1. Introduction
Communication is central to a child’s development, serving as a foundation for learning, emotional expression, and participation in social life. From early gestures and joint attention to complex discourse, communicative competence supports not only academic growth but also identity formation and social inclusion (Reilly & McKean, 2023). However, for a significant number of children and adolescents, communication disorders (CDs) interrupt these developmental trajectories. These disorders – including speech sound disorder, developmental language disorder (DLD), pragmatic language impairments, and fluency disorders (i.e., stuttering) – affect approximately 7% of the paediatric population (Gallagher, 2023). Children with CDs often experience challenges that extend beyond language, influencing peer interactions, emotional regulation, and mental well-being (Gibbard et al., 2024).
The intersection between communication and mental health is well-documented, though still insufficiently understood. Multiple studies suggest that children with CDs are more likely to experience internalising and externalising difficulties such as anxiety, depression, aggression, and social withdrawal (e.g., Clarke, 2021; Channell & Bosley, 2022; Toseeb et al., 2020). For instance, pragmatic language impairments have been linked to elevated social anxiety, while expressive language difficulties are associated with behavioural frustration and peer conflict (Bella, 2022). Adolescents who stutter often report reduced self-esteem and increased mental distress, especially in the absence of integrated psychological and speech-language support (Jones et al., 2021; Myrberg, 2020). Moreover, caregivers of children with CDs frequently report higher levels of stress, emotional burnout, and difficulty accessing coordinated services (Rahman et al., 2020; Cocquyt et al., 2024).
Despite a surge of empirical interest in the communication–mental health nexus, the research landscape remains fragmented. Studies vary in how they define and measure both communication and mental health constructs, leading to a lack of comparability across findings (e.g., Cutting, 2023; Reetzke, 2022). While some focus on diagnostic categories (e.g., DLD, ASD-Autism Spectrum Disorder, Attention Deficit Hyperactivity Disorder-ADHD), others examine functional traits (e.g., social withdrawal, emotional lability), and only a few employ a transdiagnostic lens. Interventions are similarly diverse, ranging from individual therapy to school-based programs, yet systematic insights into what works, for whom, and under what conditions remain limited (MacEvilly et al., 2024). Furthermore, populations such as culturally and linguistically diverse (CALD) children and those with co-occurring disabilities are underrepresented in this body of work (Feehan & Charest, 2024).
Several recent studies attempted to address aspects of this relationship between communication and mental health. For example, Dillon et al. (2021) explored the role of language in adolescent well-being, while Xiao et al. (2023) examined associations between early communication and emotional-behavioural outcomes. However, few have adopted a broad developmental and diagnostic scope while specifically examining how communication difficulties relate to mental health trajectories in children and adolescents. To date, no study that we could find has synthesised findings across diagnostic boundaries, communication domains (expressive, receptive, pragmatic, and fluency), and mental health constructs to provide a comprehensive map of this complex intersection.
This scoping review addresses this gap. Following the PRISMA Extension for Scoping Reviews (PRISMA-ScR) and guided by Arksey and O’Malley’s (2005) framework, this review synthesises peer-reviewed empirical studies on the relationship between communication disorders and mental health outcomes in children and adolescents. Specifically, it aims to:
Identify and describe how different types of communication disorders are associated with emotional and behavioural well-being.
Thematise common findings and distinctions across communication profiles.
Highlight implications for clinical practice, educational support, and interdisciplinary policy development.
2. Methods
The use of the PRISMA-ScR and Arksey and O’Malley’s (2005) methodological framework, was enhanced as suggested by Levac and colleagues (2010). Specifically, the review mapped and then synthesised peer-reviewed empirical research examining the relationship between communication disorders and mental health in children and adolescents. Given the diversity of definitions, populations, and assessment tools in the field, a scoping approach was considered most appropriate to provide a comprehensive overview of the literature for the purpose of identifying key themes for future investigation (Munn et al., 2018).
The primary research question guiding the review was: “What is the nature of the relationship between communication disorders and mental health outcomes in children and adolescents?” It explores how different types of communication difficulties (expressive, receptive, pragmatic, and fluency-related) are associated with internalising or externalising mental health symptoms, and how these associations vary across contexts, age groups, and diagnostic categories.
Studies were considered eligible for inclusion if they were peer-reviewed empirical investigations published in English between 2000 and 2024, with a primary focus on individuals under 18 years. Eligible studies needed to examine one or more communication disorders as defined by the American Speech-Language-Hearing Association (ASHA;
https://www.asha.org/policy/rp1993-00208/?srsltid=AfmBOoreB78T638WUtsZrAdIzZljf4-QCY-KVpbTagcXxGOESWFx2ike) and include at least one outcome related to mental health, such as anxiety, depression, behavioural difficulties, social withdrawal, or well-being. Quantitative, qualitative, and mixed-methods studies were eligible, provided that communication and mental health variables were both directly measured and/or meaningfully discussed. Studies were excluded if they focused solely on adult populations, described unrelated medical or developmental conditions, or were review articles, theoretical papers, editorials, and conference abstracts.
The search strategy was developed iteratively in consultation with a research librarian to ensure comprehensive coverage of the relevant literature. The final search was conducted in November 2024 across five databases: PubMed, PsycINFO, ERIC, CINAHL, and Scopus. The search terms combined key concepts related to communication disorders (e.g., “language disorder”, “speech impairment”, “pragmatic communication”, “stuttering”) and mental health outcomes (e.g., “anxiety”, “depression”, “emotional wellbeing”, “behaviour problems”) using Boolean operators. Terms were adapted for each database and included both subject headings and free-text terms. The full search strategy for each database is reported in
Table 1.
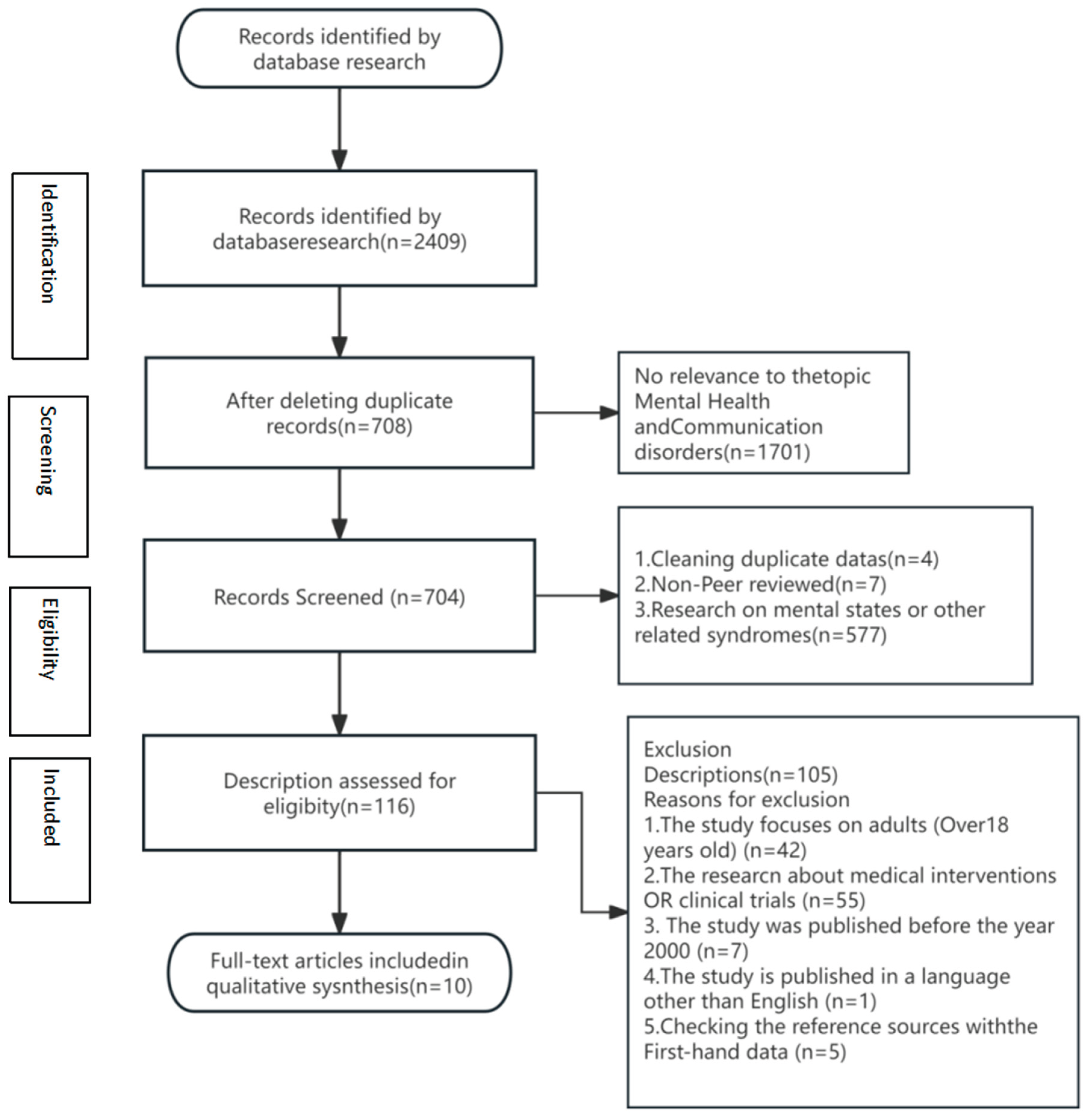
All search results were exported into EndNote, and duplicates were removed before screening. Title and abstract screening were completed independently by authors 1 and 2, who then proceeded to full-text screening for all articles deemed potentially relevant. Discrepancies were resolved through consensus discussion, with author 3 consulted where necessary. A total of 2,409 records were initially identified. After removing duplicates and screening titles and abstracts, 52 full-text articles were assessed for eligibility. Ten studies met the inclusion criteria and were included in the final synthesis. The selection process is summarised in the PRISMA flow diagram (
Figure 1).
The PRISMA flow chart provides key information related to the objectives or questions of the scoping review, such as describing the results of the search strategy and selection process (Peters et al., 2020). Key variables extracted from each study included: author(s), publication year, country, study design, participant characteristics (including age and diagnostic group), type of communication disorder, mental health outcome(s) measured, assessment tools used, and key findings relevant to the review aims. The data extraction form was piloted with three studies to ensure consistency and minor adjustments were made before proceeding with full data charting. Each study was independently charted by author 1 and verified by author 2 to enhance reliability. The final data extraction domains are presented in
Table 2.
An inductive thematic analysis was conducted to synthesise findings across the included studies. The process of integrating, categorising, and thematically organising data facilitates the interpretation of thematic directionality and systematic exploration within research (Williams & Moser, 2019). The process focused on the nature and direction of the relationship between communication and mental health outcomes, the specific communication profiles involved (e.g., pragmatic vs. expressive), the developmental stage of participants, and the role of contextual or mediating variables such as family stress, school environment, or co-occurring conditions. Themes were developed iteratively and refined through multiple rounds of discussion among the review team.
Table 3 provides an overview of the study characteristics for the final ten included studies.
While this review does not include a formal quality appraisal of the included studies, the research team critically engaged with methodological differences and limitations in the interpretation of findings (Peters et al., 2021). The scope and limitations of the evidence base are discussed transparently in later sections of the paper. By systematically mapping current evidence and identifying key patterns across communication domains and mental health outcomes, this scoping review seeks to inform clinicians, researchers, educators, and policymakers working at the interface of child development, language, and well-being.
3. Results
The ten studies included in this review spanned diverse populations, methodological designs, and communicative profiles, yet shared a common concern with the interplay between language and socio-emotional functioning and their relationship to mental health outcomes in children and adolescents. Across studies, communication disorders were not only associated with a higher prevalence of emotional and behavioural difficulties but were also embedded in complex relational and systemic contexts. Through an inductive thematic analysis of the findings, four interrelated themes were identified that characterise the ways communication and mental health challenges intersect in the lives of children and adolescents.
3.1. Theme 1: Emotional and Behavioural Manifestations
Across the reviewed studies, emotional and behavioural concerns emerged as a consistent correlate of communication disorders in children and adolescents. Participants with expressive, receptive, or mixed language impairments were frequently reported to exhibit symptoms of anxiety, emotional dysregulation, irritability, and behavioural frustration. In the study by Hahn et al. (2015), children with language impairment demonstrated significantly elevated internalising behaviours, including sadness, worry, and withdrawal, as compared to their typically developing peers, as rated by both parents and teachers. These emotional difficulties often co-occurred with academic underachievement and reduced classroom participation. MacEvilly et al. (2024) demonstrated that group interventions can enhance emotional regulation and social communication in young children. However, they also found that language and communication barriers in young children can lead to increased internalised behaviours and decreased external interactions, potentially resulting in isolated emotional activities and heightened negative emotions.
Similar findings were echoed by Cola et al. (2022), whose work on young children with language delays highlighted the presence of sustained affective symptoms, including persistent low mood and emotional lability. In some cases, these symptoms preceded formal mental health diagnoses, suggesting that emotional challenges may emerge early in the trajectory of communication difficulties. Pereira et al. (2022) also reported that children with language disorders performed significantly higher on standardised behavioural assessments of emotional distress and conduct difficulties, which raised concerns about their long-term psychosocial development.
The nature of these associations appears to be both direct and mediated. For example, Maljaars et al. (2012) observed that even in the absence of a formal mental health diagnosis, children with expressive and receptive difficulties displayed increased aggression and hyperactivity, possibly reflecting frustration associated with their inability to communicate effectively. This behavioural dysregulation often resulted in exclusionary responses from peers and disciplinary actions in educational settings, which further reinforced the emotional toll.
Taken together, the evidence suggests that emotional and behavioural symptoms in children with communication disorders are not peripheral but integral to their developmental profile. The findings emphasise the need for early identification of affective difficulties within speech-language assessments and underscore the potential for mental health symptoms to escalate in the absence of coordinated intervention.
3.2. Theme: The Social Burden of Pragmatic and Expressive Difficulties
The second theme emerging from the synthesis is the significant social burden associated with pragmatic and expressive communication impairments. Children who struggled to initiate, sustain, or interpret social communication were consistently described as being at risk of social exclusion, peer victimisation, and reduced friendship quality. These difficulties often led to internalised distress and negative self-perception.
Gillott et al. (2004) highlighted that children with pragmatic language deficits showed higher levels of loneliness and fewer reciprocal friendships compared to their neurotypical peers. The social withdrawal documented in their study was not simply a function of language ability, but rather a reflection of the child’s perceived social competence and fear of negative evaluation. In the study by Charman et al. (2015), children with social communication difficulties were more likely to experience peer rejection and bullying, which in turn were strongly associated with symptoms of anxiety and depression. The authors emphasised the cumulative impact of repeated negative social encounters, particularly for children lacking access to peer-mediated or school-based support. Luyster et al. (2008) similarly documented that children with pragmatic language impairments often misinterpreted social cues, which exacerbated peer misunderstandings and intensified feelings of frustration and social vulnerability.
Notably, these findings suggest that the social consequences of communication disorders are not merely incidental but form a central pathway through which mental health difficulties develop and are maintained. The reviewed studies point to the need for interventions that explicitly address social communication skills in tandem with emotional coping strategies, particularly in educational environments where peer interaction is critical.
3.3. Theme 3: Family and Environmental Stressors
The third theme concerns the bidirectional and compounding nature of risk factors experienced by children with communication disorders and their families. Rather than operating in isolation, communication difficulties and mental health concerns were found to interact within broader psychosocial environments, particularly in family systems where stress, limited resources, or unmet service needs were present.
Lecavalier et al. (2006) suggested that parental stress levels were significantly higher among caregivers of children with both language impairments and emotional difficulties compared to those raising children with language difficulties alone. These caregivers may feel overwhelmed by the dual burden of managing communication challenges and supporting their child’s emotional well-being, especially in contexts where access to specialised care is inconsistent or fragmented.
This cyclical dynamic—whereby a child’s limited communicative repertoire exacerbated behavioural distress, which in turn intensified parental frustration—was a recurring concern in qualitative data. Family-level challenges were also influenced by structural and systemic barriers. Houghton et al. (2013), for example, noted that families often struggled to navigate siloed health and education services, potentially leading to gaps in care that undermined both communication support and emotional regulation. These systemic issues were particularly pronounced for families from lower socioeconomic backgrounds or those residing in rural areas.
It is highlighted how communication and mental health challenges are embedded within broader ecological systems. Family stress, limited service access, and breakdowns in interprofessional collaboration often act as mediators that exacerbate child-level difficulties. These findings underscore the importance of adopting a family-centred, ecologically informed approach in both assessment and intervention planning.
3.4. Theme 4: Intervention Gaps and the Need for Integrated Care
The final theme centres on the limitations of current intervention models and the call for more integrated, interdisciplinary care. Despite strong evidence of the interdependence between communication and mental health, few studies reported interventions that simultaneously addressed both domains. Most speech-language therapy services described in the included studies focused narrowly on linguistic or articulatory targets, often without consideration of the child’s emotional state or psychological support needs.
While emotional distress is often identified in children with communication disorders, referral pathways to mental health services were inconsistent and poorly coordinated (Charman et al., 2015). Caregivers may also be unaware that speech and emotional concerns could be addressed jointly, resulting in fragmented care and delayed psychological support (Cola et al., 2022). A notable concern raised across studies was the lack of school-based or community programs that support both communication competence and emotional well-being. While there is potential for classroom-level interventions to promote social-emotional learning among children with communication difficulties (Cola et al. 2022), few programs have been formally trialled or evaluated in this population. This reflects a broader gap in the literature and practice: the absence of dual-focus models that bridge developmental, educational, and psychological disciplines.
The findings point to a pressing need for interdisciplinary models of care that position speech-language therapists, psychologists, educators, and families as collaborative agents in a child’s development. Such models could support timely screening, reduce service duplication, and ensure that emotional well-being is treated as integral—rather than incidental—to communicative functioning.
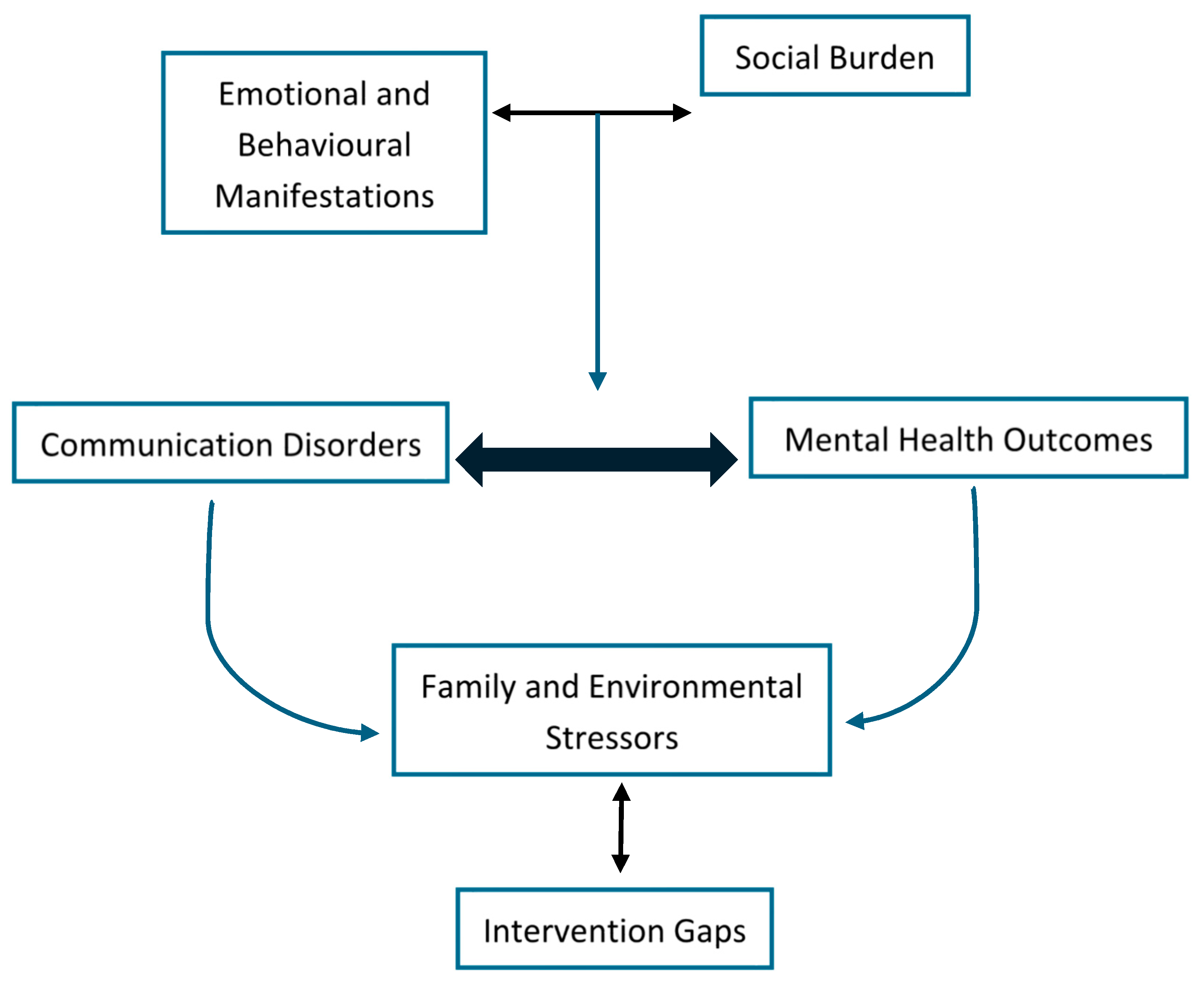
3.5. Intersecting Pathways of Communication and Mental Health: The Conceptual Framework
The four themes coalesce into a conceptual framework that maps the dynamic and reciprocal relationships between communication disorders and mental health outcomes in children and adolescents. This framework (see
Figure 2) positions communication impairments (whether expressive, receptive, pragmatic, or fluency-based) as core developmental vulnerabilities that shape and are shaped by emotional well-being, social environments, and systemic supports.
At the foundation of the model lies Theme 1, where communication difficulties are directly associated with internalising and externalising symptoms such as anxiety, mood disturbance, and behavioural dysregulation. These difficulties, in turn, restrict children’s ability to engage meaningfully in everyday settings, leading to cumulative emotional strain. Building on this foundation, Theme 2 highlights how pragmatic and expressive impairments carry a particular burden in the social domain. Children with these challenges frequently encounter peer rejection, miscommunication, and reduced social reciprocity, which not only intensify emotional difficulties but also contribute to the development of a negative self-concept. Theme 3 extends this interaction to the family and environmental level. The distress experienced by children is often mirrored by or compounded within their caregiving systems. Parents and guardians experience emotional fatigue, limited access to integrated care, and systemic navigation challenges. These stressors create feedback loops that reinforce communication and behavioural challenges over time. Finally, Theme 4 underscores the absence of coordinated care models that recognise and respond to these intersecting needs. Without integrated interventions, children and families are left to navigate fragmented services, delaying support and amplifying the developmental impact of both communication and mental health challenges.
Collectively, this framework illustrates that communication disorders do not operate in isolation. Rather, they participate in a network of reinforcing factors that impact mental health, functioning, and quality of life. Interventions targeting only one dimension risk overlooking the broader ecosystem of needs experienced by these children and their families.
4. Discussion
This review examined the complex relationship between communication disorders and mental health difficulties in children and adolescents, synthesising insights from current research and contextualising them within a broader body of literature. The findings underscore the multifaceted and interdependent nature of these challenges, which manifest not only at the individual level but also across social, familial, and systemic domains. In this section, we interpret the key themes identified, relate them to existing research, and consider their implications for future directions in research, practice, and policy.
4.1. Revisiting the Communication-Mental Health Nexus
The findings of this review confirm and extend the well-documented yet complex relationship between communication disorders and mental health challenges in childhood and adolescence. While the co-occurrence of these two domains is acknowledged in the literature, the present synthesis demonstrates that emotional and behavioural difficulties are not merely coexisting conditions, but rather are often intertwined consequences of communicative breakdown, social disconnection, and systemic limitations. This interaction was evident across all types of communication disorders examined, including expressive and receptive language difficulties, pragmatic language impairments, and fluency disorders.
The results reinforce that children with communication disorders are at elevated risk of both internalising and externalising symptoms. Across the included studies, anxiety, withdrawal, low mood, and behavioural frustration were frequently observed. Importantly, these mental health symptoms were not only secondary to communication difficulties; in some cases, they appeared concurrently or even prior to formal diagnosis, suggesting a mutually reinforcing developmental pathway. This aligns with evidence (e.g., Reetzke, 2022) indicating that communication deficits and mental health concerns in early childhood may share neurodevelopmental origins, with cascading effects over time. This argues for a transdiagnostic perspective, where cognitive-affective vulnerabilities contribute to both domains simultaneously (Channell and Bosley, 2022).
Moreover, the review adds to emerging work that challenges the assumption that communication impairment alone accounts for poor social or emotional outcomes. It shows the child’s social environment, peer responses, and access to support are equally important in shaping outcomes. The current synthesis contributes to this literature by mapping how these contextual influences interact with core communication profiles to heighten or mitigate psychological vulnerability.
Overall, the review supports a reframing of communication disorders, not merely as isolated developmental delays, but as potential drivers of broader emotional, behavioural, and psychosocial difficulties. This reconceptualisation carries significant implications for clinical assessment, which must attend to signs of emotional distress alongside speech-language profiles, and for early intervention approaches that are responsive to both communicative and emotional needs from the outset (Caban, et al., 2023).
4.2. Social and Family Systems as Mediators of Risk
This review highlights that the relationship between communication disorders and mental health difficulties is not shaped solely by individual impairments, but by the broader social and familial contexts in which children develop. Across the included studies, peer rejection, poor friendship quality, caregiver stress, and family coping difficulties consistently emerged as influential mediators that intensified the emotional burden associated with communicative challenges.
Children with pragmatic language impairments or expressive delays were particularly vulnerable to social exclusion and peer conflict. These findings align with broader research, such as Clarke (2021) and Channell (2020), who documented that difficulties in understanding or producing socially appropriate language can contribute to breakdowns in peer interaction, which in turn impact self-concept and emotional regulation. Further, adolescents with language difficulties are often found to internalise peer rejection as a personal failure, leading to increased anxiety and reduced help-seeking behaviours (Toseeb et al., 2020).
Family dynamics also played a critical role in shaping child outcomes. For example, caregivers with co-occurring communication and emotional difficulties with their children might show higher levels of stress, exhaustion, and frustration (Lecavalier et al., 2006). These responses often stemmed from persistent communicative breakdowns, difficulty interpreting the child’s needs, and a lack of access to mental health support services. Leitão et al. (2025), for example, indicated that cc than caregivers of typically developing children, with stress compounded by service system delays and inconsistent professional support.
The corpus suggests that the family environment can serve as both a buffer and an amplifier. In emotionally responsive households with coordinated access to intervention, children may experience improved outcomes despite language difficulties. However, in contexts marked by financial hardship, cultural or linguistic mismatch, or limited professional support, these same challenges may escalate. It needs to be emphasised that the accumulation of social and familial stressors—rather than the severity of the communication disorder alone—is often a stronger predictor of negative psychosocial outcomes (Lloyd et al., 2023).
This reinforces the value of ecological models of development (such as Bronfenbrenner’s ecological systems theory; see Fitzsimons & Clark, 2021), which accounts for the interactions between the children, their immediate relationships, and broader societal structures. Interventions that focus only on the child, without considering the family’s coping capacity and the social affordances around them, are unlikely to achieve sustainable improvements. Therefore, a shift toward family-centred and socially informed practice is essential in bridging the gap between communication development and emotional well-being.
4.3. Systemic Barriers and Gaps in Interdisciplinary Practice
Despite growing recognition of the link between communication disorders and mental health among the studies reviewed, the findings still reveal a persistent lack of integration between speech-language pathology and psychological services. Across the included studies, participants and caregivers reported fragmented service delivery, poorly coordinated referral pathways, and limited access to practitioners trained to support both communication and emotional needs. This siloed model of care is at odds with the complex, bidirectional nature of the challenges experienced by children with co-occurring difficulties.
One of the most striking patterns emerging from the review is the absence of routine emotional well-being screening within speech-language therapy settings. Although speech-language pathologists often reported concerns about their paediatric clients’ affective state or behavioural regulation, formal mental health referral processes were inconsistently applied, and few multidisciplinary care plans were implemented. Doody et al. (2017) identified several obstacles to effective care planning and implementation. Privacy and confidentiality were highlighted as primary concerns, alongside the crucial role of trust in interactions with health professionals, which significantly impacts the success of care plans. This echoes the claims (e.g., Carey et al., 2023) that identify considerable variation in Australian interprofessional practices involving speech-language pathologists and other allied health professionals, largely due to jurisdictional differences in service mandates and funding models.
Structural limitations significantly hinder effective care, as highlighted by Langbecker et al. (2020) and Cocquyt et al. (2024). These include long waitlists, insufficient school-based resources, and poor inter-sector communication. Compounding these issues, children often receive initial speech-language services but lack timely access to psychological support unless their symptoms reach a crisis level. This reactive approach neglects the crucial developmental and preventative needs of this population. Meanwhile, while existing programs, e.g., the PICP program, assess language skills, specifically receptive speech and passive coping styles, in children receiving speech and language services, its broader effectiveness needs further exploration. For example, Pereira et al. (2022) observed improved language skills in preschoolers with pragmatic disabilities using this program, but more research is necessary to determine its efficacy across various neurodevelopmental disorders.
There also appears in the corpus a systemic underinvestment in training that prepares professionals to work collaboratively across disciplines. While some school-based programs aim to foster multidisciplinary teams, many practitioners report limited confidence in managing overlapping issues beyond their core expertise (e.g., MacEvilly et al., 2024). As a result, opportunities for early, coordinated, and contextualised support are often missed.
The findings of this review suggest an urgent need to reconceptualise service delivery models for children with communication disorders who present with or are at risk of, mental health concerns. Integrated assessment protocols, joint case planning, and co-delivered interventions should become standard practice rather than exceptional arrangements. Investment in training, policy alignment, and interdisciplinary research is also essential to build evidence-based models that reflect the developmental interdependence of communication and mental health.
4.4. Underrepresented Populations and Equity Concerns
Another critical observation arising from this review is the marked underrepresentation of equity-focused perspectives in the research on communication disorders and mental health. Despite the well-established evidence that social determinants of health, such as socioeconomic disadvantage, cultural and linguistic diversity, and geographic location, profoundly shape access to care and developmental outcomes, few current studies meaningfully addressed these variables. This omission is particularly concerning given the disproportionate burden of communication difficulties and mental health challenges experienced by children from minoritised communities.
Socioeconomic status (SES) also intersects with both communication and mental health needs. Children from low-SES families are more likely to experience both language delay and elevated emotional distress, yet face higher thresholds to access services. Systemic constraints (including out-of-pocket costs, reduced service availability in rural areas, and limited school-based supports) significantly reduce opportunities for early intervention (Hodgkinson et al., 2017). These inequities not only widen developmental gaps but also entrench disadvantages across educational and health domains.
The lack of equity-oriented research designs in the corpus of research also limits the generalisability and translational value of the findings. A number of studies are still t conducted with predominantly white, English-speaking, urban samples, often with limited contextual information about family background, linguistic diversity, or community resources. Without intentional inclusion of diverse populations, both the evidence base and the interventions derived from it risk reinforcing existing disparities.
Addressing these gaps, in the context of linguistic diversity and community resource support, requires an explicit shift toward equity-informed inquiry and practice. This includes recruiting diverse participant samples (Iflaifel, et al., 2023), developing culturally and linguistically responsive assessment tools (Enriquez, 2023), and embedding equity considerations in service design and delivery (Bouckley, et al., 2025). It also requires a policy-level commitment to resourcing services in underserved communities and supporting the cultural competence of the workforce. Without these steps, children from minoritised backgrounds will continue to be underrepresented in research and underserved in practice, despite bearing a disproportionate share of the burden.
4.5. Translating Findings into Research, Practice, and Policy
The findings of this review point to a pressing need for more cohesive, responsive, and inclusive approaches across research, clinical practice, and policy settings. While the association between communication disorders and mental health difficulties is increasingly recognised, current responses remain fragmented and inadequate to address the complexity of children’s lived experiences.
From a research perspective, future studies must move beyond documenting co-occurrence and instead examine the mechanisms by which communication and mental health challenges influence one another across developmental stages. Longitudinal and mixed-method designs are especially needed to track trajectories over time and capture nuanced family and community influences. Importantly, there is a clear imperative for studies to prioritise the inclusion of children from underrepresented populations, particularly those from CALD, Indigenous, low-SES, and rural or remote communities, as the absence of such representation not only limits generalisability but also exacerbates inequities by failing to reflect the realities of those most in need of support.
In clinical practice, the findings of this review underscore the value of embedding emotional and behavioural monitoring within routine speech-language assessments. Practitioners should be supported to identify signs of distress, refer appropriately, and collaborate across disciplinary lines. This includes shared goal-setting with psychologists, joint case management, and co-delivered school-based interventions. Studies included in this review have shown the potential of such interdisciplinary models but also highlight the need for clearer pathways and more consistent training in interprofessional collaboration (e.g., Bloom et al., 2022; Taylor et al., 2022; Wertheimer et al, 2008). Strengthening reflective practice, trauma-informed care, and culturally responsive communication strategies will also be essential to enhancing service relevance and reach.
Additionally, at the policy level, there is an urgent need for investment in integrated care models that are developmentally and culturally informed. These must include coordinated funding across education, health, and community sectors, particularly for early intervention and school-based programs. In this sense, multi-agency planning structures and shared outcome frameworks can facilitate more efficient and family-centred service delivery (Kuo et al., 2012). Policy also plays a critical role in mandating equity-focused research funding, supporting the training of a diverse workforce, and embedding co-design principles that elevate the voices of children and families in shaping services.
Ultimately, this review reinforces the need to move beyond siloed, diagnosis-driven systems towards holistic, intersectional approaches that address the interwoven nature of communication, emotional well-being, family dynamics, and systemic structures. Children and young people will be best served when research, practice, and policy work in concert to acknowledge and respond to this complexity.
5. Strengths, Limitations, and Future Directions
This scoping review makes a timely and substantive contribution to understanding the intersection between communication disorders and mental health in childhood and adolescence. By synthesising thematic insights from a diverse set of studies and situating them within a broader field of emerging research, the review offers a multidimensional account of how communicative challenges and emotional well-being interact across developmental and social contexts.
A key strength of this review lies in its focus on the interwoven, rather than parallel, nature of communication and mental health difficulties. The identification of four cross-cutting themes, emotional-behavioural manifestations, social burden, familial stress, and systemic barriers provides a coherent framework that advances both theoretical understanding and clinical application. The review also applies an ecologically grounded lens, drawing attention to underexplored variables such as cultural identity, socioeconomic position, and interprofessional practice. This approach supports a more inclusive and contextually relevant account of children’s lived experiences.
Nonetheless, several limitations must be acknowledged. First, while the included studies offer rich insight, the small sample that a small number (n=10) of studies were found suitable for inclusion limits the scope of generalisation. Additionally, most studies focused on English-speaking contexts and lacked diversity in participant demographics, particularly with regard to CALD and Indigenous populations. Third, the quality and depth of mental health assessment across the included studies varied considerably, making direct comparisons challenging. Also, while this review aimed to balance breadth and depth, some relevant studies may have been unintentionally excluded due to strict search term limitations or language barriers.
Future research should prioritise longitudinal and mixed-method designs to examine causal pathways and resilience factors. Specifically, this research needs to address the disparity in developmental support for disadvantaged groups, who often lack access to language-rich environments and adequate social resources. Greater inclusion of culturally and linguistically diverse participants, as well as co-designed studies involving caregivers, practitioners, and young people, will be critical to advancing equity and impact. There is also a need to develop and evaluate integrated service models that bring together speech-language and mental health supports, particularly in early childhood and school settings. Such approaches hold promise not only for enhancing developmental outcomes but also for preventing the escalation of difficulties into adolescence and beyond.
6. Conclusion
This scoping review underscores the urgent need to reframe how communication disorders and mental health are understood and addressed in children and adolescents. These challenges rarely occur in isolation; rather, they are deeply intertwined, shaped by social relationships, family dynamics, and systemic service barriers. Thematic synthesis revealed that communication difficulties can both mask and magnify emotional distress, often going unrecognised in siloed systems of care. Families face compounding pressures, while many children remain underserved due to fragmented support, cultural mismatch, or inequitable access.
To move forward, research must centre diverse voices and examine developmental pathways through longitudinal and contextually grounded designs. Practice must shift toward integrated, family-centred models. Policies must fund and mandate interprofessional, culturally responsive services that reach beyond diagnostic categories. Addressing the co-occurrence of communication and mental health needs is not only clinically necessary but an equity imperative. Supporting these children early and holistically has the potential to shift trajectories, reduce long-term burden, and promote resilience across systems.
Author Contributions
Conceptualization, WH, LX. and YG; Methodology, WH, LX, YF, and SP; Formal Analysis, LX and YG; Investigation, WH, LX, YG, and SP; Writing – Original Draft Preparation, WH, LX, and YG; Writing – Review & Editing, WH, and SP.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
ADHD - Attention-deficit hyperactivity disorder
ASD - Autism Spectrum Disorder
ASHA - the American Speech-Language-Hearing Association
CALD - Culturally and linguistically diverse
CDs - communication disorders
DLD - developmental language disorder
SES - Socioeconomic status
References
- Arksey, H.; O'Malley, L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology 2005, 8(1), 19–32. [Google Scholar] [CrossRef]
- Bloom, R. D.; Tufano, V. E.; Perez, C. T. Registered nurses' and speech language pathologists' interprofessional collaboration: A systematic scoping review of the literature. Nursing Forum 2022, 57(6), 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Bouckley, T.; Peiris, D.; Nambiar, D.; et al. Addressing health equity during design and implementation of health system reform initiatives: A scoping review and framework. International Journal for Equity in Health 2025, 24, 68. [Google Scholar] [CrossRef] [PubMed]
- Caban, S.; Makos, S.; Thompson, C. M. The role of interpersonal communication in mental health literacy interventions for young people: A theoretical review, Health Communication, 2023. [CrossRef]
- Carey, B.; Erickson, S.; Block, S. A preliminary investigation of the mental health of parents of young children who stutter. Journal of Communication Disorders 2023, 103, 106329. [Google Scholar] [CrossRef]
- Channell, M. M.; Bosley, R. Mental state language use in children with Down Syndrome and the role of caregivers. Seminars in Speech and Language 2021, 42(4), 318–329. [Google Scholar] [CrossRef] [PubMed]
- Charman, T.; Ricketts, J.; Dockrell, J. E.; Lindsay, G.; Palikara, O. Emotional and behavioural problems in children with language impairments and children with autism spectrum disorders. International Journal of Language & Communication Disorders 2015, 50(1), 84–93. [Google Scholar] [CrossRef]
- Clarke, K. A. An investigation of the relationship between augmentative/alternative communication use by pediatric psychiatric inpatients with autism spectrum disorder and problem behaviors. Doctoral dissertation, The Pennsylvania State University, 2021. [Google Scholar]
- Cocquyt, M.; Claeys, T.; Derese, A.; Six, S.; Bilsen, J. Evaluating structure and content of parent-implemented early logopaedic intervention models following the three stages of communicative development in children with cleft lip and/or palate: Systematic literature review with narrative synthesis. International Journal of Language & Communication Disorders 2024, 59(5), 1923–1945. [Google Scholar]
- Cola, M.; Zampella, C. J.; Yankowitz, L. D.; Plate, S.; Petrulla, V.; Tena, K.; Parish-Morris, J. Conversational adaptation in children and teens with autism: Differences in talkativeness across contexts. Autism Research 2022, 15(6), 1090–1108. [Google Scholar] [CrossRef]
- Cutting, A. Choice and imitation skills: When teaching toddlers with autism imitation skills, does choice positively impact language development and skill generalization? Doctoral dissertation, Cambridge College, 2023. [Google Scholar]
- Doody, O.; Butler, M. P.; Lyons, R.; Newman, D. Families’ experiences of involvement in care planning in mental health services: an integrative literature review. Journal of Psychiatric and Mental Health Nursing 2017, 24(6), 412–430. [Google Scholar] [CrossRef]
- Dillon, E.; Holingue, C.; Herman, D.; Landa, R. J. Psychometrics of the pragmatic rating scale for school-age children with a range of linguistic and social communication skills. Journal of Speech, Language, and Hearing Research 2021, 64(9), 3477–3488. [Google Scholar] [CrossRef]
- Enriquez, J.; Arechiga, N.; Atherkode, S.; Otero, M.; Andrews, A.; Mason, L. Culturally responsive language assessment through a verbal operant experimental analysis. Behavior Analysis 2023, 23(2), 165–178. [Google Scholar] [CrossRef]
- Feehan, A.; Charest, M. A scoping review of oral language and social communication abilities in children with Tourette syndrome. International Journal of Language & Communication Disorders 2024, 59(1), 143–164. [Google Scholar] [CrossRef]
- Fitzsimons, D.; Clark, A. Pausing mid-sentence: An ecological model approach to language disorder and lived experience of young male offenders. International Journal of Environmental Research and Public Health 2021, 18(3), 1225. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, R. Exploring professional knowledge related to the development of communication, for children and young people with profound and multiple learning disabilities in an educational context. Doctoral dissertation, University of Exeter., 2023. [Google Scholar]
- Gibbard, D.; Roulstone, S.; Kandala, N. I.; Morgan, L.; Harding, S.; Smith, C.; Markham, C. A randomised controlled trial of the effectiveness of parent-based models of language intervention for 2-to 3-year-old children with speech, language and communication needs (SLCN) in areas of social disadvantage. International Journal of Language & Communication Disorders 2024, 59(4), 1517–1537. [Google Scholar]
- Hahn, L. J.; Brady, N. C.; Fleming, K. K.; Warren, S. F. Joint engagement and early language in young children with fragile X syndrome. Journal of Speech, Language, and Hearing Research 2016, 59(5), 1087–1098. [Google Scholar] [CrossRef] [PubMed]
- Hodgkinson, S.; Godoy, L.; Beers, L. S.; Lewin, A. Improving mental health access for low-income children and families in the primary care setting. Pediatrics 2017, 139(1), e20151175. [Google Scholar] [CrossRef]
- Houghton, K.; Schuchard, J.; Lewis, C.; Thompson, C. K. Promoting child-initiated social-communication in children with autism: Son-Rise Program intervention effects. Journal of Communication Disorders 2013, 46(5–6), 495–506. [Google Scholar] [CrossRef]
- Iflaifel, M.; Hall, C. L.; Green, H. R.; Willis, A.; Rennick-Egglestone, S.; Juszczak, E.; Townsend, M.; Martin, J.; Sprange, K. Widening participation-recruitment methods in mental health randomised controlled trials: A qualitative study. BMC Medical Research Methodology 2023, 23(1), 211. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.; Carr, E.; Feeley, K. Multiple effects of joint attention intervention for children with autism. Behavior Modification 2006, 30(6), 782–834. [Google Scholar] [CrossRef]
- Khatri, R. B.; Assefa, Y. Access to health services among culturally and linguistically diverse populations in the Australian universal health care system: Issues and challenges. BMC Public Health 2022, 22, 880. [Google Scholar] [CrossRef]
- Kuo, D. Z.; Houtrow, A. J.; Arango, P.; Kuhlthau, K. A.; Simmons, J. M.; Neff, J. M. Family-centered care: Current applications and future directions in pediatric health care. Maternal and Child Health Journal 2012, 16(2), 297–305. [Google Scholar] [CrossRef] [PubMed]
- Langbecker, D.; Snoswell, C. L.; Smith, A. C.; Verboom, J.; Caffery, L. J. Long-term effects of childhood speech and language disorders: A scoping review. South African Journal of Childhood Education 2020, 10(1), 1–13. [Google Scholar] [CrossRef]
- Lecavalier, L.; Leone, S.; Wiltz, J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research 2006, 50(3), 172–183. [Google Scholar] [CrossRef]
- Leitão, S.; St Clair, M. C.; Botting, N.; Gibson, J.; Jackson, E. "They don't realise how hard he has to try every day": The rewards and challenges of parenting a child with developmental language disorder. International Journal of Language & Communication Disorders 2025, 60(2). [Google Scholar]
- Levac, D.; Colquhoun, H.; O'Brien, K. K. Scoping studies: Advancing the methodology. Implementation Science 2010, 5(1), 69. [Google Scholar] [CrossRef] [PubMed]
- Lidstone, J. S.; Fernyhough, C.; Meins, E.; Whitehouse, A. J. Brief report: Inner speech impairment in children with autism is associated with greater nonverbal than verbal skills. Journal of Autism and Developmental Disorders 2009, 39(8), 1222–1225. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, A.; Broadbent, A.; Brooks, E.; Bulsara, K.; Donoghue, K.; Saijaf, R.; Sampson, K. N.; Thomson, A.; Fearon, P.; Lawrence, P. J. The impact of family interventions on communication in the context of anxiety and depression in those aged 14-24 years: Systematic review of randomised control trials. BJPsych Open 2023, 9(5), e161. [Google Scholar] [CrossRef]
- Luyster, R. J.; Kadlec, M. B.; Carter, A.; Tager-Flusberg, H. Language assessment and development in toddlers with autism spectrum disorders. Journal of Autism and Developmental Disorders 2008, 38(8), 1426–1438. [Google Scholar] [CrossRef]
- MacEvilly, D.; Maguire, K.; Brosnan, G.; Gaffney, L. Enhancing children's emotional regulation and social communication through group intervention–evidence of impact in an Irish outpatient Child and Adolescent Mental Health Service. Child Language Teaching and Therapy 2024, 40(1), 56–76. [Google Scholar] [CrossRef]
- Maljaars, J.; Noens, I.; Scholte, E.; van Berckelaer-Onnes, I. Language in low-functioning children with autistic disorder: Differences between receptive and expressive skills and concurrent predictors of language. Journal of Autism and Developmental Disorders 2012, 42(6), 2181–2191. [Google Scholar] [CrossRef]
- McKean, C.; Reilly, S. Creating the conditions for robust early language development for all: Part two: Evidence informed public health framework for child language in the early years. International Journal of Language & Communication Disorders 2023, 58(6), 2242–2264. [Google Scholar]
- Myrberg, K.; Hydén, L. C.; Samuelsson, C. The mini-mental state examination (MMSE) from a language perspective: An analysis of test interaction. Clinical Linguistics & Phonetics 2020, 34(7), 652–670. [Google Scholar]
- Munn, Z.; Peters, M. D.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC medical research methodology 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pereira, T.; Ramalho, A. M.; Valente, A. R. S.; Couto, P. S.; Lousada, M. The effects of the pragmatic intervention programme in children with autism spectrum disorder and developmental language disorder. Brain Sciences 2022, 12(12), 1640. [Google Scholar] [CrossRef]
- Pryor, S. M.; King, B. L.; Anderson, J. R. Gun-violence risk in youth: Prevention, response efforts, and considerations for school psychologists. Communique 2022, 51(4), 1–23. [Google Scholar]
- Peters, M. D.; Marnie, C.; Tricco, A. C.; Pollock, D.; Munn, Z.; Alexander, L.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI evidence synthesis 2020, 18(10), 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M. M.; Usman, O. L.; Muniyandi, R. C.; Sahran, S.; Mohamed, S.; Razak, R. A. A review of machine learning methods of feature selection and classification for autism spectrum disorder. Brain Sciences 2020, 10(12), 949. [Google Scholar] [CrossRef] [PubMed]
- Ravi, S.; et al. Are early social communication skills a harbinger for language development in infants later diagnosed autistic?–A longitudinal study using a standardized social communication assessment. Frontiers in Communication 2022, 7, 977724. [Google Scholar] [CrossRef]
- Reetzke, R.; Singh, V.; Hong, J. S.; Holingue, C. B.; Kalb, L. G.; Ludwig, N. N.; Landa, R. J. Profiles and correlates of language and social communication differences among young autistic children. Frontiers in Psychology 2022, 13, 936392. [Google Scholar] [CrossRef]
- Taylor, S. M.; Culic, A.; Harris, S.; Senini, R.; Stephenson, R.; Glass, B. D. Bridging allied health professional roles to improve patient outcomes in rural and remote Australia: A descriptive qualitative study. Journal of Multidisciplinary Healthcare 2022, 15, 541–551. [Google Scholar] [CrossRef]
- Toseeb, U.; Gibson, J. L.; Newbury, D. F.; Orlik, W.; Durkin, K.; Pickles, A.; Conti-Ramsden, G. Play and prosociality are associated with fewer externalizing problems in children with developmental language disorder: The role of early language and communication environment. International Journal of Language & Communication Disorders 2020, 55(4), 583–602. [Google Scholar]
- Tricco, A. C.; Lillie, E.; Zarin, W.; O'Brien, K. K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M. D. J.; Horsley, T.; Weeks, L.; Hempel, S.; Akl, E. A.; Chang, C.; McGowan, J.; Stewart, L.; Hartling, L.; Aldcroft, A.; Wilson, M. G.; Garritty, C.; Lewin, S.; Straus, S. E. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine 2018, 169(7), 467–473. [Google Scholar] [CrossRef] [PubMed]
- Wertheimer, J. C.; Roebuck-Spencer, T. M.; Constantinidou, F.; Turkstra, L.; Pavol, M.; Paul, D. Collaboration between neuropsychologists and speech-language pathologists in rehabilitation settings. The Journal of Head Trauma Rehabilitation 2008, 23(5), 273–285. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Moser, T. The art of coding and thematic exploration in qualitative research. International Management Review 2019, 15(1), 45–55. [Google Scholar]
- Xiao, N.; Shinwari, K.; Kiselev, S.; Huang, X.; Li, B.; Qi, J. Effects of equine-assisted activities and therapies for individuals with autism spectrum disorder: Systematic review and meta-analysis. International Journal of Environmental Research and Public Health 2023, 20(3), 2630. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).