Introduction
Fine needle aspiration cytology (FNAC) is a widely accepted, cost-effective, and minimally invasive diagnostic technique for evaluating various lesions in the head and neck region. It allows rapid preliminary diagnosis, facilitating early and appropriate clinical management without the need for more invasive procedures [
1,
2]
.
In most settings, FNAC plays a critical role in the preoperative assessment of cervical lymphadenopathy, salivary gland tumors, and other neck masses. Its ability to distinguish benign from malignant processes has made it an essential tool in both resource-rich and resource-limited environments [
3,
4]
. However, in Somalia, data on FNAC utilization and its diagnostic performance are lacking, despite a growing burden of cancer and neck lesions [
5,
6]
.
Over the past two decades, FNAC has become integral to head and neck lesion diagnosis globally, but no cytopathological correlation studies have yet been published from Somalia. A recent report by Tahtabasi et al. noted lymphomas, nasopharyngeal carcinoma, and salivary gland tumors among the most common head and neck cancers in the country [
6], further underscoring the need for reliable diagnostic tools.
This study presents the first report from Somalia comparing FNAC and histopathology in non-thyroidal head and neck lesions. This study aims to evaluate the accuracy, sensitivity, specificity, and predictive values of FNAC, emphasizing its diagnostic value in low-resource settings where advanced diagnostics like immunohistochemistry (IHC) and flow cytometry are often unavailable.
Methods
Study Design and Setting
This retrospective study was conducted at Mogadishu Somalia Türkiye Recep Tayyip Erdoğan Training and Research Hospital, pathology laboratory, a tertiary care center. The study period extended from January 2018 to December 2022, encompassing all patients who underwent both fine needle aspiration cytology (FNAC) and subsequent histopathological examination of non-thyroidal head and neck lesions. Data were collected over a five-year period from the hospital’s electronic health information system (HIS). Ethical approval was obtained from the hospital’s Ethical Research Committee (Ref No: 10520), and informed consent was secured from all participants or their legal guardians. A total of 265 cases were identified and included in the analysis.
Inclusion and Exclusion Criteria
Patients of all age groups and both sexes with head and neck masses (excluding thyroid lesions) who had both FNAC and histopathological evaluation were included. Cases lacking subsequent histopathological confirmation or with inadequate FNAC samples were excluded.
FNAC and Histopathology Procedures
Ultrasound-guided FNAC was performed using 23-gauge needles and 5 mL disposable syringes. Smears were prepared on six glass slides per case. Air-dried smears were stained with May-Grünwald-Giemsa, and alcohol-fixed smears were stained using Papanicolaou or hematoxylin and eosin (H&E). All FNAC procedures were performed by an interventional radiologist.
Histopathological specimens were obtained through surgical excision or core needle biopsies and were fixed in 10% buffered formalin. Routine H&E staining was used for histological evaluation. No ancillary techniques such as immunocytochemistry or flow cytometry were available in the institutional laboratory.
Pathologist Review
Cytopathology slides were initially reported independently by one pathologist, while histopathology slides were reviewed independently by another pathologist on a monthly basis. Cases identified as malignant, suspicious, or diagnostically challenging were subsequently evaluated jointly by both pathologists. In instances of diagnostic uncertainty or discordance, a third senior pathologist conducted a final review. Inter-observer agreement was formally assessed to evaluate diagnostic concordance.
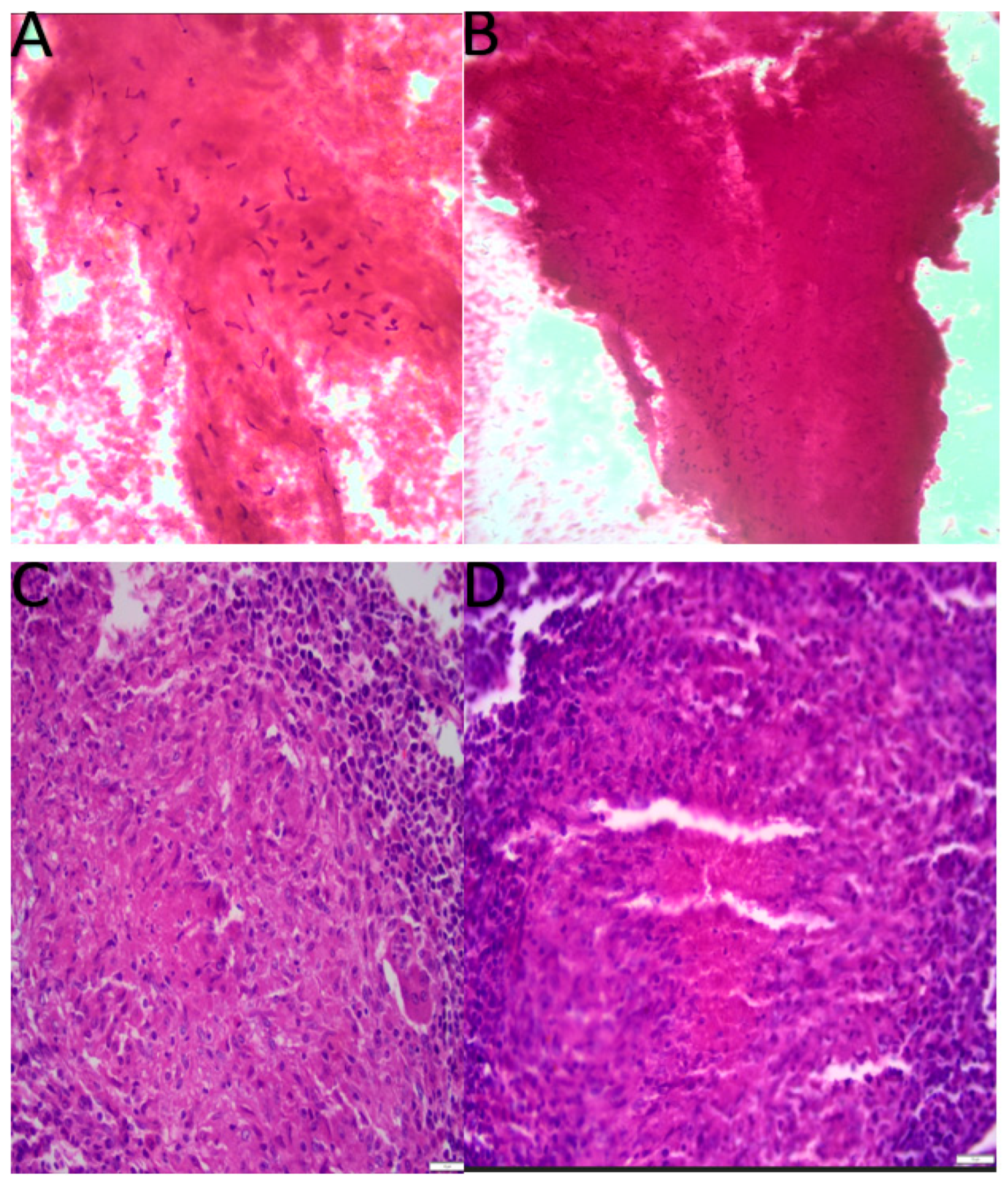
Tuberculosis was diagnosed based on classical cyto-morphologic features, granulomatous inflammation with caseous necrosis (
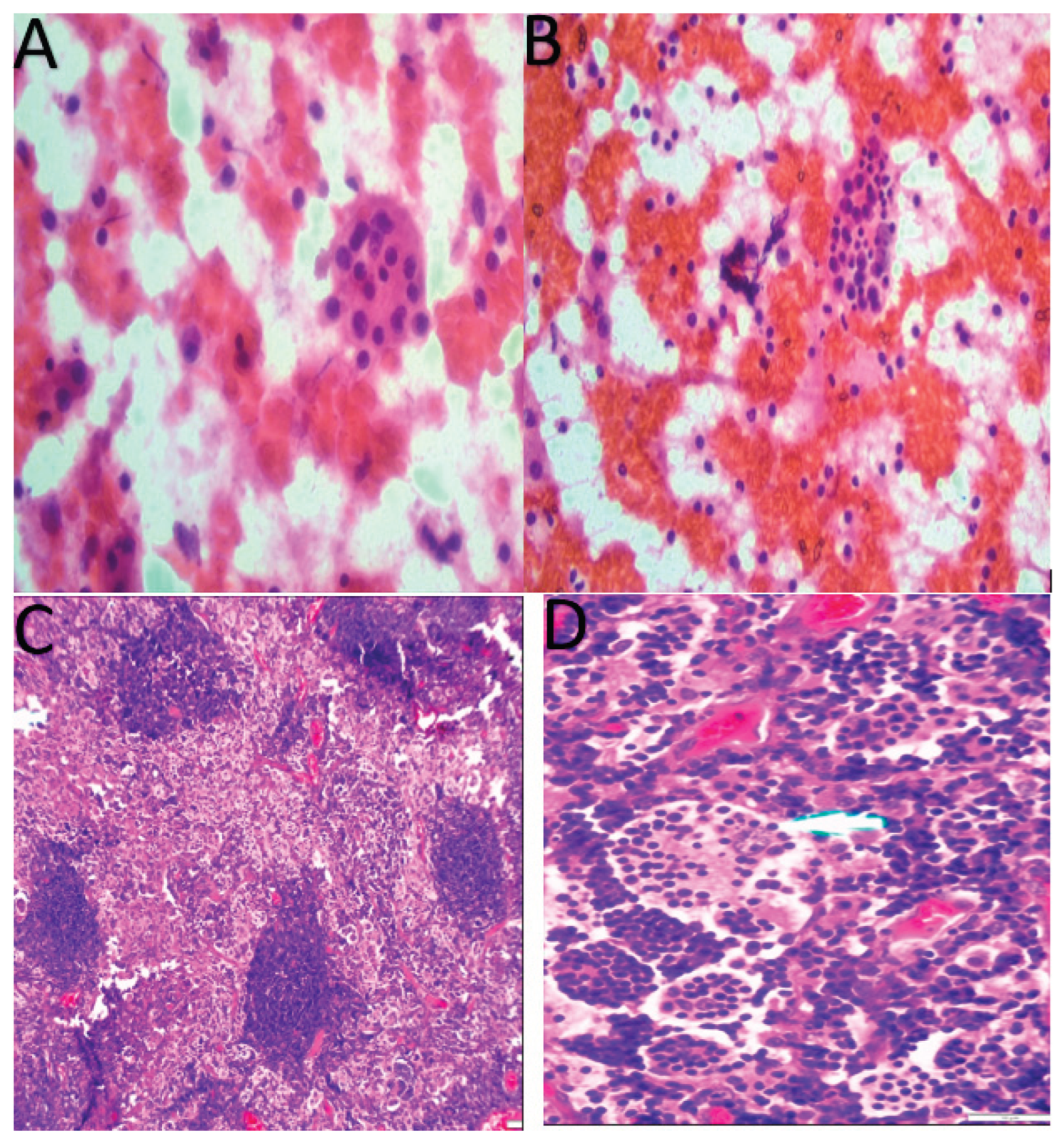
Figure 2), and supported by strong clinical and radiological correlation. Ziehl-Neelsen staining was unavailable during the study period. In the absence of ancillary diagnostic techniques such as microbiological confirmation (e.g., Ziehl-Neelsen staining), the accuracy of such diagnoses remains limited. Rare conditions such as Rosai-Dorfman disease were diagnosed using classic Cyto-histomorphologic findings (
Figure 3) and clinical correlation, with the absence of IHC acknowledged as a limitation. But Castleman disease was initially interpreted as benign lymphoid proliferations on cytology; however, subsequent histopathological examination confirmed the diagnosis of Castleman disease, demonstrating cyto-histological concordance.
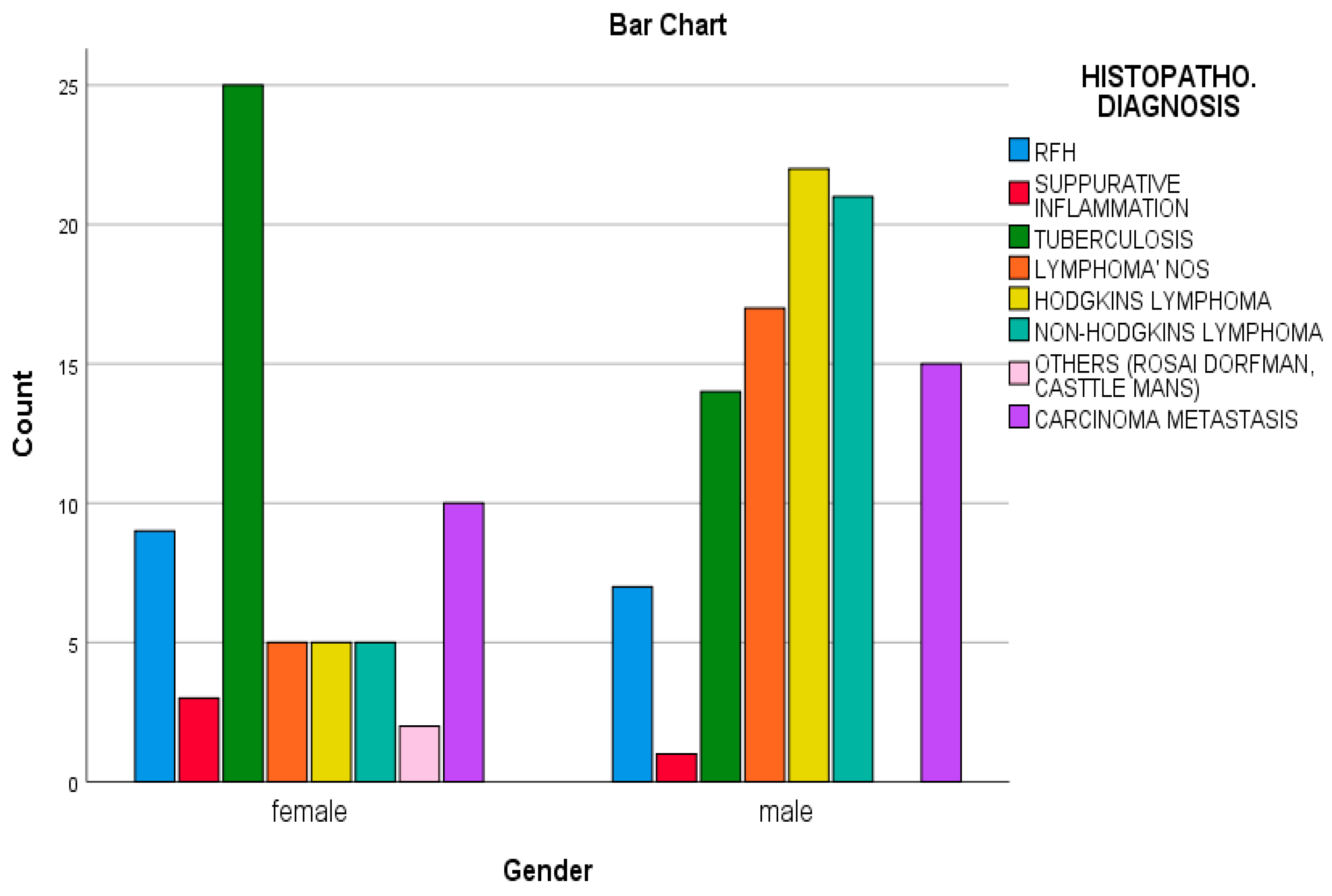
Figure 1.
Lymphnode lesions according to frequency, diagnosis, and gender distributions.
Figure 1.
Lymphnode lesions according to frequency, diagnosis, and gender distributions.
Figure 2.
Cytological and histopathological features of tuberculous lymphadenitis. (A, B) Fine needle aspiration cytology (FNAC) smears stained with H&E stain showing numerous necrotizing granulomatous inflammation. (C, D) Corresponding histopathological sections stained with hematoxylin and eosin (H&E) demonstrating granulomatous inflammation with epithelioid histiocytes, Langhans giant cells, and central caseous necrosis characteristic of tuberculosis.
Figure 2.
Cytological and histopathological features of tuberculous lymphadenitis. (A, B) Fine needle aspiration cytology (FNAC) smears stained with H&E stain showing numerous necrotizing granulomatous inflammation. (C, D) Corresponding histopathological sections stained with hematoxylin and eosin (H&E) demonstrating granulomatous inflammation with epithelioid histiocytes, Langhans giant cells, and central caseous necrosis characteristic of tuberculosis.
Figure 3.
Cytological and histopathological features of Rosai-Dorfman disease. (A, B) Fine needle aspiration cytology (FNAC) smears showing numerous large histiocytes with abundant pale cytoplasm exhibiting emperipolesis- engulfment of intact lymphocytes and plasma cells (H&E stain, high magnification). (C, D) Hematoxylin and eosin (H&E) stained lymph node sections reveal dilated sinuses filled with large histiocytes demonstrating prominent emperipolesis, surrounded by a mixed inflammatory infiltrate composed of lymphocytes and plasma cells, features characteristic of Rosai-Dorfman disease.
Figure 3.
Cytological and histopathological features of Rosai-Dorfman disease. (A, B) Fine needle aspiration cytology (FNAC) smears showing numerous large histiocytes with abundant pale cytoplasm exhibiting emperipolesis- engulfment of intact lymphocytes and plasma cells (H&E stain, high magnification). (C, D) Hematoxylin and eosin (H&E) stained lymph node sections reveal dilated sinuses filled with large histiocytes demonstrating prominent emperipolesis, surrounded by a mixed inflammatory infiltrate composed of lymphocytes and plasma cells, features characteristic of Rosai-Dorfman disease.
Surgical excision in lymphoma cases was performed mainly for diagnostic excision biopsy, not as therapeutic intervention, as FNAC was insufficient for definitive subtyping due to lack of IHC. Similarly, in nasopharyngeal carcinoma, surgical biopsies were done for diagnostic confirmation, not resection
The diagnostic accuracy of FNAC was assessed using histology as the gold standard. FNACs classified as suspicious or malignant were considered true positives (TP) if histological examination confirmed malignancy, and false positives (FP) if histology was negative for malignancy. Benign FNAC results were considered true negatives (TN) when histology also revealed benign findings, and false negatives (FN) when histological examination revealed malignancy despite benign FNAC findings.
The FNAC diagnoses of lymph nodes were categorized into eight groups: (I) benign, (II) reactive follicular hyperplasia (RFH), (III) suppurative inflammation, (IV) tuberculosis lymphadenitis, (V) suspicious for lymphoma/ lymphoma, (VI) malignant, and (VII) carcinoma metastasis.
Lymph node FNAC results were categorized using a local classification based on morphologic patterns. The Sydney System and WHO guidelines for lymph node cytopathology were not applied, as they were published after the study period and only became routinely implemented in our setting following 2024. This limitation has been acknowledged accordingly.
Salivary gland FNAC diagnoses were categorized into six groups according to the Milan System for Reporting Salivary Gland Cytopathology: (I) non-diagnostic, (II) non-neoplastic, (III) atypia of undetermined significance, (IV) neoplasm, which is further subdivided into: (IVA) benign neoplasm, (IVB) salivary gland neoplasm of uncertain malignant potential (SUMP), (V) suspicious for malignancy, and (VI) malignant.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., Armonk, NY, USA). Continuous variables such as age were presented as mean ± standard deviation (SD). Categorical variables, including sex and diagnostic categories, were summarized as frequencies and percentages. A p-value < 0.05 was considered statistically significant.
Results
A total of 265 patients with non-thyroidal head and neck masses who underwent both fine needle aspiration cytology (FNAC) and subsequent histopathological examination over a five-year period were included in this study. Patient ages ranged from 1 month to 90 years, with a median age of 41 years. Lymph node and salivary gland lesions were more frequently observed in individuals aged 10 to 25 years, whereas soft tissue masses and cystic lesions were predominantly seen in patients aged 25 to 40 years.
There was a male predominance, with 145 males (54.7%) and 120 females (45.3%), resulting in a male-to-female ratio of 1.2:1. The highest gender disparity was seen in lymph node lesions (male-to-female ratio of 1.5:1), while salivary gland lesions showed a female predominance (male-to-female ratio of 1:1.2).
Overall, 161 cases (60.8%) originated from lymph nodes (including anterior/posterior cervical, submental, and supraclavicular regions), followed by 96 cases (36.2%) involving salivary glands (parotid, submandibular, and minor salivary glands), and 8 cases (3.0%) consisting of cystic and soft tissue lesions. Anatomic distribution and diagnostic performance by lesion site are summarized in (
Table 1)
.
Among the 161 lymph node lesions, lymphoma was the most frequent histological diagnosis, observed in 46.6% (n = 75) of cases. This was followed by tuberculosis (24.2%, n = 39), metastatic carcinoma (15.5%, n = 25), reactive lymphadenitis (9.9%, n = 16), and suppurative inflammation (2.5%, n = 4). Two rare cases were diagnosed as Rosai-Dorfman disease and Castleman’s disease. (
Figure 2,
Figure 3)
Hodgkin lymphoma accounted for 36% (n = 27) of all lymphomas, while non-Hodgkin lymphoma represented 34.6% (n = 26). The remaining 29.3% (n = 22) could not be subclassified due to the unavailability of immunohistochemical markers.
Among the 25 cases of metastatic carcinoma, the most common primary was undifferentiated nasopharyngeal carcinoma (64%, n = 16), followed by thyroid carcinoma (16%, n = 4), tongue carcinoma (8%, n = 2), and three cases of cutaneous squamous cell carcinoma, melanoma, and undifferentiated carcinoma.
The diagnostic sensitivity, specificity, and accuracy for lymph node FNAC were 99%, 91.3%, and 97.6%, respectively (
Table 2,
Figure 1).
Among the 96 salivary gland lesions, the most common diagnosis was pleomorphic adenoma (73%, n = 70), followed by mucoepidermoid carcinoma (5.2%, n = 5). FNAC showed excellent correlation with histopathology, with a sensitivity of 92.3%, specificity of 98.8%
, and overall diagnostic accuracy of 98% (
Table 3).
Among the eight cystic and soft tissue lesions, diagnoses included thyroglossal cyst, branchial cleft cyst, epidermoid cyst, immature teratoma, and lipoma, all of which showed complete cyto-histological concordance.
The overall diagnostic performance of FNAC for all non-thyroidal head and neck lesions demonstrated a sensitivity of 97.1%
, specificity of 96.7%
, accuracy of 98.5%, positive predictive value of 96.3%, and negative predictive value of 98.3%. The false-negative rate and false-positive rate were 3.5% and 1.7%, respectively (
Table 4).
Discussion
Head and neck masses represent one of the most common clinical presentations encountered in daily practice. Given their broad differential diagnoses, including congenital cysts, inflammatory conditions, primary neoplasms, and metastatic tumors, an accurate and timely diagnosis is critical for guiding appropriate management strategies [
5]. Fine needle aspiration cytology (FNAC) remains a cornerstone diagnostic tool in the evaluation of such lesions, particularly due to its minimally invasive nature, cost-effectiveness, and rapid turnaround time [
1,
5].
To date, there have been no previously published studies from Somalia examining the cyto-histological correlation of non-thyroidal head and neck lesions. This study represents the first report from the region to evaluate the diagnostic accuracy of FNAC in these lesions. Our findings underscore FNAC’s utility by demonstrating high sensitivity, specificity, and overall diagnostic accuracy.
According to affected organs, an initial report of 1306 cancer cases regarding the distribution of cancer cases in Somalia reported that lymph node was the 11th most common cancer overall, while nasopharyngeal and salivary gland malignancies ranked 13th and 18th, respectively. Lymphomas were the sixth most common cancer among males in that report [
6]. Our study adds to this epidemiological context by showing that lymph node lesions were the most frequently sampled non-thyroidal head and neck mass in our cohort.
In a study from India, Patel et al. reported that head and neck cancers represent a substantial proportion of all malignancies, accounting for approximately 23% in males, 6% in females, and 5% of all childhood cancers [
7]. These rates are notably different than those reported in Somalia by Tahtabasi et al., where head and neck cancers accounted for 11.4% of all cancers in males, 9% in females, and 9.7% among pediatric malignancies [
6].
The gender distribution revealed a male predominance, with a male-to-female ratio of 1.2:1, which is consistent with earlier studies [
8,
9]. Lymph node lesions were also more common among males (1.5:1), whereas salivary gland lesions exhibited a slight female predominance. The most frequent diagnosis among lymph node lesions was lymphoma (46.6%), followed by tuberculosis (24.2%) and metastatic carcinoma (15.5%).
Our lymphoma findings are consistent with results reported by Nasreen et al., who found that 49.7% of malignant lymphadenopathies were lymphomas [
10]. In their study, non-Hodgkin lymphoma was more common than Hodgkin lymphoma (38.4% vs. 11.5%), whereas our study found a similar pattern of Hodgkin (36%) and non-Hodgkin (34.6%) lymphoma. In contrast, studies from Shahid et al. and Pathak et al. reported much lower lymphoma rates (less than 10%) and higher rates of reactive lymphadenitis, followed by metastatic carcinoma and tuberculosis [
11,
12]. Agrawal et al. also reported that 25% of lymph node lesions were tuberculous lymphadenitis, a figure comparable to our findings [
13].
In our study, FNAC achieved high diagnostic accuracy in lymph node lesions, with sensitivity, specificity, and accuracy of 99%, 91.3%, and 97.6%, respectively. These rates are higher than those reported by Nasreen et al., who found a sensitivity of 90.9% and specificity of 67.2% [
10]. FNAC demonstrated high accuracy, with sensitivity ranging from 92.3% (salivary gland) to 99% (lymph node). The diagnostic limitations in lymphomas were largely due to the unavailability of immunohistochemistry, which is essential for precise subtyping.
For salivary gland lesions, more than 85% were benign, with pleomorphic adenoma being the most common diagnosis 73%. This is consistent with the findings of Khetrapal et al., who also identified pleomorphic adenoma and chronic sialadenitis as the predominant diagnoses [
14]. FNAC performance in salivary gland lesions was also high in our study, with sensitivity, specificity, and accuracy of 92.3%, 98.8%, and 98%, respectively.
Cystic and soft tissue lesions represented only 3.0% of cases, a proportion that aligns with findings from Bhasker et al., who reported miscellaneous neck lesions in 5.1% of cases [
15].
Overall, FNAC showed a sensitivity of 97.1%, specificity of 96.7%, and diagnostic accuracy of 98.3% across all non-thyroidal head and neck lesions. Tandon et al. reported a higher specificity (98.5%), while Poorey and Rammeh reported lower specificity values of 95% and 94.4%, respectively [
5,
9]. When evaluating FNAC’s diagnostic performance, sensitivity is particularly critical, as a false-negative result can delay necessary treatment or further investigations.
In our cohort, 151 of the 265 lesions were benign, highlighting FNAC’s critical role in avoiding unnecessary surgical interventions. Our findings reinforce FNAC’s role as a safe, inexpensive, rapid, and accurate first-line diagnostic tool in the evaluation of head and neck lesions. Despite being operator-dependent, FNAC continues to gain universal acceptance due to its diagnostic reliability and clinical utility.
Study Limitations
This study has several limitations. First, it was a retrospective, single-center study with a modest sample size. A number of FNAC cases without corresponding histopathology were excluded. First, the retrospective and single-center design, along with the modest sample size, may limit the generalizability of the results. Second, the dataset lacked information on risk factors such as occupational exposures and radiation history. Third, the classification of lymph node cytology did not follow standardized systems such as the Sydney or WHO guidelines, which were introduced after the study period and are only recently being adopted in our setting. Fourth, the absence of ancillary diagnostic tools, including immunohistochemistry and Ziehl-Neelsen staining, restricted definitive subtyping and microbiological confirmation, particularly in cases of lymphoma and tuberculosis. Finally, long-term clinical follow-up and outcome data were not available due to logistical and geographic challenges affecting patient tracking.
Nonetheless, this is the first Somali study to evaluate the cyto-histological correlation and diagnostic performance of FNAC in non-thyroidal head and neck lesions. It demonstrates FNAC’s value in a low-resource setting and establishes a foundation for future diagnostic standardization and quality improvement in cytopathology services in Somalia.
Conclusion
This study demonstrates a high degree of diagnostic accuracy and concordance between fine needle aspiration cytology (FNAC) and histopathology for non-thyroidal head and neck lesions in a low-resource setting. FNAC proved to be a reliable, rapid, and minimally invasive diagnostic tool, particularly effective in identifying benign and malignant lesions of the salivary glands and lymph nodes. However, its limitations in subtyping lymphomas and diagnosing rare entities without immunohistochemistry highlight the need for further development of pathology infrastructure in Somalia.
Author Contributions
All authors made substantial contributions to the conception and design of the work, acquisition, analysis, and interpretation of data; participated in drafting, revising, and critically reviewing the manuscript; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Review Board of Mogadishu Somalia Türkiye Recep Tayyip Erdogan Research and Training Hospital (Ref No: 10520). The study was conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all study participants. For participants under 18 years of age, consent was obtained from a parent or legal guardian.
Consent for publication
Not applicable.
Abbreviations
| RFH |
Reactive follicular hyperplasia |
| FNAC |
Fine needle aspiration cytology |
| AUS |
Atypia of undetermined significance |
| H&E |
Hematoxylin and eosin |
| Pap stain |
Papanicolaou stain |
| HPE |
Histopathological examination |
| PPV |
Positive predictive value |
| NPV |
Negative predictive value |
| FP |
False positive |
| FN |
False negative |
| TN |
True negative |
| TP |
True positive |
| SUMP |
Salivary gland neoplasm of uncertain malignant potential |
| PLGA |
Polymorphous low-grade adenocarcinoma |
References
- Abdullahi, I.M.; Yasin, N.A.; Dirken, E.S.; Mohamoud, A.M.; Guler, I.; Adani, A.A. Comparative study of fine needle aspiration cytology and histopathology in thyroid nodules at a tertiary care hospital: First report from Somalia. Asian J. Surg. 2022, 46, 4202–4207. [CrossRef]
- Iacob, A.; Zazgyva, A.; Ormenişan, A.; Mezei, T.; Sin, A.; Tilinca, M. Effectiveness of fine-needle aspiration cytology in the diagnosis of lateral cervical nonthyroid tumors. Medicine 2016, 95, e4448. [CrossRef]
- Rajbhandari, M.; Dhakal, P.; Shrestha, S.; Sharma, S.; Pokharel, M.; Shrestha, I.; Shrestha, B.; Makaju, R. The Correlation Between Fine Needle Aspiration Cytology and Histopathology of Head and Neck Lesions in Kathmandu University Hospital. Kathmandu Univ. Med J. 2015, 11, 296–299. [CrossRef]
- Fathima A, Tyagi S, Viswanatha B. The role of ultrasonography and fine needle aspiration cytology in the diagnosis of neck swellings—Our experience. Res Otolaryngol. 2019;8(1):1–5.
- Leoncini, E.; Ricciardi, W.; Cadoni, G.; Arzani, D.; Petrelli, L.; Paludetti, G.; Brennan, P.; Luce, D.; Stucker, I.; Matsuo, K.; et al. Adult height and head and neck cancer: a pooled analysis within the INHANCE Consortium. Eur. J. Epidemiology 2013, 29, 35–48. [CrossRef]
- Tahtabasi, M.; Abdullahi, I.M.; Kalayci, M.; Ibrahim, I.G.; Er, S. Cancer Incidence and Distribution at a Tertiary Care Hospital in Somalia from 2017 to 2020: An Initial Report of 1306 Cases. Cancer Manag. Res. 2020, ume 12, 8599–8611. [CrossRef]
- Patel, J.P.; Jansari, T.R.; Chauhan, A.P.; Jasani, J.H. Role of Fine Needle Aspiration Cytology in Assessment of Head and Neck Lesions - A Study at a Tertiary Care Centre. J. Evol. Med Dent. Sci. 2021, 10, 527–531. [CrossRef]
- SMS, J Ingin R, Geetanjali. Utility of cytology in head and neck pathology—a one year study. IP J Diagn Pathol Oncol. 2019;4(2):143–7.
- Rammeh, S.; Romdhane, E.; Sassi, A.; Belhajkacem, L.; Blel, A.; Ksentini, M.; Lahiani, R.; Farah, F.; Ben Salah, M.; Ferjaoui, M. Accuracy of fine-needle aspiration cytology of head and neck masses. Diagn. Cytopathol. 2018, 47, 394–399. [CrossRef]
- Hafez, N.H.; Tahoun, N.S. Reliability of fine needle aspiration cytology (FNAC) as a diagnostic tool in cases of cervical lymphadenopathy. J. Egypt. Natl. Cancer Inst. 2011, 23, 105–114. [CrossRef]
- Shahid F, Mirza T, Mustafa S, Sabahat S, Sharafat S. An experimental status of fine needle aspiration cytology of head and neck lesions in a tertiary care scenario. J Basic Appl Sci. 2010;6(2):159–62.
- Pathak, R.; Prasad, K.; Rauniyar, S.; Pudasaini, S.; Pande, K.; Koirala, S.; Kafle, S.; Jha, A.; Chalise, S.; Basnyat, A. Fine needle aspiration cytology of head and neck lesions and its correlation with histopathology. J. Pathol. Nepal 2016, 6, 985–989. [CrossRef]
- Agrawal, N.; Sharma, H.; Hansrajani, V.; Samadhiya, M.; Raghuwanshi, V.; Khandelwal, P.; Tignath, A. Study of Cervical Neck Masses and Role of Fine Needle Aspiration Cytology in Central India. Ann. Int. Med Dent. Res. 2017, 3. [CrossRef]
- Khetrapal S, Jetley S, Jairajpuri Z, Rana S, Kohli S, Safia R. FNAC of head & neck lesions and its utility in clinical diagnosis: A study of 290 cases. Natl J Med Res. 2015;5(1):33–8.
- Bhasker, N.; Pathak, M. Critical analysis of head and neck swelling with respect to cytomorphological diagnosis: A retrospective study. IP Arch. Cytol. Histopathol. Res. 2020, 5, 58–62. [CrossRef]
Table 1.
Anatomic distribution of FNAC and its histopathologic specimens.
Table 1.
Anatomic distribution of FNAC and its histopathologic specimens.
| Location of lesion |
Lymph node |
Salivary gland |
Cysts |
Soft tissue |
Total |
| Cases (%) |
161 (60.8%) |
96(36.2%) |
7(2.6%) |
1(0.3%) |
265 |
| Sensitivity |
99% |
92.3% |
100% |
100% |
100% |
| Specificity |
91.3% |
98.8% |
100% |
100% |
100% |
| Accuracy |
97.6% |
98% |
100% |
100% |
100% |
Table 2.
Cyto-histological correlation of lymph node.
Table 2.
Cyto-histological correlation of lymph node.
| FNAC Reports (n) |
Histopathological Report REPORTS (n) |
Accuracy Rate |
- 1)
Benign (n=22) |
Reactive follicular hyperplasia (n=15)
Suppurative inflammation (n=4)
Castle mens disease (n=1)
Rosiadormans disease (n=1)
Lymphoma (n=1) |
95.6%
(2 False positive for malignancy) |
- 2)
Tuberculosis(n=38) |
Tuberculosis(n=39) |
97.4% (1 False negative for tuberculosis) |
- 3)
Suspicious for malignancy (n=31) - 4)
Lymphoma (n=45) |
Lymphoma, non-specified (n=21)
Hodgkin Lymphoma(n=27)
Non-Hodgkins Lymphoma (n=26)
Reactive follicular hyperplasia (n=1) |
97.4%
(1 False negative for malignancy) |
- 5)
Metastatic carcinoma(n=25) |
Metastatic carcinoma(n=25) |
100% |
Table 3.
Cyto-Histological Correlation of Salivary Glands, Cystic masses and soft tissue lesions.
Table 3.
Cyto-Histological Correlation of Salivary Glands, Cystic masses and soft tissue lesions.
| FNAC Reports (n) |
Histopathological Report REPORTS (n) |
Accuracy Rate |
| Pleomorphic adenoma (n=69, 71.9%) |
Pleomorphic adenoma (n=70, 72,9%) |
98.6% |
| Mucoepidermoid carcinoma (n=4, 4,2%) |
Mucoepidermoid carcinoma (n=5, 5.2%) |
80% (1 False negative for malignancy. |
| Tuberculosis (n=3, 3.1%) |
Tuberculosis (n=3, 3.1%) |
100% |
| Chronic sialadenitis (n =3, 3.1%) |
Chronic sialadenitis (n=3, 3.1%) |
100% |
| Basal cell adenoma (n =3, 3.1%) |
Basal cell adenoma (n=3, 3.1%) |
100% |
| Adenocarcinoma (n =3, 3.1%) |
Adenocarcinoma (n=3, 3.1%) |
100% |
| Warthin’s tumor (n=2, 2%) |
Warthin’s tumor (n=2, 2%) |
100% |
| Oncocytoma (n=2, 2 %) |
Oncocytoma (n=2, 2 %) |
100% |
| Adenoid cystic carcinoma (n=2, 2%) |
Adenoid cystic carcinoma (n =2, 2%) |
100% |
|
Polymorphous low-grade adenocarcinoma (PLGA) (n=1, 1%)
|
Polymorphous low-grade adenocarcinoma (PLGA) (n=1, 1%)
|
100% |
| Acinic cell carcinoma (n=1, 1%) |
Acinic cell carcinoma (n=1, 1%) |
100% |
| Carcinoma metastasis (n=1, 1 %) |
Carcinoma metastasis (n=1, 1 %) |
100% |
| Cysts |
|
|
| Thyroglossal cyst (n=1, 14.3%) |
Thyroglossal cyst (n=1, 14.3%) |
100% |
| Branchial cyst (n=2, 28.6%) |
Branchial cyst (n=2, 28.6%) |
100% |
| Epidermoid cyst (n=3, 42.8%) |
Epidermoid cyst (n=3, 42.8%) |
100% |
| Immature teratoma (n=1, 14.3%) |
Immature teratoma (n=1, 14.3%) |
100% |
| Soft tissue lesions |
|
|
| Lipoma (n=1, 100%) |
Lipoma (n=1, 100%) |
100% |
Table 4.
Diagnostic accuracy rates compared with previous reports.
Table 4.
Diagnostic accuracy rates compared with previous reports.
| |
Our study |
Rammeh S et al 16 |
Poorey VK et al 15 |
Tandon S et al7 |
| Sensitivity |
94.8% |
92% |
89.6% |
89.6% |
| Specificity |
97.6% |
94.4% |
96.5% |
98.5% |
| Accuracy rate |
96.5% |
93.5% |
93.1% |
95.1% |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).