1. Introduction
The information required to analyze the factors influencing the progression of idiopathic scoliosis (IS) is sourced from scoliosis clinics in hospitals and School Scoliosis Screening (SSS) programs. Within SSS programs, examiners frequently detect cases of mild or early-stage IS, enabling them to collect data from this specific group of children. Conversely, physicians in outpatient clinics primarily gather information from patients with more advanced scoliosis, at a stage suggesting that may not have been captured during the initial or mild phases of the condition. This distinction in data collection is significant, as the underlying biomechanical characteristics of early-stage and mild scoliosis are likely different from those observed in severe cases
. Furthermore, the identification of curves that will progress beyond the surgical threshold was historically a significant challenge of orthopedic surgeons who examine and treat children with mild and moderate scoliotic curves [
1].
At the onset of IS and in its milder forms, genetic, epigenetic, and biological factors play a predominant role in its development, with minimal to no structural changes in the skeleton. However, the influence of patho-biomechanics, though initially secondary, becomes more pronounced as the condition progresses and skeletal deformities become well established [
2].
Noshchenko et al. (2015) highlighted that inconsistencies across published studies, coupled with variations in assessment methods and clinical parameters, limit the reliability of existing criteria for predicting which children with mild IS will experience curve progression necessitating intervention. Furthermore, their review did not identify any predictive models for the progression of adolescent idiopathic scoliosis (AIS) that could be recommended as clinical diagnostic tools [
3].
Commonly cited predictors in the literature include biological factors (such as sex, age, and growth patterns), anatomical and clinical characteristics (including thoracic deformity, rib hump, leg length discrepancy, and trunk imbalance), radiographic or imaging markers (such as the Cobb angle, vertebral rotation, torsion, tilt, wedging of the vertebral body, segmental thoracic ratios, Rib-Vertebra Angles (RVAs), segmental RVAs, and the torsion index), as well as genetic influences (including specific genes and familial inheritance patterns). A multivariate logistic regression model which includes biomarkers as well as clinical and radiographic findings was recently intoduced by Zhang et al to predict curves that will possibly exceed a Cobb angle of 40 degrees [
4].
In contemporary research, three-dimensional analysis is increasingly employed to examine IS curve morphology, as studies limited to coronal, sagittal, or transverse planes alone have inherent limitations. However, key radiological parameters—such as the Cobb angle, Mehta RVAs, and Perdriolle angles—are traditionally measured using posteroanterior (PA) and lateral radiographs. While 3D assessments of the spine and rib cage provide valuable insights, they require specialized imaging equipment, and 3D reconstructions from CT scans are not routinely performed due to radiation exposure concerns [
5,
6,
7,
8,
9,
10,
11]. There are numerous efforts in the literature to create predictive models for curve progression but most of them proved to be ineffective mainly due to the fact that the weighting of each individual factor in these models is not known [
12].
Recent years have seen a rise in interdisciplinary research applying machine learning to clinical data to develop predictive models for scoliosis progression. These studies often employ specialized terminology, which can be complex and difficult to interpret, yet the models themselves frequently rely on 2D parameters extracted from standard radiographs [
13,
14,
15,
16,
17,
18].
From a practical standpoint, studies utilizing PA radiographs continue to offer significant value. Lateral radiographs are not routinely obtained for children with IS, and many hospitals face limitations in conducting retrospective studies, often relying primarily on frontal-plane radiographs. Additionally, standard chest radiographs of children and adolescents, commonly archived in medical records, can be effectively repurposed for research without necessitating additional radiation exposure. A recent effort has explored generating sagittal radiographs from coronal views using a Generative Adversarial Network (GAN) based deep learning framework for AIS. However, as the study authors acknowledge, "although these synthetic images appear visually similar to real ones, their quality is still inadequate for precise clinical evaluation." [
19].
This review aims to summarize the parameters used in a representative selection of studies as predictors of scoliosis curve progression. Furthermore, it introduces the Rib Index and Segmental Rib Index as potential predictors for IS progression.
2.Cobb Angle – Rib Hump
Normal spine consists of bony vertebrae which connect the base of the skull to the pelvis and are joined by cartilagenous intervertabral discs. The vertebral column is straight in the coronal plane and presents four curves in the sagital plane, two kyphotic in the thoracic and in the sacral level and two lordotic in the cervical and in the lumbar segment respectively. Any deviation of the spine in the coronal plane beyond 10 degrees is considered as a scoliotic curvature and it usually affects additionally the saggital curves and eventually a 3D deformity of the spine occurs.
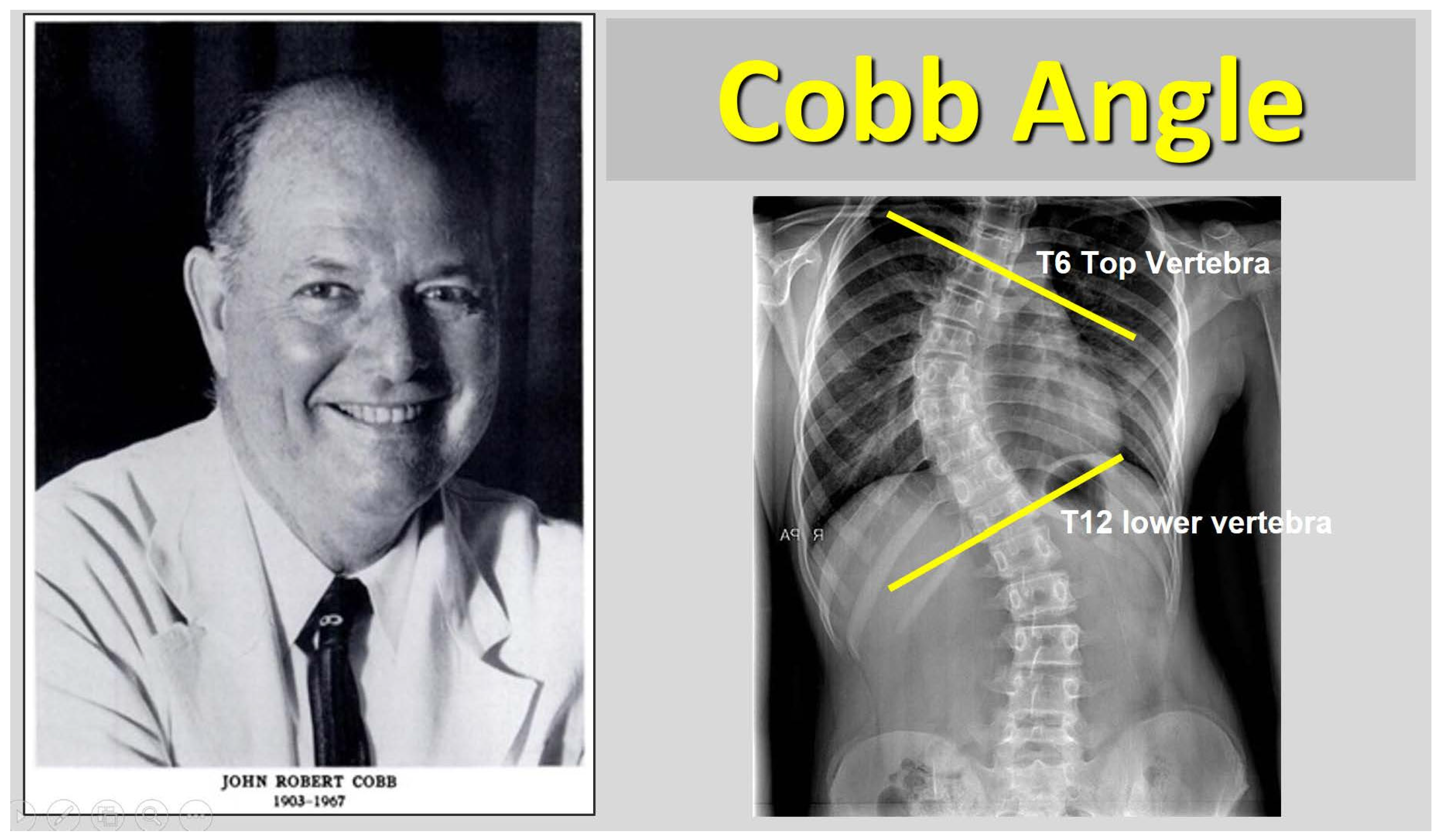
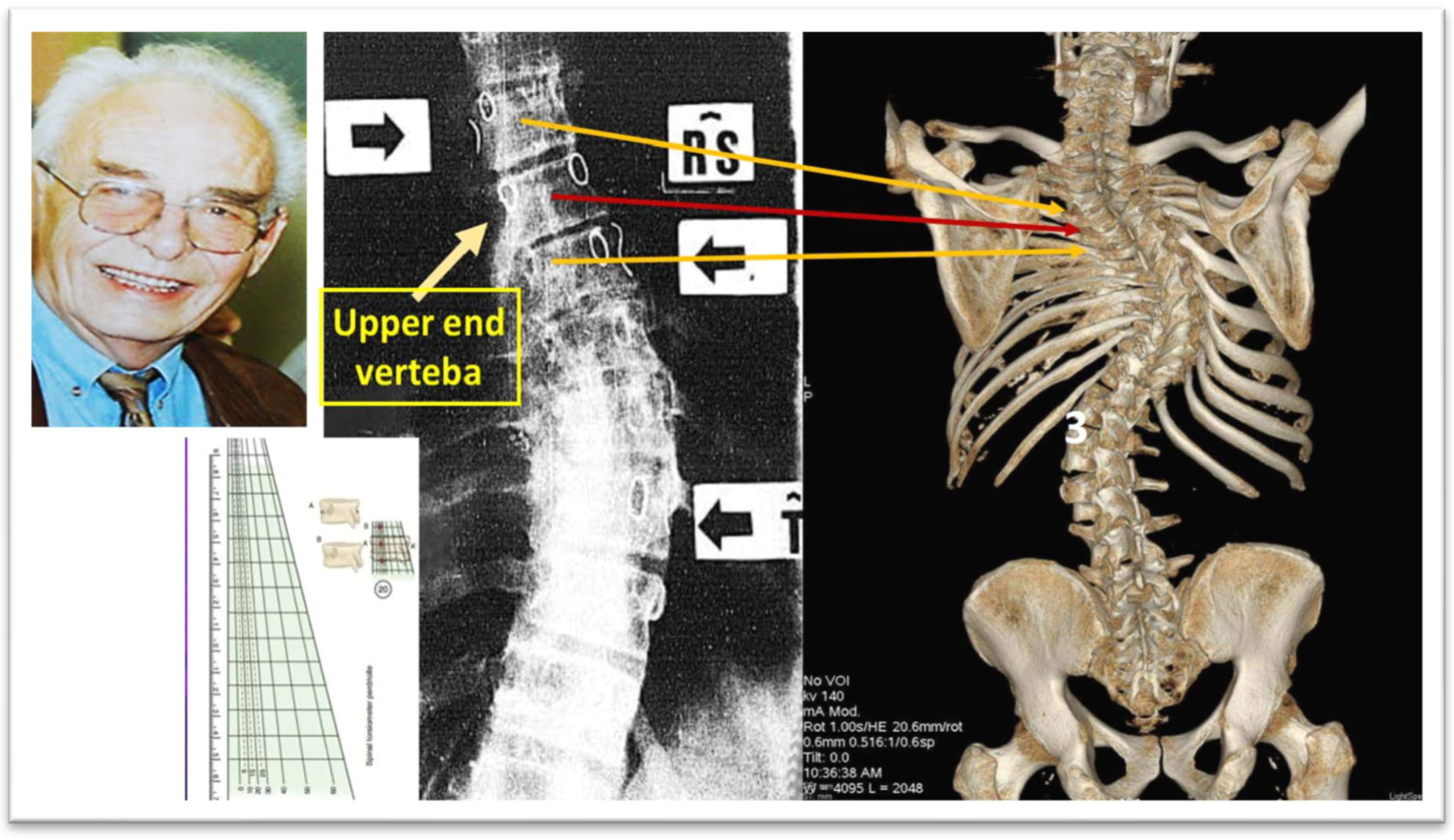
Since 1948, when John Robert Cobb introduced his technique for evaluating scoliotic curvature, the Cobb angle has been recognized as the benchmark for determining the severity of IS. Furthermore, it serves as the primary predictor in nearly all research studies and models related to IS progression (
Figure 1, [
20]).
The forward bending test, also known as the Adams test, was named after the English physician William Adams, who first described it in 1865 [
21]. This test is commonly used as an initial clinical evaluation for children suspected of having IS. It is frequently employed in school scoliosis screening programs and can also be applied to patients with a family history of scoliotic posture or cases where scoliosis of uncertain origin is observed. Duval-Beauper (1992) reported that over 95% of patients with an initial supine angle exceeding 17 degrees, a standing angle greater than 24 degrees, and a rib hump larger than 11 mm experienced progressive scoliosis [
22,
23]. Additionally, in 95-100% of patients whose parameters at follow-up surpassed these thresholds (supine angle: 17 degrees, standing angle: 24 degrees, rib hump: 11 mm), the condition continued to worsen, confirming curve progression.
3. Methods for Assessing the Degree of Skeletal Maturity
Assessing skeletal maturity in AIS could significantly influence disease management. However, given that AIS is a complex and multifactorial condition, it is unlikely that a single metric will suffice to accurately predict its progression. As more contributing factors to IS progression are identified, it is crucial for the scientific community to collaborate in developing treatment strategies grounded in reliable and consistent algorithms [
24].
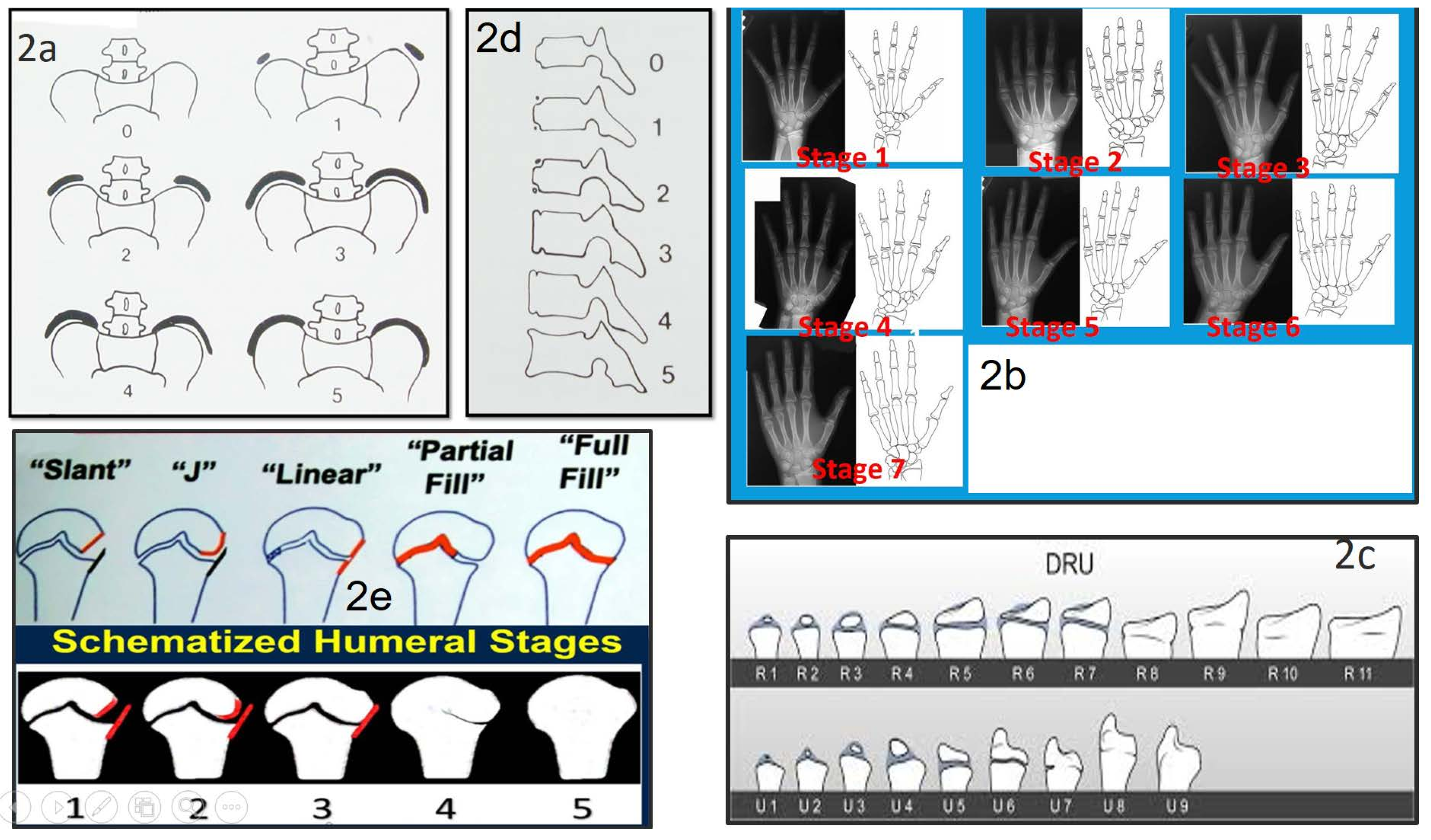
Several methods have been utilized to determine skeletal maturity, including Risser’s method (Risser sign), the Sanders maturity scoring system, the Distal Radius and Ulna (DRU) classification, ossification of the vertebral epiphyseal rings, ossification of the humeral head, and ossification of the calcaneal apophysis, as shown in
Figure 2 [
25,
26,
27,
28,
29,
30].
3.1. The Iliac Apophysis and the Evolution of Curves in Scoliosis
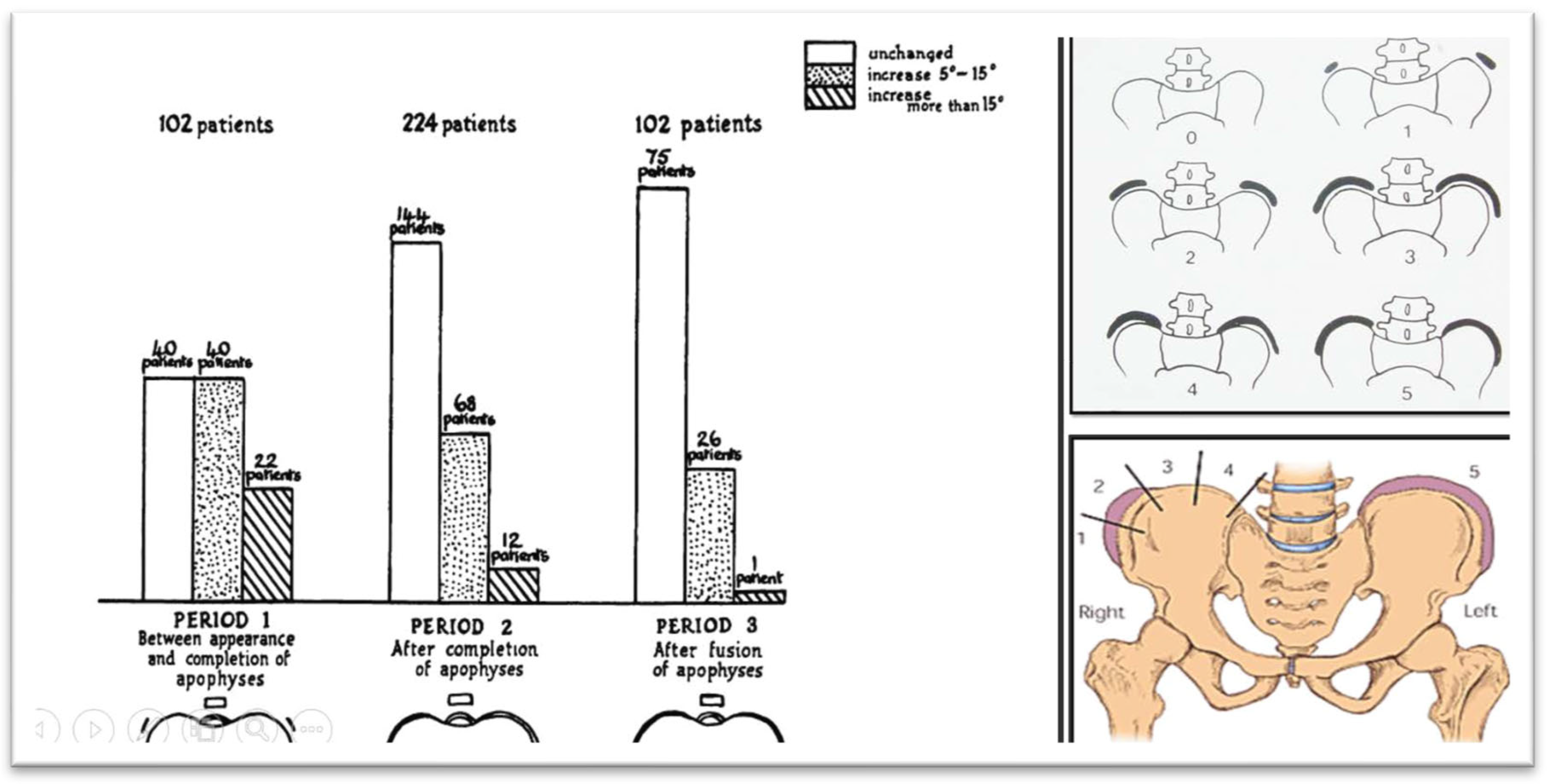
Zaoussis and James (1958) carried out a study investigating the radiographic characteristics of the ossification center in the iliac apophysis and its correlation with other indicators of maturation, including the onset of menstruation and the formation of vertebral body apophyses in relation to scoliosis curve progression. This study was the first to present statistical evidence demonstrating that skeletal maturation, marked by the complete development of the iliac apophysis, signifies the conclusion of substantial scoliosis progression (
Figure 3, [
31]).
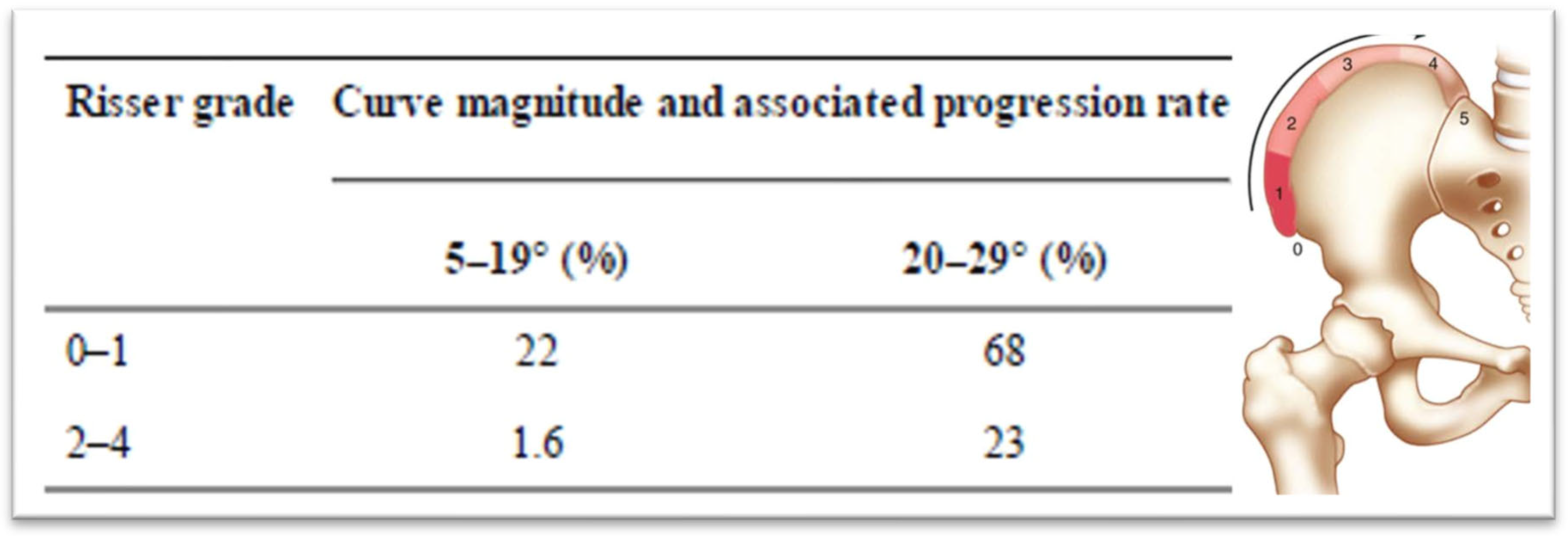
In 1984, Lonstein and Carlson presented research on the probability of curve progression in untreated AIS during growth, considering the Risser sign grade and curve severity (
Figure 4, [
32]).
3.2. Sanders Skeletal Maturity Staging System
The Sanders Skeletal Maturity Staging System is a simplified approach to evaluating skeletal development. It is a reliable method that exhibits a stronger association with the progression of IS compared to the Risser sign or skeletal age assessment using the Greulich and Pyle method. Although it requires some initial learning, it is easy to implement in clinical settings. When combined with information about the curve type and size, this system effectively predicts the likely progression of IS curves over time [
26]. Curve progression in IS showed a strong correlation with the initial curve magnitude and skeletal maturity in both female and male children. All patients at Sanders stage (SS) 2 with an initial Cobb angle of 25° or greater experienced progression, as did those at SS1 and SS3 with an initial Cobb angle of 35° or greater. Similarly, all patients with an initial Cobb angle of 40° or greater progressed, except those in SS7. On the other hand, none of the patients with an initial Cobb angle of 15° or less, or those in SS5, SS6, and SS7 with an initial Cobb angle of 30° or less, showed progression [
26].
3.3. Distal Radius and Ulna Classification (DRU) Scheme in Predicting Growth Peak and Curve Progression in Idiopathic Scoliosis
The DRU (Distal Radius and Ulna) classification by Luk et al. (2014), serves as a prognostic framework for evaluating growth potential in children and adolescents. It relies on radiographic assessment to determine skeletal maturity, categorizing development into 11 radius stages (R1–R11) and 9 ulna stages (U1–U9). Significant markers within this system include a
Peak Growth Phase which is recognized at radius stage R7 and ulna stage U5, signifying a period of accelerated growth and an
end of growth phase which is represented by radius stage R10 and ulna stage U9, indicating that skeletal growth is approaching completion or has ceased. This classification has been validated as a dependable tool for forecasting growth stages, making it particularly valuable in clinical applications for growth-related interventions, such as those in IS [
27].
3.4. Ossification of the Vertebral Epiphyseal Rings
The ossification center in the epiphyseal ring emerges between the ages of 11 and 14, appearing earlier in girls than in boys. This timeframe largely coincides with the period of curve progression in AIS [
29].
3.5. Ossification of the Humeral Head
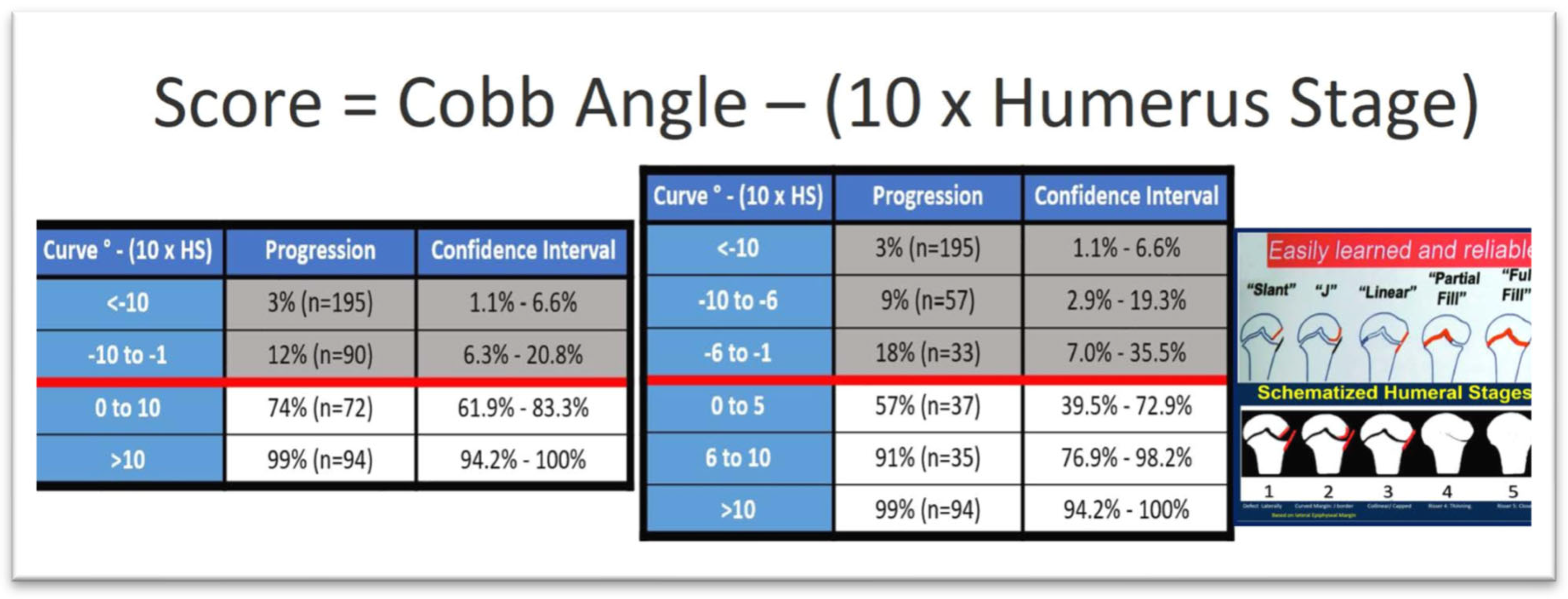
The proximal humeral ossification system provides a reliable method for estimating Peak Height Velocity (PHV) in individuals with IS using a standard spine radiographs, thus removing the need for a separate hand radiographs to assess bone age. This method improves the precision of maturity predictions, enabling healthcare providers to more accurately assess a patient’s skeletal maturity in relation to PHV. As a result, it supports more informed treatment decisions while minimizing additional radiation exposure, time, and costs. Assessing the proximal humeral physis in spine radiographs that include the shoulder serves as a practical and valuable tool for determining skeletal maturity in adolescents with IS, also it was reported that the humeral head classification system showed a strong relationship with the age at PHV and the remaining growth percentage. Furthermore, the staging system demonstrated excellent reliability in both inter-observer and intra-observer assessments, suggesting its broad applicability [
33]. Additionally Li et al (2018), presented a formula to assess the progression to a surgical range of a AIS curve and the score is calculated by subtracting from the Cobb angle the tenfold stage of ossification of the humeral head,
Figure 5 [
33].
3.6. Ossification of Calcaneal Apophysis
The calcaneal apophysis undergoes ossification in a well-defined sequence, divided into six stages. These stages are closely tied to specific periods related to the PHV, making the calcaneal system a reliable method for assessing skeletal maturity. The PHV occurs before the iliac bone begins to ossify, while the calcaneal apophysis follows a sequence of four ossification stages before PHV and two stages after it [
34].
Ossification of the calcaneal apophysis is an effective indicator of skeletal maturity during adolescence. The calcaneal system is most useful in pinpointing maturity in the five years leading up to PHV, whereas the Sanders system is more effective for identifying maturity after PHV. By combining different maturity systems, it is possible to achieve a more accurate assessment of maturity than relying on any single system alone [
30].
4. Prognostic Factors of IS Progression According to the Patient’s Presentation Age
After evaluating a child or adolescent with scoliosis, both the parents and the patient often inquire about the prognosis of the condition. A useful way to categorize the prognosis is based on the patient’s age and presentation, which includes: Infantile Idiopathic Scoliosis (IIS), Childhood Idiopathic Scoliosis (CIS), Adolescent Idiopathic Scoliosis (AIS) in its untreated form, AIS patients who have been treated with braces, and those with Skeletally Mature Idiopathic Scoliosis (IS).
4.1. Infantile Idiopathic Scoliosis (IIS)
IIS can be categorized based on the resolution or progression of the spinal curve into several types: early resolving, late resolving, benign progressive, malignant progressive, and dysplastic. It is more commonly seen in boys, particularly with left thoracic or thoracolumbar curves. A distinctive feature of IIS is that it is the only form of IS known to sometimes resolve on its own, improving or even disappearing without the need for treatment, except for monitoring.
In 1930, Hartenstein [
35,
36] reported that spontaneous correction could occur without intervention, although it was not possible to predict this at the time of diagnosis. Mehta, in 1972, introduced the rib-vertebra angle (RVA) as a tool to differentiate between resolving and progressive IIS. Her study found that when the RVA difference (RVAD) was less than 20°, around 80% of patients experienced spontaneous resolution of their scoliosis. However, in patients with an RVAD greater than 20°, 80% showed progression of their scoliosis [
37].
A study by Agadir et al. (1992) followed 18 patients with progressive IIS over an average of 7 years. It showed that the relationship between the progression of the spinal curvature (measured by Cobb Angle, CA) and apical vertebral rotation (AVR) could identify four types of progressive IIS curves. Type I showed synchronous progression of CA and AVR, Type II showed progression of CA while AVR resolved to some extent, Type III showed resolution of CA while AVR continued to progress, and Type IV showed temporary resolution of both CA and AVR before they progressed again [
38]. This dissociation between CA and AVR progression suggests complex neuromuscular factors that regulate scoliosis development in both the frontal and transverse planes [
39,
40].
Progressive IIS, like AIS, may result from asymmetries in the central pattern generators (CPGs) controlling trunk movements during gait [
41,
42]. According to Mehta (1972), progressive IIS occurs when the apical RVAD exceeds 20° during and is at phase 2 [
43]. Kristmundsdottir et al. (1985) found that a convex RVA measurement was as reliable as the RVAD in predicting prognosis, with an RVA under 68° on the initial radiograph typically indicating curve progression [
44].
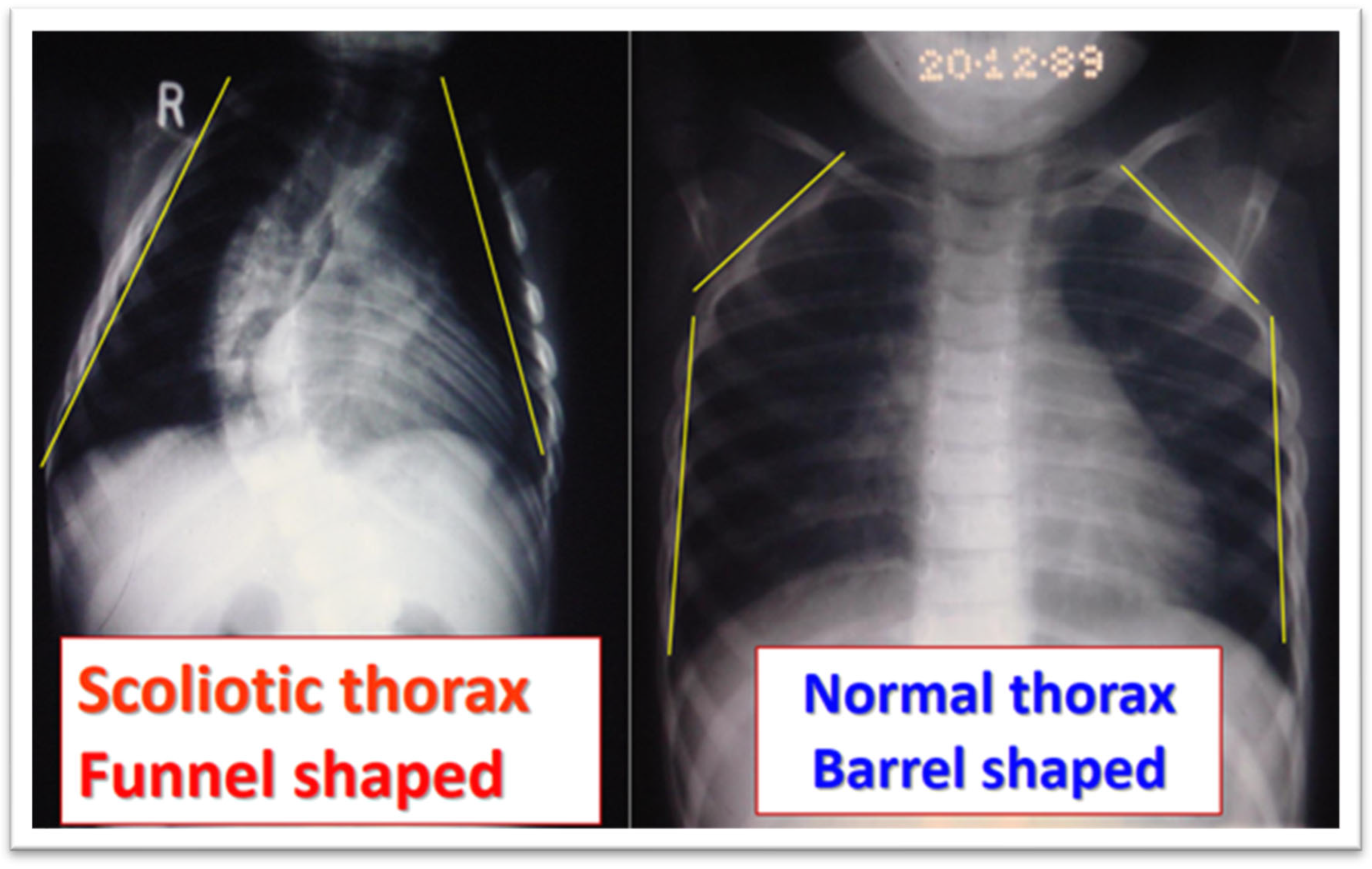
In studies by Grivas et al. (1990, 1991, 1992, 2006), radiological assessments of the spine and rib cage showed that children with progressive IIS had narrower rib cages compared to controls, with a funnel-shaped upper chest,
Figure 6 and
Figure 7. They also found that vertebral rotation at the upper limit of the thoracic curve could predict the progression of IIS, suggesting neuromuscular factors contribute to the condition [
45,
46,
47]. Additionally, in surgically treated IIS cases, preoperative counter-rotation of the T4 vertebra predicted apical vertebral rotation at follow-up, and a decrease in vertebral tilt from T5 to T1 in the upper chest was observed on preoperative PA radiographs. The maximum RVAD of 50° was found at T6, above the apical vertebra [
42,
43,
44,
45,
46,
47].
Perdriolle and Vidal (1985) [
48] stated that Specific Rotation (SR) serves as an indicator of IIS progression. This refers to the total of the two rotational angles observed in the vertebrae adjacent to the upper end-vertebra. IIS is likely to progress if the SR exceeds 5 degrees at the age of 2, 10 degrees at the age of 4, and 20 degrees at the age of 6 [
48],
Figure 8.
4.2. Juvenile Idiopathic Scoliosis—JIS
Juvenile Idiopathic Scoliosis (JIS) emerges between the ages of 4 and 10, accounting for 10–15% of all IS cases. Curvatures measuring 30° or greater in Cobb angle are prone to worsening, with 95% of affected individuals eventually requiring surgical intervention [
52]. If left untreated, these spinal deformities can lead to severe cardiopulmonary complications [
53].
Early detection is crucial, particularly if the scoliosis worsens within the first year of puberty. Predicting the progression of curves measuring between 21 degrees and 30 degrees during the initial two years of puberty remains challenging. However, when juvenile scoliosis surpasses 30 degrees, it tends to accelerate rapidly, with a nearly certain likelihood of requiring surgery once the curvature exceeds 40 to 45 degrees. Key indicators of progression include the curve pattern, the Cobb angle at the onset of puberty, and the rate of curve advancement [
54].
4.3. Predictors for Progression of Adolescent Idiopathic Scoliosis—AIS
The factors typically suggested in clinical practice to predict curve progression and guide appropriate treatment for AIS are: 1. Age at Diagnosis, 2. Sex, 3. Magnitude of the Curve, 4. Growth Potential, 5. Curve Type, 6. Curve Location and Cobb Angle, 7. Menstrual Status (for females),8. Curve Pattern (Single vs. Double Curves), 10. Family History, predictors for progression of AIS patients undergoing Brace treatment [
55,
56].
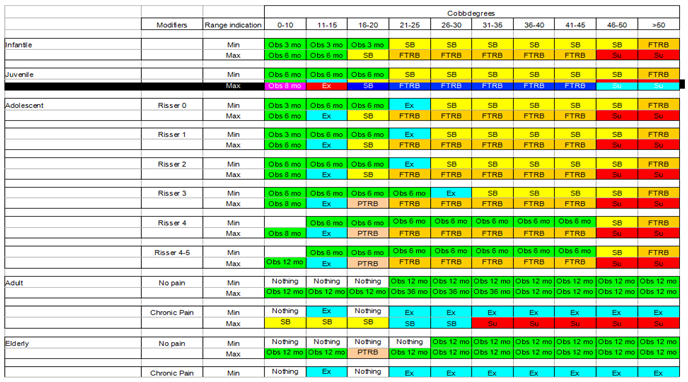
To tailor the treatment of AIS patients undergoing bracing, Society on Scoliosis Orthopaedic and Rehabilitartion Treatment (SOSORT) adapted a modified version of the Lonstein and Carlson (1984) method to assess prognostic risk during the pubertal growth spurt. Additionally, SOSORT provided recommendations on bracing based on the Risser sign for patients with IIS, JIS, AIS, as well as in elders, as outlined in
Figure 9 and
Table 1 [
57].
4.4. Predictors for Progression of Braced Adolescent Idiopathic Scoliosis (AIS)
Cheung et al. (2020) stated that when the flexibility rate exceeds 28%, the chances of preventing curve progression through bracing increase, whereas a lower flexibility rate reduces this probability [
58,
59].
The Supine Correction Index (SCI) is determined by dividing the correction rate by flexibility. Wong et al. (2022) found that a higher supine flexibility (18.1%), an increased correction rate (28.8%), and an SCI above 1.21 were linked to a lower risk of curve progression [
60].
According to Cheung et al. (2019-2020), among AIS patients receiving bracing, those who begin treatment at a younger age and have greater vertebral wedging are more likely to experience curve progression. However, when spinal flexibility surpasses 28%, bracing is more effective in preventing progression; otherwise, the risk increases [
58].
Sitoula et al. (2015) reported that 51% of patients adhered to brace treatment, and half of them still experienced curve progression. Additionally, 34% of patients who showed progression despite bracing were classified within stages SS1 and SS2 [
26,
55].
Khodaei et al. (2025), conducted a study to identify predictors of brace treatment outcomes for adolescents and adults with IS. They found that eleven parameters were associated with bracing outcomes; however, most studies exhibited a moderate risk of bias. Among these parameters, only one—longer treatment duration—was predictive of better long-term SRS-22 total scores, though with limited strength of evidence. Given the generally unclear level of evidence, the study highlighted common weaknesses and emphasized the need for high-quality research to improve predictions of bracing outcomes [
61]. However, a major limitation of this study is that the sole predictive parameter (longer treatment time) was derived from the SRS-22 questionnaire, which was originally developed for surgical treatment of idiopathic scoliosis rather than bracing. As a result, the use of an incorrect treatment questionnaire, despite the existence of questionnaires specifically developed for brace treatment, introduces uncertainty into the findings.
4.5. The Prediction of Curve Progression in Untreated Idiopathic Scoliosis During Growth
The Iowa study, which originated from research on school scoliosis screening in children, is regarded as a foundational study in understanding the progression of AIS and in developing the first predictive model for its progression.
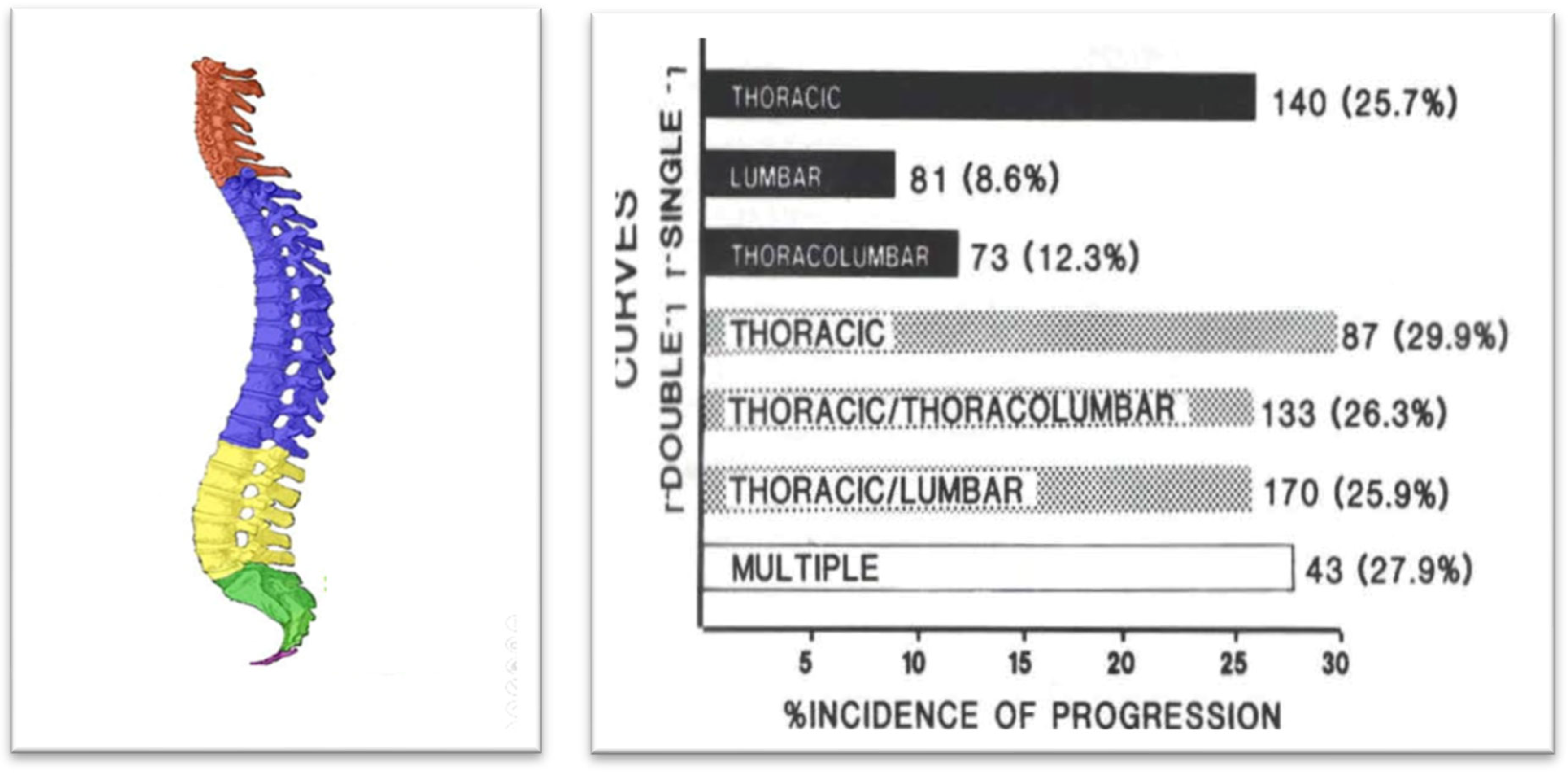
Figure 10 illustrates the incidence of progression for each curve pattern. The numbers to the right of the bars represent the number of patients with each pattern, while the numbers in parentheses indicate the percentage of cases that progressed [
32]. Predictors of AIS curve progression have been found to include curve pattern and magnitude, the patient’s age at presentation, Risser sign, and menarchial status.
Curve progression during growth is very important not only because it may end up in surgical treatmnet but it may also alter the patients self-perception and sports practice of adolescents with IS [
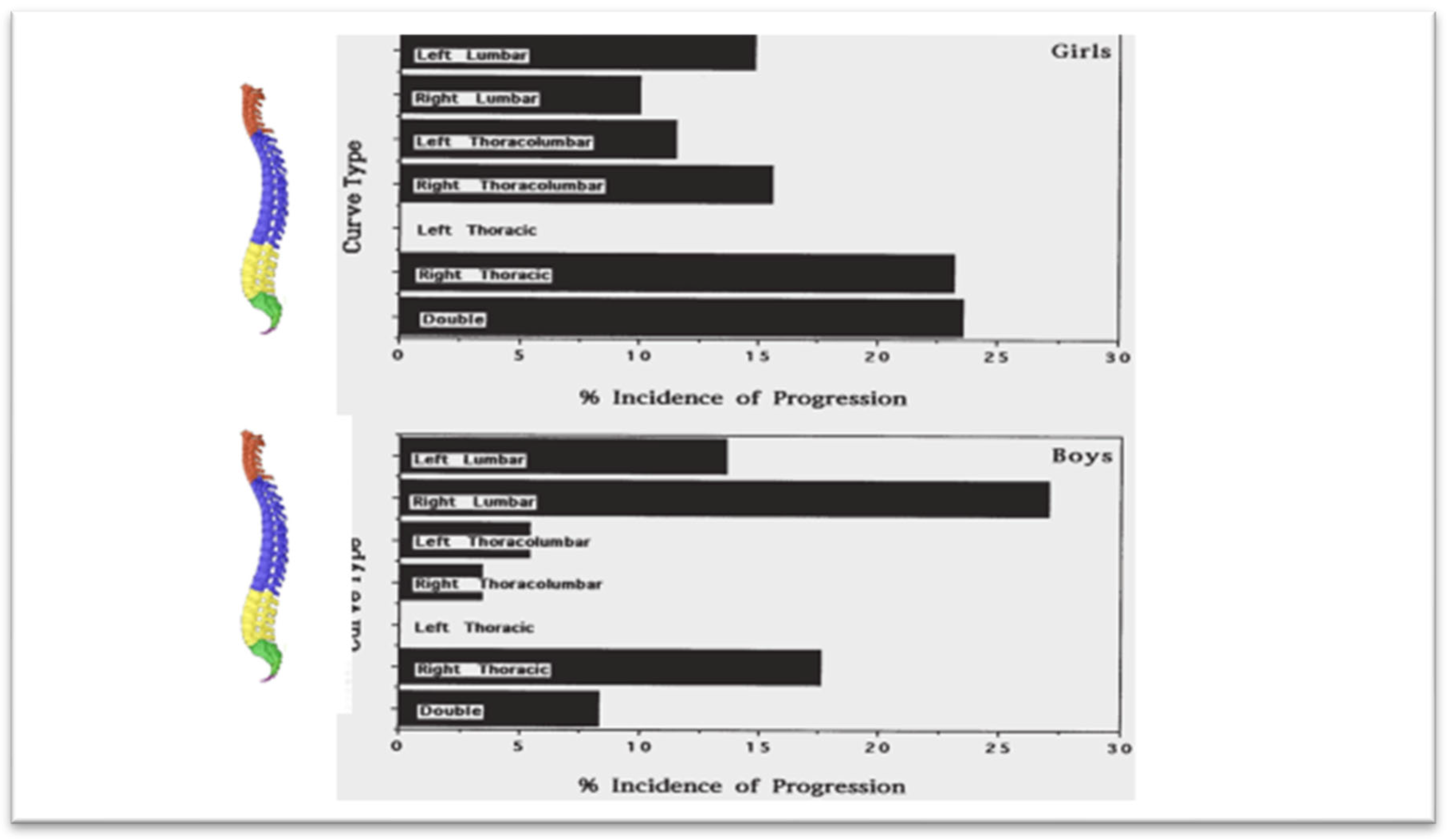
62]. Soucacos et al. (1998), through the implementation of the SSS program, examined 85,622 children. Among 1,436 children re-examined for scoliosis, 14.7% had a Cobb angle greater than 10 degrees. A follow-up at 3.2 years assessed curve progression, identifying strong predictors such as sex, curve pattern, and skeletal maturity, while age and curve magnitude showed a weaker association. The incidence of curve progression, categorized by curve pattern and direction (left vs. right) for both boys and girls, is presented in
Figure 11. Notably, none of the left thoracic curves exhibited progression. The incidence of progression in right thoracic curves among girls was as high as that observed for double curves, while boys with right lumbar curves had a higher progression rate than girls [
63].
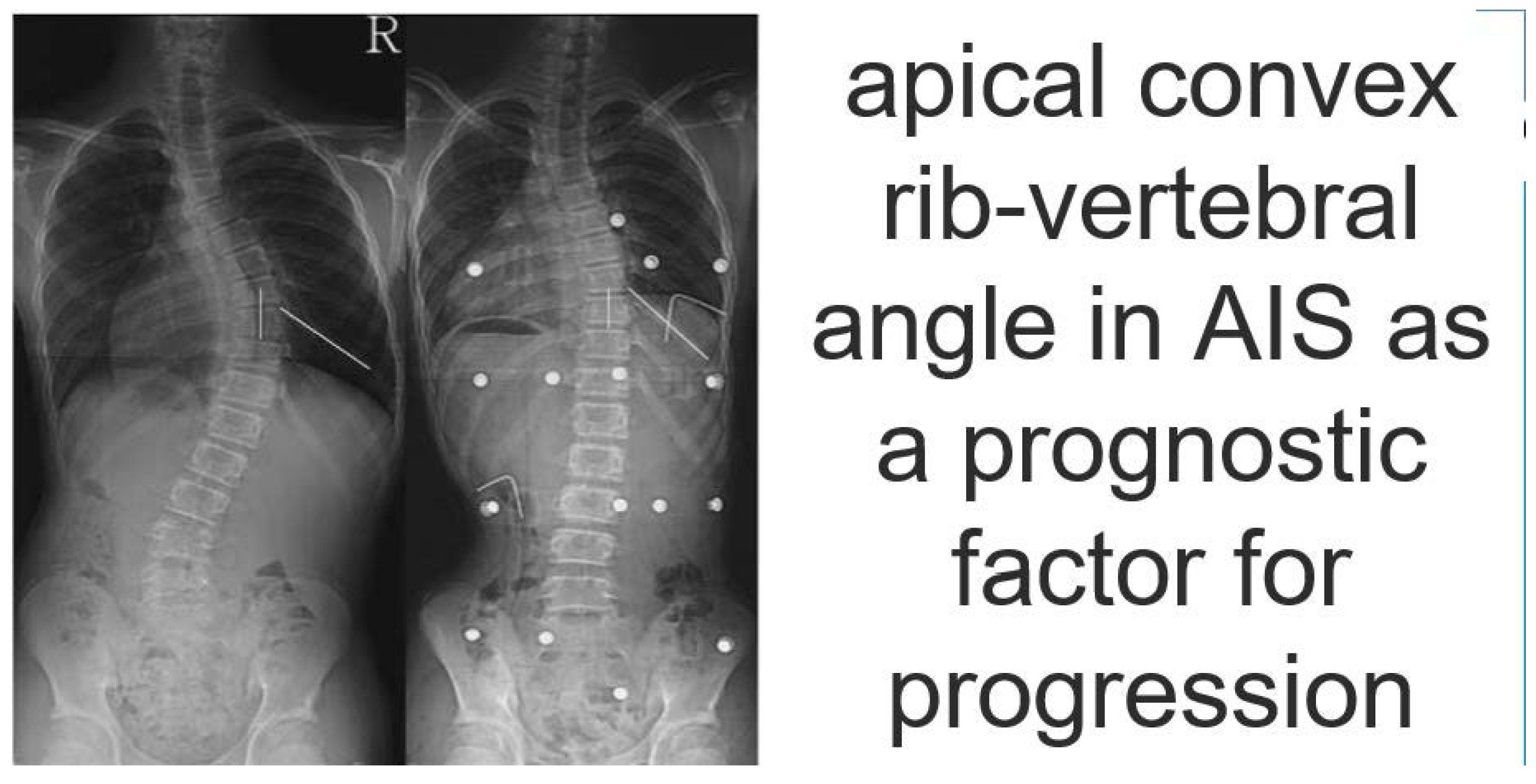
4.6. Apical Convex Rib-Vertebral Angle in AIS as a Prognostic Factor for Progression
Modi et al 2009 recommend measuring the drooping value in the apical RVA on the convex side at regular follow-up to check further progression of the curve and deciding other treatment options. Measurement of the drooping value in convex RVA is equally important as that of initial convex RVA or RVAD in the literature,
Figure 12 [
64].
5. Predictors for Curve Progression at Skeletal Maturity
Examining the predictors of curve progression at skeletal maturity, research indicates that curves reaching 50 degrees are likely to continue progressing into adulthood at an average rate of 1 degree per year, as primarily shown in the Iowa studies [
65].
The progression of thoracolumbar/lumbar curves is also associated with L3 and L4 tilt, particularly when exceeding 16 degrees [
66]. Additionally, a Rib Index threshold of 1.915 at maturity is an indicator of rapid progression [
67]. Surgical treatment should be considered for skeletally mature patients with curves exceeding 50 degrees.
6. Models of Prediction of Progression of IS
In recent years, there has been a growing emphasis on transdisciplinary research that integrates machine learning with clinical data to develop specialized in-house programs for predicting curve progression. However, the use of complex terminology in these studies can make them not only difficult to comprehend but also challenging to assess. Additionally, current predictive models for evaluating the progression of IS curves primarily rely on parameters obtained from 2D radiographic imaging. We believe these models require further time and validation studies to establish their reliability before they can be widely accepted and universally implemented [
13,
68].
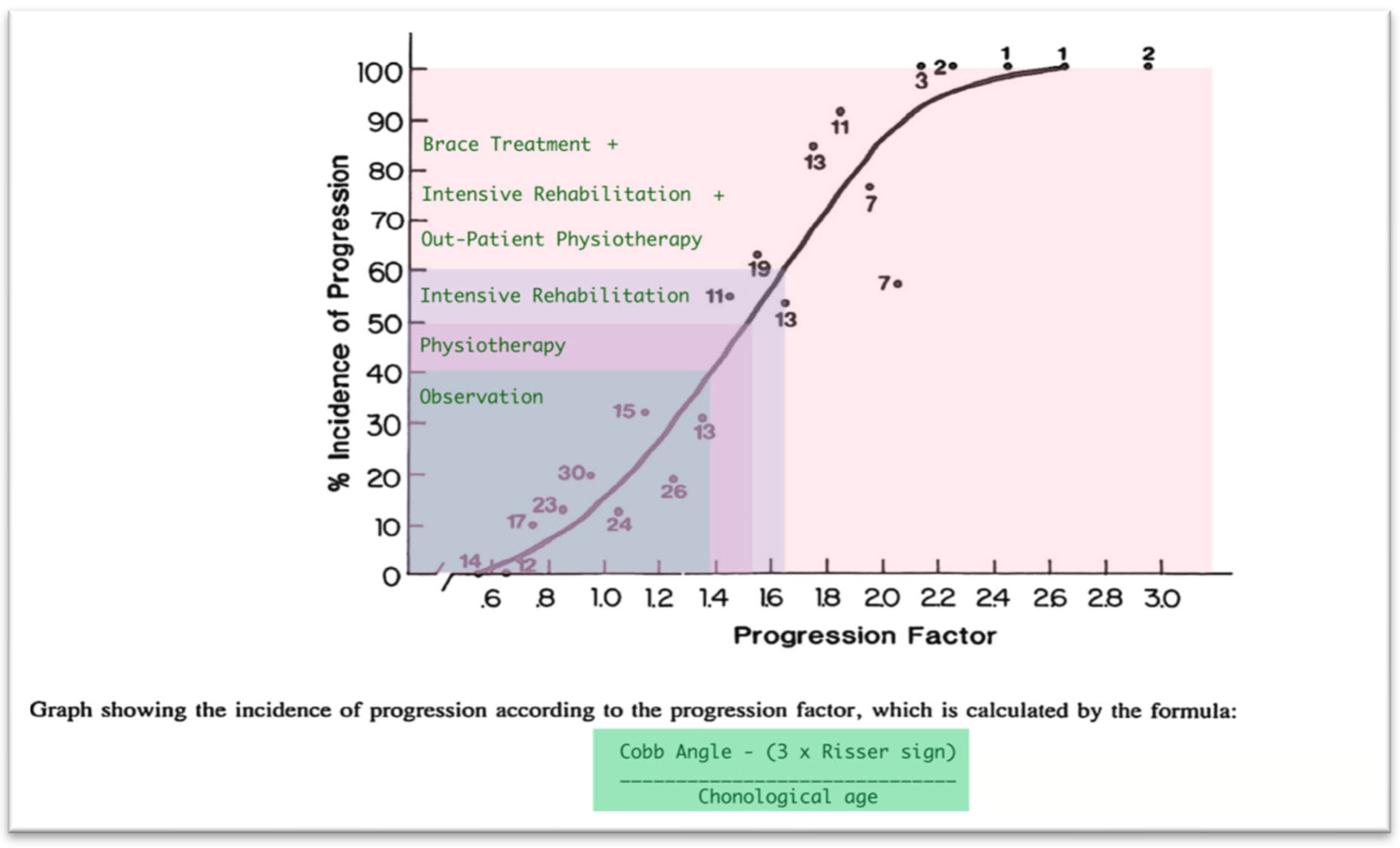
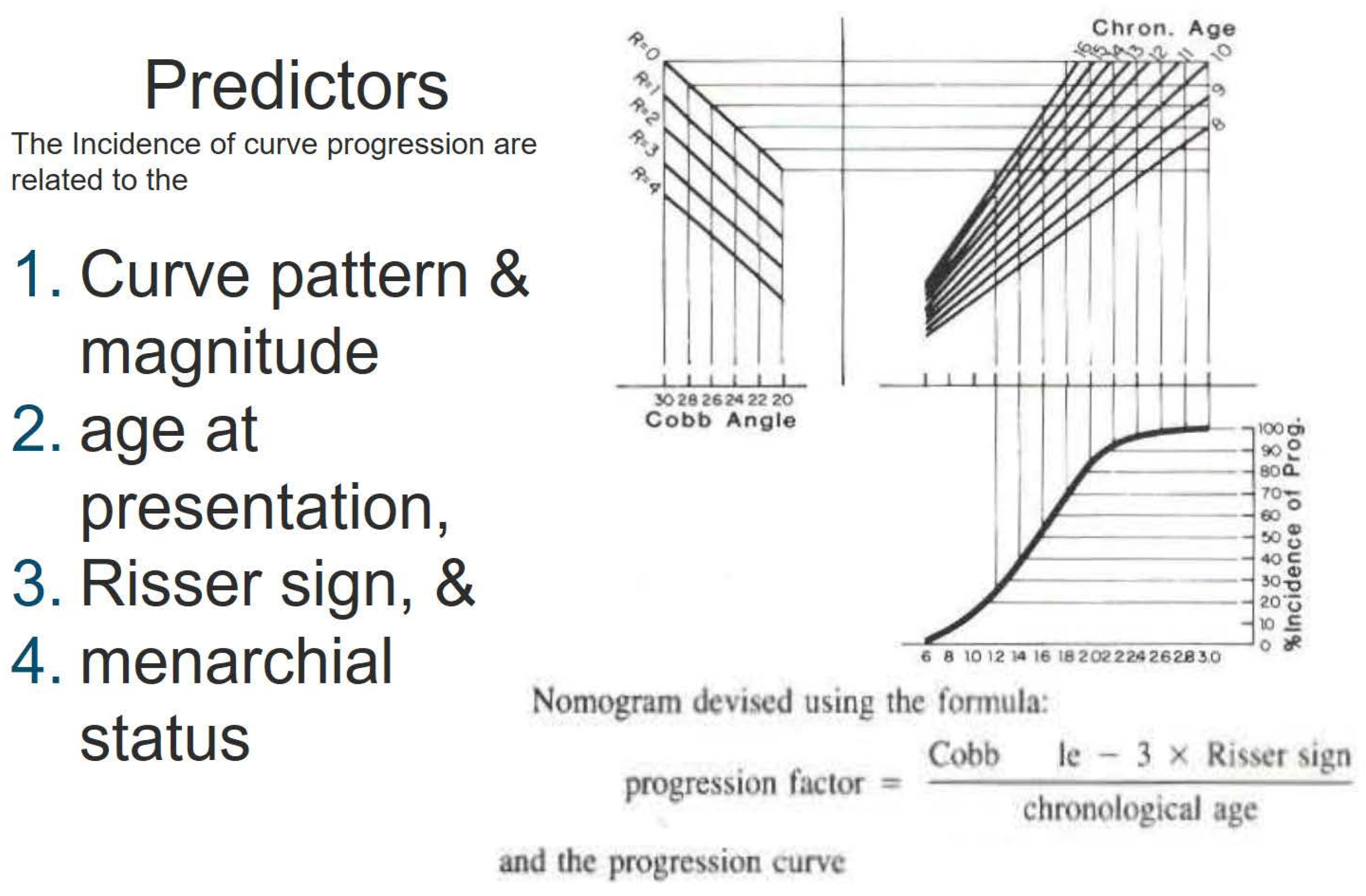
One of the earliest models introduced was likely the Lonstein and Carlson prediction model for assessing the risk of AIS curve progression. This model calculates the risk factor using a specific formula, as illustrated in the
Figure 13, [
32]. The key predictors used in this model to estimate the percentage incidence of curve progression include Cobb angle, patient age, and Risser sign.
Dolan et al. (2019) conducted a study on the development and validation of a prognostic model for untreated adolescent idiopathic scoliosis (AIS) using the simplified skeletal maturity system. Their model incorporated predictors such as Cobb angle, age, sex, curve type, triradiate cartilage status, and skeletal maturity stage. As their final functional model, they recommended using skeletal maturity stage, Cobb angle, and curve type. [
68].
A linear mixed-effects model was applied to 2,317 patients with idiopathic scoliosis (IS) aged 6 to 25 years. The predictors included age, sex, maximum Cobb angle, Risser stage, and curve type. These validated models demonstrated good accuracy in predicting future Cobb angles in untreated IS across the entire growth spectrum [
13].
Wan et al. (2024), reported on a 3D prediction model based on 2D radiological reconstruction. The risk of bias was assessed using the Quality in Prognostic Studies (QUIPS) tool and the Appraisal Tool for Cross-Sectional Studies (AXIS). Additionally, the level of evidence for each predictor was rated using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach. Key predictors included torsion index (TI), apical vertebral rotation (AVR), thoracic hypokyphosis, sagittal wedging, and initial Cobb angle. In mild curves, TI and AVR were identified as predictors of curve progression, with TI > 3.7° and AVR > 5.8° considered significant thresholds [
69].
In recent years, 3D reconstruction of biplanar radiographs has gained validation for its accuracy and reproducibility [
10,
70]. Despite providing extensive quantitative data, commercially available biplanar reconstruction programs still require substantial manual effort to map spinal landmarks before automated measurements can be performed [
71].
Dufvenberg et al. (2024), conducted a prospective cohort study involving 127 patients, aiming to develop a prognostic model for assessing the risk of curve progression in AIS. The study utilized the Cox proportional hazards (CoxPH) regression survival model for model development and validation, comparing its performance with machine learning models using a 66.6/33.3 train/test data split, as well as the patient-reported Spinal Appearance Questionnaire (pSAQ). The models were adjusted for treatment exposure, and 34 candidate prognostic variables were evaluated. The final prognostic model, incorporating Risser stage, Cobb angle, pSAQ, and menarche, demonstrated acceptable discriminative ability in predicting curve progression of more than 6 degrees in Cobb angle. The inclusion of patient-reported pSAQ may have clinical significance in forecasting curve progression. The CoxPH model (Cox, 1972) remains the most widely used multivariate approach for analyzing survival time data in medical research, describing the relationship between event incidence (expressed via the hazard function) and a set of covariates [
72].
Nault et al. (2020), developed a predictive model for AIS progression based on 3D spinal parameters assessed at the initial visit. A general linear model with backward selection was employed, using the final Cobb angle—measured either just before surgery or at skeletal maturity—as the outcome variable. The analysis, conducted on 172 patients, identified significant predictors, including initial skeletal maturation, curve type, frontal Cobb angle, angle of the plane of maximal curvature, and 3D disc wedging (T3-T4, T8-T9) [
11].
Alfraihat et al. (2022), utilized a random forest machine learning (ML) model to predict AIS curve progression. The study incorporated radiographic features previously associated with curve progression, applying Sequential Backward Floating Selection (SBFS) to determine the most predictive subset of features. The key predictors identified were Cobb angle, spinal flexibility, initial lumbar lordosis angle, initial thoracic kyphosis angle, age at last visit, number of levels involved, and Risser "+" stage at the first visit. However, the relative importance and optimal combination of these predictive factors remain uncertain [
73].
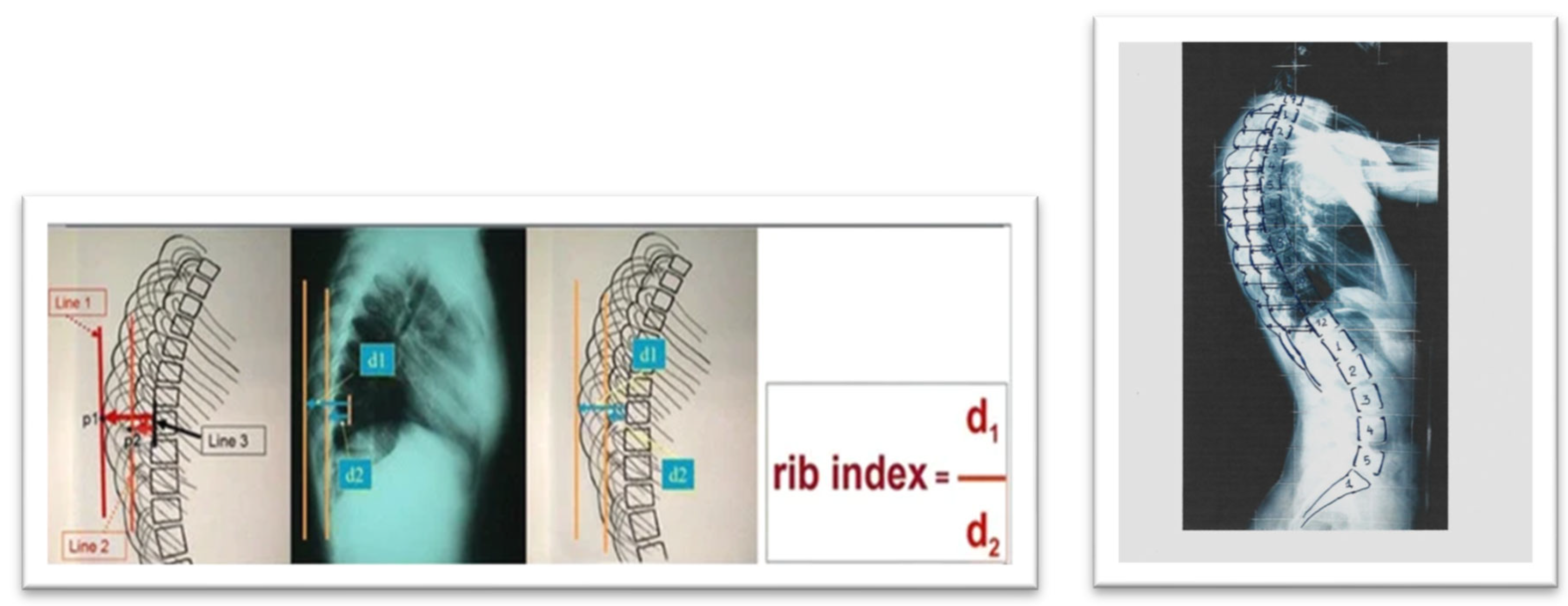
7. Rib Index: A Thoracic Deformity Parameter as Predictor of Progression
The Rib Index (RI) method was first introduced in 1999 [
74] and was later associated with scoliogenesis [
75,
76]. It was developed from the Double Rib Contour Sign (DRCS) to evaluate rib hump deformity (RHD) in individuals with IS, providing a reliable and consistent approach for assessing RHD using lateral radiographs,
Figure 14, [
77,
78].
Clinically, beyond documenting the deformity [
79], the RI method has been utilized for evaluating physiotherapeutic-specific scoliosis exercises (PSSE) [
80], assessing brace treatment [
81,
82], and conducting pre- and post-operative evaluations of thoracic deformity correction across various instrumentation techniques [
78,
83,
84,
85,
86,
87,
88,
89].
Upon reviewing the literature, only one comprehensive review was found that analyzed rib cage deformity parameters in scoliosis and provided a detailed description of them [
90].
However, there is limited information regarding the relationship between these parameters and their impact on spinal deformity. A review of existing studies identified only one publication addressing thoracic deformity parameters used to predict progression in skeletally mature AIS curves measuring 40–50 degrees. Shea et al. (2024) [
67], in their study
"Rib Index Prognoses Accelerated Deterioration in Skeletally Mature AIS Curves of 40–50° Using Uniplanar Radiographic Measures," reported that a Rib Index threshold of 1.915 at maturity was associated with rapid progression.
Further research on segmental rib index (SRI) in IS rib cages [
91] revealed that at any level from T1 to T12, a segmental RI value of 1.45–1.50 or higher primarily indicates a significantly asymmetrical rib cage deformity, suggesting notable asymmetric rib growth at that spinal level. This RI threshold represents an increasing and progressive rib cage deformity [
87]. The term
"pattern of segmental RI asymmetry" refers to the number of rib levels (from T1 to T12) exhibiting this severe asymmetry (≥1.45–1.50) and may serve as a predictor of T and TL curve progression.
Another intriguing implication is that spinal deformity results from rib cage asymmetry, aligning with the late Prof. John Sevastikoglou’s (Sevastik’s) thoracospinal concept [
92].
The perspective that rib deformation is not closely linked to vertebral rotation and that it precedes spinal deformation, particularly in thoracic curves, is primarily supported by the research of Professor J. Sevastik [
93,
94,
95,
96,
97,
98,
99,
100,
101,
102,
103,
104,
105] and other published studies [
106,
107].
Theoretically, if rib cage deformation were solely due to vertebral rotation, then surgically aligning and derotating the vertebral column would fully correct the rib cage deformity postoperatively. However, clinical practice shows this is not the case. Therefore, analyzing published postoperative outcomes of IS scoliosis correction on rib cage deformities can provide an objective answer to this question [
67,
87,
88]. This suggests that rib hump deformity (RHD) is more likely a result of asymmetric rib development rather than vertebral rotation, contrary to common belief [
106].
We recommend using the rib index (RI) and segmental rib index (SRI) as reliable predictors of IS curve progression. This recommendation is based on findings from both preoperative AIS cases and postoperative cases with progression [
67,
87,
88].
Igoumenou et al. (2021), reported preoperative RI values in different surgical constructs: full pedicle screw constructs (group A), hybrid constructs (group B), and Harrington rods (group C). The preoperative mean RI was 2.05 ± 0.23 in group A, 1.93 ± 0.27 in group B, and 2.06 ± 0.25 in group C. Postoperatively, the RI values were 1.37 ± 0.12 (group A), 1.38 ± 0.12 (group B), and 1.61 ± 0.26 (group C). The mean RI correction was 32.7 ± 5.1% for group A, 28.7 ± 5.5% for group B, and 26.8 ± 6.9% for group C [
83,
84]. This statement implies that the post-operative average correction of the RI in this study clearly illustrates that spinal alignment and vertebral derotation achieved through instrumental posterior spinal fusion are not sufficient to fully correct the rib hump or overall trunk rotation, regardless of the surgical technique used.
Consequently, it is suggested that the primary factor contributing to rotational deformity in AIS is the asymmetrical growth of rib pairs. These findings also suggest that the rib cage deformity observed in preoperative IS patients, as measured by the RI and SRI, could serve as a predictor of spinal curve progression. In other words, when an IS patient reaches the stage where surgical intervention is indicated, the RI reflects the degree of rib cage deformity present. Therefore, this level of rib cage deformity could reasonably be considered a predictor for the necessity of surgical treatment.
While comparing the RI and SRI with other methods for predicting scoliosis progression would be insightful, it is not currently scientifically feasible due to the lack of relevant studies. Nonetheless, we acknowledge this absence as a limitation of our study."
8. Critical Opinion
The rationale for proposing the RI and SRI as useful predictors is based on the following consideration: Existing literature on IS includes publications reporting surgical outcomes in patients with widely accepted indications for surgical intervention—that is, patients with advanced IS, [
67,
78,
83,
86,
87,
88,
92]. In these studies, the preoperative RI was compared to the postoperative RI. If IS has reached the stage where surgery is indicated, then the RI, which reflects the thoracic transverse plane deformity, must be reliably abnormal. This suggests that the RI can serve as a valid indicator of deformity progression, as other established indicators.
9. Conclusions
Prediction of curve progression was always a challenge for physicians who treated children with idiopathic scoliosis. Cobb angle and skeletal maturity were traditionally used in decision making, while age of scoliosis diagnosis was a prognostic factor for progression of the curve and determines which treatment is suitable for each individual. The present paper summarizes the current knowledge of factors that are involved in curve progression in idiopathic scoliosis and cites the numerous models that have been developed for prediction of IS progression. It also highlights the importance of the thorax in scoliotic deformity and introduces for the first time two factors that describe the deformity of the rib cage, namely the Rib Index and Segmental Rib Index as predictors of IS progression.
Author Contributions
T.B.G.: conceptualization and writing—original draft preparation; review and editing; EV; review and editing, KS, GK ML review, NS, DL, CM, AM, DP, EP, AK, ET participation in our SSS program, review. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The first author, (TBG), wishes to express gratitude and acknowledge all the colleagues who have participated in our school scoliosis screening program over the years. Their voluntary support has contributed not only to the prevention of IS but also to enhancing the quality of life for children and adolescents in this country. Furthermore, their assistance played a crucial role in collecting the data that served as the foundation for several new concepts discussed in this report. The list of names follows: Papadakis Stamatios, Chandrinos Michael, Vynichakis George, Lykouris Dimitrios, Vasiliadis Elias, Kaspiris Angelos, Deimentes Panagiotis, Skouteli Myrto, Mazioti Christina, Mamzeri Aristea, Papagianni Despoina, Katarachia Eleni, Katopodi Anastasia, Mparka Elissavet, Grozou Anna, Noutsos George, Mouzakis Vasileios, Triantafyllopoulos George, Tsilimidos Gerasimos, Kastrinis Alexandros, Theodosopoulos Evangelos, Katzouraki Galateia, Benekou Christina, Papathanasiou Eleni-Evaggelia, Protopapadakis George, Dimitrakis Nikolaos, Sorolopidou Kalliroi, Fryda Zoi, Armakola Filomeni, Potamiti Eleni, Paspati Ioanna, Skaftourou Eva, Sekouris Nikolaos, Kosti Melpomeni, Gocha Magdalene, Melissaridi Dimitra, Papagiannakopoulou Leto, Lykissas Marios, Papadopoulos Elias.
Conflicts of Interest
TBG, EV, KS, GK ML, NS, DL, CM, AM, DP, EP declare that they have no conflict of interest concerning this article. AΚ,ΕΤ Athens Scoliosis, Moschato, Attica, Greece.
References
- Peterson L-E, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from The Brace Study of the Scoliosis Research Society. The Journal of bone and joint surgery American volume. 1995;77(6):823–7. [CrossRef]
- Grivas TB, Vasiliadis E, Katzouraki G, Lykouris D, Sekouris N, Mazioti C, Mamzeri A, Papagianni D, Mparka E, Kataraxia E. The multiplane initial skeletal remodeling during scoliogenesis. Accepted for publication in Acta Orthopaedica & Traumatologica Hellenica.
- Noshchenko A, Hoffecker L, Lindley EM, Burger EL, Cain CM, Patel VV, Bradford AP (2015) Predictors of spine deformity progression in adolescent idiopathic scoliosis: a systematic review with meta-analysis. World J Orthop 6(7):537–558. [CrossRef]
- Zhang J, Cheuk KY, Xu L, Wang Y, Feng Z, Sit T, Cheng KL, Nepotchatykh E, Lam TP, Liu Z, Hung ALH, Zhu Z, Moreau A, Cheng JCY, Qiu Y, Lee WYW. A validated composite model to predict risk of curve progression in adolescent idiopathic scoliosis. eClinicalMedicine. 2020;18:100236. [CrossRef]
- Dansereau J, Stokes IAF, Moreland MS 1987. Radiographic reconstruction of 3D human rib cage. In Surface Topography and Spinal Deformity Edited by: Stokes IAF, Pekelsky JR, Moreland MS. Stuttgart: Gustav Fischer; 1987:67-76.
- Dansereau J, Stokes IAF: 1988. Measurements of three-dimensional shape of the rib cage. J Biomech 1988.21: 893– 901. [CrossRef]
- Hierholzer E, Hackenberg L. 2002.Three-dimensional shape analysis of the scoliotic spine using MR tomography and rasterstereography. Stud Health Technol Inform. 2002; 91: 184-9. [PubMed]
- Sangole AP, Aubin CE, Labelle H, Stokes IA, Lenke LG, Jackson R, Newton P 2009, Three-dimensional classification of thoracic scoliotic curves. Spine (Phila Pa 1976). 2009 Jan 1;34(1):91-9. [CrossRef] [PubMed]
- Ilharreborde B, Steffen JS, Nectoux E, et al. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine (Phila Pa 1976). 2011;36(20):E1306–13. [CrossRef]
- Donzelli S, Poma S, Balzarini L, Borboni A, Respizzi S, Villafane JH, Zaina F, Negrini S 2015. State of the art of current 3-D scoliosis classifications: a systematic review from a clinical perspective. J Neuroeng Rehabil. 2015 Oct 16;12:91. [CrossRef] [PubMed]
- Nault, M.-L. , Mac-Thiong, J.-M., Roy-Beaudry, M., Turgeon, I., deGuise, J., Labelle, H., & Parent, S. (2014). Three-Dimensional Spinal Morphology Can Differentiate Between Progressive and Nonprogressive Patients with Adolescent Idiopathic Scoliosis at the Initial Presentation. a prospective study. Spine, 39(10), E601–E606. [CrossRef]
- Lonstein J, Carlson J. The prediction of curve progression in untreated idiopathic scoliosis. J Bone Jt Surg. 1984;3(2):1061–71. [CrossRef]
- Parent EC, Donzelli S, Yaskina M, et al. Prediction of future curve angle using prior radiographs in previously untreated idiopathic scoliosis: natural history from age 6 to after the end of growth (SOSORT 2022 award winner). Eur Spine J. 2023;32(6):2171–2184. [CrossRef]
- Vergari C, Gajny L, Courtois I, Ebermeyer E, Abelin-Genevois K, Kim Y, Langlais T, Vialle R, Assi A, Ghanem I, Dubousset J, Skalli W. Quasi-automatic early detection of progressive idiopathic scoliosis from biplanar radiography: a preliminary validation. Eur Spine J. 2019;28(9):1970–1976. [CrossRef] [PubMed]
- Vergari C, Gajny L, Ebermeyer E, Abelin-Genevois K, Kim Y, Courtois I, Langlais T, Vialle R, Assi A, Ghanem I, Dubousset J, Skalli W. Early detection of progressive idiopathic scoliosis through the quasi-automatic 3D reconstruction of the spine from biplanar radiography. Eur Spine J. 2019;28:2878–2879. [CrossRef] [PubMed]
- Lv Z, Lv W, Wang L, Ou J. Development and validation of machine learning-based models for prediction of adolescent idiopathic scoliosis: a retrospective study. Medicine (Baltimore). 2023;102(14):e33441. [CrossRef]
- Meng N, Wong K-Y, Zhao M, Cheung JPY, Zhang T. Radiograph comparable image synthesis for spine alignment analysis using deep learning with prospective clinical validation. E Clinical Medicine. 2023;61: 102050. [CrossRef]
- Zhang T, Zhu C, Zhao Y, et al. Deep learning model to classify and monitor idiopathic scoliosis in adolescents using a single smartphone photograph. JAMA Netw Open. 2023;6(8):e2330617. [CrossRef]
- Bassani T , Cina A, Galbusera F, Cazzato A, Pellegrino ME, Albano D, Sconfienza LM. Feasibility of generating sagittal radiographs from coronal views using GAN-based deep learning framework in adolescent idiopathic scoliosis. European Radiology Experimental (2025)9:11. [CrossRef]
- Cobb J. 1948. Outline for the study of scoliosis. Instr Course Lect. 1948; 5:261 275.7.
- Adams W. Lectures on the Pathology and Treatment of Lateral and Other Forms of Curvature of the Spine” in 1865.
- Duval-Beaupere G, Lamireau TH (1985) Scoliosis at less than 30~ property of the evolutivity (risk of progression). Spine 10:421-424.
- Duval-Beaupère G. Rib hump and supine angle as prognostic factors for mild scoliosis Spine (Phila Pa 1976) 1992 Jan;17(1):103-7. [CrossRef]
- Manzetti M, Ruffilli A, Barile F, Viroli G, Traversari M, Vita F, Cerasoli T, Arceri A, Artioli E, Mazzotti A, Faldini C. Is there a skeletal age index that can predict accurate curve progression in adolescent idiopathic scoliosis? A systematic review 2024 Feb;54(2):299-315. [CrossRef] [PubMed]
- Risser JC (1948): Important Practical Facts in the Treatment of Scoliosis. American Academy of Orthopaedic Surgeons’ Instructional Course Lectures, 5, 248.
- Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF III, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting Scoliosis Progression from Skeletal Maturity: A Simplified Classification During Adolescence, J Bone Join Surg: March 01, 2008 - Volume 90 - Issue 3 - pp 540-553.
- Luk KDK, Saw LB, Grozman S, Cheung KMC, Samartzis D. Assessment of skeletal maturity in scoliosis patients to determine clinical management: a new classification scheme using distal radius and ulna radiographs. Spine J, 2014 Feb 1;14(2):315-25. [CrossRef] [PubMed]
- Yang Li,Saihu Mao,Bo Shi,Zhen Liu,Dun Liu,Xu Sun,Yong Qiu,Zezhang Zhu. Utilization of distal radius and ulna classification scheme in predicting growth peak and curve progression in idiopathic scoliosis girls undergoing bracing treatment, Eur Spine J. 2020 Apr;29(4):770-778. [CrossRef] [PubMed]
- Makino T,Kaito T, Sakai Y, Kashii M, Yoshikawa H Asymmetrical ossification in the epiphyseal ring of patients with adolescent idiopathic scoliosis: a retrospective review Bone Joint J, 2016 May;98-B(5):666-71. [CrossRef] [PubMed]
- Nicholson AD, Sanders JO, Liu RW, Cooperman DR. The relationship of calcaneal apophyseal ossification and Sanders hand scores to the timing of peak height velocity in adolescents. Bone Joint J 2015;97-B:1710–17. [CrossRef]
- Zaoussis AL, and James JIP: The Iliac Apophysis and the Evolution of Curves in Scoliosis. J. Bone and Joint Surg., 40-B(3): 442-453,, 1958.
- Lonstein J E, Carlson J M The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 1984 Sep;66(7):1061-71. [PubMed]
- Li T, Cui JJ, DeVries S, Nicholson AD, Li E, Petit, Kahan JB, Sanders JO, Liu RW, Cooperman DR, Smith BG. Humeral Head Ossification Predicts Peak Height Velocity Timing and Percentage of Growth Remaining in Children J Pediatr Orthop.. 2018 Oct;38(9):e546-e550. [CrossRef] [PubMed] [PubMed Central]
- Blythe CS, Reynolds MS, Gregory LS. Quantifying the ossification and fusion of the calcaneal apophysis using computed tomography. J Anat. 2022 Aug;241(2):484-499. [CrossRef] [PubMed]
- Harrenstein, RJ. Die Skoliose bei Sauglingen und ihre behandlung, Zeitschrift fur Orthopaedische Chirurgie, 52, 1-40.
- Harrenstein, RJ. Das Entstehen von Skoliose infolge einseitiger Zwerchfellähmung , Ztschr. f. orthop. Chir. 56:101, 1932.
- Mehta MH. The natural history of infantile idiopathic scoliosis. In: Scoliosis, Proceedings of a Fifth Symposium held at the Cardiothoracic Institute Brompton Hospital. London, 21-22 September 1976. (Ed.) P.A. Zorab. London: Academic.
- Agadir M, Burwell RG, Grivas TB, Moulton A, Webb JK (1992): Progressive infantile idiopathic scoliosis: a longitudinal radiological study with aetiological implications. In Proceedings of British Scoliosis Society. 17th Annual Meeting at Slieve Donard Hotel. Newcastle, Co. Down, 19-21 March, UK 1992. J Bone Joint Surg 74-B: Supp III, 303.
- Agadir M, Burwell RG, Grivas TB, Moulton A, Webb JK, Wemyss-Holden SA (1991-1992): Progressive infantile idiopathic scoliosis: a longitudinal radiological study with aetiological implications: In Proceedings of British Association of Clinical Anatomists, Winter Scientific Meeting and the Annual General Meeting 1991, Queen Mary and Westfield College, London, England, Wednesday, 18 December 1991. Clin Anat, 1992, 5: 326.
- Agadir M, Burwell RG, Grivas TB, Moulton A, Webb JK (1992): Progressive infantile idiopathic scoliosis: a longitudinal radiological study with aetiological implications. Proceedings of British Scoliosis Society, 17th Annual Meeting at Slieve Donard Hotel. Newcastle, Co. Down, 19-21 March, UK 1992. J Bone Joint Surg, 1992, 74-B: Supp III, 303.
- Burwell RG, Cole AA, Cook TA, Grivas TB, Kiel AW, Moulton A, Thirlwall AS, Upadhyay SS, Webb JK, Wemyss-Holden SA, Whitwell DJ, Wojcik AS, Wythers DJ (1991-1992): Pathogenesis of Idiopathic Scoliosis. The Nottingham Concept. In: Symposium on idiopathic scoliosis. Orthopedica Belgica, Gent, 20-22 March 1991, (ed D. Uyttendaele). Acta Orthop Belgica 1992; 58:33-58.
- Burwell RG, Dangerfield PH. Etiologic theories of idiopathic scoliosis: neurodevelopmental concepts to be evaluated. Stud Health Technol Inform ,2002:91:15-9. [PubMed]
- Mehta, MH. Mehta MH. The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J Bone Joint Surg [Br] 1972;54:230-243.
- Kristmundsdottir F, Burwell RG, James I, The rib-vertebra angles on the convexity and concavity of the spinal curve in infantile idiopathic scoliosis. Clin Orthop Relat Res.1985 Dec:(201):205-9. [CrossRef] [PubMed]
- Grivas TB, Burwell RG, Webb JK. (1991). The funnel-shaped upper chest of progressive infantile idiopathic scoliosis (lIS): significance for rib growth patterns, rib dysplasia and aetiology of the spinal deformity (IIS): Clinical Anatomy 1991, 4(1):73.
- Grivas TB, Burwell GR, Vasiliadis ES, Webb JK. (2006). A segmental radiological study of the spine and rib--cage in children with progressive infantile idiopathic scoliosis. Scoliosis. 2006 Oct 18; 1:17. [CrossRef] [PubMed]
- Grivas TB, Burwell RG, Purdue M, Webb JK, Moulton A (1990-1992): The Rib-Cage deformity in infantile idiopathic scoliosis-the funnel-shaped upper chest in relation to specific rotation as a prognostic factor. An evaluation of thoracic shape in progressive scoliosis and control children during growth. In Proceedings of VIth International Symposium on Surface Topography and Spinal Deformity. Hotel Estoril Eden, 19-20 September, ed. A. Alberti. Lisbon: Faculdade Ciencias Medicas 1990. Surface Topography and Spinal deformity VI, Alberty, Drerup, Hierholzer (ed), Gustav Fischer Verlag, Stuttgart, Jena, New York, 1992, pp. 93-109.
- Perdriolle, R., Vidal, J. Thoracic idiopathic scoliosis curve evolution and prognosis, Spine, 1985, 10, 785-791. [CrossRef]
- Grivas TB, Webb JK, Burwell RG. Arrest of curve progression by epiphysiodesis and rodding for early onset scoliosis. In: Proceedings of British Association of Clinical Anatomists Meeting. London, England, 5th January 1990. Clinical Anatomy 1990; 3:241.
- Grivas TB, Webb JK, Burwell RG. The effects of epiphysiodesis and rodding for early onset scoliosis. In: Proceedings of the 15th Annual Meeting of the British Scoliosis Society. Southampton, UK, 22-24 March 1990. J Bone Joint Surg 1991; 73B(Suppl. I):32-3.
- Grivas TB, Webb JK, Burwell RG. Progressive infantile idiopathic scoliosis: a comparison of three methods and the derotation of a combined procedure. In: Proceedings of the 25th Annual Meeting of the Scoliosis Research Society. Honolulu, Hawaii, USA, 25-27 September. 1990; 73.
- Coillard C, Circo AB, Rivard CH (2010) SpineCor treatment for juvenile idiopathic scoliosis: SOSORT award 2010 winner. Scoliosis 5:25.
- Markus Rafael Konieczny, Hüsseyin Senyurt, Rüdiger Krauspe. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2012 Dec 11;7(1):3–9. [CrossRef]
- Yann Philippe Charles, Jean-Pierre Daures, Vincenzo de Rosa, Alain Diméglio. Progression risk of idiopathic juvenile scoliosis during pubertal growth Spine (Phila Pa 1976) 2006 Aug 1;31(17):1933-42. [CrossRef]
- Sitoula P, Verma K, Holmes L Jr, Gabos PG, Sanders JO, Yorgova P, Neiss G, Rogers K, Shah SA Prediction of Curve Progression in Idiopathic Scoliosis: Validation of the Sanders Skeletal Maturity Staging System.. Spine (Phila Pa 1976). 2015 Jul 1;40(13):1006-13. [CrossRef] [PubMed]
- Tan KJ, Moe MM, Vaithinathan R, Wong HK. Curve progression in idiopathic scoliosis: follow-up study to skeletal maturity. Spine (Phila Pa 1976). 2009 Apr 1;34(7):697-700. [CrossRef] [PubMed]
- Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, Diers H, Grivas TB, Knott P, Kotwicki T, Lebel A, Marti C, Maruyama T, O’Brien J, Price N, Parent E, Rigo M, Romano M, Stikeleather L, Wynne J, Zaina F. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018 Jan 10;13:3. [CrossRef] [PubMed]
- Cheung JPY, Cheung PWH, Yeng WC, Chan LCK. Does Curve Regression Occur During Underarm Bracing in Patients with Adolescent Idiopathic Scoliosis? Clin Orthop Relat Res. 2020;478(2):334–45. https:// doi. org/ 10. 1097/ CORR. 00000 00000 000989.
- Cheung and Cheung Cheung JPY, Cheung PWH. Supine flexibility predicts curve progression for patients with adolescent idiopathic scoliosis undergoing underarm bracing Bone Joint J. Bone Joint J. 2020 Feb;102-B(2):254-260. [CrossRef]
- Wong LPK, Cheung PWH, Cheung JPY. Supine correction index as a predictor for brace outcome in adolescent idiopathic scoliosis. Bone Joint J. 2022;104-B(4):495–503. [CrossRef]
- Khodaei M, Parent EC, Wong J, Chan A, Coutts B, Dlikan M, Fehr B, Logithasan V, Sayed T, Mendoza A, Ganzert C, Lou EHM. Identifying predictors of brace treatment outcomes for adolescents or adults with idiopathic scoliosis: a systematic review. Eur Spine J. 2025 Feb 26. [CrossRef] [PubMed]
- Notarnicola A, Farì G, Maccagnano G, Riondino A, Covelli I, Bianchi FP, Tafuri S, Piazzolla A, Moretti B. Teenagers’ perceptions of their scoliotic curves. An observational study of comparison between sports people and non- sports people. Muscles Ligaments Tendons J. 2019;9(2):225-35.
- Soucacos PN, Zacharis K, Gelalis J, Soultanis K, Kalos N, Beris A, Xenakis T, Johnson EO. Assessment of curve progression in idiopathic scoliosis. Eur Spine J. 1998;7(4):270-7. [CrossRef] [PubMed]
- Modi HN, Suh SW, Song HR, Yang JH, Ting C, Hazra S. Drooping of apical convex rib-vertebral angle in adolescent idiopathic scoliosis of more than 40 degrees: a prognostic factor for progression. J Spinal Disord Tech. 2009 Jul;22(5):367-71. [CrossRef] [PubMed]
- Agabegi SS, Kazemi N, Sturm PF, Mehlman CT. Natural History of Adolescent Idiopathic Scoliosis in Skeletally Mature Patients: A Critical Review.. J Am Acad Orthop Surg. 2015 Dec;23(12):714-23. [CrossRef] [PubMed]
- Ohashi M, Watanabe K, Hirano T, Hasegawa K, Katsumi K, Shoji H, Mizouchi T, Endo N. Predicting Factors at Skeletal Maturity for Curve Progression and Low Back Pain in Adult Patients Treated Nonoperatively for Adolescent Idiopathic Scoliosis With Thoracolumbar/Lumbar Curves: A Mean 25-year Follow-up. Spine (Phila Pa 1976). 2018 Dec 1;43(23):E1403-E1411. [CrossRef] [PubMed]
- Shea G K-H, Ng S Y-L, Zhang C, Wang G. Prognosticating accelerated deterioration in skeletally mature adolescent idiopathic scoliosis curves of 40–50° using uniplanar radiographic measures of axial rotation. Spine Deformity (2024) 12:1729–1734. [CrossRef]
- Dolan LA, Weinstein SL, Abel MF, Bosch PP, Dobbs MB, Farber TO, Halsey MF, Hresko MT, Krengel WF, Mehlman CT, Sanders JO, Schwend RM, Shah SA, Verma K (2019) Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST):. Spine Deform 7(6):890-898.e4. [CrossRef]
- Hiu-Tung S Wan, Darren L L Wong, Ching-Hang S To, Nan Meng, Teng Zhang, Jason P Y Cheung. 3D prediction of curve progression in adolescent idiopathic scoliosis based on biplanar radiological reconstruction. Bone Jt Open. 2024 Mar 25;5(3):243-251. [CrossRef] [PubMed] [PubMed Central]
- Ferrero E, Lafage R, Vira S, et al. Three-dimensional reconstruction using stereoradiography for evaluating adult spinal deformity: a reproducibility study. Eur Spine J. 2017;26(8):2112–2120. [CrossRef]
- Garg B, Mehta N, Bansal T, Malhotra R. EOS imaging: concept and current applications in spinal disorders. J Clin Orthop Trauma. 2020;11(5): 786–793. [CrossRef]
- Dufvenberg M, Charalampidis A, Diarbakerli E, Öberg B, Tropp H, Aspberg Ahl A, Wezenberg D, Hedevik H, Möller H, Gerdhem P, Abbott A; CONTRAIS Study Group. Acta Orthop. 2024 Sep 13:95:536-544. [CrossRef] [PubMed]
- Alfraihat A, Samdani AF, Balasubramanian S Predicting curve progression for adolescent idiopathic scoliosis using random forest model. 2022, PLoS ONE 17(8): e0273002. https://doi. org/10.1371/journal.pone.0273002.
- Grivas TB, Dagas S, Lafogianni S, Samelis P, Polyzois D: The double rib contour sign (DRCS) of the hemithoracic ribs in the lateral vertebral radiographs. Is there a causal relationship with scoliosis? 25th Anniversary Symposium on Spine Diseases of "N. Giannestras, P. Smyrnis" meeting. Patras: Hotel Porto Rio; 1999.
- Grivas TB, Daggas S, Polyzois B, Samelis P: The Double Rib Contour Sign (DRCS) in lateral spinal radiographs: aetiologic implications for scoliosis. Clermont, France: In Proceeding of International Research Society of Spinal Deformities meeting; 2000. 23-26 May 2000, Proceedings: page 9.IRSSD 2000.
- Grivas TB, Dangas S, Polyzois BD, Samelis P. The Double Rib Contour Sign (DRCS) in lateral spinal radiographs: aetiologic implications for scoliosis. Stud Health Technol Inform. 2002;88:38-43. [PubMed]
- Grivas, TB. Rib index. Scoliosis 9, 20 (2014). [CrossRef]
- Lykissas MG, Sharma V, Jain VV, Crawford AH. Assessment of Rib Hump Deformity Correction in Adolescent Idiopathic Scoliosis with or Without Costoplasty Using the Double Rib Contour Sign. J Spinal Disord Tech 2015;28:134–139. [CrossRef]
- Grivas TB, Jevtic N, Ljubojevic D, Pjanic S, Golic F, Mazioti C, Papagianni D, Mamzari A, Vasiliadis E Rib index is a strong surrogate of scoliometric reading in idiopathic scoliosis. Eur Spine J. 2024 Jun;33(6):2451-2456. [CrossRef] [PubMed]
- Lebel A and Lebel V: Rib index, an objective measure to document changes of the rib hump deformity in a Risser 4 progressive AIS patient treated with the Schroth method. 11th International Conference on Conservative Management of Spinal Deformities, 9th SOSORT Annual Meeting, 8-10 May 2014, Wiesbaden, Germany. Proceedings: page 40. Lebel, A., Lebel, V. Rib index, an objective measure to document changes of the rib hump deformity in a risser 4 progressive AIS patient treated with the Schroth method. Scoliosis 9 (Suppl 1), O18 (2014). [CrossRef]
- Grivas TB: Chapter: Radiological appraisal of thoracic deformity - improvement or deterioration using the convex/concave rib-hump index (‘double rib contour sign’) in curves Lenke Type 1, 3, 5 and 6. In Scoliosis Research Society • Half-Day Courses. Scoliosis Research Society, Editors: SRS 2012-2013 Education Committee; 29–30.
- Grivas TB, Triantafyllopoulos G, Mazioti C. Assessment of early RH deformity correction in adolescent idiopathic scoliosis treated with a dynamic derotation brace using the double rib contour sign. Scoliosis. 2013;8(Suppl 2):O54. [CrossRef]
- Stavropoulos NA, Soultanis KC, Grivas TΒ, Starantzis KA, Tsiavos K, Sarlikiotis T, Mimidis G, Papagelopoulos PJ: Measurement of rib hump deformity correction in adolescent idiopathic scoliosis treated with full screw or hybrid constructs using the double rib contour sign. 7o Panhellenic Spinal Meeting, 31.10 - 2.11 2013. Makedonia Palace, Thessaloniki, Greece.
- Hwang, S.W.; Samdani, A.F.; Marks, M; Bastrom, T.; Garg, H.; Lonner, B.; Bennett, J.T.; Pahys, J.; Shah, S.; Miyanji, F.; et al. Five-year clinical and radiographic outcomes using pedicle screw only constructs in the treatment of adolescent idiopathic scoliosis. Eur. Spine J. 2013, 22, 1292-1299. [CrossRef]
- Haber LL, Hughes JD, Womack ED, Roberson RM, Wrigh PB. Screw versus hybrid constructs for flexible thoracic curves in adolescent idiopathic scoliosis: a prospective, randomized study. Spine Deform. 2014;2(5):367–373. [CrossRef]
- Stavropoulos NA, Soultanis KC, Grivas TB, Tsiavos K, Starantzis K, Sarlikiotis T, Karamanis E, Papagelopoulos PJ. Measurement of RH deformity correction in adolescent idiopathic scoliosis treated with full screw or hybrid constructs using the double rib contour sign. London, United Kingdom: 15th EFORT Congress; 2014.
- Igoumenou, V.G.; Megaloikonomos, P.D.; Tsiavos, K; Georgopoulos, G.; Liontos, M.; Mavrogenis, A.F.; Grivas, T.B.; Soultanis, K; Papagelopoulos, P.J. Postoperative rib hump deformity correction in patients with adolescent idiopathic scoliosis. Comparison of a three generations spinal fusion systems. In Proceedings of the Combined Meeting of the International Research Society of Spinal Deformities and the Society on Scoliosis Orthopaedic and Rehabilitation Treatment, Banff, AB, Canada, 25-28 May 2016.
- Igoumenou, V.G.; Melamud, E.; Vazifehdan, F.; Megaloikonomos, P.D.; Grivas, T.B.; Mavrogenis, A.F.; Papagelopoulos, P.J.; Soultanis, K. Rib Hump Deformity Correction in Patients with Adolescent Idiopathic Scoliosis: A Comparison of Three Spinal Fusion Systems. J. Long Term Eff. Med. Implant. 2021, 31, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Easwar, T.R.; Hong, J.-Y.; Yang, J.H.; Suh, S. W.; Modi, HN. Does lateral vertebral translation correspond to Cobb angle and relate in the same way to axial vertebral rotation and rib hump index? A radiographic analysis on idiopathic scoliosis. Eur. Spine J. 2011, 20, 1095–1105. [Google Scholar] [CrossRef] [PubMed]
- Harris JA, Mayer OH, Shah SA, Campbell RM Jr, Balasubramanian S. A comprehensive review of thoracic deformity parameters in scoliosis. Eur Spine J. 2014 Dec;23(12):2594-602. [CrossRef] [PubMed]
- Grivas TB, Jevtic N, Ljubojevic D, Pjanic S, Golic F, Vasiliadis E. Segmental Rib Index and Spinal Deformity: Scoliogenic Implications. Healthcare (Basel). 2023 Nov 20;11(22):3004. [CrossRef] [PubMed]
- Soultanis, K.C.; Stavropoulos, N.A.; Grivas, T.B.; Tsiavos, K.; Starantzis, K.; Papagelopoulos, P.J. Rib hump deformity assessment using the rib index in adolescent idiopathic scoliotics treated with full screw or hybrid constructs: Aetiological implications. Scoliosis 2015, 10 (Suppl. S2), S10. [Google Scholar] [CrossRef] [PubMed]
- Sevastik, J.A.; Aaro, S.; Normelli, H. Scoliosis: Experimental and clinical studies. Clin. Orthop. Relat. Res. 1984, 191, 27–34. [Google Scholar] [CrossRef]
- Normelli, H.; Sevastik, J.; Wallberg, H. The thermal emission from the skin and the vascularity of the breasts in normal and scoliotic girls. Spine 1986, 11, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Sevastik, J.A.; Aaro, S.; Lindholm, S.T.; Dalhborn, M. Experimental scoliosis in growing rabbits by operations on the rib cage. Clin. Orthop. Relat. Res. 1987, 136, 282–286. [Google Scholar]
- Agadir, M.; Sevastik, B.; Sevastik, J.A.; Persson, A.; Isberg, B. Induction of scoliosis in the growing rabbit by unilateral rib-growth stimulation. Spine 1988, 13, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Normelli, H.; Sevastik, J.A.; Ljung, G.; Jönsson-Söderström, A.M. The symmetry of the breasts in normal and scoliotic girls. Spine 1986, 11, 749–752. [Google Scholar] [CrossRef]
- Sevastik, J.; Agadir, M.; Sevastik, B. Effects of rib elongation on the spine: I. Distortion of the vertebral alignment in the rabbit. Spine 1990, 15, 822–825. [Google Scholar]
- Sevastik, J.; Agadir, M.; Sevastik, B. Effects of rib elongation on the spine: II. Correction of scoliosis in the rabbit. Spine 1990, 15, 826–829. [Google Scholar]
- Agadir, M.; Sevastik, B.; Reinholt, F.P.; Perbeck, L.; Sevastik, J. Vascular Changes in the Chest Wall After Unilateral Resection of the Intercostal Nerves in the Growing Rabbit. J. Orthop. Res. 1990, 8, 283–290. [Google Scholar] [CrossRef]
- Sevastik, B.; Xiong, B.; Lundberg, A.; Sevastik, J.A. In vitro opto-electronic analysis of 3-D segmental vertebral movements during gradual rib lengthening in the pig. Acta Orthop. Belg. 1995, 61, 218–225. [Google Scholar] [PubMed]
- Gréalou, L.; Aubin, C.E.; Sevastik, J.A.; Labelle, H. Simulations of rib cage surgery for the management of scoliotic deformities. Stud. Health Technol. Inform. 2002, 88, 345–349. [Google Scholar] [PubMed]
- Sevastik, J.A. Dysfunction of the autonomic nerve system (ANS) in the aetiopathogenesis of adolescent idiopathic scoliosis. Stud. Health Technol. Inform. 2002, 88, 20–23. [Google Scholar] [PubMed]
- Sevastik, J.A.; Burwell, R.G.; Dangerfild, P.H. A new concept for the etiopathogenesis of the thoracospinal deformity of idiopathic scoliosis: Summary of an electronic focus group debate of the IBSE. Eur. Spine J. 2003, 12, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Sevastik, J.A. Right convex thoracic female adolescent scoliosis in the light of the thoracospinal concept. Stud. Health Technol. Inform. 2006, 123, 552–558. [Google Scholar] [PubMed]
- Grivas, T.B.; Vasiliadis, E.S.; Mihas, C.; Savvidou, O. The effect of growth on the correlation between the spinal and rib cage deformity: Implications on idiopathic scoliosis pathogenesis. Scoliosis 2007, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Doi T, Matsumoto Y, Tono O, Tarukado K, Harimaya K, Okada S, Kubota K, Hayashida M, Iwamoto Y A shallow chest correlates with the aortic position in the normal spine: features resembling those observed in structural scoliosis. . Scoliosis. 2014 Aug 30;9:14. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).