 60, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst. Rev. 2022, 4(4):CD011136. [CrossRef]
- Greenland, K.B.; Eley, V.; Edwards, M.J.; Allen, P.; Irwin, M.G. The origins of the sniffing position and the three axes alignment theory for direct laryngoscopy. Anaesth. Intensive Care 2008, 36, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Greenland, K.B. Two curves and three columns–A reappraisal of direct laryngoscopy. Operative Techniques in Otolaryngology-Head and Neck Surgery 2020, 31, 83–88. [Google Scholar] [CrossRef]
- Aziz, M.F.; Bayman, E.O.; Van Tienderen, M.M.; Todd, M.M. StAGE Investigator Group; Brambrink, A.M. Predictors of difficult videolaryngoscopy with GlideScope® or C-MAC® with D-blade: secondary analysis from a large comparative videolaryngoscopy trial. Br. J. Anaesth. 2016, 117, 118–123. [Google Scholar] [CrossRef]
- Aziz, M.F.; Abrons, R.O.; Cattano, D.; Bayman, E.O.; Swanson, D.E.; Hagberg, C.A.; Todd, M.M.; Brambrink, A.M. First-attempt intubation success of video laryngoscopy in patients with anticipated difficult direct laryngoscopy: A multicenter randomized controlled trial comparing the C-MAC D-blade versus the GlideScope in a mixed provider and diverse patient population. Anesth. Analg. 2016, 122, 740–750. [Google Scholar] [CrossRef]
- Cooper, R.M.; Pacey, J.A.; Bishop, M.J.; McCluskey, S.A. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can. J. Anaesth. 2005, 52, 191–198. [Google Scholar] [CrossRef]
- Saul, S.A.; Ward, P.A.; McNarry, A.F. Airway management: The current role of videolaryngoscopy. J. Pers. Med. 2023, 13, 1327. [Google Scholar] [CrossRef]
- Ruetzler, K.; Bustamante, S.; Schmidt, M.T.; Almonacid-Cardenas, F.; Duncan, A.; Bauer, A.; Turan, A.; Skubas, N.J.; Sessler, D.I.; Collaborative VLS Trial Group. Video laryngoscopy vs direct laryngoscopy for endotracheal intubation in the operating room: A cluster randomized clinical trial. JAMA. 2024, 331, 1279–1286. [Google Scholar] [CrossRef]
- Prekker, M.E.; Driver, B.E.; Trent, S.A.; Resnick-Ault, D.; Seitz, K.P.; Russell, D.W.; Gaillard, J.P.; Latimer, A.J.; Ghamande, S.A.; Gibbs, K.W.; Vonderhaar, D.J.; Whitson, M.R.; Barnes, C.R.; Walco, J.P.; Douglas, I.S.; Krishnamoorthy, V.; Dagan, A.; Bastman, J.J.; Lloyd, B.D.; Gandotra, S,; Goranson, J.K.; Mitchell, S.H.; White, H.D.; Palakshappa, J.A.; Espinera, A.; Page, D.B.; Joffe, A.; Hansen, S.J.; Hughes, C.G.; George, T.; Herbert, J.T.; Shapiro, N.I.; Schauer, S.G.; Long, B.J.; Imhoff, B.; Wang, L.; Rhoads, J.P.; Womack, K.N.; Janz, D.R.; Self, W.H.; Rice, T.W.; Ginde, A.A.; Casey, J.D.; Semler, M.W.; DEVICE Investigators and the Pragmatic Critical Care Research Group. Video versus direct laryngoscopy for tracheal intubation of critically ill adults. N. Engl. J. Med. 2023, 389, 418-429. [CrossRef]
- Prekker, M.E.; Trent, S.A.; Lofrano, A.; Russell, D.W.; Barnes, C.R.; Brewer, J.M.; Doerschug, K.C.; Gaillard, J.P.; Gandotra, S.; Ginde, A.A.; Ghamande, S.; Gibbs, K.W.; Hughes, C.G.; Janz, D.R.; Khan, A.; Mitchell, S.H.; Page, D.B.; Rice, T.W.; Self, W.H.; Smith, L.M.; Stempek, S.B.; Vonderhaar, D.J.; West, J.R.; Whitson, M.R.; Casey, J.D.; Semler, M.W.; Driver, B.E. Laryngoscopy and tracheal intubation: Does use of a video laryngoscope facilitate both steps of the procedure? Ann. Emerg. Med. 2023, 82, 425–431. [Google Scholar] [CrossRef]
- Sgalambro, F.; Sorbello, M. Videolaryngoscopy and the search for the Holy Grail. Br. J. Anaesth. 2017, 118, 471–472. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.; Wen, X.; Wang, X.; Yang, J.; Zhou, H.; Guo, J.; Su, Y.; Zhang, T. Comparison of outcomes between video laryngoscopy and flexible fiberoptic bronchoscopy for endotracheal intubation in adults with cervical neck immobilization: A systematic review and meta-analysis of randomized controlled trials. PLoS. One 2024, 19, e0313280. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.Z.; Cheng, X.X.; Zhang, T.; Zhang, G.L.; Zhang, G.J.; Wu, W.W.; Li, R.H. A visual laryngoscope combined with a fiberoptic bronchoscope improves intubation outcomes in patients with predicted difficult airways in thoracic surgery. BMC. Pulm. Med. 2024, 24, 558. [Google Scholar] [CrossRef]
- Shikani, A.H. New "seeing" stylet-scope and method for the management of the difficult airway. Otolaryngol. Head Neck Surg. 1999, 120, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Matek, J.; Kolek, F.; Klementova, O.; Michalek, P.; Vymazal, T. Optical devices in tracheal intubation-State of the art in 2020. Diagnostics (Basel) 2021, 11, 575. [Google Scholar] [CrossRef]
- Hung, O.R.; Pytka, S.; Morris, I.; Murphy, M.; Launcelott, G.; Stevens, S.; MacKay, W.; Stewart, R.D. Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology 1995, 83, 509–514. [Google Scholar] [CrossRef]
- Agrò, F.; Hung, O.R.; Cataldo, R.; Carassiti, M.; Gherardi, S. Lightwand intubation using the Trachlight: a brief review of current knowledge. Can. J. Anaesth. 2001, 48, 592–599. [Google Scholar] [CrossRef]
- Hung, O. Why can't I get a Trachlight™? Can. J. Anaesth. 2025, 72, 230–232. [Google Scholar] [CrossRef]
- Kitamura, T.; Yamada, Y.; Du, H.L.; Hanaoka, K. Efficiency of a new fiberoptic stylet scope in tracheal intubation. Anesthesiology 1999, 91, 1628–1632. [Google Scholar] [CrossRef]
- Thong, S.Y.; Wong, T.G. Clinical uses of the Bonfils retromolar intubation fiberscope: a review. Anesth. Analg. 2012, 115, 855–866. [Google Scholar] [CrossRef]
- Godai, K.; Moriyama, T.; Kanmura, Y. Comparison of the MultiViewScope stylet scope and the direct laryngoscope with the Miller blade for the intubation in normal and difficult pediatric airways: A randomized, crossover, manikin study. PLoS. One 2020, 15, e0237593. [Google Scholar] [CrossRef] [PubMed]
- Nabecker, S.; Ottenhausen, T.; Theiler, L.; Braun, M.; Greif, R.; Riva, T. Prospective observational study evaluating the C-MAC video stylet for awake tracheal intubation: a single-center study. Minerva Anestesiol. 2021, 87, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Luk HN, Luk HN, Qu JZ, Shikani A. A paradigm shift of airway management: the role of video-assisted intubating stylet technique. In: Lovich-Sapola J, ed. Advances in Tracheal Intubation [Working Title]. London: Inte-chOpen [Internet]; 2022. [CrossRef]
- Luk HN, Qu JZ, Shikani A. Styletubation: The paradigmatic role of video-assisted intubating stylet technique for routine tracheal intubation. Asian J Anesthesiol. 2023;61(2):102-106. [CrossRef]
- Luk HN, Qu JZ, Shikani A. Styletubation for routine tracheal intubation for ear-nose-throat surgical procedures. Annal of Otol Head and Neck Surg. 2023;2(3):1-13.
- Luk, HN.; Qu, JZ. Styletubation versus laryngoscopy: A new paradigm for routine tracheal intubation. Surgeries. 2024;5,135-161. [CrossRef]
- Lee HC, Wu BG, Chen BC, Luk HN, Qu JZ. Structured routine use of styletubation for oro-tracheal intubation in obese patients undergoing bariatric surgeries—A case series report. Healthcare (Basel). 2024;12,1404. [CrossRef]
- Cortellazzi, P.; Caldiroli, D.; Byrne, A.; Sommariva, A.; Orena, E.F.; Tramacere, I. Defining and developing expertise in tracheal intubation using a GlideScope(®) for anaesthetists with expertise in Macintosh direct laryngoscopy: an in-vivo longitudinal study. Anaesthesia 2015, 70, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Halligan, M.; Charters, P. A clinical evaluation of the Bonfils intubation fibrescope. Anaesthesia 2003, 58, 1087–1091. [Google Scholar] [CrossRef]
- Jiang, L.; Qiu, S.; Zhang, P.; Yao, W.; Chang, Y.; Dai, Z. The midline approach for endotracheal intubation using GlideScope video laryngoscopy could provide better glottis exposure in adults: a randomized controlled trial. BMC. Anesthesiol. 2019, 19, 200. [Google Scholar] [CrossRef]
- Karamchandani, K.; Nasa, P.; Jarzebowski, M.; Brewster, D.J.; De Jong, A.; Bauer, P.R.; Berkow, L.; Brown, C.A. 3rd.; Cabrini, L.; Casey, J.; Cook, T.; Divatia, J.V.; Duggan, L.V.; Ellard, L.; Ergan, B.; Jonsson Fagerlund, M,; Gatward, J.; Greif, R.; Higgs, A.; Jaber, S.; Janz, D.; Joffe, A.M.; Jung, B.; Kovacs, G.; Kwizera, A.; Laffey, J.G.; Lascarrou, J.B.; Law, J.A.; Marshall, S.; McGrath, B.A.; Mosier, J.M.; Perin, D.; Roca, O.; Rollé, A.; Russotto, V.; Sakles, J.C.; Shrestha, G.S.; Smischney, N.J.; Sorbello, M.; Tung, A.; Jabaley, C.S.; Myatra, S.N.; Society of Critical Care Anesthesiologists (SOCCA) Physiologically Difficult Airway Task Force. Tracheal intubation in critically ill adults with a physiologically difficult airway. An international Delphi study. Intensive Care Med. 2024, 50, 1563-1579. [CrossRef]
- Levitan, R.M. Design rationale and intended use of a short optical stylet for routine fiberoptic augmentation of emergency laryngoscopy. Am. J. Emerg. Med. 2006, 24, 490–495. [Google Scholar] [CrossRef]
- Chiu, W.C.; Wu, Z.F.; Lai, M.F.; Lai, H.C. Combination use of laryngoscope, jaw thrust, and Trachway for improving difficult tracheal intubation in obese. J. Med. Sci. 2022, 42, 197–198. [Google Scholar] [CrossRef]
- Bonilla González, A.I.; Rivas Alpuche, J.G.; Navarrete García, H.E.; Wong Salazar, L.H.; Atondo Laguna, C.M.; Avilés Sánchez, P.A. Successful intubation with a flexible optical stylet in a patient with predictors of difficult airway using pharyngeal clearance technique with a laryngoscope: A case report. Med. Int. (Lond). 2025, 5, 40. [Google Scholar] [CrossRef]
- Van Zundert, A.A.; Pieters, B.M. Combined technique using videolaryngoscopy and Bonfils for a difficult airway intubation. Br. J. Anaesth. 2012, 108, 327–328. [Google Scholar] [CrossRef]
- Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-twin technique for airway management, combining video-intubating stylet with videolaryngoscope: A case series report and review of the literature. Healthcare (Basel) 2022, 10, 2175. [Google Scholar] [CrossRef]
- Villa, D.; Aspi, M.T.B.; Cruz, R.M.P. Combined use of C-MAC video laryngoscope and Bonfils intubating fiberscope in a pediatric patient with a huge laryngeal mass: A case report. Acta Medica Philippina 2022, 56. [Google Scholar] [CrossRef]
- Witkam, R.L.; Bruhn, J.; Hoogerwerf, N.; Koch, R.M.; van Eijk, L.T. Combining a McGrath video laryngoscope and C-MAC video stylet for the endotracheal intubation of a patient with a laryngeal carcinoma arising from the anterior side of the epiglottis: A case report. Anesth. Res. 2025, 2, 5. [Google Scholar] [CrossRef]
- Cormack, R.S.; Lehane, J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984, 39, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Krage, R.; van Rijn, C.; van Groeningen, D.; Loer, S.A.; Schwarte, L.A.; Schober, P. Cormack-Lehane classification revisited. Br. J. Anaesth. 2010, 105, 220–227. [Google Scholar] [CrossRef]
- Kriege, M. , Noppens, R.R.; Turkstra, T.; Payne, S.; Kunitz, O.; Tzanova, I.; Schmidtmann, I.; EMMA Trial Investigators Group. A multicentre randomised controlled trial of the McGrath™ Mac videolaryngoscope versus conventional laryngoscopy. Anaesthesia 2023, 78, 722–729. [Google Scholar] [CrossRef] [PubMed]
- Kriege, M.; Lang, P.; Lang, C.; Schmidtmann, I.; Kunitz, O.; Roth, M.; Strate, M.; Schmutz, A.; Vits, E.; Balogh, O.; Jänig, C. A comparison of the McGrath videolaryngoscope with direct laryngoscopy for rapid sequence intubation in the operating theatre: a multicentre randomised controlled trial. Anaesthesia 2024, 79, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Tsay, P.J.; Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted intubating stylet technique for difficult intubation: A case series report. Healthcare (Basel) 2022, 10, 741. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhao, K.Y.; Zhang, P.; Li, R.H. Comparison of video laryngoscope, video stylet, and flexible videoscope for transoral endotracheal intubation in patients with difficult airways: a randomized, parallel-group study. Trials 2023, 24, 599. [Google Scholar] [CrossRef]
- Crawley, S.M.; Dalton, A.J. Predicting the difficult airway. BJA. Education 2015, 15, 253–257. [Google Scholar] [CrossRef]
- Roth, D.; Pace, N.L.; Lee, A.; Hovhannisyan, K.; Warenits, A.M.; Arrich, J.; Herkner, H. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst. Rev. 2018, 5, CD008874. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, J.E.; Jeong, D.H.; Lee, J. Combined use of a McGrath® MAC video laryngoscope and Frova Intubating Introducer in a patient with Pierre Robin syndrome: A case report. Korean J. Anesthesiol. 2014, 66, 310–313. [Google Scholar] [CrossRef]
- Peterson, J.D.; Puricelli, M.D.; Alkhateeb, A.; Figueroa, A.D.; Fletcher, S.L.; Smith, R.J.H.; Kacmarynski, D.S.F. Rigid video laryngoscopy for intubation in severe Pierre Robin sequence: A retrospective review. Laryngoscope 2021, 131, 1647–1651. [Google Scholar] [CrossRef] [PubMed]
- Leong, S.M.; Tiwari, A.; Chung, F.; Wong, D.T. Obstructive sleep apnea as a risk factor associated with difficult airway management-A narrative review. J. Clin. Anesth. 2018, 45, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Nagappa, M.; Wong, D.T.; Cozowicz, C.; Ramachandran, S.K.; Memtsoudis, S.G.; Chung, F. Is obstructive sleep apnea associated with difficult airway? Evidence from a systematic review and meta-analysis of prospective and retrospective cohort studies. PLoS. One 2018, 13, e0204904. [Google Scholar] [CrossRef] [PubMed]
- Seet, E.; Chung, F.; Wang, C.Y.; Tam, S.; Kumar, C.M.; Ubeynarayana, C.U.; Yim, C.C.; Chew, E.F.F.; Lam, C.K.M.; Cheng, B.C.P.; Chan, M.T.V. Association of obstructive sleep apnea with difficult intubation: Prospective multicenter observational cohort study. Anesth. Analg. 2021, 133, 196–204. [Google Scholar] [CrossRef]
- Neto, J.M.; Teles, A.R.; Barbosa, J.; Santos, O. Teeth damage during general anesthesia. J. Clin. Med. 2023, 12, 5343. [Google Scholar] [CrossRef]
- Chari, A.; Tejesh, C.A.; Sudarshan, K.S. ; TAScope-guided rapid sequence intubation of a case of retrognathia with a history of failed intubation. Saudi J. Anaesth. 2023, 17, 427–429. [Google Scholar] [CrossRef]
- De Jong, A.; Molinari, N.; Pouzeratte, Y.; Verzilli, D.; Chanques, G.; Jung, B.; Futier, E.; Perrigault, P.F.; Colson, P.; Capdevila, X.; Jaber, S. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. Br. J. Anaesth. 2015, 114, 297–306. [Google Scholar] [CrossRef]
- Thota, B.; Jan, K.M.; Oh, M.W.; Moon, T.S. Airway management in patients with obesity. Saudi J. Anaesth. 2022, 16, 76–81. [Google Scholar] [CrossRef]
- Ng, M.; Hastings, R.H. Successful direct laryngoscopy assisted by posture in a patient with ankylosing spondylitis. Anesth. Analg. 1998, 87, 1436–1437. [Google Scholar] [CrossRef]
- Saricicek, V.; Mizrak, A.; Gul, R.; Goksu, S.; Cesur, M. GlideScope video laryngoscopy use tracheal intubation in patients with ankylosing spondylitis: a series of four cases and literature review. J. Clin. Monit. Comput. 2014, 28, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Lili, X.; Zhiyong, H.; Jianjun, S. A comparison of the GlideScope with the Macintosh laryngoscope for nasotracheal intubation in patients with ankylosing spondylitis. J. Neurosurg. Anesthesiol. 2014, 26, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.C.; Lin, S.; He, H.F. Case report: double visualization intubation strategy for patients with ankylosing spondylitis. Front. Med. (Lausanne) 2022, 9, 659624. [Google Scholar] [CrossRef] [PubMed]
- Tsay, P.J.; Hsu, S.W.; Peng, H.C.; Wang, C.H.; Lee, S.W.; Lai, H.Y. Trachway intubating stylet for tracheal intubation in an ankylosing spondylitis patient undergoing total hip replacement under general anesthesia. Acta Anaesthesiol. Taiwan. 2011, 49, 159–161. [Google Scholar] [CrossRef]
- Ndoko, S.K.; Amathieu, R.; Tual, L.; Polliand, C.; Kamoun, W.; El Housseini, L.; Champault, G.; Dhonneur, G. Tracheal intubation of morbidly obese patients: a randomized trial comparing performance of Macintosh and Airtraq laryngoscopes. Br. J. Anaesth. 2008, 100, 263–268. [Google Scholar] [CrossRef]
- Hoshijima, H.; Denawa, Y.; Tominaga, A.; Nakamura, C.; Shiga, T.; Nagasaka, H. Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: A systematic review and meta-analysis. J. Clin. Anesth. 2018, 44, 69–75. [Google Scholar] [CrossRef]
- Lee, J.M.; Lee, S.K.; Jang, M.; Oh, M.; Park, E.Y. A comparison of the effectiveness of the McCoy laryngoscope and the C-MAC D-blade video laryngoscope in obese patients. Medicina 2024, 60, 1285. [Google Scholar] [CrossRef]
- Suppan, L.; Tramèr, M.R.; Niquille, M.; Grosgurin, O.; Marti, C. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: systematic review and meta-analysis of randomized controlled trials. Br. J. Anaesth. 2016, 116, 27–36. [Google Scholar] [CrossRef]
- Dutta, K.; Sriganesh, K.; Chakrabarti, D.; Pruthi, N.; Reddy, M. Cervical spine movement during awake orotracheal intubation with fiberoptic scope and McGrath videolaryngoscope in patients undergoing surgery for cervical spine instability: A randomized control trial. J. Neurosurg. Anesthesiol. 2020, 32, 249–255. [Google Scholar] [CrossRef]
- Paik, H.; Park, H.P. Randomized crossover trial comparing cervical spine motion during tracheal intubation with a Macintosh laryngoscope versus a C-MAC D-blade videolaryngoscope in a simulated immobilized cervical spine. BMC. Anesthesiol. 2020, 20, 201. [Google Scholar] [CrossRef]
- Chaudery, H.; Hameed, H.; Sharif, Z.; Asinger, S.; McKechnie, A. Comparative efficacy of videolaryngoscopy and direct laryngoscopy in patients living with obesity: A meta-analysis. Cureus 2024, 16, e76558. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Kim, J.A.; Kim, C.S.; Ahn, H.J.; Yang, M.K.; Choi, S.J. Comparison of tracheal intubation with the Airway Scope or Clarus Video System in patients with cervical collars. Anaesthesia 2011, 66, 694–698. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.; Lee, Y.; Park, H.P.; Chung, J.; Yoon, H.K.; Kim, T.K. Cervical spine motion during tracheal intubation using an Optiscope versus the McGrath videolaryngoscope in patients with simulated cervical immobilization: A prospective randomized crossover study. Anesth. Analg. 2019, 129, 1666–1672. [Google Scholar] [CrossRef]
- Yoon, H.K.; Lee, H.C.; Park, J.B.; Oh, H.; Park, H.P. McGrath MAC videolaryngoscope versus Optiscope video stylet for tracheal intubation in patients with manual inline cervical stabilization: A randomized trial. Anesth. Analg. 2020, 130, 870–878. [Google Scholar] [CrossRef]
- Park, J.W.; An, S.; Park, S.; Nahm, F.S.; Han, S.H.; Kim, J.H. Comparison of a new video intubation stylet and McGrath® MAC video laryngoscope for intubation in an airway manikin with normal airway and cervical spine immobilization scenarios by novice personnel: A randomized crossover study. Biomed. Res. Int. 2021, 2021, 4288367. [Google Scholar] [CrossRef]
- Hung, K.C.; Chang, Y.J.; Chen, I.W.; Lin, C.M.; Liao, S.W.; Chin, J.C.; Chen, J.Y.; Yew, M.; Sun, C.K. Comparison of video-stylet and video-laryngoscope for endotracheal intubation in adults with cervical neck immobilisation: A meta-analysis of randomised controlled trials. Anaesth. Crit. Care Pain Med. 2021, 40, 100965. [Google Scholar] [CrossRef]
- Chen, I.W.; Li, Y.Y.; Hung, K.C.; Chang, Y.J.; Chen, J.Y.; Lin, M.C.; Wang, K.F.; Lin, C.M.; Huang, P.W.; Sun, C.K. Comparison of video-stylet and conventional laryngoscope for endotracheal intubation in adults with cervical spine immobilization: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 2022, 101, e30032. [Google Scholar] [CrossRef]
- Sanu, A.; Ahmed, S.M. A comparative study between video laryngoscope and video stylet for tracheal intubation in patients with simulated cervical fracture injury: A prospective randomised controlled study. Cureus 2024, 16, e66360. [Google Scholar] [CrossRef]
- Yoo, J.Y.; Park, S.Y.; Kim, J.Y.; Kim, M.; Haam, S.J.; Kim, D.H. Comparison of the McGrath videolaryngoscope and the Macintosh laryngoscope for double lumen endobronchial tube intubation in patients with manual in-line stabilization: A randomized controlled trial. Medicine (Baltimore) 2018, 97, e0081. [Google Scholar] [CrossRef]
- Huang, P.; Zhou, R.; Lu, Z.; Hang, Y.; Wang, S.; Huang, Z. GlideScope® versus C-MAC®(D) videolaryngoscope versus Macintosh laryngoscope for double lumen endotracheal intubation in patients with predicted normal airways: a randomized, controlled, prospective trial. BMC. Anesthesiol. 2020, 20, 119. [Google Scholar] [CrossRef]
- Rajagopal, S.; Gardner, R.N.; Swanson, E.; Kim, S.; Sondekoppam, R.; Ueda, K.; Hanada, S. Comparison of time to intubation of a double-lumen endobronchial tube utilizing C-MAC® versus GlideScope® versus Macintosh blade: A randomized crossover manikin study. Cureus 2023, 15, e50523. [Google Scholar] [CrossRef] [PubMed]
- Yao, W.; Li, M.; Zhang, C.; Luo, A. Recent advances in videolaryngoscopy for one-lung ventilation in thoracic anesthesia: A narrative review. Front. Med. (Lausanne) 2022, 9, 822646. [Google Scholar] [CrossRef] [PubMed]
- Maracaja, L.; Coffield, A.; Smith, L.D.; Bradshaw, J.D.; Saha, A.K.; McLauglin, C.S.; Templeton, T.W. A novel combined approach to placement of a double lumen endobronchial tube using a video laryngoscope and fiberoptic bronchoscope: a retrospective chart review. BMC. Anesthesiol. 2024, 24, 142. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Kim, J.A.; Ahn, H.J.; Choi, J.W.; Kim, D.K.; Cho, E.A. Double-lumen tube tracheal intubation using a rigid video-stylet: a randomized controlled comparison with the Macintosh laryngoscope. Br. J. Anaesth. 2013, 111, 990–995. [Google Scholar] [CrossRef]
- Seo, H.; Lee, G.; Ha, S.I.; Song, J.G. An awake double lumen endotracheal tube intubation using the Clarus video system in a patient with an epiglottic cyst: a case report. Korean J. Anesthesiol. 2014, 66, 157–159. [Google Scholar] [CrossRef]
- Xu, T.; Li, M.; Guo, X.Y. Comparison of Shikani optical stylet and Macintosh laryngoscope for double-lumen endotracheal tube intubation. Beijing Da Xue Xue Bao Yi Xue Ban (in Chinese) 2015, 47, 853–857. [Google Scholar] [PubMed]
- Gu, Y.; Zhou, Q.; Zhou, H.; Liu, M.; Feng, D.; Wei, J.; Min, K.; Zhu, W.; Chen, Y.; Lv, X. A randomized study of rigid video stylet versus Macintosh laryngoscope for double-lumen endobronchial tube intubation assistance in thoracoscopic pulmonary surgery. J. Clin. Med. 2023, 12, 540. [Google Scholar] [CrossRef]
- Lingappan, K.; Neveln, N.; Arnold, J.L.; Fernandes, C.J.; Pammi, M. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in neonates. Cochrane Database Syst. Rev. 2023, 5, CD009975. [Google Scholar] [CrossRef]
- Stein, M.L.; Sarmiento Argüello, L.A.; Staffa, S.J.; Heunis, J.; Egbuta, C.; Flynn, S.G.; Khan, S.A.; Sabato, S.; Taicher, B.M.; Chiao, F.; Bosenberg, A.; Lee, A.C.; Adams, H.D.; von Ungern-Sternberg, B.S.; Park, R.S.; Peyton, J.M.; Olomu, P.N.; Hunyady, A.I.; Garcia-Marcinkiewicz, A.; Fiadjoe, J.E.; Kovatsis, P.G.; PeDI Collaborative Investigators. Airway management in the paediatric difficult intubation registry: a propensity score matched analysis of outcomes over time. EClinicalMedicine 2024, 69, 102461. [Google Scholar] [CrossRef]
- Riveros, R.; Sung, W.; Sessler, D.I.; Sanchez, I.P.; Mendoza, M.L.; Mascha, E.J.; Niezgoda, J. Comparison of the Truview PCD™ and the GlideScope(®) video laryngoscopes with direct laryngoscopy in pediatric patients: a randomized trial. Can. J. Anaesth. 2013, 60, 450–457. [Google Scholar] [CrossRef]
- Sun, Y.; Lu, Y.; Huang, Y.; Jiang, H. Pediatric video laryngoscope versus direct laryngoscope: a meta-analysis of randomized controlled trials. Paediatr. Anaesth. 2014, 24, 1056–1065. [Google Scholar] [CrossRef]
- Takeuchi, R.; Hoshijima, H.; Mihara, T.; Kokubu, S.; Sato-Boku, A.; Nagumo, T.; Mieda, T.; Shiga, T.; Mizuta, K. Comparison of indirect and direct laryngoscopes in pediatric patients with a difficult airway: A systematic review and meta-analysis. Children (Basel) 2023, 11, 60. [Google Scholar] [CrossRef]
- Garcia-Marcinkiewicz, A.G.; Kovatsis, P.G.; Hunyady, A.I.; Olomu, P.N.; Zhang, B.; Sathyamoorthy, M.; Gonzalez, A.; Kanmanthreddy, S.; Gálvez, J.A.; Franz, A.M.; Peyton, J.; Park, R.; Kiss, E.E.; Sommerfield, D.; Griffis, H.; Nishisaki, A.; von Ungern-Sternberg, B.S.; Nadkarni, V.M.; McGowan, F.X. Jr.; Fiadjoe, J.E.; PeDI Collaborative investigators. First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial. Lancet 2020, 396, 1905–1913. [Google Scholar] [CrossRef]
- Riva, T.; Engelhardt, T.; Basciani, R.; Bonfiglio, R.; Cools, E.; Fuchs, A.; Garcia-Marcinkiewicz, A.G.; Greif, R.; Habre, W.; Huber, M.; Petre, M.A.; von Ungern-Sternberg, B.S.; Sommerfield, D.; Theiler, L.; Disma, N. ; OPTIMISE Collaboration. Direct versus video laryngoscopy with standard blades for neonatal and infant tracheal intubation with supplemental oxygen: a multicentre, non-inferiority, randomised controlled trial. Lancet Child Adolesc. Health 2023, 7, 101–111. [Google Scholar] [CrossRef]
- Geraghty, L.E.; Dunne, E.A.; Ní Chathasaigh, C.M.; Vellinga, A.; Adams, N.C.; O'Currain, E.M.; McCarthy, L.K.; O'Donnell, C.P.F. Video versus direct laryngoscopy for urgent intubation of newborn infants. N. Engl. J. Med. 2024, 390, 1885–1894. [Google Scholar] [CrossRef] [PubMed]
- Pfitzner, L.; Cooper, M.G.; Ho, D. The Shikani Seeing StyletTM for difficult intubation in children: Initial experience. Anaesthesia and Intensive Care 2002, 30, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.H.; Chen, L.C.; Hsu, W.H.; Lin, T.Y.; Lee, M.; Lu, C.W. A Comparison of McGrath videolaryngoscope versus Macintosh laryngoscope for nasotracheal intubation: A systematic review and meta-analysis. J. Clin. Med. 2022, 11, 2499. [Google Scholar] [CrossRef] [PubMed]
- Amir, S.H.; Ali, Q.E.; Bansal, S. A comparative evaluation of video stylet and flexible fibre-optic bronchoscope in the performance of intubation in adult patients. Indian J. Anaesth. 2017, 61, 321–325. [Google Scholar] [CrossRef]
- Cheng, T.; Wang, L.K.; Wu, H.Y.; Yang, X.D.; Zhang, X.; Jiao, L. Shikani optical stylet for awake nasal intubation in patients undergoing head and neck surgery. Laryngoscope 2021, 131, 319–325. [Google Scholar] [CrossRef]
- Osman, Y.M.; Abd El-Aziz, R.A.E.R. Effectiveness of C-MAC video-stylet versus C-MAC D-blade video-laryngoscope for tracheal intubation in patients with predicted difficult airway: Randomized comparative study. Egyptian J. Anaesthesia 2023, 39, 233–240. [Google Scholar] [CrossRef]
- Lee, M.C.; Tseng, K.Y.; Shen, Y.C.; Lin, C.H.; Hsu, C.W.; Hsu, H.J.; Lu, I.C.; Cheng, K.I. Nasotracheal intubation in patients with limited mouth opening: a comparison between fibreoptic intubation and the Trachway®. Anaesthesia 2016, 71, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Ou, S.Y.; Kuo, Y.T.; Chia, Y.Y. Randomized, active-controlled, parallel-group clinical study assessing the efficacy and safety of FKScope® for nasotracheal intubation in patients scheduled for oral and maxillofacial surgery under general anesthesia. Asian J. Anesthesiol. 2021, 59, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.K.; Zhang, X.; Wu, H.Y.; Cheng, T.; Xiong, G.L.; Yang, X.D. Impact of choice of nostril on nasotracheal intubation when using video rigid stylet: a randomized clinical trial. BMC. Anesthesiol. 2022, 22, 360. [Google Scholar] [CrossRef] [PubMed]
- McCauley, P.; Moore, M.; Duggan, E. Anaesthesia for reconstructive free flap surgery for head and neck cancer. Br. J. Hosp. Med. (Lond). 2022, 83, 1–9. [Google Scholar] [CrossRef]
- Yokogawa, F.; Oe, K.; Hosokawa, M.; Masui, K. Lateral position for difficult intubation in a patient with history of hemiglossectomy and flap reconstruction: a case report. JA. Clin. Rep. 2022, 8, 16. [Google Scholar] [CrossRef]
- Nagarkar, R.; Kokane, G.; Wagh, A.; Kulkarni, N.; Roy, S.; Tandale, R.; Pawar, S. Airway management techniques in head and neck cancer surgeries: a retrospective analysis. Oral Maxillofac. Surg. 2019, 23, 311–315. [Google Scholar] [CrossRef]
- Shah, S.V.; Chaggar, R.S. Advanced airway management techniques in anaesthesia for oral cancer surgery: a review. J. Oral Maxillofac. Anesth. 2023, 2, 8. [Google Scholar] [CrossRef]
- Zheng, G.; Feng, L.; Lewis, C.M. A data review of airway management in patients with oral cavity or oropharyngeal cancer: a single-institution experience. BMC. Anesthesiol. 2019, 19, 92. [Google Scholar] [CrossRef]
- Hofmeyr, R.; Llewellyn, R.; Fagan, J.J. Multidisciplinary difficult airway challenges: Perioperative management of glottic and supraglottic tumors. Oper. Tech. Otolaryngol. Head Neck Surg. 2020, 31, 120–127. [Google Scholar] [CrossRef]
- Jeong, H.W.; Song, E.J.; Jang, E.A.; Kim, J. Managing a difficult airway due to supraglottic masses: successful videolaryngoscopic intubation after induction of general anesthesia. Perioper. Med. (Lond). 2024, 13, 21. [Google Scholar] [CrossRef]
- Yang, D.; Li, S.; Lan, J.; Ye, S.; Zhang, L. Use of the Disposcope endoscope for awake orotracheal intubation in an elderly patient with a large vocal cord polyp -a case report. Korean J. Anesthesiol. 2024, 77, 392–396. [Google Scholar] [CrossRef]
- McElwain, J.; Malik, M.A.; Harte, B.H.; Flynn, N.M.; Laffey, J.G. Comparison of the C-MAC videolaryngoscope with the Macintosh, Glidescope, and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia 2010, 65, 483–489. [Google Scholar] [CrossRef]
- Maartens, T.; de Waal,B. A comparison of direct laryngoscopy to video laryngoscopy by paramedic students in manikin-simulated airway management scenarios. Afr. J. Emerg. Med. 2017, 7, 183–188. [Google Scholar] [CrossRef]
- Yong, S.A.; Chaou, C.H.; Yu, S.R.; Kuan, J.T.; Lin, C.C.; Liu, H.P.; Chiu, T.F. Video assisted laryngoscope facilitates intubation skill learning in the emergency department. J. Acute Med. 2020, 10, 60–69. [Google Scholar] [CrossRef]
- Ghotbaldinian, E.; Dehdari, N.; Åkeson, J. Maintenance of basic endotracheal intubation skills with direct or video-assisted laryngoscopy: A randomized crossover follow-up study in inexperienced operators. AEM. Educ. Train. 2021, 5, e10655. [Google Scholar] [CrossRef]
- Pujari, V.S.; Thiyagarajan, B.; Annamalai, A.; Bevinaguddaiah, Y.; Manjunath, A.C.; Parate, L.H. A comparative study in airway novices using King Vision videolaryngoscope and conventional Macintosh direct laryngoscope for endotracheal intubation. Anesth. Essays Res. 2021, 15, 57–61. [Google Scholar] [CrossRef]
- Yi, I.K.; Hwang, J.; Min, S.K.; Lim, G.M.; Chae, Y.J. Comparison of learning direct laryngoscopy using a McGrath videolaryngoscope as a direct versus indirect laryngoscope: a randomized controlled trial. J. Int. Med. Res. 2021, 49, 3000605211016740. [Google Scholar] [CrossRef] [PubMed]
- Nalubola, S.; Jin, E.; Drugge, E.D.; Weber, G.; Abramowicz, A.E. Video versus direct laryngoscopy in novice intubators: A systematic review and meta-analysis. Cureus 2022, 14, e29578. [Google Scholar] [CrossRef] [PubMed]
- Malito, M.L.; Mathias, L.A.D.S.T.; Kimura Junior, A.; Correa, G.H.; Bardauil, V.R. The impact of introducing a videolaryngoscope in the initial training of laryngoscopy for undergraduate medical students: a simulation randomized trial. Braz. J. Anesthesiol. 2023, 73, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Tseng, K.Y.; Chau, S.W.; Su, M.P.; Shih, C.K.; Lu, I.C.; Cheng, K.I. A comparison of Trachway intubating stylet and Airway Scope for tracheal intubation by novice operators: a manikin study. Kaohsiung J. Med. Sci. 2012, 28, 448–451. [Google Scholar] [CrossRef]
- Hung, K.C.; Tan, P.H.; Lin, V.C.; Wang, H.K.; Chen, H.S. A comparison of the Trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J. Anesth. 2013, 27, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.; Lee, C.L.; Huang, S.J.; Shyr, M.H. Comparison between the Trachway video intubating stylet and Macintosh laryngoscope in four simulated difficult tracheal intubations: A manikin study. Tzu Chi Med. J. 2016, 28, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Pius, J.; Noppens, R.R. Learning curve and performance in simulated difficult airway for the novel C-MAC® video-stylet and C-MAC® Macintosh video laryngoscope: A prospective randomized manikin trial. PLoS. One 2020, 15, e0242154. [Google Scholar] [CrossRef] [PubMed]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation: a Cochrane systematic review and meta-analysis update. Br. J. Anaesth. 2022, 129, 612–623. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, M.; Greif, R.; Schoettker, P.; Savoldelli, G.L.; Nabecker, S.; Theiler, L.G. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: a multicentre randomized controlled trial. Br. J. Anaesth. 2016, 116, 670–679. [Google Scholar] [CrossRef]
- Zhang, K.; Zhong, C.; Lou, Y.; Fan, Y.; Zhen, N.; Huang, T.; Chen, C.; Shan, H.; Du, L.; Wang, Y.; Cui, W.; Cao, L.; Tian, B.; Zhang, G. Video laryngoscopy may improve the intubation outcomes in critically ill patients: a systematic review and meta-analysis of randomised controlled trials. Emerg. Med. J. 2023, emermed-2023-213860. [Google Scholar] [CrossRef]
- Azam, S.; Khan, Z.Z.; Shahbaz, H.; Siddiqui, A.; Masood, N.; Anum Arif, Y.; Memon, Z.U.; Khawar, M.H.; Siddiqui, F.F.; Azam, F.; Goyal, A. Video versus direct laryngoscopy for intubation: Updated systematic review and meta-analysis. Cureus 2024, 16, e51720. [Google Scholar] [CrossRef]
- De Jong, A.; Sfara, T.; Pouzeratte, Y.; Pensier, J.; Rolle, A.; Chanques, G.; Jaber, S. Videolaryngoscopy as a first-intention technique for tracheal intubation in unselected surgical patients: a before and after observational study. Br. J. Anaesth. 2022, 129, 624–634. [Google Scholar] [CrossRef]
- Cook, T.M.; Aziz, M.F. Has the time really come for universal videolaryngoscopy? Br. J. Anaesth. 2022, 129, 474–477. [Google Scholar] [CrossRef]
- Lyons, C.; Harte, B.H. Universal videolaryngoscopy: take care when crossing the Rubicon. Anaesthesia 2023, 78, 688–691. [Google Scholar] [CrossRef]
- Mirrakhimov, A.E.; Torgeson, E. Use of videolaryngoscopy as the first option for all tracheal intubations: not so fast. Comment on Br. J. Anaesth. 2022; 129: 624-634. Br. J. Anaesth. 2023, 130, e12–e13. [Google Scholar] [CrossRef] [PubMed]
- Webb, A.; Kolawole, H.; Leong, S.; Loughnan, T.E.; Crofts, T.; Bowden, C. Comparison of the Bonfils and Levitan optical stylets for tracheal intubation: a clinical study. Anaesth. Intensive Care 2011, 39, 1093–1097. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.H.; Luk, H.N.; Qu, J.Z.; Shikani, A. An approach to improve the effectiveness of the video-assisted intubating stylet technique for tracheal intubation: A case series report. Healthcare (Basel) 2023, 11, 891. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; Onwochei, D.N.; Muldoon, S.; Keane, O.; El-Boghdadly, K. Airway management research: a systematic review. Anaesthesia 2019, 74, 225–236. [Google Scholar] [CrossRef]
- Ward, P.A.; Irwin, M.G. Man vs. manikin revisited - the ethical boundaries of simulating difficult airways in patients. Anaesthesia 2016, 71, 1399–1403. [Google Scholar] [CrossRef]
- Theiler, L.; Greif, R.; Bütikofer, L.; Arheart, K.; Kleine-Brueggeney, M. The skill of tracheal intubation with rigid scopes - a randomised controlled trial comparing learning curves in 740 intubations. BMC. Anesthesiol. 2020, 20, 263. [Google Scholar] [CrossRef]
- Oh, S.H.; Heo, S.K.; Cheon, S.U.; Ryu, S.A. The effects of backward, upward, rightward pressure maneuver for intubation using the OptiscopeTM: a retrospective study. Anesth. Pain Med. (Seoul) 2021, 16, 391–397. [Google Scholar] [CrossRef]
- Weng, L.; Yu, B.; Ding, L.; Shi, M.; Wang, T.; Li, Z.; Qiu, W.; Lin, X.; Lin, B.; Gao, Y. Visual rigid laryngoscopy versus video laryngoscopy for endotracheal intubation in elderly patients: A randomized controlled trial. PLoS. One 2024, 19, e0309516. [Google Scholar] [CrossRef]




| 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Total anesthesia number | 16077 | 17831 | 17998 | 19307 | 19721 | 19244 | 19765 | 22438 | 25046 | |
| GA number | 15339 | 16893 | 17497 | 18481 | 19009 | 18574 | 19061 | 22099 | 24368 | |
| LMA-GA number | 5544 | 5134 | 5816 | 5902 | 5863 | 5714 | 4932 | 5763 | 6585 | |
| ET-GA number | 5953 | 6504 | 6920 | 6966 | 7418 | 6982 | 7602 | 8329 | 8889 | |
| VL | 0 | 0 | 20 | 100 | 635 | 336 | 305 | 280 | 350 | |
| Styletubation | 5953 | 6504 | 6900 | 6866 | 6783 | 6646 | 7297 | 8049 | 8539 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





