Introduction
Traumas involving pregnant women are uncommon but potentially serious, as both the mother and fetus face significant risks [
1]. Blunt abdominal trauma is the leading non-obstetric cause of maternal mortality [
2], with road traffic accidents (55%), falls (22%), and assaults (22%) being the most common causes [
3,
4,
5,
6,
7]. The precise incidence is difficult to determine, as most available data come from observational and retrospective studies or case series [
8]. It is estimated that one in twelve pregnancies could be complicated by trauma [
8], especially in the third trimester [
7].
Blunt abdominal trauma is considered a medical emergency due to its association with significant maternal and fetal morbidity and mortality [
7,
9,
10,
11]. Reported mortality rates vary widely, from 13% to 51% [
5,
12], and pregnant women face almost double the mortality risk compared to non-pregnant trauma patients [
13]. In fact, 50% of maternal deaths during pregnancy are attributed to trauma [
14].
Gestational trauma has substantial implications for the fetus as well [
8]. Although life-threatening trauma accounts for less than 8% of all traumas, it carries a 40% to 50% risk of fetal loss [
1,
15] due to complications such as premature rupture of membranes, premature labor, uterine rupture, placental abruption, direct fetal injury, or maternal shock [
8,
15]. Fetal loss is more likely to occur as the severity of the trauma increases. For example, it is estimated that at least 3.7 fetal and neonatal deaths per 100,000 pregnancies are related to automobile accidents [
16], with placental abruption being the second most common cause of post-traumatic fetal death when the mother survives [
8].
Thus, the early detection and management of trauma-related complications require multidisciplinary care at a trauma referral center. This team should include specialists from emergency medicine, obstetrics, gynecology, general surgery, and intensive care.
The aim of this article is to present a case of blunt abdominal trauma in a pregnant woman in her third trimester complicated by intestinal ischemia. After a thorough literature review, we found no similar cases previously reported.
Case Presentation
A 41-year-old pregnant patient at 33 weeks and 6 days of gestation was admitted after a traffic accident. She was seated in the front passenger seat of a 4-wheeled vehicle, wearing an adapted seat belt, when the vehicle left the road and overturned. After initial on-site assistance by emergency services, she was found to have respiratory distress with severe pain in the right hemithorax and moderate hypoxemia. No hypotension or neurological deterioration was observed.
The patient was transferred to a level-one trauma referral center equipped for obstetric care [
7,
16]. Physical examination revealed subcutaneous emphysema in the right hemithorax and paradoxical breathing. A chest X-ray showed a right pneumothorax, prompting the placement of emergent endothoracic drainage due to multiple fractures of the right anterior costal arches (from the 2nd to the 7th ribs). This accounted for both the right pneumothorax and the flail chest. The pelvis was stable, and there was no abdominal pain on palpation or genital bleeding. Superficial injuries, including abrasions, a small supraumbilical hematoma, and another hematoma on the lateral wall of the upper abdomen, were noted, with no clear signs of seat belt injury.
In the initial Focused Assessment with Sonography for Trauma (FAST), no solid organ injuries or free fluid in the Morrison space, splenorenal space, or Douglas pouch were observed. A gynecological assessment via obstetric ultrasound confirmed fetal vitality and normal placental positioning, with no evidence of placental abruption. Fetal monitoring showed no pathological patterns, and there was no uterine activity on admission.
During the first 72 hours in the Intensive Care Unit (ICU), the patient's condition remained stable. She received optimal pain control with intravenous analgesia, and her vital signs, as well as blood analyses, remained consistent throughout her stay. The evolution of her vital parameters during hospitalization is shown in
Table 1.
After this period, the patient began to experience uterine activity, which was initially treated with tocolytics. Pulmonary maturation was also induced due to her gestational age, in anticipation of potential preterm delivery.
On the fourth day of admission, there was an abrupt deterioration. The patient developed severe gastrointestinal symptoms, including intense epigastric pain, heartburn, nausea, and recurrent vomiting, which complicated food intake. These symptoms persisted despite antacid treatment. On examination, her abdomen was distended, firm, and diffusely tender to palpation. Constipation was noted, despite administering a cleansing enema.
Given the suspicion of paralytic ileus, a conservative approach was initially taken, with nasogastric decompression resulting in partial improvement and evacuation of a significant volume of fecal content. Non-invasive imaging studies were requested, including an obstetric ultrasound to verify fetal viability and an abdominal ultrasound to investigate potential intra-abdominal trauma-related complications. The obstetric ultrasound revealed a fetus in cephalic presentation with normal heart rate and movements. The abdominal ultrasound showed a significantly distended stomach, but no other pathological findings.
Laboratory results showed no significant changes since admission. The evolution of these findings is detailed in
Table 2.
Given the marked clinical worsening of the patient, an arterial blood gas analysis was performed, showing pH 7.3, arterial CO2 pressure of 29 mmHg, and HCO3 of 18 mEq/L, indicating metabolic acidosis, likely due to repeated vomiting and tachypnea.
As the patient's hemodynamic and respiratory condition deteriorated, clinical signs such as tachycardia, tachypnea, and moderate hypoxemia were noted (detailed in
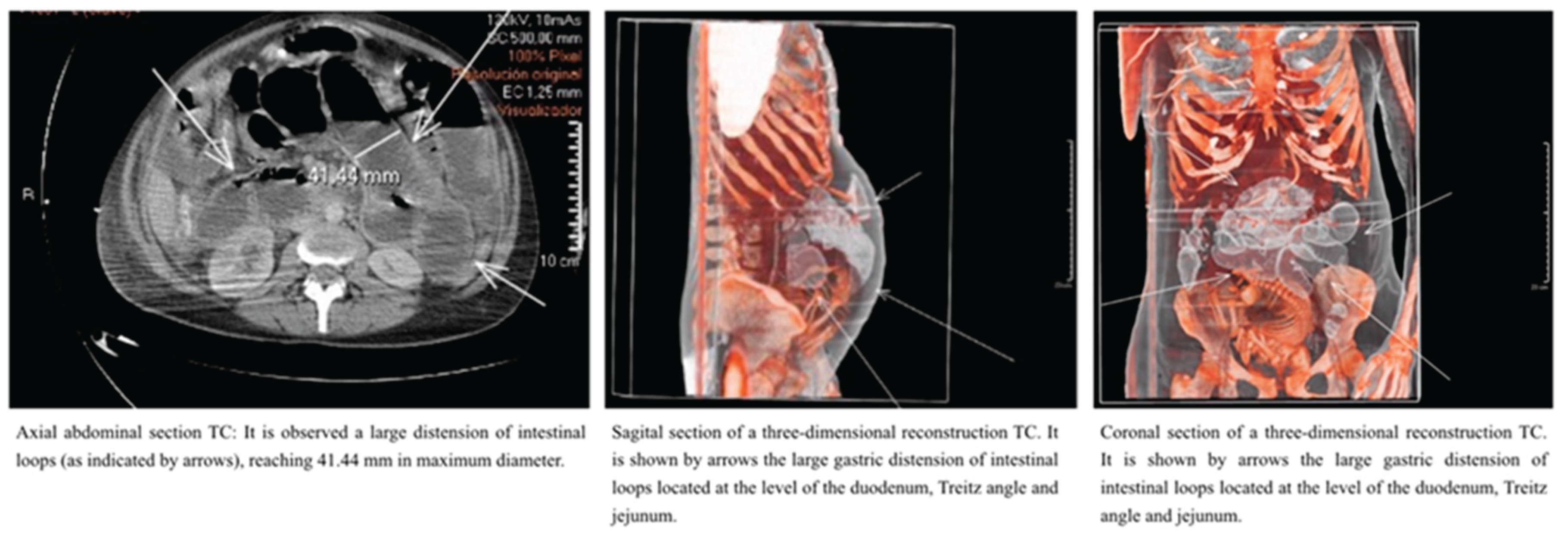
Table 1). Combined with the suspicion of intestinal pseudo-obstruction, emergency medical specialists, in agreement with obstetrics specialists, decided to pursue a more accurate and relevant diagnostic imaging test. After weighing the risk-benefit ratio with the Radiology Department and minimizing fetal risk, a thoraco-abdomino-pelvic computed tomography (CT) was performed. The CT scan revealed no solid organ injury but showed significant gastric distension and dilated intestinal loops at the level of the duodenum, Treitz ligament, and jejunum. There were no signs of loop ischemia, intestinal obstruction, perforation, or mesenteric vessel thrombosis (
Figure 1).
Following the CT, when the patient was transferred back to the ICU, she began experiencing regular and painful uterine contractions. Given the clinical instability and high suspicion of acute abdomen, and after verifying fetal viability in a near-term pregnancy, a multidisciplinary team (including intensivists, obstetricians, and general surgeons) reached a consensus to perform an emergency cesarean section. Vaginal delivery was ruled out due to concerns for maternal-fetal well-being and the potential for unresolved obstetric complications.
A Pfannenstiel incision was made, following standard procedure. After the birth of a live newborn, the abdominal cavity was explored, and the incision was extended infraumbilically. This revealed a serous-purulent collection, consistent with secondary peritonitis affecting all four abdominal quadrants. Additionally, a small bowel loop at the ileal level, approximately 10 cm from the ileocecal valve, showed signs of ischemic damage, with a 15 cm necrotic section identified. An intestinal resection was performed on the affected loop, followed by end-to-end anastomosis.
In the postoperative period, the patient's clinical course was favorable. She was discharged home two weeks after surgery without any postoperative complications.
Discussion
The management of severely polytraumatized patients requires well-established protocols to ensure a rapid, coordinated response that leads to favorable functional and survival outcomes. When the patient is a pregnant woman, as in the case described, the complexity of management increases significantly, necessitating a multidisciplinary approach involving various medical and surgical specialties to ensure both maternal and fetal safety.
Trauma complicates up to 7% of pregnancies and is the leading non-obstetric cause of maternal morbidity, mortality, and intrauterine fetal death [
2]. The management of trauma during pregnancy should largely mirror that of non-pregnant patients [
4], recognizing that the best treatment for the fetus is optimal maternal resuscitation. Special attention must be given to complications that can directly threaten maternal and fetal well-being, such as placental abruption and uterine rupture.
The anatomical and physiological changes during pregnancy complicate the assessment of traumatic injuries [
14,
15], particularly after 12 weeks of gestation [
18]. These changes may also affect responses to resuscitation and diagnostic test results. As gestation progresses, the growing uterus and fetus increase the risk of fetal and placental injury, with the third trimester being the period of highest risk [
19].
The primary obstetric concern in cases of blunt trauma is the tension and displacement of the uterus during impact, which can lead to placental abruption due to backblow mechanisms [
8]. Direct fetal injury may occur due to blunt force impact, such as hitting the steering wheel in a car accident or due to intracranial trauma associated with pelvic fractures when the fetus is in a cephalic presentation during the third trimester. Additionally, the growing uterus pushes the intestinal loops upwards, making the intestines one of the more protected organs from blunt trauma, though this was not the case in our patient. The presence of abrasions in the right upper abdominal quadrant during the initial physical exam could have indicated possible blunt abdominal trauma.
Unlike penetrating trauma, blunt trauma lacks obvious external signs, making it difficult to gauge the severity of injuries, which can result in delayed diagnoses of severe, life-threatening intra-abdominal injuries [
4]. Moreover, clinical signs of peritoneal irritation are less obvious in pregnant women, reducing the effectiveness of physical exams in detecting such injuries.
In pregnancy, the hyperdynamic and hypervolemic state can mask significant blood loss [
2,
14]. A pregnant woman may not exhibit typical signs of shock even after losing up to 20% of her blood volume [
7]. Only after blood loss exceeds 2,500 milliliters may the mother's condition rapidly decline, reducing the chances of fetal survival to 20% [
3].
Healthcare providers face the challenge of managing two patients simultaneously: the mother and the fetus [
17]. A multidisciplinary approach is critical to optimizing care, and the main focus must remain on stabilizing the mother since fetal outcomes are directly linked to maternal survival and stability [
8]. What is beneficial for the mother is beneficial for the fetus [
8,
15].
After maternal stabilization, radiological tests (e.g., chest and pelvic X-rays, computed tomography) should be performed if necessary and should not be delayed due to unfounded concerns about fetal effects [
2,
8]. Studies show that these tests can identify significant, silent lesions in symptomatic patients, even when abdominal ultrasound results are inconclusive [
8,
18,
20]. When ionizing radiation is required, the uterus should be shielded, and it is important to note that radiation doses below 5 rads (0.05 Gy) are not associated with increased risks of anomalies, spontaneous abortion, or fetal growth restriction [
14,
15]. CT scanning remains the fastest and most accessible diagnostic tool for abdominal and pelvic trauma [
21].
Treatment for blunt abdominal trauma in pregnant patients who are hemodynamically stable is typically conservative [
14,
22]. However, early surgical intervention may be necessary in cases of hemodynamic instability or when bowel injury is highly suspected. Hypotension and sepsis are particularly dangerous and can be fatal to both the mother and the fetus [
14].
Gastrointestinal injuries in the context of blunt trauma are rare, with a prevalence of only 1% among trauma admissions in the general population [
23]. The most commonly affected hollow organ is the small intestine, and injuries in this location can be silent, delaying diagnosis and treatment and significantly increasing maternal and fetal morbidity and mortality [
23]. The initial diagnosis of hollow viscera injury relies on physical exam findings and CT imaging, with sensitivities between 55% and 95%, and specificities ranging from 48% to 92%, and a false negative rate of up to 15% [
23]. In cases of diagnostic uncertainty, urgent surgery should be considered.
In specific situations where maternal deterioration is imminent, as in this case, emergency cesarean sections should be considered to safeguard both maternal and fetal life. Studies report that, in pregnant women beyond 25 weeks of gestation [
3], cesarean section performed for trauma-related indications results in a 45% fetal survival rate and a 72% maternal survival rate [
3]. This knowledge is crucial to making the correct multidisciplinary decision, which can lead to optimal maternal and neonatal outcomes, as demonstrated in this case.
Conclusions
Intestinal ischemia following blunt abdominal trauma in a pregnant patient is a rare and difficult-to-diagnose condition. Delayed treatment can result in significant morbidity and mortality for both mother and fetus. Rapid surgical intervention through cesarean section and exploratory laparotomy is necessary in cases of clinical deterioration and maternal instability to identify and treat life-threatening injuries. Coordinated multidisciplinary care is key to early detection of silent complications, potentially preventing avoidable deaths and achieving favorable maternal and neonatal outcomes.
Authors ‘contributions:
M.D., A.M.F., M.M. and L.C. contribute to conception and design. M.D. was responsible to acquisition of data. M.D., A.M.F., M.M., J.E.G. and L.C. contribute to analysis and interpretation of data. All authors contribute to drafting the article and revising it critically for important intellectual content. All authors contributed to the write up of the manuscript and approved the final version for submission.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Informed consent was obtained from the patient for the study.
Informed Consent Statement
Written consent has been obtained from the patient to publish this paper.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
List of Abbreviations
ECO- FAST Focused Evaluation with Sonography in Trauma.
ICU Intensive Care Unit.
CT Computed Tomography.
References
- Aryan N, Grigorian A, Lucas AN, et al. Outcomes for advanced aged (35 and older) versus younger aged pregnant trauma patients: A multicenter study. Am J Surg. 2023;226:798–802. [CrossRef]
- Rossignol M. Trauma and pregnancy: What anesthesiologist should know. Anaesth Crit Care Pain Med. 2016;35–34. Available from. [CrossRef]
- Tasneem B, Fox D, Akhter S. Blunt Abdominal Trauma in the Third Trimester: Eight Departments, Two Patients, One Survivor. Cureus. 2021;13. [CrossRef]
- Neeki MM, Hendy D, Dong F, et al. Correlating abdominal pain and intra-abdominal injury in patients with blunt abdominal trauma. Trauma Surg Acute Care Open. 2017;2(1–7). [CrossRef]
- Page N, Roloff K, Modi AP, et al. Management of Placental Abruption Following Blunt Abdominal Trauma. Cureus. 2020;12(9). [CrossRef]
- Suchecki G, Tilden H, Roloff K, et al. Management of Traumatic Uterine Rupture in Blunt Abdominal Trauma: A Case Report and Literature Review. Cureus. 2020;12:6–13. [CrossRef]
- Greco PS, Day LR, Pearlman MD. Guidance for Evaluation and Management of Blunt Abdominal Trauma in Pregnancy. Obstet Gynecol. 2019;134(6):1343–57. [CrossRef]
- Mendez-Figueroa H, Dahlke JD, Vrees RA, et al. Trauma in pregnancy: An updated systematic review. Am J Obstet Gynecol. 2013;209(1):1–10. [CrossRef]
- Taha E, et al. Blunt abdominal trauma to a pregnant woman resulting in a child with hemiplegic spastic cerebral palsy and permanent eye damage. BMC Res Notes. 2013;6(517). [CrossRef]
- Wortman JR, Uyeda JW, Fulwadhva UP, et al. Dual-energy CT for abdominal and pelvic trauma. Radiographics. 2018;38(2):586–602. [CrossRef]
- Altun G, Pulathan Z, Hemsinli D. Use of the autologous spiral vein graft: a two-stage iliac bypass in a potentially fatal case of pelvic trauma and contaminated tissues. Nagoya J Med Sci. 2019;81(2):331–6. [CrossRef]
- Shojaee M, Sabzghabaei A, Heidari A. Efficacy of new scoring system for diagnosis of abdominal injury after blunt abdominal trauma in patients referred to emergency department. Chin J Traumatol. 2020;23(3):145–8. [CrossRef]
- Deshpande NA, Kucirka LM, Smith RN, Oxford CM. Pregnant trauma victims experience nearly 2-fold higher mortality compared to their nonpregnant counterparts. Am J Obstet Gynecol. 2017;217(5):590.e1-590. [CrossRef]
- Petrone P, Marini CP. Trauma in pregnant patients. Curr Probl Surg. 2015;52(8):330–51. [CrossRef]
- Mattox KL, Goetzl L. Trauma in pregnancy. Crit Care Med. 2005;33(10). [CrossRef]
- Yamada S, Nishijima K, Takahashi J, et al. Intrauterine fetal death caused by seatbelt injury. Taiwan J Obstet Gynecol. 2017;56(4):558–60. [CrossRef]
- Committee on Trauma. American College of Surgeons. Resource for optimal care of the injured patient. Available at: https://www.facs.org/quality-programs/trauma/tqp/center-programs/vrc/resources. Retrieved September 23, 2019.
- Bouyou J, Gaujoux S, Marcellin L, et al. Abdominal emergencies during pregnancy. J Visc Surg. 2015;152. [CrossRef]
- Hill C, Pickingpaugh J. Trauma and surgical emergencies in obstetric patients. Surg Clin N Am. 2008;88(2):421-439. [CrossRef]
- MacArthur B, Foley M, Gray K, et al. Trauma in Pregnancy: A Comprehensive Approach to the Mother and Fetus. Am J Obstet Gynecol. 2019;220(5):465-468.e1. [CrossRef]
- American College of Obstetricians and Gynecologists, Committee Opinion No.723. Guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol 2017;130–5. [CrossRef]
- Ling XS, Anthony Brian Tian WC, Augustin G, Catena F. Can small bowel obstruction during pregnancy be treated with conservative management? A review. World J Emerg Surg. 2024;19(1):13. [CrossRef]
- Coleman JJ, Zarzaur BL. Surgical Management of Abdominal Trauma: Hollow Viscus Injury. Surg Clin North Am. 2017;97(5):1107–17. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).