1. Introduction
Congenital anomalies of the aortic valve (CAAV) are rare, affecting approximately 1–2% of the general population [
1,
2,
3,
4]. Pentacuspid aortic valve (PAV), defined by the presence of five aortic cusps, is the rarest form, with estimated prevalence of less than 1 in a million people [
2]. Most of very few reported PAV cases are associated with valvular dysfunction, primarily aortic regurgitation (AR), and a subset are complicated by ascending aortic aneurysms [
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17]. The pathophysiological mechanisms linking abnormal cusp morphology and aortopathy remain incompletely understood but may share features with those seen in bicuspid aortic valve (BAV) related aortopathy [
3,
18,
19].
This case report describes a patient with severe AR and ascending aortic aneurysm caused by a functionally pentacuspid valve and discusses its clinical and surgical implications in the context of available literature.
2. Case Presentation
A 39-year-old male presented with symptoms of exertional dyspnea, orthopnea, and episodes of shortness of breath. Ten months prior to admission, he experienced pulmonary edema, which was managed medically at a regional hospital. The patient had no known comorbidities but was an active smoker.
Upon admission, he was normotensive (blood pressure 120/70 mmHg) and receiving the following medications: bisoprolol 2.5 mg once daily, ramipril 2.5 mg once daily, atorvastatin 20 mg once daily, furosemide once daily, and spironolactone 25 mg once daily. Electrocardiogram showed sinus rhythm with a heart rate of 76 beats per minute.
Transthoracic echocardiography (TTE) revealed a left ventricular end-diastolic diameter (LVEDD) of 65 mm and end-systolic diameter (LVESD) of 48 mm, with a preserved ejection fraction (LVEF) of 56%. Severe aortic regurgitation (grade 4+) was present, with an effective regurgitant orifice area (EROA) of 0.41 cm², regurgitant volume (RV) of 65 mL/beat, and regurgitant fraction (RF) of 52% [
20]. The aortic annulus measured 27 mm, the sinotubular junction 40 mm, and the ascending aorta 54 mm. Mild mitral and tricuspid regurgitations (1+) were observed, with a systolic pulmonary artery pressure of 58 mmHg. The aortic valve was functionally described as bicuspid, though leaflet morphology was not clearly defined. Coronary angiography revealed normal coronary arteries.
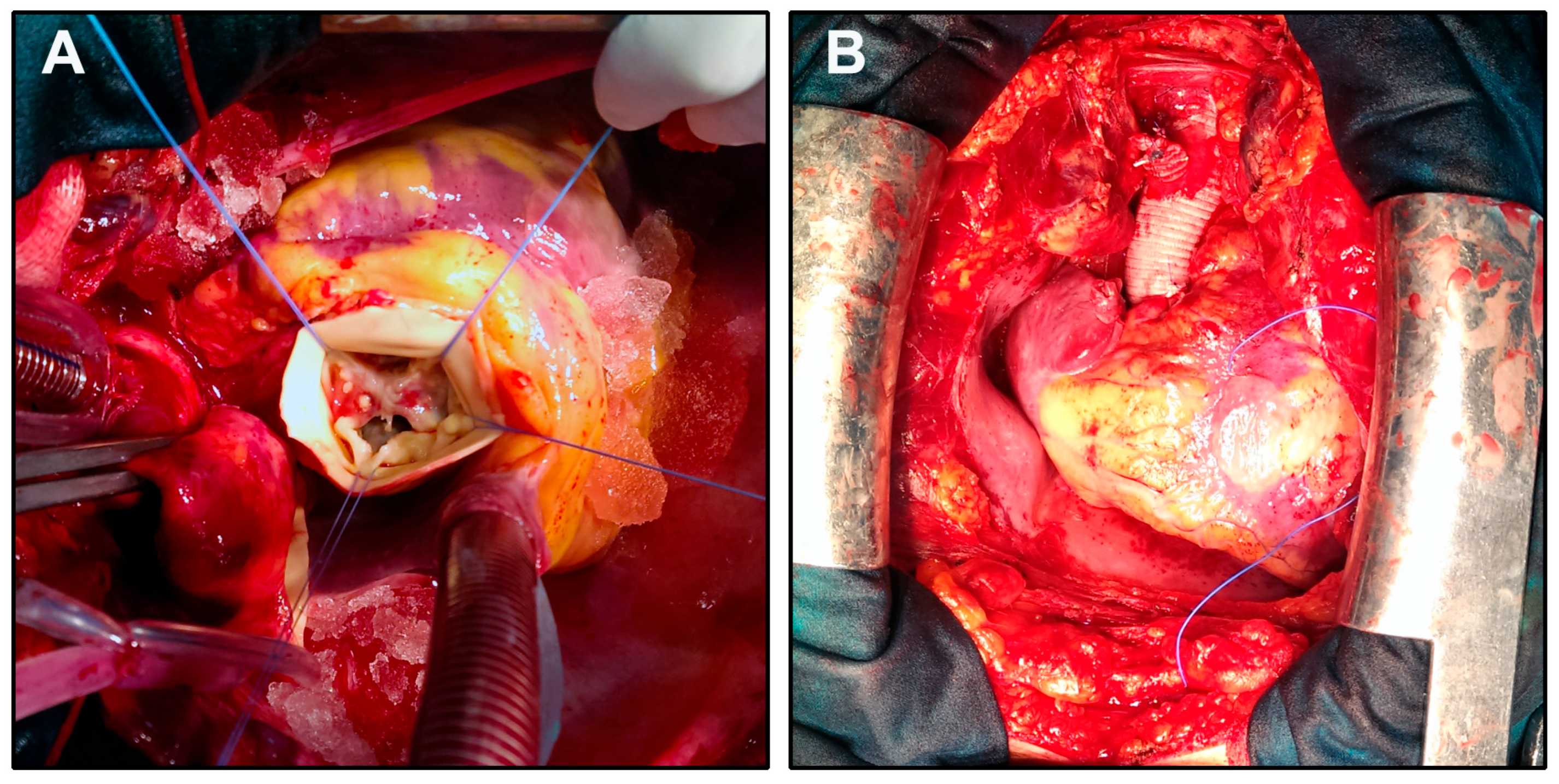
The patient underwent surgery via anterograde partial cardiopulmonary bypass (CPB). A Bentall procedure with hemiarch replacement was performed using a composite On-X Ascending Aortic Prosthesis (25 mm) with Vascutek Gelweave Valsalva Graft (26 mm) (Terumo Cardiovascular Systems, Ann Arbor, MI). The cardiopulmonary bypass time was 185 minutes, aortic cross-clamp (ACC) time 105 minutes, and circulatory arrest (CA) time 10 minutes (open distal anastomosis) at a core temperature of 19°C and jugular venous oxygen saturation of 100% (
Figure 1). Intraoperative transesophageal echocardiography (TEE) showed normal prosthetic valve function and satisfactory hemodynamic performance.
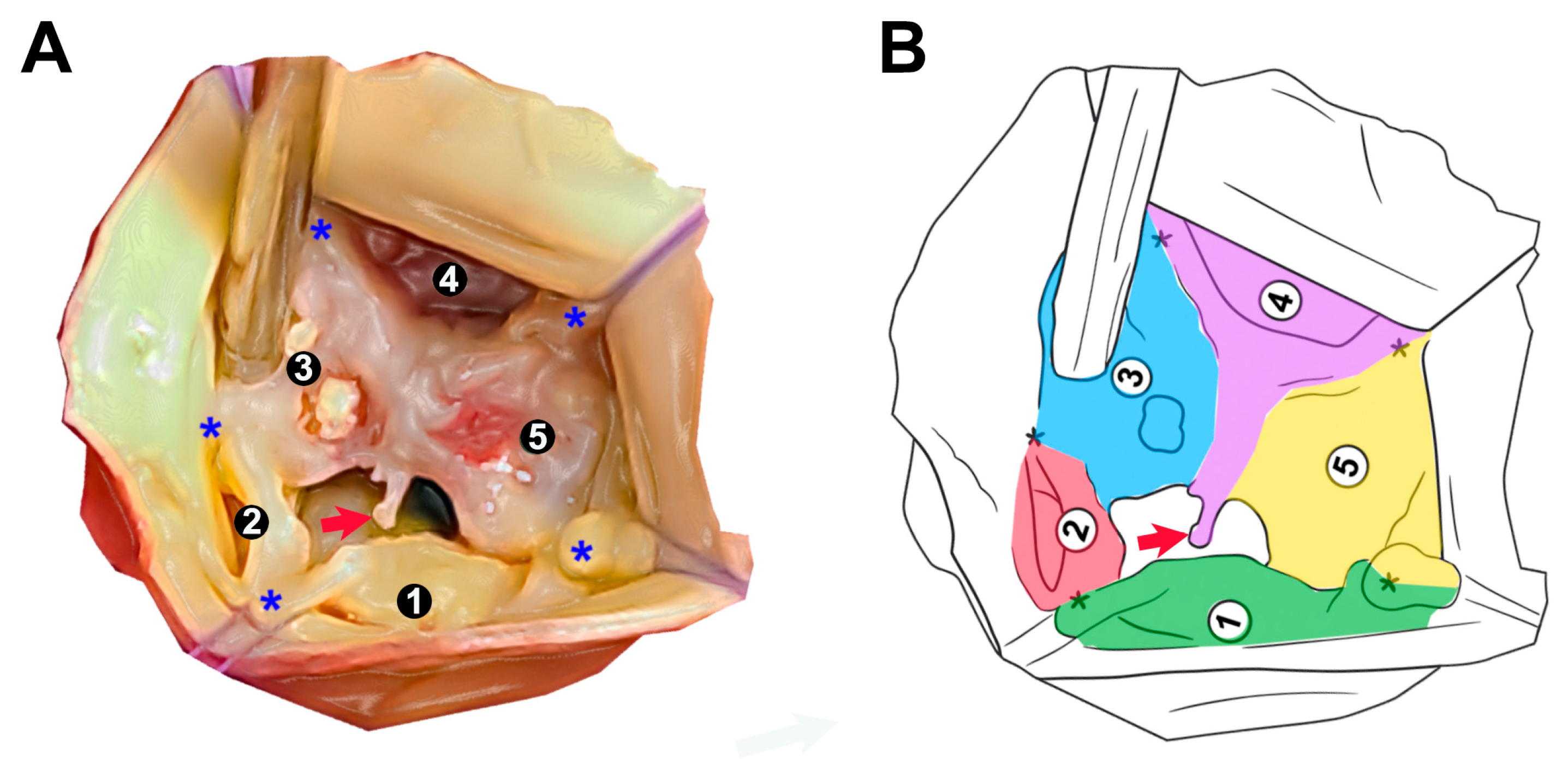
Intraoperative aortic root analysis (
Figure 2) revealed a severely dysmorphic PAV with five identifiable cusp regions of irregular sizes and partial fusion predisposing central malcoaptation and eccentric aortic regurgitation. Cusp 1 (green) appears well-developed and free-standing, corresponding with non-coronary cusp of normal, tricuspid valve, with true commissures towards neighboring cusps. Cusp 2 (red) is the smallest accessory cusp. Between cusps 3 (blue), 4 (purple), and 5 (yellow), there appears to be a fusion zone forming raphe-like structures. The commissures between these cusps are asymmetric and seem shallower or less developed, consistent with pseudocommissures [
4]. Partial cusp fusion is visible between cusps 2 and 3. Anomalous cord, extending from the raphe of the conjoined cusp, is protruding into excentric orifice [
21]. Present morphology with cusp asymmetry and fusion is likely to exhibit bicuspid physiology, as seen on TEE.
The postoperative period was marked by prolonged leukocytosis and neutrophilia (until postoperative day 6), with leukocyte counts to 19×10⁹/L and neutrophils up to 85%. A de-escalation antibiotic regimen including vancomycin and meropenem was administered. The patient remained afebrile throughout hospitalization. Urine and blood cultures, as well as surgical wound swabs, were negative for infection. Upon normalization of white blood cell counts (Leu 9.1×10⁹/L, Neu 65.7%), the patient was discharged on postoperative day 13 in stable hemodynamic condition and without signs of systemic or local infection.
At 11-year follow-up, the patient remains in good general condition with normal function of the aortic prosthesis and preserved left ventricular systolic function.
3. Discussion
Structural CAAV affect approximately 1–2% of the general population, with BAV being the most common, occurring in 0.5–1.4% of individuals [
22,
23]. Unicuspid aortic valve (UAV) is considerably rarer, with an estimated prevalence of 0.02% [
24], while quadricuspid aortic valve (QAV) is observed in 0.003–0.013% of the population [
25]. In contrast, PAV is extraordinarily rare, with only isolated case reports in the literature and no robust epidemiological data, suggesting a prevalence likely well below 0.0001%, or fewer than 1 in 1 million [
4]. This extreme rarity has precluded formal population-based prevalence estimates and highlights the need for systematic reporting and surveillance.
Review of 14 reported PAV cases (
Supplementary Material: Table S1) reveals a consistent association between the young age (24–39 years), asymmetric cusp morphology, severe eccentric AR, and aortic dilatation, particularly of the root or ascending aorta, in four (28.6%) cases, including the current report [
6,
9,
10]. Of those, three cases underwent root and ascending aorta reconstructions (i.e. Robicsek, Bentall), in addition to AV replacement [
9,
10]. In our case, the patient underwent a Bentall procedure with hemiarch replacement, which remains the treatment of choice in patients with combined valvular insufficiency and ascending aortic aneurysm [
26]. In this case, the decision to use a mechanical composite graft was appropriate given the patient's young age, preserved ventricular function, and the need for durable correction. The uneventful recovery and excel-lent 11-year follow-up outcome reinforce the long-term efficacy of this approach when tailored appropriately.
The observed asymmetry, including a rudimentary cusp (Cusp 2) and raphe formation between cusps 3, 4, and 5 (
Figure 2), supports the hypothesis that cusp malformation and fusion contribute to poor coaptation and progressive AR [
4]. In addition, the anomalous cord arising from the raphe’s free margin, and floating within the regurgitant orifice (
Figure 2), adds a unique structural abnormality not previously described with PAV. Similar structure, with its free portion attached to the aorta, has been documented in some BAV cases, contributing to chronic and acute AR [
21].
The co-occurrence of root and ascending aortic dilatation in current and previously reported cases, contribute to the hemodynamic burden on the aortic wall, either directly (via eccentric regurgitant jets) or indirectly (through altered flow patterns and wall stress), promoting aneurysmal formation and remodeling [
4]. There is also accumulating evidence that CAAV share some genetics and embryological defects involving both valvulogenesis and aortic wall maturation, predisposing aortopathy. Rare histological examination of the resected PAV demonstrated myxomatous degeneration, may support possible underlying connective tissue abnormality [
27].
Associated congenital anomalies were reported in two cases: patent foramen ovale [
8], and renal arteries dysplasia [
13].
Despite the rarity of PAV, this case underscores the importance of considering it in the differential diagnosis of unexplained AR, especially in young people and when associated with ascending aortic dilation. Preoperative recognition remains difficult but may improve with advances in imaging techniques such as 3D echocardiography, MDCT and cardiac MRI, which can better delineate commissural architecture and leaflet morphology [
28].
4. Conclusions
Pentacuspid aortic valve (PAV) represents an exceptionally rare congenital anomaly, most often presenting with asymmetric cusp morphology, severe aortic regurgitation, and, in a subset of patients, ascending aortic dilatation. Review of the literature reveals a reproducible pattern of functional insufficiency and structural aortopathy, frequently necessitating combined valvular and aortic surgical intervention. These findings suggest a pathophysiological overlap with BAV–associated aortopathy and support the notion that PAV should be approached as a valvulo-aortic disease entity.
However, current understanding is severely limited by the rarity of PAV, lack of centralized registries, heterogeneous reporting, and scarce histological or genetic characterization. As a result, long-term outcomes, optimal timing of intervention, and risk stratification remain largely undefined.
Future efforts should prioritize the development of multicenter registries and standardized morphological classification schemes. Advanced imaging techniques may enhance preoperative recognition, while systematic histological and molecular investigations could uncover developmental or genetic substrates underlying PAV and its associated aortopathy. Such coordinated strategies are essential to transition PAV from an anecdotal curiosity to a better-understood clinical and surgical entity.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table S1: Literature review of the reported PAV cases.
Funding
This research received no external funding.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hinton, R.B.; Yutzey, K.E. Heart valve structure and function in development and disease. Annu Rev Physiol 2011, 73, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Perloff, J.K. The Howard Gilman Foundation Lecture. Where have we come from and where are we going? Valve management past, present and future. Adv Cardiol 2004, 41, 1–8. [Google Scholar] [CrossRef]
- Michelena, H.I.; Corte, A.D.; Evangelista, A.; Maleszewski, J.J.; Edwards, W.D.; Roman, M.J.; Devereux, R.B.; Fernández, B.; Asch, F.M.; Barker, A.J.; et al. International Consensus Statement on Nomenclature and Classification of the Congenital Bicuspid Aortic Valve and Its Aortopathy, for Clinical, Surgical, Interventional and Research Purposes. Radiology: Cardiothoracic Imaging 2021, 3, e200496. [Google Scholar] [CrossRef]
- Dallard, J.; Boodhwani, M.; Labrosse, M. Aortic Valve Mechanics. In Cardiovascular Mechanics. In Cardiovascular Mechanics, Labrosse, M., Ed.; CRC Press/Taylor & Francis Group: Boca Raton, FL, 2019; pp. 279–318. [Google Scholar]
- Simonds, J. Congenital malformations of the aortic and pulmonary valves. The American Journal of the Medical Sciences (1827-1924) 1923, 166, 584. [Google Scholar] [CrossRef]
- Bogers, J.J.; Aytug, Z.; Hendriks, F.F.; Huysmans, H.A. Quinticuspid aortic valve causing aortic valve incompetence and stenosis. Thorax 1982, 37, 542–543. [Google Scholar] [CrossRef] [PubMed]
- Yates, A. Editorial comment. J Cardiovasc Surg (Torino) 1984, 25, 254. [Google Scholar] [CrossRef]
- Cemri, M.; Cengel, A.; Timurkaynak, T. Pentacuspid aortic valve diagnosed by transoesophageal echocardiography. Heart 2000, 84, E9. [Google Scholar] [CrossRef]
- Meng, Y.; Zhang, L.; Zhang, Z.; Wang, Y.; Yang, X. Cardiovascular magnetic resonance of quinticuspid aortic valve with aortic regurgitation and dilated ascending aorta. J Cardiovasc Magn Reson 2009, 11, 28. [Google Scholar] [CrossRef]
- Wang, S.; Meng, X.; Zhang, H.; Wang, J.; Han, J. Pentacuspid Aortic Valve With Severe Aortic Regurgitation. The Annals of Thoracic Surgery 2010, 89, 2034–2036. [Google Scholar] [CrossRef]
- Kuroki, H.; Hirooka, K.; Ohnuki, M. Pentacuspid aortic valve causing severe aortic regurgitation. The Journal of Thoracic and Cardiovascular Surgery 2012, 143, e11–e12. [Google Scholar] [CrossRef]
- Ozyilmaz, S.; Akgul, O.; Guzeltas, A.; Ozyilmaz, I. Diagnosis of pentacuspid aortic valve with severe regurgitation using three-dimensional transesophageal echocardiography. Echocardiography 2015, 32, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Patanè, F.; Ceresa, F.; Ferrazzo, G.; de Gregorio, C. Pentacuspid aortic valve associated with bilateral renal artery dysplasia. J Cardiovasc Med (Hagerstown) 2020, 21, 717–719. [Google Scholar] [CrossRef] [PubMed]
- Al Ansari, A.E.; Abdulrahman, A.; Shaikho, N.M.G.; Saif, S.A. A very rare cause of aortic regurgitation: pentacuspid aortic valve. Eur Heart J Case Rep 2021, 5, ytab038. [Google Scholar] [CrossRef]
- Beddingfield, R.H.; Rashid, Z.A.; Pagel, P.S. A Five-Leaf Clover or an Exceptionally Rare Cause of Severe Aortic Insufficiency? Journal of Cardiothoracic and Vascular Anesthesia 2022, 36, 4534–4537. [Google Scholar] [CrossRef]
- Motoki, T.; Ikeno, Y.; Suehiro, Y.; Kurushima, A.; Okita, Y.; Fukumura, Y. A successful repair of pentacuspid aortic valve. JTCVS Tech 2022, 14, 69–72. [Google Scholar] [CrossRef]
- Albogmi, D.M.; Alharthi, D.A.; Alharbi, D.M.; Alareef, D.M.; Aldohan, D.M. Case Report of a Pentacuspid Aortic Valve with Aortic Insufficiency. International Journal of Applied Science and Research 2023, 6, 27–30. [Google Scholar] [CrossRef]
- Ahmed, A.; Wang, T.K.M. Non-Trileaflet Aortic Valve Aortopathies. Life 2025, 15, 713. [Google Scholar] [CrossRef]
- Henderson, D.J.; Eley, L.; Chaudhry, B. New Concepts in the Development and Malformation of the Arterial Valves. Journal of Cardiovascular Development and Disease 2020, 7, 38. [Google Scholar] [CrossRef]
- Lancellotti, P.; Tribouilloy, C.; Hagendorff, A.; Popescu, B.A.; Edvardsen, T.; Pierard, L.A.; Badano, L.; Zamorano, J.L. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2013, 14, 611–644. [Google Scholar] [CrossRef]
- Vowels, T.J.; Gonzalez-Stawinski, G.V.; Ko, J.M.; Trachiotis, G.D.; Roberts, B.J.; Roberts, C.S.; Roberts, W.C. Anomalous cord from the raphe of a congenitally bicuspid aortic valve to the aortic wall producing either acute or chronic aortic regurgitation. J Am Coll Cardiol 2014, 63, 153–157. [Google Scholar] [CrossRef]
- Sillesen, A.S.; Vøgg, O.; Pihl, C.; Raja, A.A.; Sundberg, K.; Vedel, C.; Zingenberg, H.; Jørgensen, F.S.; Vejlstrup, N.; Iversen, K.; et al. Prevalence of Bicuspid Aortic Valve and Associated Aortopathy in Newborns in Copenhagen, Denmark. Jama 2021, 325, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Rizza, V.; Ancona, F.; Ingallina, G.; Stella, S.; Margonato, D.; Tavernese, A.; Belli, M.; Biondi, F.; Fiore, G.; Barki, M.; et al. Prevalence, clinical characterization, management and evolution of bicuspid aortic valve classified according to the 2021 International Consensus Statement in a tertiary care hospital. European Journal of Cardio-Thoracic Surgery 2025, 67. [Google Scholar] [CrossRef] [PubMed]
- Kumanayaka, D.D.; Otto, A.; Chauhan, M.; Belinschi, V.; Mirza, N.; Rayad, M.N.; Suleiman, A. Unicuspid Aortic Valve, an Extremely Rare Congenital Anomaly in Adults: A Systemic Review. World Journal of Cardiovascular Diseases 2023, 13, 283–288. [Google Scholar] [CrossRef]
- Janssens, U.; Klues, H.G.; Hanrath, P. Congenital quadricuspid aortic valve anomaly associated with hypertrophic non-obstructive cardiomyopathy: a case report and review of the literature. Heart 1997, 78, 83–87. [Google Scholar] [CrossRef]
- Vendramin, I.; Bortolotti, U.; De Manna, D.N.; Lechiancole, A.; Sponga, S.; Livi, U. Combined Replacement of Aortic Valve and Ascending Aorta-A 70-Year Evolution of Surgical Techniques. Aorta (Stamford) 2021, 9, 118–123. [Google Scholar] [CrossRef]
- Messner, B.; Bernhard, D. Bicuspid aortic valve-associated aortopathy: Where do we stand? Journal of Molecular and Cellular Cardiology 2019, 133, 76–85. [Google Scholar] [CrossRef]
- D’Alonzo, M.; Grande, A.M.; Casale, I.; Fiore, A. Multimodal imaging in the assessment of quadricuspid aortic valve. Journal of Cardiothoracic Surgery 2025, 20, 148. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).