Introduction
Congenital ostium defect secundum has a prevalence of 4 to 8 per 1000 live newborns in Ecuador and constitutes an important cause of infant mortality, with complications that have a negative effect on the patient's quality of life and prognosis [
1]. The defect is the result of poor development of the atrial septum as well as increased cell death of the septum primum in the dorsal roof of the atrium, or the septum secundum does not close the ostium secundum after birth causing a shunting of blood supply from the left to the right atrium [
2] Identification of the ostium secundum can be difficult in primary care since its clinical presentation may be null at early ages, although some exercise intolerance may be present, usually the clinical manifestations are already present in adulthood with symptoms such as dyspnea on exertion, palpitations, there may also be a characteristic murmur of soft systolic ejection over the pulmonary area combined with a wide and fixed division of sound 2 or signs of right heart failure, it may also produce a rise in pulmonary vascular resistance that ends in the development of pulmonary arterial hypertension, which may be present in up to 16% of patients with atrial septal defect [
3,
4]. The treatment for this type of congenital conditions is surgical, with percutaneous techniques or median sternotomy; however, minimally invasive surgery may be an option to substitute sternotomy for the correction of this type of cardiac anomalies [
5]. There is recent scientific evidence that the use of this surgical technique gives better esthetic results and less psychological impact for the patient [
6,
7,
8,
9,
10]. Different studies recommend using this technique in children as the first choice, being able to correct different congenital cardiac conditions such as ostium secundum, primum and coronary sinus without roof, presenting several benefits for patients, compared to median sternotomy, which has a larger incision and is much more traumatic [
11,
12,
13]. The use of the minimally invasive technique is scarce, in spite of reducing pain, use of blood products, hospitalization days (1 to 5 days), monetary costs and that it can be used safely with knowledge of the potential dangers such as pneumothorax and subcutaneous emphysema which have the same incidence as other surgical procedures; it should also be considered that the heavier the patient, the longer the surgical time, but it does not affect the extracorporeal circulation times [
14]. In a study of 538 patients followed up for 20 years, it was shown that they are currently in good condition without limitation for physical activity, only 5.8% suffered postoperative complications, showing that the minimally invasive approach is safe and effective in both children and adults with a very high rate of satisfaction with the esthetic result [
15]. The use of the minimally invasive technique demonstrates ample advantages that should be considered, such as shorter recovery time, better pain management by reducing the size of the incision, giving positive clinical and economic results by reducing hospitalization time and psychological results by reducing the size of the scar [
14]. The importance of this research is to demonstrate a better management of congenital heart conditions in a minimally injurious way, making this project useful to the research priorities of the Ministry of Public Health (MSP) in its last update 2013-2017, area 13 Congenital, genetic and chromosomal in the cardiac anomalies section, laying the foundations of national research for the use of this technique and benefiting the large number of births with this condition [
16].
Management of Atrial Septal Defect (Ostium Secundum)
- -
Patients with an atrial septal defect with an opening of less than 5 mm usually experience spontaneous closure of the defect during the first year of life [
17,
18].
- -
In adult patients with small atrial septal defect without signs of right heart failure it is recommended to observe the evolution of the patient with echocardiography every 2 to 3 years, evaluating the function and structure of the right heart, since it tends to increase in size if the defect worsens ,[
17,
18].
- -
If the patient presents an communication interatrial with an opening greater than 1cm, medical and surgical intervention (percutaneous closure, mini thoracotomy, sternotomy) is usually required to close the congenital defect [
17,
18].
- -
Patients requiring medical management prior to surgery are usually patients with arrhythmias whose cardiac rhythm and anticoagulation are controlled or patients with pulmonary hypertension with prostacyclin drugs, phosphodiesterase 5 inhibitors, endothelin receptor antagonists [
17,
18].
Comparison of Techniques
Table 1.
Comparative table of percutaneous procedure and surgical procedure for closure of atrial septal defect type ostium secundum by author [
2,
14,
17,
19,
20].
Table 1.
Comparative table of percutaneous procedure and surgical procedure for closure of atrial septal defect type ostium secundum by author [
2,
14,
17,
19,
20].
| |
COMPARATIVE TABLE OF SURGICAL TECHNIQUES |
| PERCUTANEOUS |
SURGICAL (patientmini-thoracotomy ) |
| INDICATIONS |
1. atrial septal defect Hemodynamically significant with secundum Qp/Qs ≥ 1.5:1.
2. Stroke or recurrent transient ischemic attack caused by a transient shunt of the communicationright-to-left .interatrial
3. Symptoms related to cyanosis caused by a transient right-to-left shunt of the ASD.
4. Defect with opening smaller than 38mm and presence of edges that support the septal occluders. |
1. Septal defects of venous sinus, type.theprimum, unroofed coronary sinus and secundum
2. Septal defect with an opening greater than 38mm.
3. Inadequate margins for anchoring a device
4. Small babies
5. If the device interferes with atrioventricular valve function.
6. Systemic or pulmonary venous drainage |
| CONTRAINDICATIONS |
1. type defect Small that does not involve hemodynamic complications.secundum
2. Atrial septal defects typeprimum , venous sinus type and unroofed coronary sinus defects.
3. type septal defect secundum with advanced pulmonary hypertension. |
1. Pulmonary (relative).hypertension
2. A pulmonary vascular resistance greater than 8 Woods units.
3. Presence of Eisenmenger's syndrome.
|
| INCISION |
Less than 5mm at the siteincision |
From 3 to 9 cm (7cm in the patient). |
| RECOVERY DAYS |
4-5 days.
|
4-5 days. |
| COMPLICATIONS |
1. Embolization of the device.
2. Cardiac erosions.
3. New onset atrial arrhythmia.
4. Atrioventricular block (atrioventricular block).
5. Thromboembolism |
6. Postoperative arrhythmias
7. Pneumothorax.
8. Subcutaneous emphysema |
Case Report
Female patient, 28 years old, married, ARH+ blood, refers that in the year 2020 goes to a gynecologist for family planning where in her medical history she refers dizziness and syncope in adolescence so she requests an electrocardiogram (EKG) and is sent to a private for cardiologist transthoracic echocardiogram showing right cavity growth, After the results, the patient was sent to the hospital third level José Carrasco Arteaga, and a transesophageal echocardiogram was requested, which showed evidence of defect interatrial (ASD) type ostium secundum wide of 47 millimeters without borders for percutaneous closure, plus severe pulmonary hypertension 55 mmHg, so the patient was referred to the cardiac surgery service where after evaluation and complementary tests it was decided to admit the patient for surgical resolution.
Current
mid-effort dyspnea
Admission
The patient was admitted to the operating room on July 21, 2022 for scheduled surgery for correction of congenital heart disease type Ostium secundum, the physical examination on admission the patient had blood pressure 100/60 mmHg, heart rate 71 beats per minute, respiratory rate 18 breaths per minute, temperature 36.5 degrees, oxygen saturation 93%, FIO2 21%, weight 53 kg, height: 1.55 meters; Heart: R1 and R2 synchronous with the pulse, auscultation of murmur mesosystolic in pulmonary focus of grade II - III in intensity.
Surgery
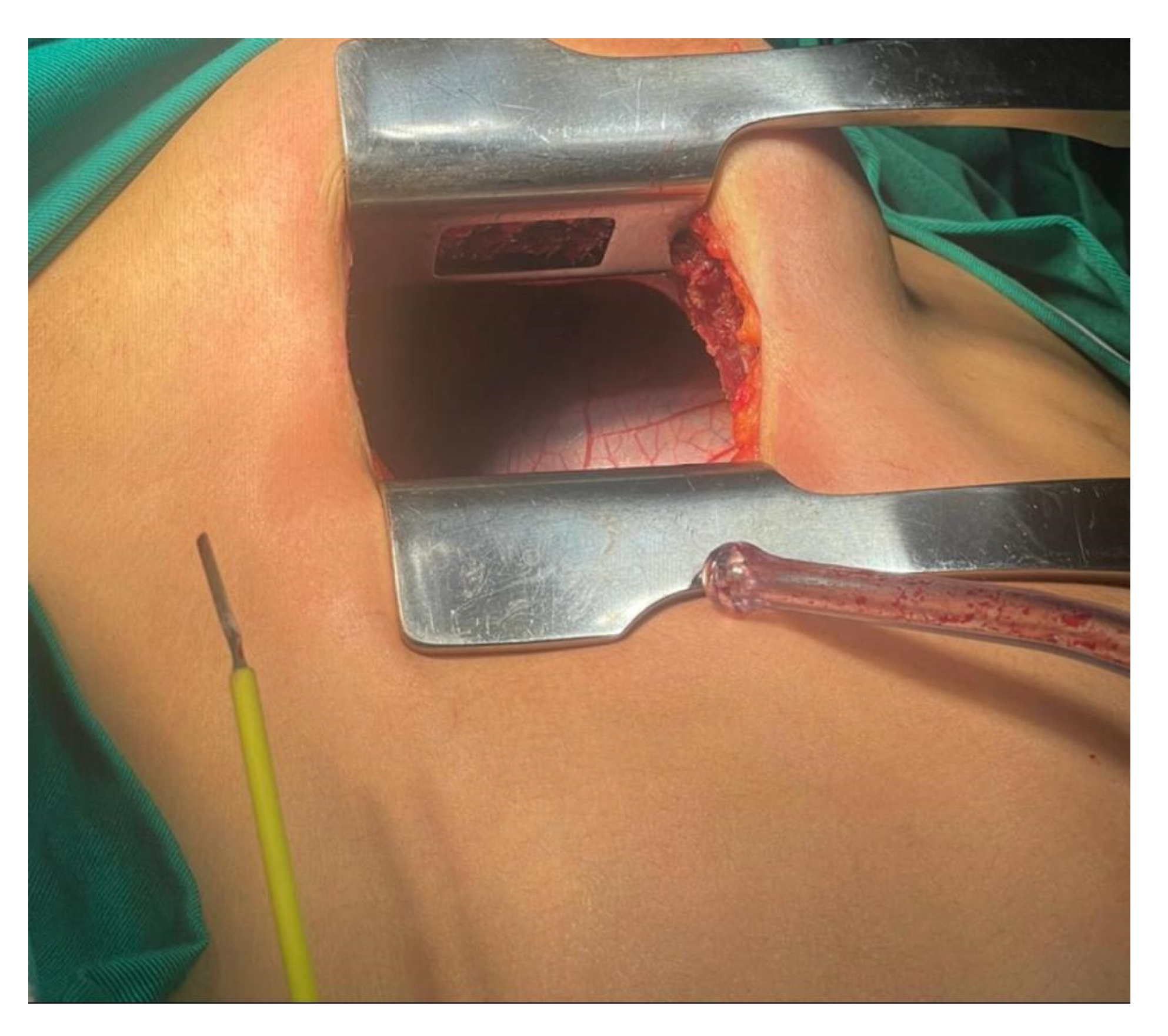
Under asepsis and antisepsis standards with anesthesiology and nursing protocol is performed by right thoracotomy. A polyester suture (is placed at the level of the ascending aorta 2-0 ) for arterial cannulation, a non-absorbable propylene (suture is placed in the right atrium Ethibond4-0 ) and superior vena cava for venous cannulation. Heparin is administered and with optimal activated clotting time (ACT) the aorta and venae cavae are cannulated with cannulationprolenebicave , a 4-0 non-absorbable propylene suture is placed for cardioplegia, with optimal clotting time and patient stability, ECC (extracorporeal circulation) is started, Aorta is clamped and solution is administered cardioplegia by cannulation of the aorta and temperature is lowered to 36 degrees, a 4-0 non-absorbable propylene suture is placed in the right superior pulmonary vein and suction ventilation of the left cavities is placed to assist emptying of the left atrium. right atrium is sectioned Atriotomy through the submammary incision (
Image 1).
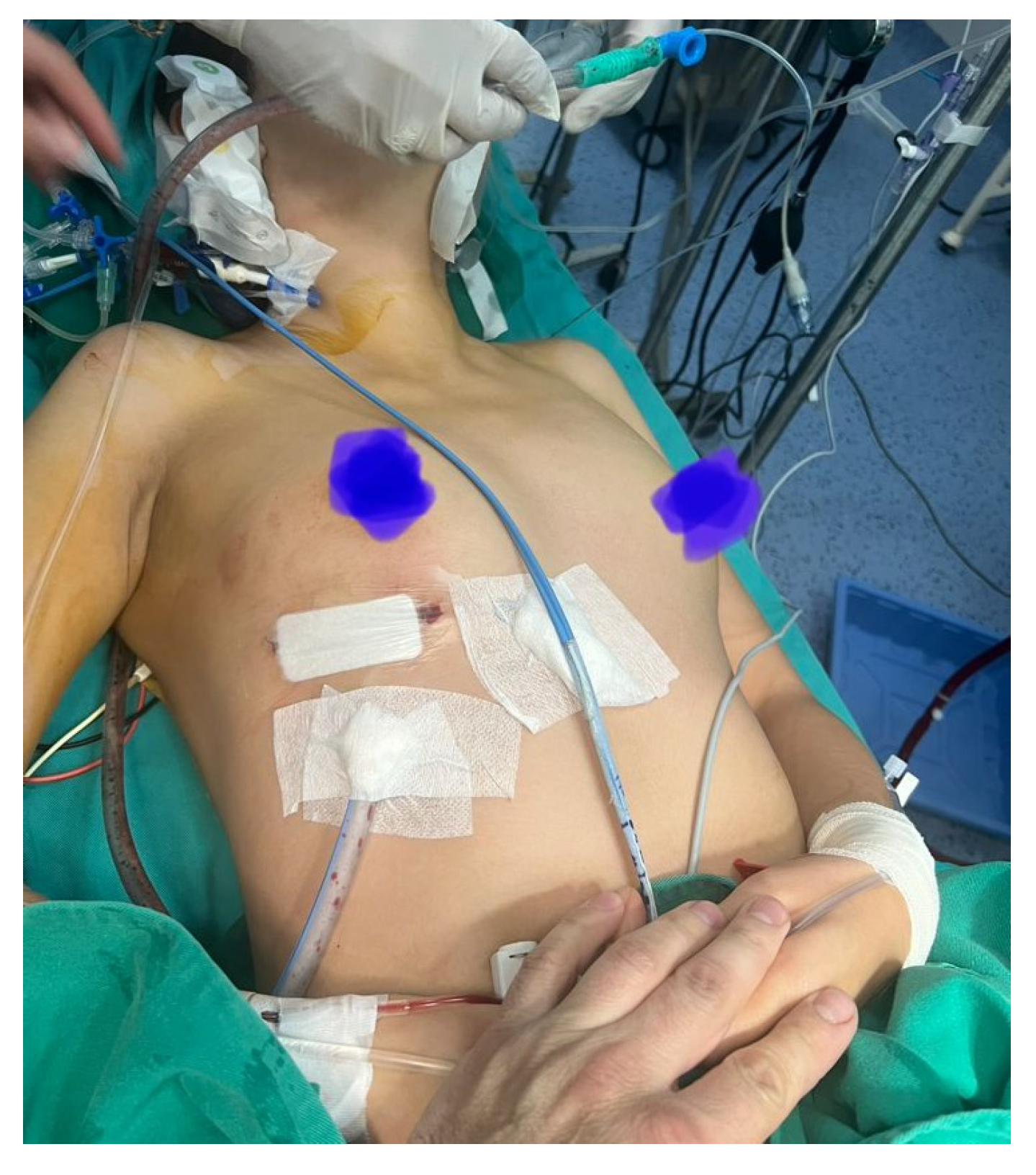
Non-absorbable 4-0 propylene suture exposure stitches are placed. A wide atrial septal defect is identified, normal venous connection. Closure with bovine patch, then left ventricular de-airing maneuvers, closure of the right atrium with non-absorbable 4-0 propylene suture. An pacemaker lead is placed epicardial in the right ventricle free wall, pacemaker operation is checked, the aorta is unclamped and sinus rhythm is restored. Aortic root is aspirated, in hemodynamic stability, root aspiration, caval veins and aortic root , protamine is administered for reversal of heparin, 1 28FR tube is placed at right thoracic level, fixed with 2-0 polyester suture and a suture with absorbable polyglactin suture. Closure of the pericardium with 2-0 polyglactin absorbable suture. With intradermal suture, the patient was transferred to the intensive care unit in stability, extubated, monitored with rhythm on the monitor that showed sinus rhythm without vasoactive support and permeable drainage (
Image 2).are decannulated
The surgical procedure required a duration of extracorporeal circulation of 60 minutes, aortic clamping time of 40 minutes, and there was a bleeding of 200cc, she had no complications and was extubated from the operating room (
Image 2).
Twenty-four hours after surgery, prophylaxis with cefazolin, anticoagulation with enoxaparin and analgesia with fentanyl, the patient remains in intensive care hemodynamically stable and without vasoactive support, with vital signs: Blood pressure: 111/54; Heart rate: 87; Respiratory rate: 18 rpm; Temperature: 36.8; Oxygen saturation: 94%.
Prescription in the Intensive Care Unit (ICU) included soft diet, continuous monitoring, capillary glycemia every 8 hours, oxygen by mask to saturate greater than 90%, maintenance fluids with electrolytes (potassium) and analgesia with fentanyl.
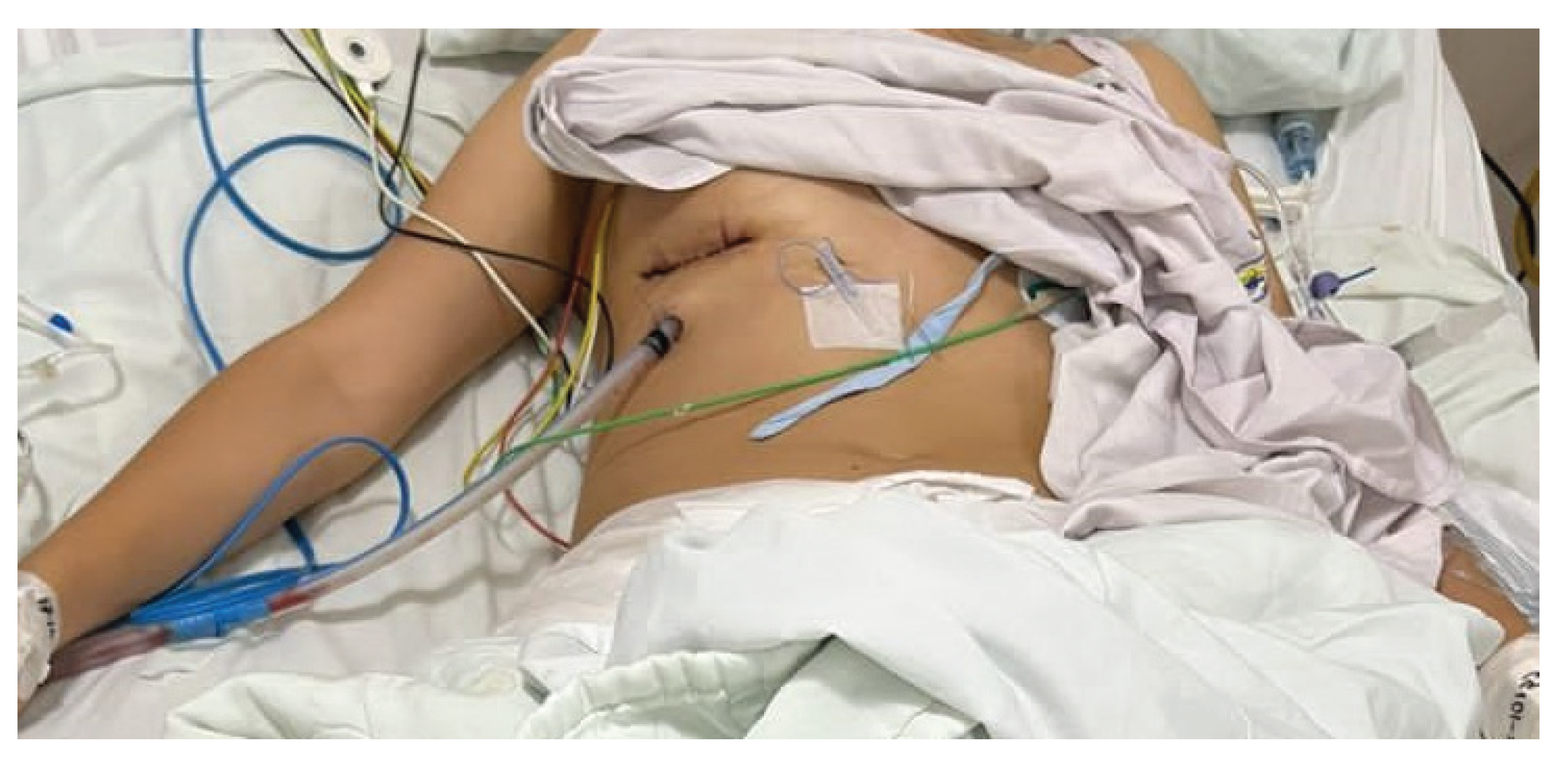
At 48 hours post-surgery analgesic therapy with fentanyl is replaced by suspending it and administering paracetamol instead (
Image 3).
After 72 hours of the postoperative period after a favorable evolution without complications or signs of wound infection or systemic infection, antibiotic therapy is terminated, and the patient is transferred to the surgical floor where she remains until her fifth day of hospital stay when the patient is hemodynamically stable without vasoactive support, with good ventilatory mechanics, without supplemental oxygen support, paraclinical within normal parameters, with good evolution, adequate pain management, wound in adequate healing process and is finally discharged from the hospital. In summary, the patient had 5 days of hospital stay of which 3 days were spent in the intensive care unit (ICU) and then 2 days until her medical discharge to the surgical floor.
Discussion
Regarding the surgical technique of choice for the correction of congenital malformations, the minimally technique has recently gained popularityinvasive, which can be performed through some types of incisions such as a vertical infra axillary one on the right side, a left anterolateral one and a right anterolateral one, This type of technique is the one that seeks to perform the least possible traumatic impact on the patient, however, there is much controversy in his choice for the correction of congenital cardiac malformations. Starting with the literature postulated by Steele et.al [
21], in which the patients in which they underwent surgery and follow up was between 1953 and 1978 and indicates that they presented poor results in a long term follow up as the progression of symptoms or death, however, this study was performed when the control and treatment of pulmonary hypertension was not routinely performed as nowadays, compared to nowadays. In contrast to what Steele postulateset.al [
21] , there is updated bibliography which promotes a surgical approach in patients with pulmonary hypertension, as stated by Tokaya et.al [
22], a study in which the preoperative treatment of pulmonary tension to reduce the value to moderate or mild figures facilitates surgical intervention in patients with ostium secundum, thus supporting the management that was performed in the patient presented in this case.
Regarding the choice of the method of correction of atrial septal defect, there are several updated bibliography that support the use of minimally invasive techniques as in the case of the patient presented, over conventional techniques such as sternotomy, there are current studies which motivate the use of the minimally invasive technique as the surgical method of choice, an example of this is a retrospective study published in 2022 by Amirghofran et.al [
10], which included 48 cases of patients treated with minimally invasive technique and 35 cases treated with conventional sternotomy which were followed for an average of 18 years and 6 months by transthoracic echocardiography and electrocardiography before, during and after the procedure, having pediatric and adult patients; Within these two groups of patients those who underwent minimally invasive surgery showed a reduction in thoracic drainage and blood transfusion volume, and of the 48 cases with minimally invasive technique only one presented mild stenosis of the superior vena cava but without the need for reintervention, thus demonstrating that the minimally invasive approach is a safe and practical approach ensuring a quality correction comparable to sternotomy with the advantage of not having too large a scar.
There is also a study by Luo Z Rong et.al [
9], published in 2020, included 136 patients who were divided into three groups according to the minimally invasive technique used with vertical infra axillary and incision inframammary and conventional sternotomy, and in all of them satisfactory results were obtained, this study claims not to find statistically significant differences in the operative time, duration of cardiopulmonary bypass, mechanical ventilation time, amount of blood transfusion, time spent in intensive care, hospital stay and therefore hospital costs, unlike conventional sternotomy which left a large and noticeable wound in the patient, denoting a better cosmetic result with minimally invasive techniques.
These results are not exclusive to these studies since Zhu et.al [
13](14, refers in their study that 472 patients were all operated with minimally invasive techniques of which only 19 patients presented complications such as thoracic exploration due to hemorrhage, reintervention due to dehiscence, transient neural dysfunction, atelectasis, and study they performed a minimally invasive sternotomy in 472 patientsdiaphragm but there was no mortality of the patients, just as ), who reported in their study, that in their paresis Bayya et.al .al [
14], who in their research also adds complications such as emphysema and paresis as the most common, pointing out that there is also an increase in surgical time with greater patient weight, whether adult or pediatric, but without altering extracorporeal circulation times.
Another study by Atalay et.al [
8], ,published in 2022 included all patients who underwent minimally invasive surgery through a right infra axillary incision between 2019 and 2021 and describes that the minimally invasive technique is a safe alternative for the correction of congenital heart defects even in pediatric patients. Also a study by Said et.al [
11], which was published in 2023, affirms that the use of minimally invasive techniques in pediatric patients has no late mortality or reinterventions and Yang et.al [
12] confirms these statements by showing in his study that this type of surgical approach has a high percentage of acceptance among patients and relatives of the patient for the cosmetic result.
However, in contrast to the other studies Vida et.al [
15], in their study shows some complications in female patients with prepubertal age such as a slight transitory deficit of sensitive skin in the mammary area and an asymmetric breast development, however this type of complications is also explained by the study that a great part is due to the professional component of the surgeon and his expertise, taking into account that the larger the incision, even if a minimally invasive approach is performed, the more defects will be obtained in the results in the development of female patients, although as far as the cosmetic results of the scar are concerned, there will be a high percentage of acceptance.
Conclusions
In conclusion, minimally invasive surgical approaches should be performed more frequently as a therapeutic option to replace sternotomy or as an alternative to the option percutaneous in young patients and adults taking into account the aesthetic advantages for the patient, also the decrease in economic costs for the patient by reducing hospitalization or care days in a patient without complications; taking into account that its use does not increase the risks of complications or death in patients who practice it. The disadvantages of the use of this technique would be the skill of the professional surgeon to reduce the possibilities of complications or surgical risks which may affect younger patients in their mammary development in female patients.
Conflict of Interest
There is no conflict of interest among the researchers.
References
- Cardiopathies archives - Sociedad Ecuatoriana de Cardiología [Internet]. [cited May 21, 2023]. Available from: https://www.scardioec.org/category/cardiopatias/.
- Menillo A, Lee L, Pearson-Shaver A. Atrial Septal Defect. 2023. Atrial Septal Defect.
- Courtney M. Townsend, R. Daniel Beauchamp, B. Mark Evers, Kenneth L. Mattox. Sabiston. A treatise on surgery. In: Elsevier, publisher. Sabiston Treatise on Surgery. 21st ed. Elsevier; 2022. p. 1641-78.
- Bradley EA, Zaidi AN. Atrial Septal Defect. Cardiol Clin. Aug 2020;38(3):317-24.
- Connolly Heidi M, Taggart Nathan. Surgical and percutaneous closure of atrial septal defects in adults [Internet]. 2021 [cited 2023 Jul 9, 2023]. Available from: https://www-uptodate-com.vpn.ucacue.edu.ec/contents/surgical-and-percutaneous-closure-of-atrial-septal-defects-in-adults?search=ostium%20secundum&source=search_result&selectedTitle=2~75&usage_type=default&display_rank=2#.
- Mirmohammadsadeghi A, Firouzbakht B, Mirmohammadsadeghi M. Right anterior minithoracotomy vs. Conventional median sternotomy in surgical ostium secundum atrial septal defect closure: Assessment of clinical outcomes and health-related quality of life. Int Cardiovasc Res J [Internet]. September 2020 [cited April 19, 2023];14(3):102-7. Available from: https://www-scopus-com.vpn.ucacue.edu.ec/record/display.uri?eid=2-s2.0-85091822293&origin=resultslist&sort=plf-f&src=s&st1=ostium+secundum+thoracotomy&sid=2ff44f740826fae9346a42c36c2ed3ac&sot=b&sdt=b&sl=42&s=TITLE-ABS-KEY%28ostium+secundum+thoracotomy%29&relpos=4&citeCnt=0&searchTerm=#funding-details.
- Guariento A, Doulamis IP, Blitzer D, Cattapan C, Padalino MA, Vida VL. Minimally invasive congenital cardiac surgery: A large volume European experience. Congenit Heart Dis. 2020;15(3):127-39. [CrossRef]
- Atalay A, Yilmaz M, Turkcan BS, Ecevit AN, Ozler B, Azak E, et al. Can Right Infra-Axillary Vertical Thoracotomy Make a Big Difference in Surgical Technique Preference? Heart Lung Circ. Oct 2022;31(10):1419-24.
- Luo Z rong, Chen Q, Yu L li, Chen L wan, Huang Z yao. Comparative Study between Surgical Repair of Atrial Septal Defect via Median Sternotomy, Right Submammary Thoracotomy, and Right Vertical Infra-Axillary Thoracotomy. Braz J Cardiovasc Surg. 2020;35(3).
- Amirghofran AA, Nirooei E, Edraki M, Ramsheh AR, Ajami G, Amoozgar H, et al. Minimally invasive versus sternotomy approach for double-patch repair of partial anomalous pulmonary venous connection and sinus venosus defect in pediatric and adult patients: Mid to long-term outcomes. J Card Surg. December 2, 2022;37(12):4808-15. [CrossRef]
- Said SM, Greathouse KC, McCarthy CM, Brown N, Kumar S, Salem MI, et al. Safety and Efficacy of Right Axillary Thoracotomy for Repair of Congenital Heart Defects in Children. World J Pediatr Congenit Heart Surg. January 27, 2023;14(1):47-54. [CrossRef]
- Yang X, Hu Y, Dong J, Huang P, Luo J, Yang G, et al. Right vertical axillary incision for atrial septal defect: a propensity score matched study. J Cardiothorac Surg. on Oct 5, 2022;17(1):256. [CrossRef]
- Zhu J, Zhang Y, Bao C, Ding F, Mei J. Individualized strategy of minimally invasive cardiac surgery in congenital cardiac septal defects. J Cardiothorac Surg. on Dec 15, 2022;17(1):5. [CrossRef]
- Bayya PR, Kottayil BP, Srimurugan B, Balachandran R, Jayashankar JP, Baquero L, et al. Transaxillary Approach for Surgical Repair of Simple Congenital Cardiac Lesions: Pitfalls, and Complications. World J Pediatr Congenit Heart Surg. on May 4, 2021;12(3):337-43. [CrossRef]
- Vida VL, Zanotto L, Zanotto L, Tessari C, Padalino MA, Zanella F, et al. Minimally invasive surgery for atrial septal defects: a 20-year experience at a single centre. Interact Cardiovasc Thorac Surg. on June 1, 2019;28(6):961-7. [CrossRef]
- Health research priorities, 2013-2017. 2013.
- Brida M, Chessa M, Celermajer D, Li W, Geva T, Khairy P, et al. Atrial septal defect in adulthood: a new paradigm for congenital heart disease. Eur Heart J. July 21, 2022;43(28):2660-71. [CrossRef]
- Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. on April 2, 2019;139(14).
- Chambault AL, Olsen K, Brown LJ, Mellor SL, Sorathia N, Thomas AE, et al. Transcatheter versus surgical closure of atrial septal defects: a systematic review and meta-analysis of clinical outcomes. Cardiol Young. on January 25, 2022;32(1):1-9.
- Yang M, Wu J. Recent review of transcatheter closure of atrial septal defect. Kaohsiung J Med Sci. on July 30, 2018;34(7):363-9.
- Steele P, Fuster V, Cohen M, Ritter D, McGoon D. Surgical and percutaneous closure of atrial septal defects in adults [Internet]. 1987 [cited December 18, 2023]. Available from: https://pubmed.ncbi.nlm.nih.gov/3664992/.
- Takaya Y, Akagi T, Sakamoto I, Kanazawa H, Nakazawa G, Murakami T, et al. Efficacy of treat-and-repair strategy for atrial septal defect with pulmonary arterial hypertension. 2022 [cited 2023 Dec 19]; Available from: https://pubmed.ncbi.nlm.nih.gov/34415851/. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).