Introduction
Pediatric chronic pain is a biopsychosocial phenomenon that is increasingly being recognized as a family matter[
1]. With pediatric chronic pain affecting 20.8% of youth[
2], the impact on family systems and communities is significant. Paired with the impact on family systems, is the cultural and ethnic consideration regarding the experience of chronic pain. According to the Pew Research Center[
3], Asian Americans are the fastest growing racial group in the US. Therefore, it is important to understand the intersection of this vastly growing population and its representation – or lack thereof – in the pediatric chronic pain literature. We recognize the Asian/Asian American diaspora as highly diverse, encompassing many cultures. For this paper, we use the term “Asian” to broadly refer to individuals of Asian descent in the US, including those from various immigrant backgrounds.
Although the population of Asians in the US continues to grow, Asian families are consistently underrepresented in pain clinics and show low rates of help-seeking behaviors[
4]. This trend is inconsistent with research demonstrating that Asians report lower levels of pain tolerance and higher ratings of pain unpleasantness[
5] compared to their Non-Hispanic White (NHW) counterparts. Sensitivity to acute pain is a known risk factor for developing chronic pain[
6], suggesting a potential gap in our understanding of chronic pain experiences among Asian youth and the low representation in pain clinics. Literature addressing the intersection of Asian families in pediatric chronic pain contexts is sparse. Limited research has highlighted Asians experiencing higher baseline and stress heart rate levels along with higher parental expectations and greater parental criticism in comparison to their NHW counterparts[
5]. Consistently, Wang et al.[
7] found that Asian Americans experience greater internalizing symptoms, family conflict, and lower self-esteem compared to their NHW peers. These symptoms are noteworthy as internalizing symptoms have been found to increase the likelihood of chronic pain in pediatric populations[
8].
Parent protective behaviors, such as providing more pain-related attention to the child or allowing them to miss school, have been associated with greater functional disability[
9], increased somatic symptoms[
10], slower recovery from surgery[
11] and more. Further, parent protective behaviors have demonstrated negative associations with youth overall function, school, pain intensity, and depression[
12]
,[
13]. However, a major limitation of these studies is their limited generalizability, as most youth seeking pain treatment have been Caucasian or NHW[
14]. Parent protective behaviors are shaped by family socialization practices, which in Asian families, parents have been found to often limit praise, favor criticism[
7] and express warmth in more nonverbal and indirect ways[
7,
15]. The collectivistic cultural emphasis on stoicism and the suppression of personal expression[
16] may contribute to increased physiological stress[
17]. Given the unique dynamics within Asian families – characterized by both higher family conflict and stronger family cohesion – parent protective behaviors may have a distinct impact on the chronic pain experience of Asian youth. Possibly, explicit protective behaviors, which may provide validation and support, could help mitigate the emotional burden of chronic pain for Asian youth, counteracting the effects of stoicism and limited emotional expression. This study explores this psychosocial phenomenon by examining cultural influences on parenting. Since cultural beliefs shape parenting attitudes and behaviors[
16] we will specifically focus on parent protective behaviors in the context of youth with chronic pain.
Aims and Hypotheses
Our overarching aim is to explore how parent protective behaviors impact Asian youth in their experience of chronic pain. Specifically, the first aim is to compare reports of parent protective behaviors, youth global distress (anxiety and depression), and pain-related distress (pain intensity, pain catastrophizing, and pain interference) between Asian youth and their NHW counterparts. We hypothesized that Asians would report higher parent protective behaviors, greater global distress, and lower pain-related distress in comparison to NHW youth.
The second aim is to investigate how parent protective factors impact the relationship between youth global distress and pain-related distress in Asian versus NHW families. We hypothesized that the impact of protective factors would differ by ethnicity: in NHW families, parent protective behaviors are expected to moderate, and thus strengthen the relationship between youth global distress and pain-related distress, consistent with existing literature[
9], while in Asian families, we predict that greater parent protective behaviors will buffer the impact that global distress has on pain-related distress.
Materials and Methods
Participants
Data was retrospectively extracted from the Pediatric-Collaborative Health Outcomes Information Registry (Peds-CHOIR). The pediatric adaptation of the Collaborative Health Outcomes Information Registry (Peds-CHOIR) is a free, open-source, flexible learning health care system (LHS) that meets the call by the Institute of Medicine for the development of national registries to guide research and precision pain medicine.
Using a web-based interface, the registry has capabilities to capture data at each clinic visit; display graphical, real-time results that inform point-of-care decisions; and track patient treatment responses longitudinally[
18]
. The registry is a part of the clinical infrastructure and completed by all patients who are seen in the tertiary Pediatric Pain Management Clinic (PPMC) at Stanford Children’s Health, California, an interdisciplinary clinic. Data included in this study was cross-sectional completed before the initial evaluation at the PPMC. The data included in this analysis was extracted from June 2014 to August 2023 and included patients 8-17 years old. Furthermore, patients included in this study self-identified as Non-Hispanic White (NHW) or Non-Hispanic Asian.
Measures:
Demographic Questionnaire
The Demographics and Pain History Questionnaire includes patient demographic information including age, sex, gender identity, race, and ethnicity.
Average Pain Intensity
An 11-point numeric rating scale from 0 (no pain) to 10 (worst pain possible) is used to quantify pain intensity (REF).
PROMIS Pediatric Patient and Caregiver (Proxy) Outcome Measures
PROMIS Pain Interference, Anxiety, and Depression measures were used in this study. The PPMC uses the PROMIS computer adaptive testing (CAT) version and item response theory (IRT) to understand patient reports of mental, physical, and social functioning. CAT administers items from an item bank based on responses to earlier items which reduces the number of items administered to patients but has been shown to improve precision. The final score, however, has been shown to reflect the construct being evaluated. This measure was validated in a representative sample of US patients with chronic conditions and their families, as well as in the general population through schools and primary care clinics.
PROMIS scores are centered at a mean of 50 and a standard deviation of 10, using a T-score distribution. The pediatric PROMIS measures assess physical, social, and psychological functioning domains in children 8 to 17 years old. Responses are on a 1-5 scale (1= “Never/Not able to do” and 5= “Almost always/With no trouble”).
Pain Interference
The PROMIS pediatric pain assessment asks questions to understand the impact of pain on social, psychological, and physical functioning (e.g., “It was hard for me to have fun when I had pain”). Higher scores indicate increased pain interference.
Pediatric Anxiety
The PROMIS pediatric anxiety questionnaire assesses patient worries, fears, and nervousness (e.g., “In the past 7 days I felt worried”). Elevated scores indicate higher levels of anxiety.
Pediatric Depression
The PROMIS pediatric depression questionnaire assesses patients’ negative mood, social cognition, and self-perceptions (e.g., “In the past 7 days I felt alone”). Elevated scores indicate more depressive symptoms.
Parental Protective Behavior:
Adult Responses to Children’s Symptoms (ARCS) Questionnaire is an assessment that seeks to understand parent/guardian responses to children’s symptoms and behaviors. Higher scores indicate more protective behaviors and items are scored on a scale from 0 = “Never” to 4 = “Always”. Examples include, “When your child is in pain, how often do you... spend more time than usual with your child, stay home from work or come home early (or stay home instead of going out or running errands), and let your child sleep later than usual in the morning?” There are no clinical ranges for Parent Protective Behaviors; higher scores denote greater parent protective behaviors.
Pain Catastrophizing Scale (PCS-C)
Patient pain catastrophizing (PCS-C) was analyzed which seeks to understand child and adolescent feelings of helplessness and catastrophic thoughts. Examples of questions asked are “When I am in pain, it’s awful and I feel that it overwhelms me”, “When I am in pain, I want the pain to go away,” and “When I am in pain, I am afraid that the pain will get worse”. The PCS-C questionnaire is a 13-item measure rated with 0= “Not at all true” to 4 = “Extremely true”. Higher scores indicate heightened pain catastrophizing with clinical bands as follows: Low = 0-14, Moderate = 15-25, and High ≥ 26.
Global distress was separately measured by the Pediatric Anxiety and Pediatric Depression scales. Similarly, pain-related distress also comprised of three distinct measures: Average Pain Intensity, Pain Interference, and Pain Catastrophizing scales. These scales were not collapsed into one value (i.e., “global distress value” or “pain-related distress value”) and were analyzed separately.
Data Analyses
Data were analyzed using SPSS 29.0.2.0. Prior to conducting the primary analyses, frequency and pattern of missing values were assessed. Missing values were deleted from the analyses. To assess the pattern of missing data, Little’s MCAR (Missing Completely at Random) test was conducted across variables for each group, including pain intensity, pain interference, anxiety, depression, pain catastrophizing, and parent protective behaviors. The test yielded a significant chi-square value for the Asian population (χ²(16) = 26.54, p = .047) and for the White population (χ²(36) = 96.32, p < .001), indicating non-MCAR data. Of note, missing data for the Parent Protective Behaviors variable (13.9%) were not MCAR. When Parent Protective Behaviors was excluded for the White population only, the data met MCAR assumptions. To ensure robustness and, to ensure that the results were not an artifact of the method chosen for handling missing data, a sensitivity analysis was conducted, by comparing results from listwise deletion and mean imputation. Results revealed key findings to be consistent across both Listwise Deletion and Series Mean Imputation, indicating that the results were not highly sensitive to the missing data. Consequently, listwise deletion was used to maintain the full variability of the data. All variables were then mean-centered to reduce multicollinearity.
Aim #1: Compare reports of parent protective behaviors, youth global distress (anxiety and depression), and pain-related distress (pain intensity, pain catastrophizing, and pain interference) between Asian youth and their NHW counterparts.
To address the first aim, an Independent Samples T-test was conducted to compare Asian and Non-Hispanic White (NHW) youth in their reports of pain-related distress, global distress, and parent protective behaviors. Due to unequal sample sizes between Asian and NHW youth, Levene’s test for homogeneity of variances was conducted to assess whether assumption of equal variances is met for each variable across the two groups.
Aim #2: Investigate how parent protective factors impact the relationship between youth global distress and pain-related distress in Asian versus NHW families.
For the second aim, six hierarchical multiple regression analyses were conducted for each ethnic group to understand the extent to which parent protective behaviors interacted with the relationship between global distress (anxiety or depression) and pain-related distress (pain intensity, pain catastrophizing, or pain interference). Each model examined one combination of global distress (either anxiety or depression) and parent protective behaviors as independent variables, with a pain-related distress variable (i.e., pain intensity, pain interference, or pain catastrophizing) as the dependent variable. Parent protective behaviors were tested as the moderator (interaction with global distress) across all models. For each model, the following variables were entered for the stepwise linear regression analysis. In the first step, demographic variables associated with the independent and dependent variables – sex and patient age – were added as control variables. In the second step, the independent variables of anxiety or depression and parent protective behaviors were added. In the third step, the interaction term between parent protective behaviors and global distress was included to assess the moderating effect.
Finally, to data containing both ethnic groups, a post-hoc model with a 3-way interaction was conducted only for the significant moderation model. Thus, the 3-way interaction was fitted to investigate the relationship of ethnic group, parent protective behaviors and global distress on pain catastrophizing. This model also contained anxiety or depression, and parent protective behaviors, and their two-way interaction.
*P<0.05 was considered statistically significant throughout.
Results
There were 1179 NHW patients and 236 Asian patients included in the total sample.
Table 1 presents the bivariate correlations for all variables for Asian families and NHW families.
For Aim 1, Asian youth reported lower average pain intensity (
M=5.16,
SD=2.46) and pain interference (
M=57.63,
SD=8.16) compared to NHW youth as indicated in
Table 2. Cohen’s d effect sizes indicated large, statistically significant differences
(t(1177) = -2.97,
p<0.01; and
t(1177) =-3.46,
p<0.001, respectively). Asian parents reported significantly higher parent protective behaviors compared to NHW parents
(M=1.79,
SD=0.95), with moderate and significant effect sizes
(t(1177) = 4.53, p < 0.001). Levene’s test indicated that the assumption of homogeneity of variances was met for all dependent variables (p>0.05), except for parent protective behaviors (F = 11.499, p<0.001). Unequal variance assumption was violated for parent protective behaviors, and therefore Welch’s correction was applied. Using Welch’s
t-test to account for this, Asians exhibited significantly higher parent protective behaviors than Whites (t(300.595) = 4.492,
p < 0.001, mean difference = 0.296, 95% CI [0.166, 0.426]). There were no significant differences between Asian and NHW youth in pain catastrophizing, anxiety and depression.
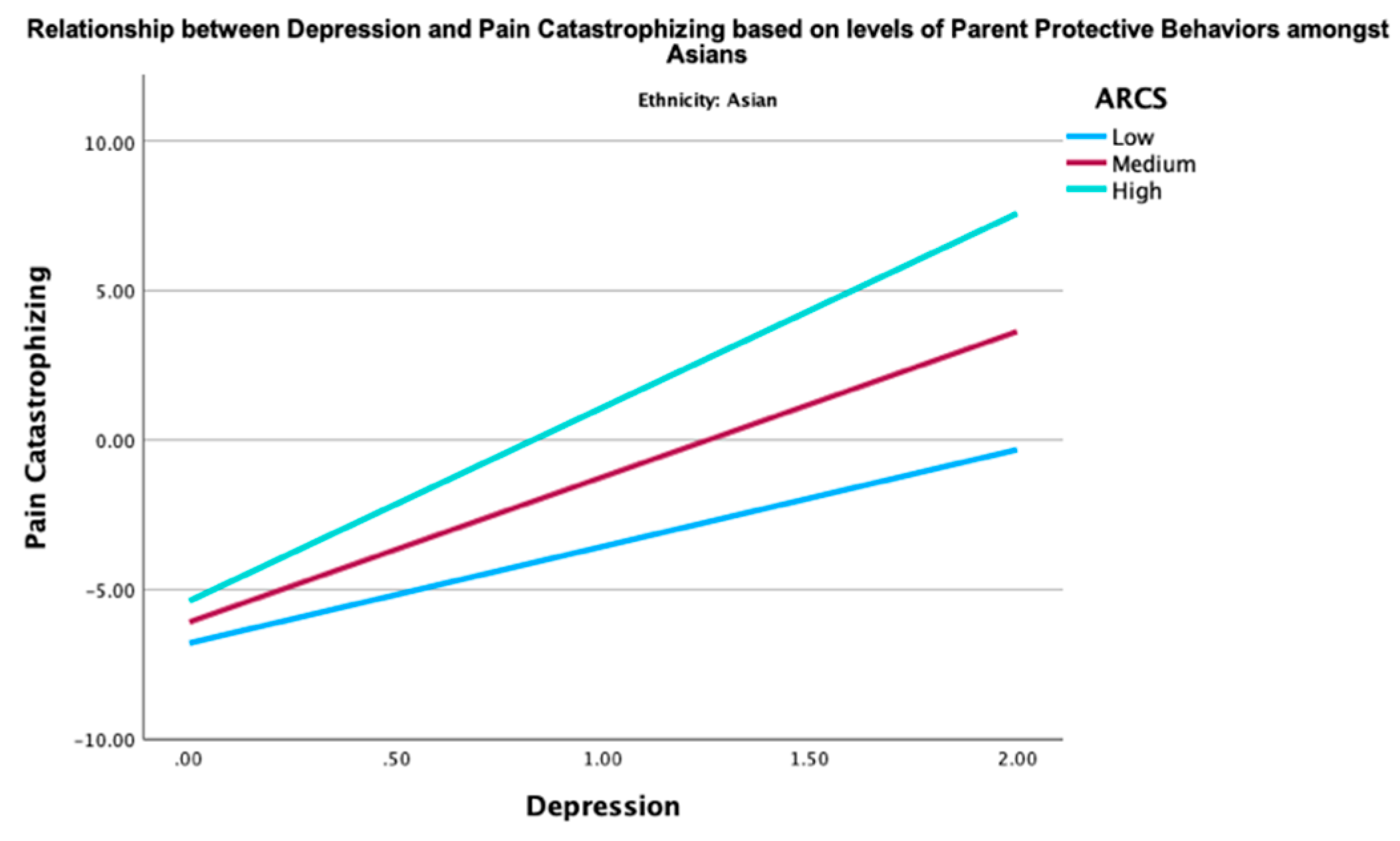
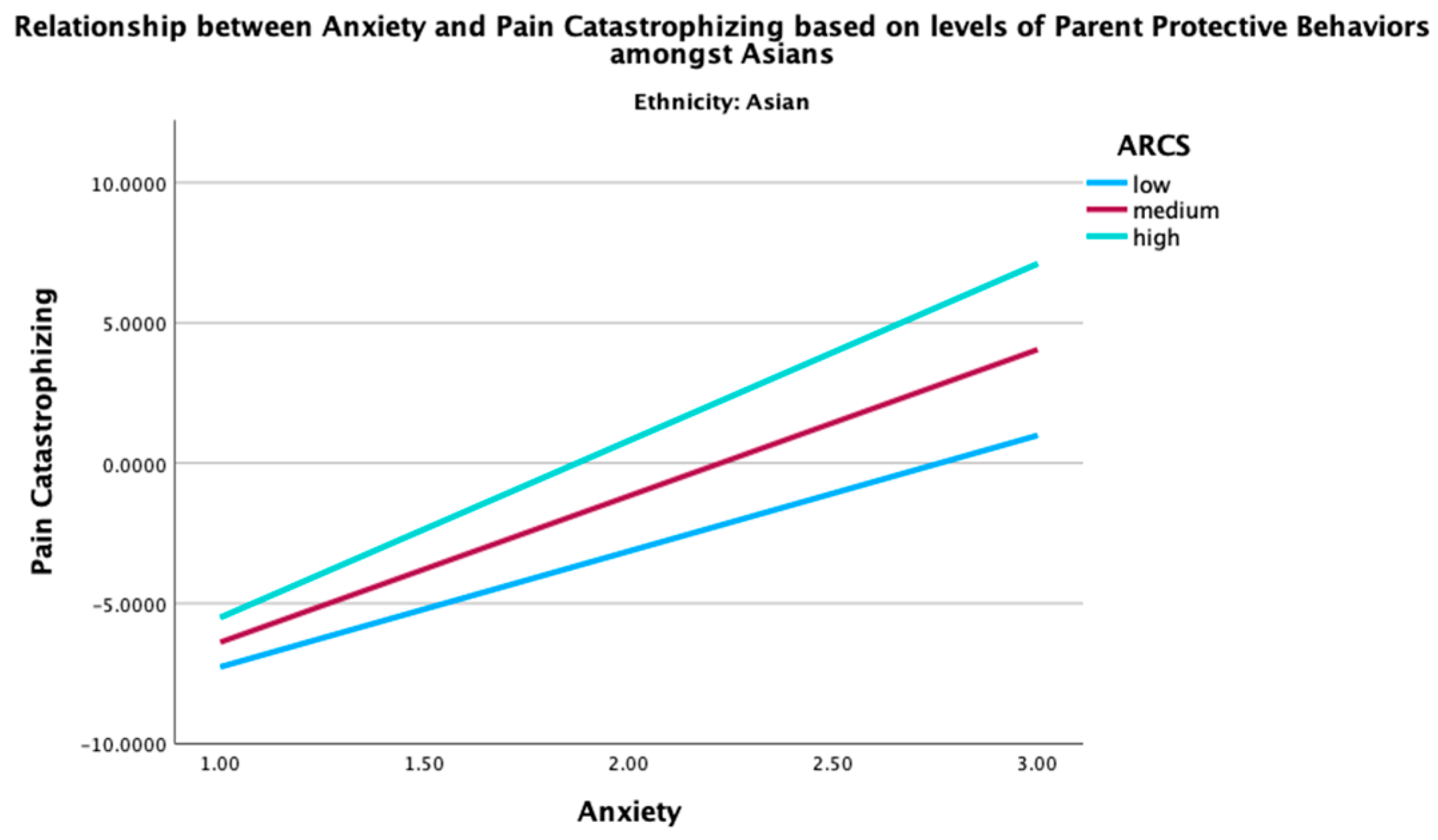
For aim 2, none of the moderation effects of all six models for the NHW population were statistically significant. Two of the moderation effects for the Asian population were statistically significant as indicated in
Table 3. Parent protective behaviors moderated the relationship between anxiety and pain catastrophizing (B = 0.19, SE = 0.06, β = 0.18,
p = .002). Secondly, parent protective behaviors moderated the relationship between depression and pain catastrophizing (B = 0.13, SE = 0.06, β = 0.12,
p = .038).
Given the significant moderation effect of the parent protective behaviors in the relationship between global distress and pain catastrophizing in Asian youth, two post-hoc three-way interaction analyses were conducted to examine how ethnicity, parent protective behaviors, and global distress (depression or anxiety) together influence pain catastrophizing. The three-way interactions between ethnicity, parent protective behaviors, and global distress (depression (B = -0.22
, p <0.001) and anxiety (B = -.18, p = 0.008) were both significant. These findings indicate that the combined effect of parent protective behaviors and global distress on pain catastrophizing was moderated by ethnicity. Specifically, the interaction term between ethnicity and parent protective behaviors revealed that the association between parent protective behaviors and pain catastrophizing was stronger among Asians, as elucidated in
Figure 1 and
Figure 3 in comparison to their NHW counterparts (
Figure 2 and
Figure 4). This may imply that Asian youth with higher levels of anxiety or depression are more sensitive to the effects of parent protective behaviors on pain catastrophizing than their NHW counterparts.
Discussion
The current study provides important insights into the experience of pediatric chronic pain within Asian families, a growing demographic that has been underrepresented in previous research. One of the most striking findings in the current study was the significant ethnic differences in pain intensity, pain interference, and parent protective behaviors. Asian youth reported lower levels of pain intensity and pain interference compared to their NHW counterparts, with the differences being large and statistically significant. This suggests that cultural factors may play a role in how pain is perceived and reported, aligning with their low representation in tertiary pain clinics[
14]. Further, Asian parents reported significantly higher levels of parent protective behaviors than NHW parents. These behaviors likely include actions such as shielding children from stressful situations, providing emotional support during pain episodes, and possibly limiting exposure to pain-inducing activities. The finding that Asian parents engage in more protective behaviors is consistent with cultural values that emphasize family cohesion[
19] and parental involvement[
16], which may be more pronounced in some Asian cultures compared to Western ones. This could reflect cultural norms around parenting, where greater parental control or care is perceived as a form of protection or support for children[
16], particularly when managing distress or pain. However, pain catastrophizing, depression, and anxiety were not significantly different between the two racial/ethnic groups.
Secondly, for Asians only, parent protective behaviors moderated the relationship between global distress and pain catastrophizing. Contrary to our hypothesis—that greater parent protective behaviors might buffer or mitigate the effects of global distress on pain-related outcomes—our results indicate that for Asian youth, the association between global distress and pain catastrophizing is strengthened when parent protective behaviors are high. Furthermore, the significant three-way interaction among ethnicity, parent protective behaviors, and global distress suggests that the influence of parent protective behaviors on pain catastrophizing is not uniform across ethnic groups; it is notably stronger among Asian youth. These findings suggest cultural differences in the interplay between parenting practices, psychological distress, and pain-related outcomes. This may be reflective of the “Striving, Persistent, Behavioral Style” (SPBS)
17, which posits that while Asian adolescents are driven and high achieving, they also tend to suppress emotional expression due to cultural values such as stoicism
18. This aligns with existing literature showing Asian youth are more prone to internalizing symptoms, such as anxiety and depression, than their NHW peers[
7,
20].
Combined with the existing research of Asian youth and mental health, these findings present an inconsistent narrative: while Asian youth report higher rates of mental health challenges, they also report lower pain intensity and prevalence, accompanied by greater levels of parent protective behaviors. This inconsistency highlights the importance of considering cultural frameworks and coping mechanisms, such as stoicism and collectivistic values that may influence healthcare-seeking behaviors and pain reporting.
Several explanations may help frame the results of our study. Broadly, Western analysis characterizes Asian families to differ from Caucasian families due to a collectivistic mindset (as opposed to individualistic), in which Asians prefer interdependence and group harmony over independence and meeting individual needs
7. This collectivistic framework may partly explain l
ower rates of formal help-seeking (e.g., from healthcare providers) compared to other ethnic groups [
21]
often due to a sense of familial obligation[
16]
. Rooted in Confucian value of familism, which positions the family as society’s foundation[
22]
this cultural value may discourage help-seeking when it appears to prioritize individual needs over the needs and concerns of the family. Additionally, help-seeking behaviors amongst Asians may be influenced by preference for complementary and alternative medicine (CAM) use of treatment[
23,
24]
, lack of knowledge of healthcare access[
4]
, perception of pain as a natural part of life rather than a treatable condition [
25,
26]
, or adoption of stoicism[
26]
Additionally, we may be misassessing the chronic pain experience among Asians due to the influence of the model minority myth both systemically and individually internalized. Systemically internalized model minority myth has made a faulty assumption that there is a reduced urgency to address the distress experienced by Asians, due to their high functionality, resilience, and academic competence. This assumption is reinforced by low levels of pain prevalence, pain intensity, and pain interference. A personally internalized model minority myth may also shape how Asian youth perceive, cope with, and report pain, leading them to minimize their experiences in favor of group needs, consistent with a collectivistic mindset[
16,
20]. Together, these systemic and individual expressions of the model minority myth are cyclical; research on Asian populations in health literature is sparse due to the perception that there is not a need for such research, survey measures administered in clinical spaces have not sought to ask questions specific to the Asian experience and different expressions of pain, and Asians may align their externalizing expressions of pain with societal and personal expectations. Stoicism, reinforced by the model minority myth, may further contribute to this phenomenon, as evidenced by a few striking pediatric studies. For example, Thai children relied significantly more on covert coping methods (e.g., distraction via thinking of favorite things) whereas American children reported more explicit coping methods (e.g., screaming)[
27,
28]. Similarly, when undergoing immunization, Japanese babies were significantly more likely to demonstrate low behavioral, but high cortisol response compared to White infants who were more likely to display high behavioral but low cortisol response[
28,
29]. These studies align with SPSB’s[
17] conceptualization of emotion suppression, prevention motivation, and unmodulated persistence. Furthermore, Asians who function in the SPBS framework are nested under contexts such as oppression, structural racism, and chronic stress, which increase allostatic load and risk for health problems such as pediatric chronic pain.
However, it is also important to note
resiliency factors that may be unique to Asian families. Asian families may pull from resiliency factors such as: greater openness to complementary/integrative management procedures [
24,
30] reliance on community/family system[
31], and overall self-management protocols to navigate pain [
32]. The SPBS also denotes grit, perseverance, and resilience as an undeniable component to the framework[
17], that when nested in more supportive systems, may highly serve the Asian demographic. These findings underscore the importance of cultural context when considering interventions for youth with chronic pain and distress. For Asian youth, interventions that target family dynamics—particularly those aimed at optimizing parent-child interactions—may be critical. Tailored interventions might include training for parents to provide supportive but not overprotective behaviors, thereby mitigating the amplifying effect of high global distress on pain catastrophizing. Clinically it may be particularly important to attend to Asian youth with higher reported distress, as results indicate that they may be more negatively impacted by the interaction of parent protective behaviors, thus exacerbating pain catastrophizing. A personalized approach to treatment that considers cultural values, family dynamics, and individual coping strategies is essential in providing optimal care for youth facing both depression and chronic pain.
Several limitations must be acknowledged. First, the cross-sectional design precludes causal inferences. Future longitudinal studies are needed to examine how these relationships develop over time. Second, the disparity in group sizes, particularly the smaller Asian sample, warrants caution; future studies should aim to recruit larger and more geographically diverse Asian samples. Third, the study’s measures (e.g., the unidimensional assessment of parent protective behaviors) may not fully capture the culturally nuanced behaviors unique to different Asian subgroups. Finally, the label “Asian” encompasses a highly heterogeneous group, tracing its roots to more than 20 different countries; future research should explore intra-Asian differences, including the roles of immigration status, language proficiency, and acculturation. Future studies may also examine differences in parent protective behaviors by age group of youth experiencing chronic pain to better understand the interplay of developmental milestone on ways that parenting practices influence pain outcomes.
Limitations notwithstanding, this study is the first to investigate pediatric chronic pain in a large sample of Asian youth, revealing nuanced interactions among cultural values, parent protective behaviors, and psychological and pain related distress. Our findings challenge the assumption that Asian youth are at lower risk for pain-related issues simply because they report lower pain intensity and interference. In fact, our results suggest that youth experiencing greater levels of anxiety and depression may be more sensitive to parent protective behaviors, thus intensifying pain catastrophizing. These insights underscore the need for culturally informed approaches in both research and clinical practice, ensuring that interventions are sensitive to the unique experiences and challenges faced by Asian youth with chronic pain. Future directions should investigate the mechanism of parent protective behaviors in Asian families and experience of chronic pain. Specifically, the severity of mental health may differentially impact the way in which parent protective behaviors are internalized and therefore have a different influence on pain-related outcomes. Further research is needed to gather experiences of chronic pain in the community to assess culturally informed healthcare barriers. Qualitative studies are essential to lean into lived, rich, and heterogenous experiences of Asians, identifying vulnerability and resiliency factors that influence access to tertiary pain clinics, and examining familial dynamics in pediatric chronic pain. A deeper understanding of these elements will inform more inclusive, culturally responsive pain management strategies, ultimately improving care for underserved populations.
Author Contributions
Conceptualization, Y.K.K., R.M., and R.P.B.; Methodology, Y.K.K., R.M., and R.P.B.; Formal analysis, Y.K.K.; Writing – Y.K.K., R.M., and R.P.B.; Supervision, R.P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Approval was obtained from the Stanford University ethics committee.
Informed Consent Statement
Consent was not required for this study as information collected was retrospective patient chart review within standard clinical care.
Data Availability Statement
The deidentified dataset is not publicly available due to Stanford Medicine policy regarding patient privacy and data sharing. Request to access the dataset should be directed to Dr. Kim (
yoonheek@stanford.edu) to inquire regarding the possibility of a data-sharing agreement.
Acknowledgements
The authors would like to acknowledge Beth De Souza, PhD, Data analyst, for her consultation and support in the data analysis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Birnie, K.A.; Heathcote, L.C.; Bhandari, R.P.; Feinstein, A.; Yoon, I.A.; Simons, L.E. Parent physical and mental health contributions to interpersonal fear avoidance processes in pediatric chronic pain. Pain 2020, 161, 1202–1211. [CrossRef]
- Chambers, C.T.; Dol, J.; Tutelman, P.R.; Langley, C.L.; Parker, J.A.; Cormier, B.T.; Macfarlane, G.J.; Jones, G.T.; Chapman, D.; Proudfoot, N.; et al. The prevalence of chronic pain in children and adolescents: a systematic review update and meta-analysis. Pain 2024, 165, 2215–2234. [CrossRef]
- Ruiz, A.B. and N.G. Asian Americans are the fastest-growing racial or ethnic group in the U.S. Pew Research Center 2021.
- Yang, K.G.; Rodgers, C.R.R.; Lee, E.; Lê Cook, B. Disparities in Mental Health Care Utilization and Perceived Need Among Asian Americans: 2012–2016. PS 2020, 71, 21–27. [CrossRef]
- Rowelll, L.N.; Mechlinl, B.; Jil, E.; Addamol, M.; Girdlerl, S.S. Asians differ from non-Hispanic Whites in experimental pain sensitivity. European Journal of Pain 2011, 15, 764–771. [CrossRef]
- McGreevy, K.; Bottros, M.M.; Raja, S.N. Preventing chronic pain following acute pain: Risk factors, preventive strategies, and their efficacy. European Journal of Pain Supplements 2011, 5, 365–376. [CrossRef]
- Wang, C.; Liu, J.L.; Havewala, M.; Zhu, Q.; Do, K.A.; Shao, X. Parent–Child Connect: A culturally responsive parent training for Asian American parents at school. Psychology in the Schools 2021, 58, 1624–1641. [CrossRef]
- Kolaitis, G.; Van Der Ende, J.; Zaravinos-Tsakos, F.; White, T.; Derks, I.; Verhulst, F.; Tiemeier, H. The occurrence of internalizing problems and chronic pain symptoms in early childhood: what comes first? Eur Child Adolesc Psychiatry 2022, 31, 1933–1941. [CrossRef]
- Peterson, C.C.; Palermo, T.M. Parental Reinforcement of Recurrent Pain: The Moderating Impact of Child Depression and Anxiety on Functional Disability. Journal of Pediatric Psychology 2004, 29, 331–341. [CrossRef]
- Walker, L.S. Social Consequences of Children’s Pain: When Do They Encourage Symptom Maintenance? Journal of Pediatric Psychology 2002, 27, 689–698. [CrossRef]
- Gidron, Y.; McGrath, P.J.; Goodday, R. The physical and psychosocial predictors of Adolescents’ recovery from oral surgery. J Behav Med 1995, 18, 385–399. [CrossRef]
- Palermo, T.M.; Chambers, C.T. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain 2005, 119, 1–4. [CrossRef]
- Donnelly, T.J.; Palermo, T.M.; Newton-John, T.R.O. Parent cognitive, behavioural, and affective factors and their relation to child pain and functioning in pediatric chronic pain: a systematic review and meta-analysis. PAIN 2020, 161, 1401. [CrossRef]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [CrossRef]
- Choi, Y.; Kim, Y.S.; Kim, S.Y.; Park, I.J.K. Is Asian American parenting controlling and harsh? Empirical testing of relationships between Korean American and Western parenting measures. Asian American Journal of Psychology 2013, 4, 19–29. [CrossRef]
- Benito-Gomez, M.; Williams, K.N.; McCurdy, A.; Fletcher, A.C. Autonomy-Supportive Parenting in Adolescence: Cultural Variability in the Contemporary United States. J of Family Theo & Revie 2020, 12, 7–26. [CrossRef]
- Doan, S.N.; Yu, S.H.; Wright, B.; Fung, J.; Saleem, F.; Lau, A.S. Resilience and Family Socialization Processes in Ethnic Minority Youth: Illuminating the Achievement-Health Paradox. Clin Child Fam Psychol Rev 2022, 25, 75–92. [CrossRef]
- Bhandari, R.P.; Feinstein, A.B.; Huestis, S.E.; Krane, E.J.; Dunn, A.L.; Cohen, L.L.; Kao, M.C.; Darnall, B.D.; Mackey, S.C. Pediatric-Collaborative Health Outcomes Information Registry (Peds-CHOIR): a learning health system to guide pediatric pain research and treatment. Pain 2016, 157, 2033–2044. [CrossRef]
- Ta, V.M.; Holck, P.; Gee, G.C. Generational Status and Family Cohesion Effects on the Receipt of Mental Health Services Among Asian Americans: Findings From the National Latino and Asian American Study. Am J Public Health 2010, 100, 115–121. [CrossRef]
- Choi, Y.; Park, M.; Lee, J.P.; Lee, M. Explaining the Asian American Youth Paradox: Universal Factors versus Asian American Family Process Among Filipino and Korean American Youth. Family Process 2020, 59, 1818–1836. [CrossRef]
- Guo, S.; Nguyen, H.; Weiss, B.; Ngo, V.K.; Lau, A.S. Linkages between mental health need and help-seeking behavior among adolescents: Moderating role of ethnicity and cultural values. Journal of Counseling Psychology 2015, 62, 682–693. [CrossRef]
- Ta, C.K. Parenting in Context: Considering Culture and Context in the Evaluation of Harsh Parenting and Parent-child Relationships. Ph.D., Fuller Theological Seminary, School of Psychology: United States -- California, 2019.
- Groenewald, C.B.; Beals-Erickson, S.E.; Ralston-Wilson, J.; Rabbitts, J.A.; Palermo, T.M. Complementary and alternative medicine use by children with pain in the United States. Acad Pediatr 2017, 17, 785–793. [CrossRef]
- Complementary and Alternative Medicine Use Among Asian-American Subgroups: Prevalence, Predictors, and Lack of Relationship to Acculturation and Access to Conventional Health Care Available online: https://www.liebertpub.com/doi/epdf/10.1089/acm.2006.12.1003 (accessed on Dec 11, 2024).
- Dickson, G.L.; Kim, J.I. Reconstructing a Meaning of Pain: Older Korean American Women’s Experiences with the Pain of Osteoarthritis. Qual Health Res 2003, 13, 675–688. [CrossRef]
- Pillay, T.; Zyl, H.A.V.; Blackbeard, D. Chronic Pain Perception and Cultural Experience. Procedia - Social and Behavioral Sciences 2014, 113, 151–160. [CrossRef]
- McCarty, C.A.; Weisz, J.R.; Wanitromanee, K.; Eastman, K.L.; Suwanlert, S.; Chaiyasit, W.; Band, E.B. Culture, Coping, and Context: Primary and Secondary Control among Thai and American Youth. Journal of Child Psychology and Psychiatry 1999, 40, 809–818. [CrossRef]
- Kristjánsdóttir, Ó.; Unruh, A.M.; McAlpine, L.; McGrath, P.J. A Systematic Review of Cross-Cultural Comparison Studies of Child, Parent, and Health Professional Outcomes Associated With Pediatric Medical Procedures. The Journal of Pain 2012, 13, 207–219. [CrossRef]
- Lewis, M.; Ramsay, D.S.; Kawakami, K. Differences between Japanese Infants and Caucasian American Infants in Behavioral and Cortisol Response to Inoculation. Child Development 1993, 64, 1722–1731. [CrossRef]
- Felicilda-Reynaldo, R.F.D.; Choi, S.Y.; Driscoll, S.D.; Albright, C.L. A National Survey of Complementary and Alternative Medicine Use for Treatment Among Asian-Americans. J Immigrant Minority Health 2020, 22, 762–770. [CrossRef]
- Kim, H.S.; Sherman, D.K.; Taylor, S.E. Culture and social support. American Psychologist 2008, 63, 518–526. [CrossRef]
- Kawi, J.; Reyes, A.T.; Arenas, R.A. Exploring Pain Management Among Asian Immigrants with Chronic Pain: Self-Management and Resilience. J Immigrant Minority Health 2019, 21, 1123–1136. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).