2.1. Case 1
A 67-year-old woman with well-controlled diabetes mellitus, hypertension, hyperlipidemia, and peripheral vascular disease presented to the emergency department with a one-week history of worsening neck pain, along with numbness and weakness in both the upper and lower limbs. She was a non-smoker and non-alcoholic, and remained independent in her activities of daily living. She reported no urinary retention, bowel incontinence, headache, dizziness, fever, or history of gout.
On initial assessment, her vital signs were stable: blood pressure was 137/82 mmHg, body temperature was mildly elevated at 37.7 °C, and her Glasgow Coma Scale (GCS) score was 15. There was no spinal tenderness on examination.
Neurological assessment of the lower limbs showed bilateral weakness, more pronounced on the right side. Muscle power was graded 4/5 (Medical Research Council scale) in hip flexion, knee extension, and big toe dorsiflexion. Sensory examination was intact, and the digital rectal exam (DRE) was normal.
In the upper limbs, muscle power was reduced bilaterally to grade 3/5 in wrist dorsiflexion, shoulder abduction, and finger abduction. A positive Hoffmann sign and brisk reflexes in both upper and lower limbs raised suspicion of cervical spinal cord compression.
Initial blood investigations revealed a white blood cell count of 15.13, an elevated erythrocyte sedimentation rate (ESR) of 85, and a C-reactive protein (CRP) level of 14.0, indicating inflammation. Bone metabolism tests were normal, but Vitamin D 25-Hydroxy levels were low.
Lumbar spine X-ray showed loss of normal lumbar lordosis, grade 1 retrolisthesis of L3 over L4, moderate compression fractures at L4 and L5, and mild anterior wedging at L1 and L2. The orthopedic spine team assessed the patient and made a preliminary diagnosis of cervical myelopathy, recommending an MRI of the whole spine.
The following day, upper limb strength deteriorated further, prompting an urgent whole-spine MRI. Intravenous dexamethasone (8 mg stat, followed by 4 mg three times daily) was initiated, and the patient was kept nil per os (NPO) in preparation for potential emergency surgery. ASIA scoring was conducted every two hours, and a CT brain scan was requested to rule out a cerebrovascular event.
2.1.1. Imaging Findings
CT Brain: Normal.
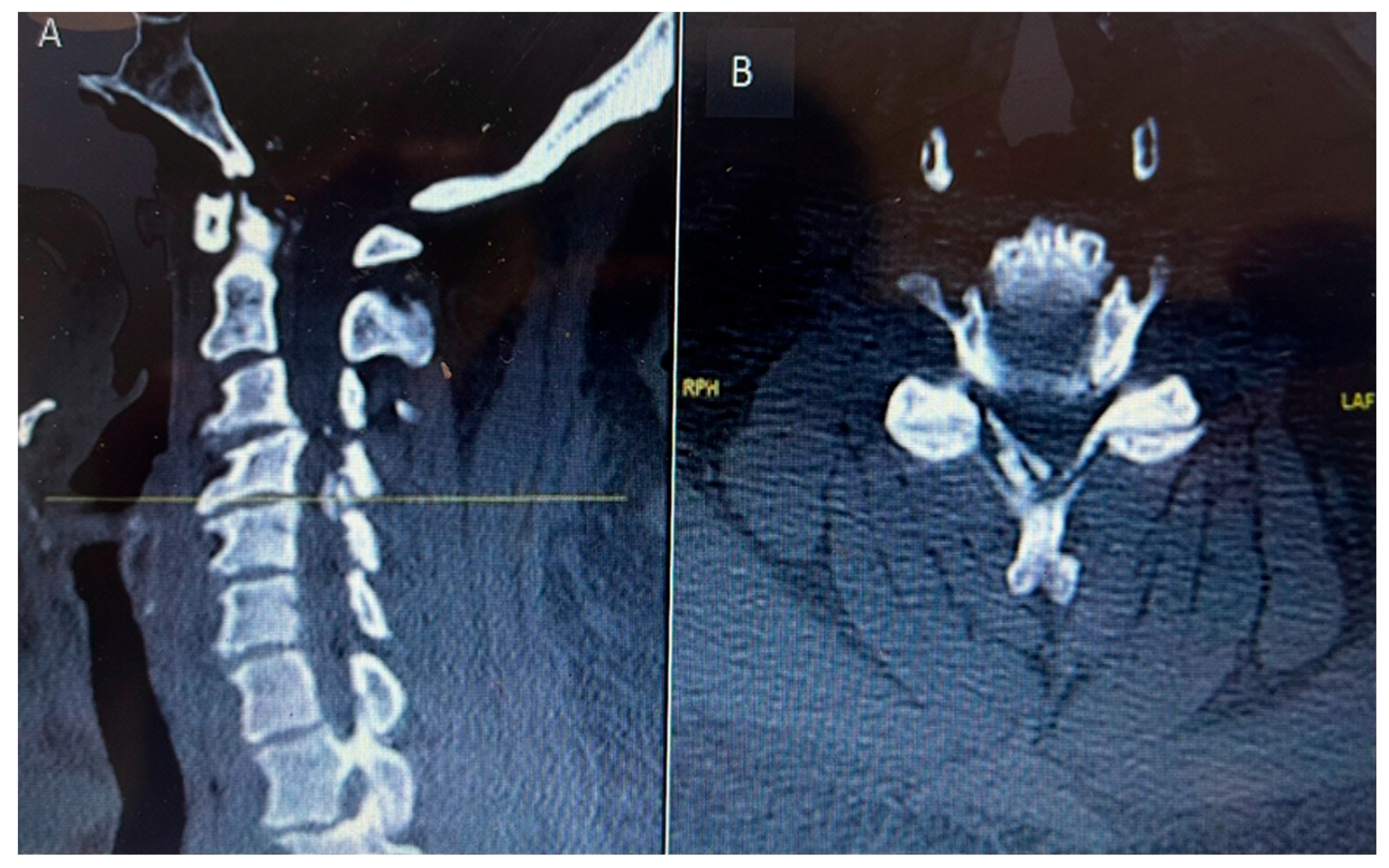
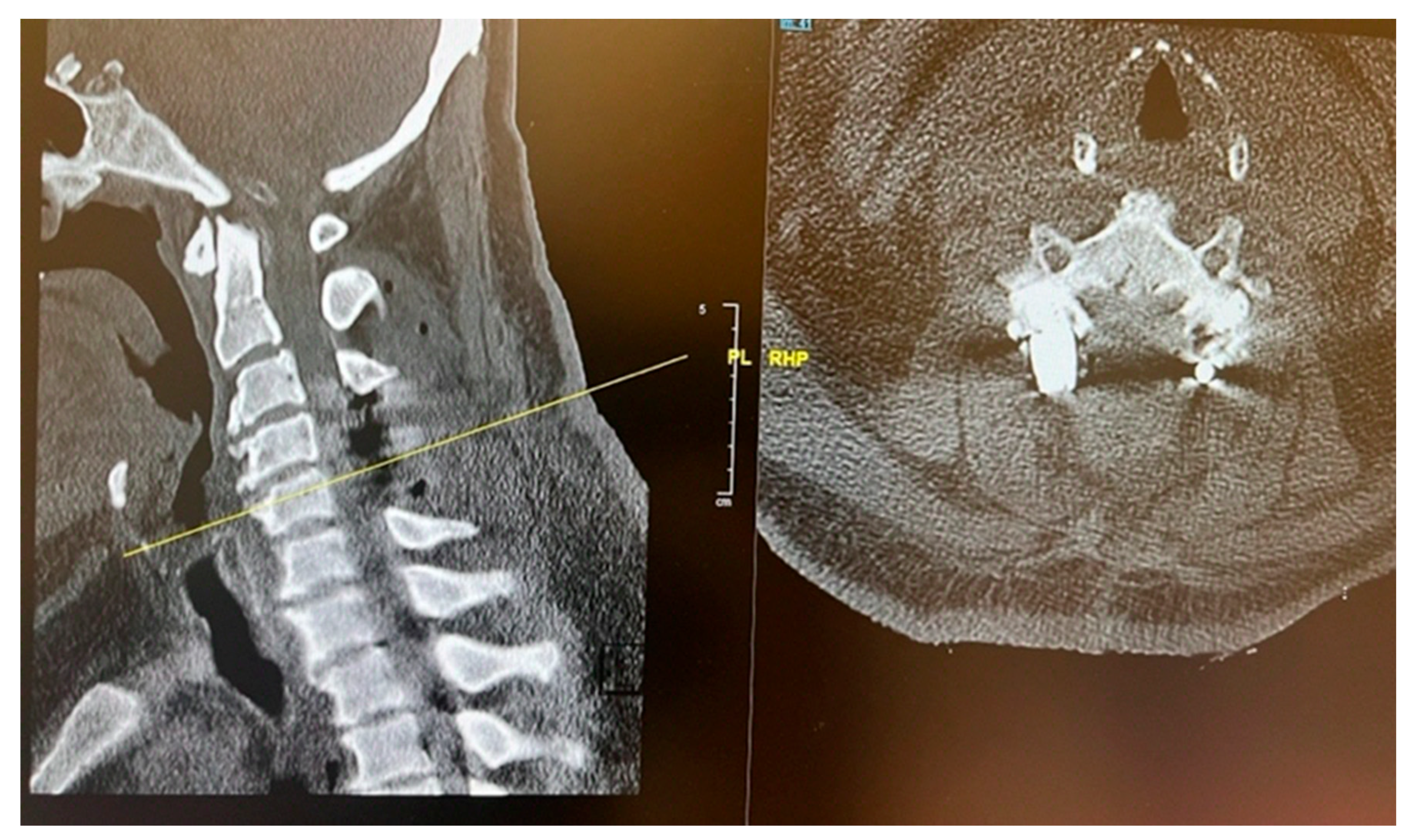
CT C Spine: Ossification of the right-side ligamentum flavum noted at C4/C5 and C5/C6 levels, with associated spinal canal narrowing, more severe at C4/C5.
Figure 1.
Preoperative sagittal (A) and axial (B) CT cervical spine showing calcific deposit at the cervical 4 level causing spinal stenosis.
Figure 1.
Preoperative sagittal (A) and axial (B) CT cervical spine showing calcific deposit at the cervical 4 level causing spinal stenosis.
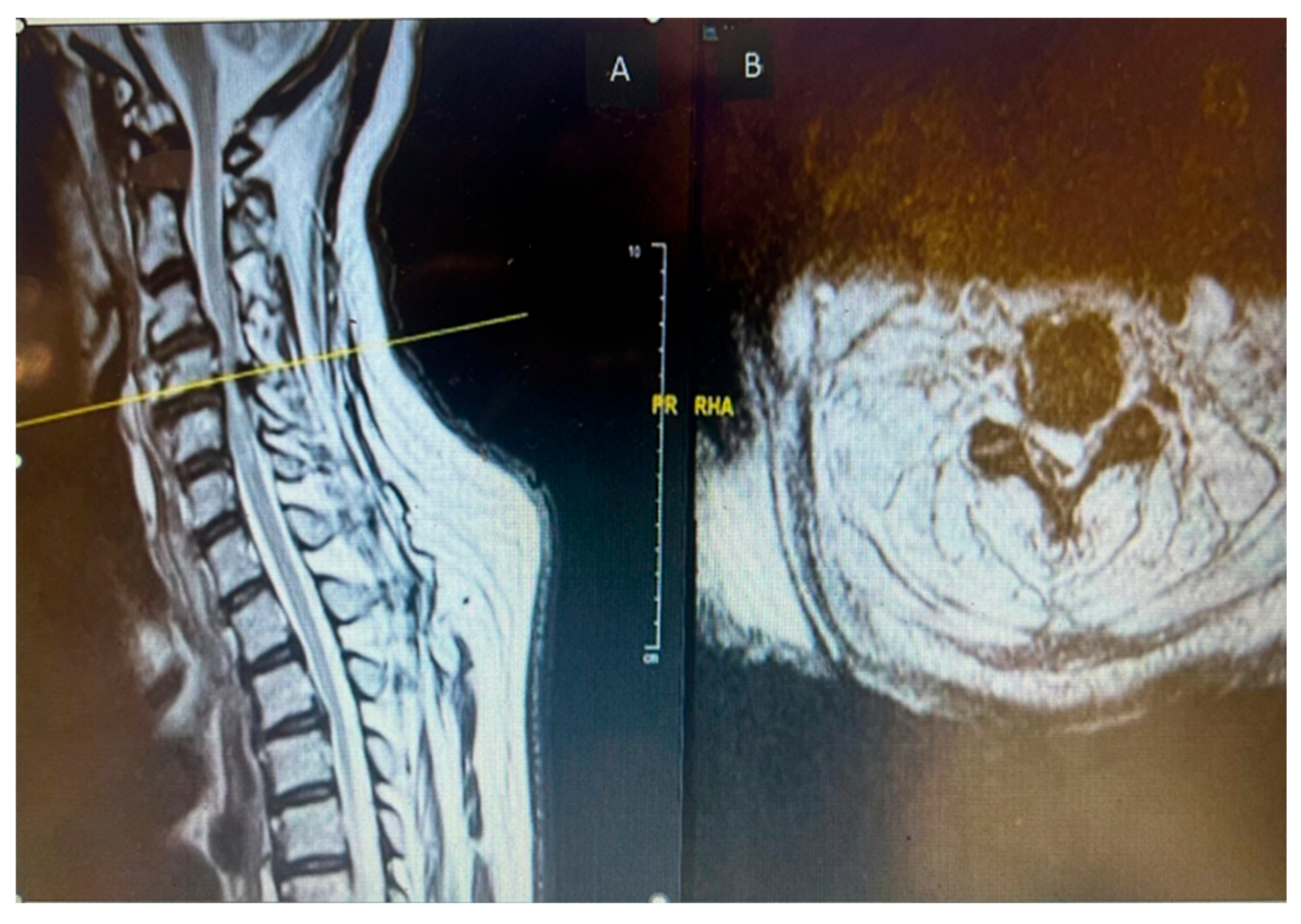
MRI Whole Spine: Severe central canal narrowing causing compression of the spinal cord with myelomalacia at C4/C5 level, with mild retrolisthesis at C4 over C5, thickening of the posterior longitudinal ligament, and ligamentum flavum hypertrophy. Various degrees of central canal narrowing and neural foraminal narrowing were noted at C3/C4, C4/C5, C5/C6, and C6/C7 levels, with additional findings including a small synovial cyst at C6/C7.
Figure 2.
Preoperative MRI cervical spine T2 weighted sagittal (A) and axial (B) showing cord compression posteriorly with cord signal change at cervical 4 level.
Figure 2.
Preoperative MRI cervical spine T2 weighted sagittal (A) and axial (B) showing cord compression posteriorly with cord signal change at cervical 4 level.
2.1.2. Treatment and Management
The patient and her family were informed about her clinical condition and the MRI findings. Surgical management was planned, involving posterior cervical instrumentation from C3 to C5, along with decompressive laminectomy at the C4 and C5 levels. Preoperative intravenous antibiotics were administered. The posterior cervical spine was surgically exposed, and central decompression was achieved through complete laminectomy of C4 and C5. Lateral mass screw fixation was carried out from C3 to C5.
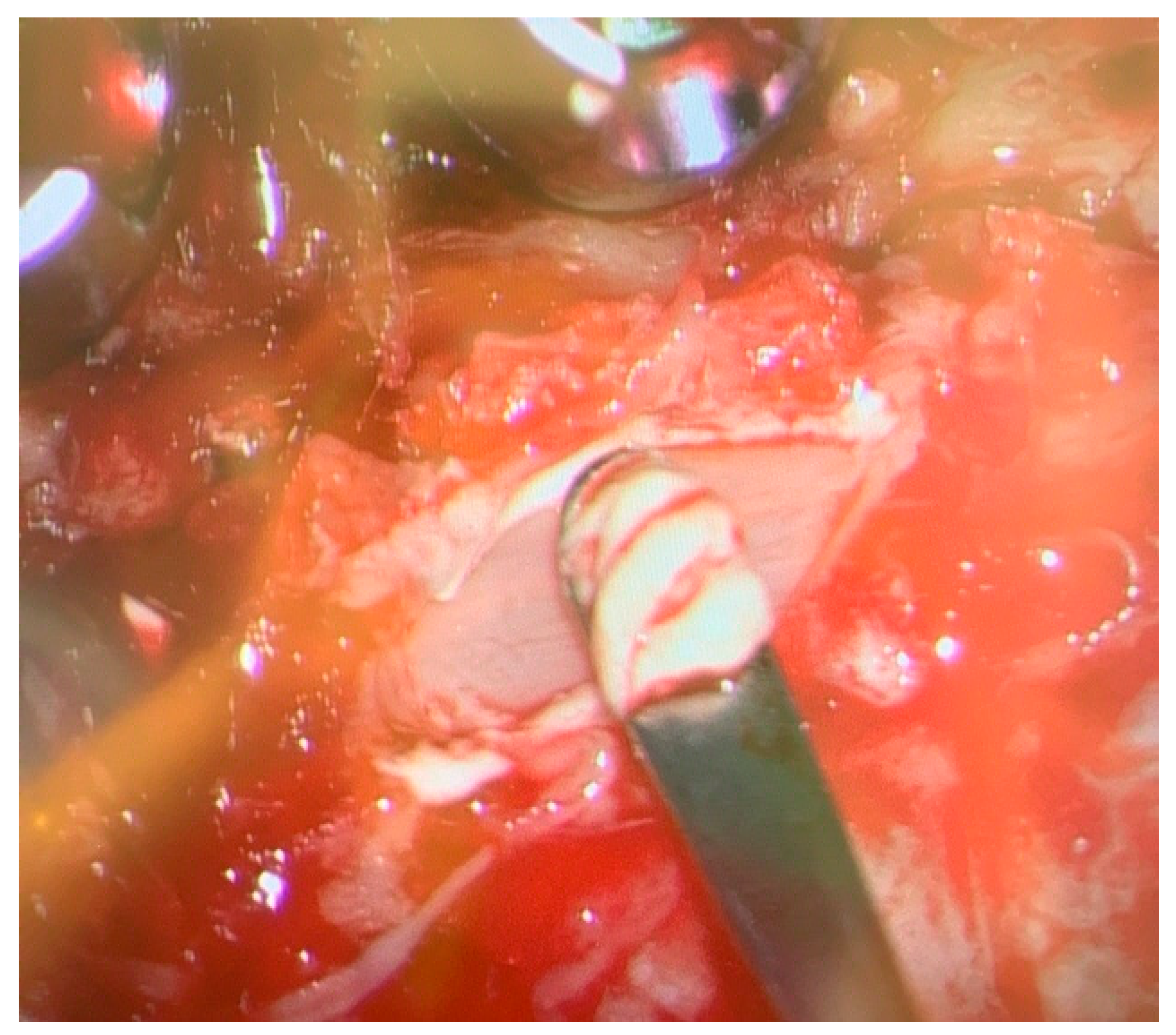
During the procedure, chalky white deposits were observed in the right-sided epidural space at the level of C4, overlying the ligamentum flavum. These deposits were removed in a piecemeal fashion, decompressing the spinal cord. Specimens were collected and sent for histopathological examination and culture. Baseline neuromonitoring showed weak somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP) in both the upper and lower limbs, with no signs of nerve irritation detected on electromyography (EMG).
2.1.3. Postoperative Findings
The chalky white deposits were sent for histopathological analysis; however, they were preserved in formalin, which precluded crystal analysis. Cultures taken from the epidural space showed no bacterial growth. Postoperatively, the patient's serum uric acid level was elevated at 445 µmol/L (normal range: 150–370 µmol/L). She was referred to rheumatology for further management of hyperuricemia and commenced postoperative rehabilitation, which led to noticeable improvement in both upper and lower limb weakness. A Dual Energy CT (DECT) scan of the cervical spine was performed to detect urate crystal deposition. However, the findings were inconclusive, likely due to the extensive removal of tophaceous material and thorough decompression during surgery.
Figure 3.
Intraoperative image showing chalky white deposit over the ligamentum flavum at.cervical 4 level.
Figure 3.
Intraoperative image showing chalky white deposit over the ligamentum flavum at.cervical 4 level.
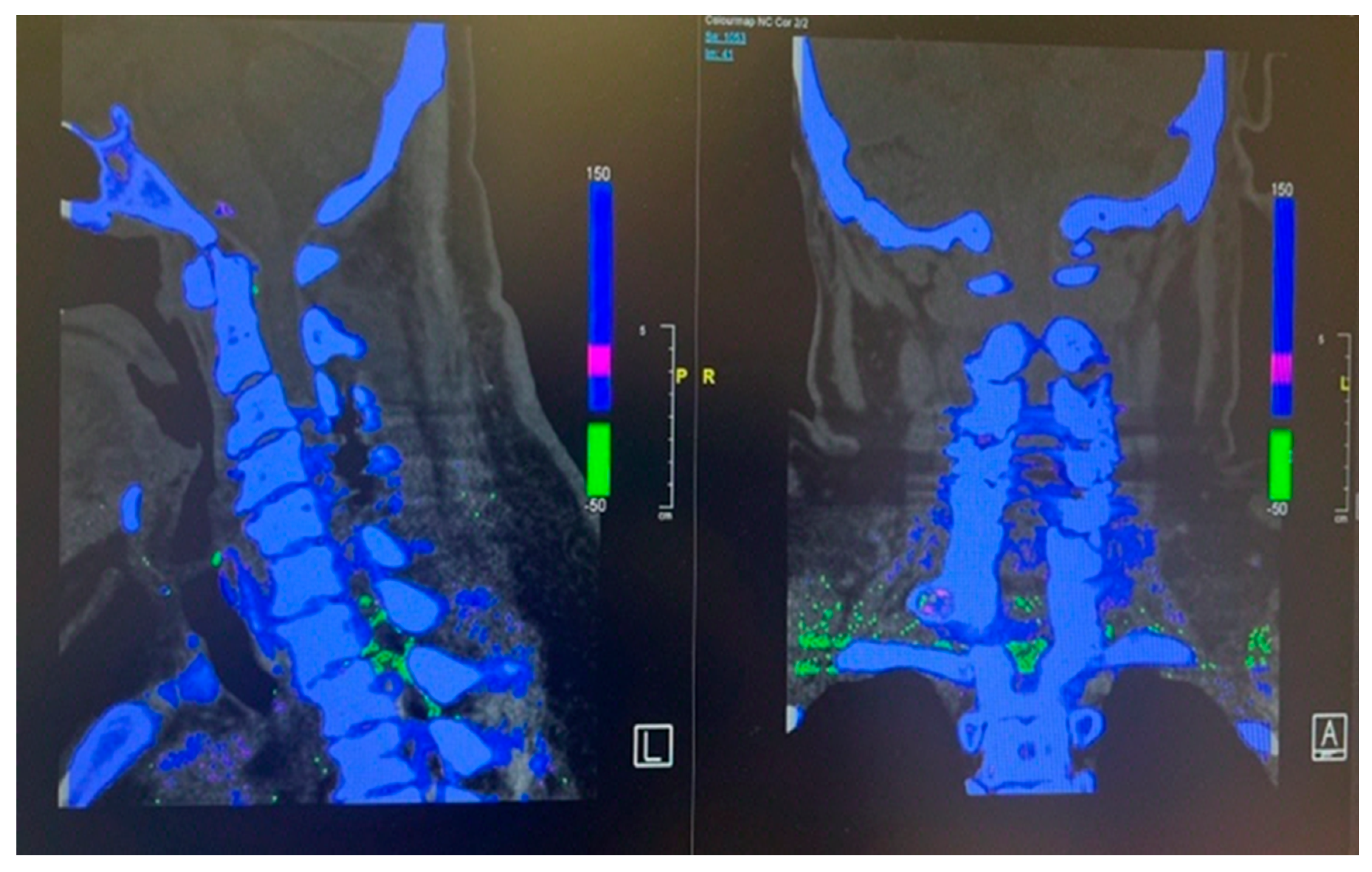
Figure 4.
Post operative dual energy CT scan of cervical spine showing.absence green color urate Crystals at the site of the surgery due to removal of Gout tophi.
Figure 4.
Post operative dual energy CT scan of cervical spine showing.absence green color urate Crystals at the site of the surgery due to removal of Gout tophi.
Figure 5.
Post operative CT scan of the cervical spine showing complete decompression at the cervical 4 and 5 levels.
Figure 5.
Post operative CT scan of the cervical spine showing complete decompression at the cervical 4 and 5 levels.
2.2. Case 2
This 68 years old male having past medical history of Obesity, Diabetes Mellitus, hypertension, chronic kidney disease 3b, Knee osteoarthritis, Psoriasis, ureteric calculus and right-side Meralgia paresthetica presented to emergency department with the complaint of 3 days history of abdominal pain radiating to towards right lower back worst on bending forward. There was associated foul smelling urine without fever, frequency, dysuria and hematuria. On examination patient was vitally stable, having generalized psoriatic rashes with negative bilateral negative renal punches and normal testicular examination. Laboratory tests showed flat total white cells count with Neutrophil count of 7.10. Renal functions test was unremarkable. Urine dipstick result was suggestive of UTI therefore urine culture and sensitivity test were sent. X Ray KUB revealed 0.5 cm radio density along right hemi pelvis likely a phlebolith as seen before on prior CT with no calculus along the urinary tract. Degenerative changes were reported in lumbar spine and left pelvis on X Ray Lumbar spine, pelvis and hip joints. Patient was discharged from emergency with Orthopedics and spine follow up.
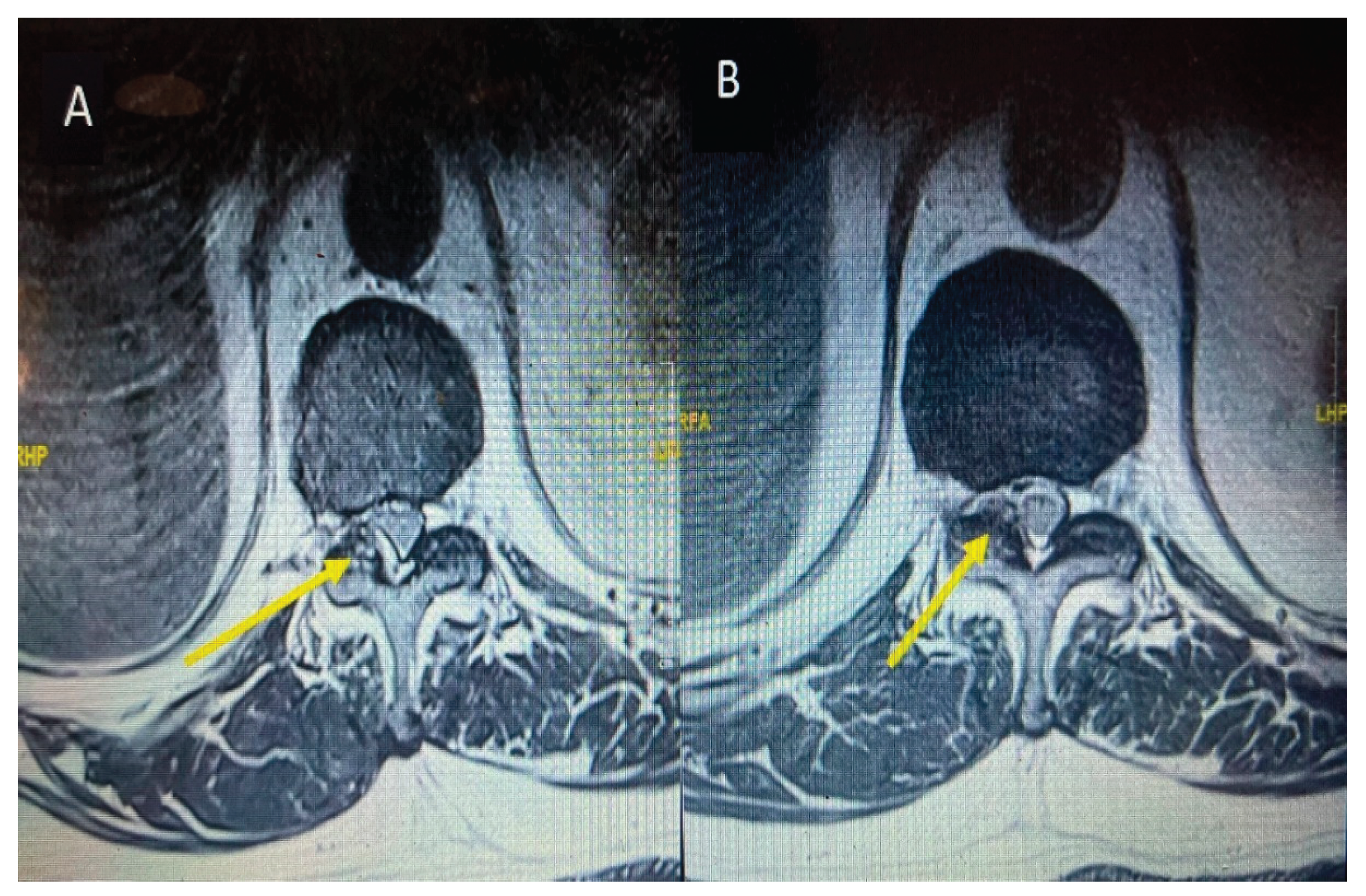
2 days after discharge from emergency, patient again presented to the emergency department with the complaint of right iliac fossa pain for 1 day, therefore after relieving pain was referred to general surgery. CT abdomen and pelvis was ordered by General surgery team reported left stage horn calculus and left upper ureter inflammatory urethritis, with possible secondary minimal left pyelonephritis. He was referred to Urology for further management. Subsequently, patient developed right lower limb pain along entire right thigh, posterior leg and both surfaces of right foot. There was also associated bilateral knee pain. There was 2/5 power in bilateral L2 and L3 myotomes limited by pain with the rest neurological examinations unremarkable. The patient was referred to Hip and Knee and ortho spine. On suggestion of spine team, the primary team arranged MRI Lumbar spine with contrast and sent inflammatory markers. MRI report revealed fluid within the right L5/S1 and edema in the adjacent L5/S1 vertebral bodies suspicious for L5/S1 spondylodiscitis with osteomyelitis involving right side more than left. Other than this at the same level L5/S1 posterior annular fissure and posterior disc protrusion causing moderate right exit foraminal narrowing abutting the right L5 exiting nerve root as shown in the
Figure 6 (A). Additionally, right sided facet joint synovial cyst at T11/12 was noted having size of 12 mm causing severe right sided sub articular stenosis compressing right T12 descending nerve root and moderate right exit foraminal narrowing abutting the right T11 exiting nerve root as shown in the
Figure 8 (A).
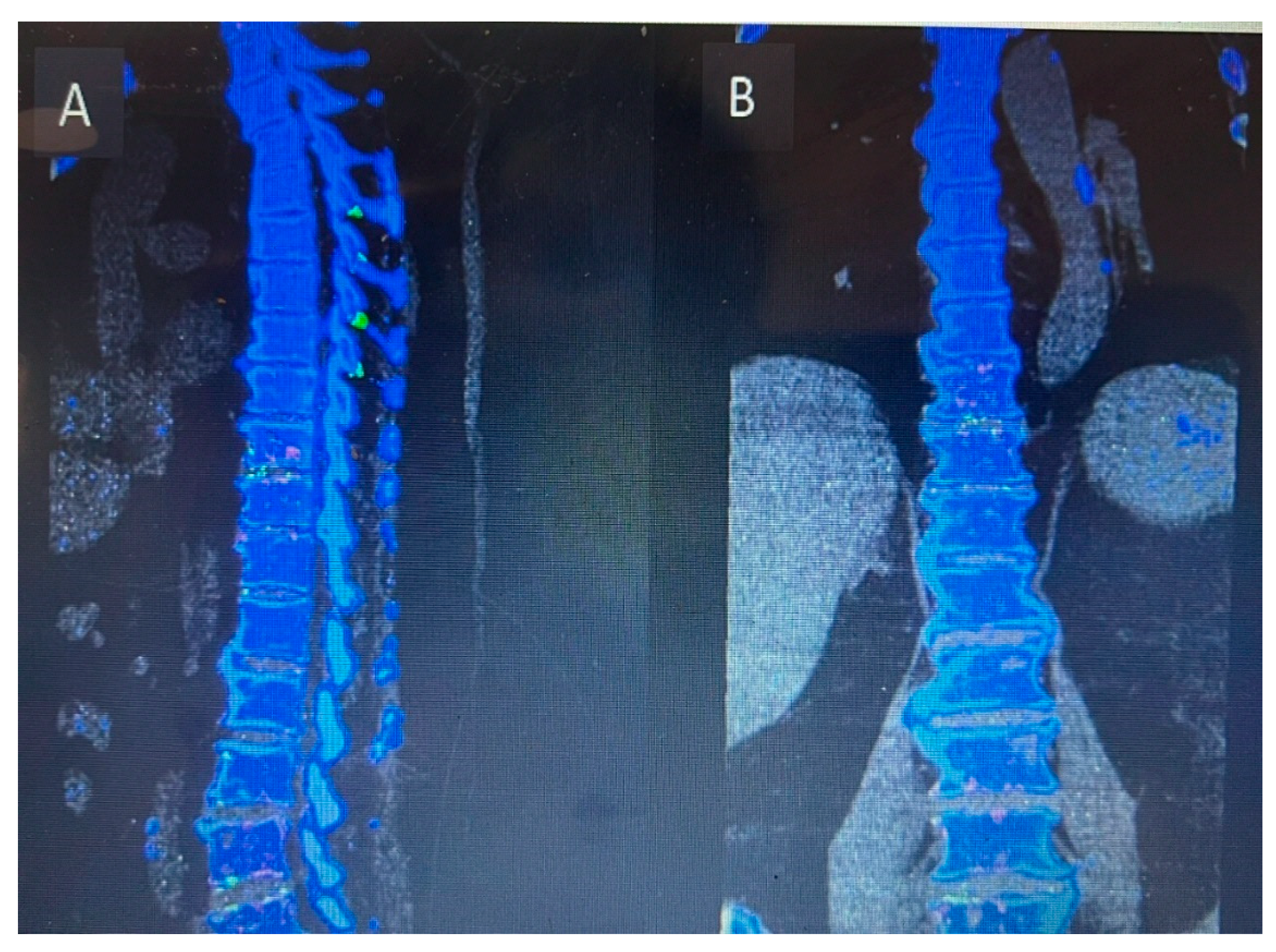
Inflammatory markers showed raised CRP level of 292. Meanwhile Hip and Knee team advised X Rays both knees reported as bilateral osteoarthritis with bilateral moderate to large suprapatellar effusion. Later on, they did bilateral knee joints aspiration and sent aspirate for laboratory evaluation which showed raised nucleated cells (35415), neutrophils (92%) and negatively birefringent crystals Based on knee joint aspiration result the patient was referred to Rheumatology for further assessment and serum Uric acid was sent as per their suggestion showed raised level of 532. Patient was counselled for image guided biopsy of the reported levels on MRI spine in order to exclude infective spondylodiscitis and septic arthritis but due to patient reluctance it was not done. While keeping in mind the patient clinical, radiological and lab tests picture dual energy CT whole spine was done reported as Urate deposits at the T10/11 and lower lumbar discs especially at L5/S1. Green pixelation in the rest of the thoracolumbar spine appears to represent artifact rather than further urate deposits. In particular, there does not appear to be urate deposits at the region of right the right T11/12 facet joint as shown in the
Figure 7 (A) and (B). In order to start a definitive treatment, image guided biopsy was discussed with the patient but not done due to patient reluctance. Meanwhile multidisciplinary meeting was held between Infectious disease and Rheumatology teams while keeping in mind the differential diagnosis and a conclusion was made to treat the patient for Gout. Rheumatology team started the patient on 3 weeks tapering dose of prednisolone followed by 5 mg OD dose for few months for Gout prophylaxis. He was also started on Allopurinol an anti-Gout medication with a dose of 50 mg OD. Later on, Patient was transferred under the care of rehabilitation team. Patient CRP and serum Uric acid were trended over the time and showed progressive declined in their levels along with clinical improvement. Follow up MRI lumbar and thoracic spine revealed improvement in the form of slight signals improvement at L5/S1 shown in
Figure 5 (B) and disappearance of right T10/11 facet cyst shown in the
Figure 8 (B). After completing rehabilitation, the patient was discharged to the home with the follow up schedule with different concerned specialties.
Figure 6.
MRI Lumbar spine short tau inversion recovery sequency sagittal views first MRI before starting anti gout medications (A) and follow up MRI after starting anti gout medications (B) showing spondylodiscitis at the level of lumbar 5, sacral 1 level.
Figure 6.
MRI Lumbar spine short tau inversion recovery sequency sagittal views first MRI before starting anti gout medications (A) and follow up MRI after starting anti gout medications (B) showing spondylodiscitis at the level of lumbar 5, sacral 1 level.
Figure 7.
Dual energy CT of whole spine sagittal view (A) and coronal view (B) showing Urate crystal deposits at the levels of T10/11 and L5/S1. The rest of the green pixelation is an artifact rather than urate crystals.
Figure 7.
Dual energy CT of whole spine sagittal view (A) and coronal view (B) showing Urate crystal deposits at the levels of T10/11 and L5/S1. The rest of the green pixelation is an artifact rather than urate crystals.
Figure 8.
MRI thoracic spine T2 weighted at the level of T10/11 axial section before starting anti gout. Medications (A) and axial section of follow up MRI after starting anti gout medications (B) showing a cyst on the right side as indicated by yellow arrow and total disappearance as shown by yellow arrow after starting anti gout medications.
Figure 8.
MRI thoracic spine T2 weighted at the level of T10/11 axial section before starting anti gout. Medications (A) and axial section of follow up MRI after starting anti gout medications (B) showing a cyst on the right side as indicated by yellow arrow and total disappearance as shown by yellow arrow after starting anti gout medications.