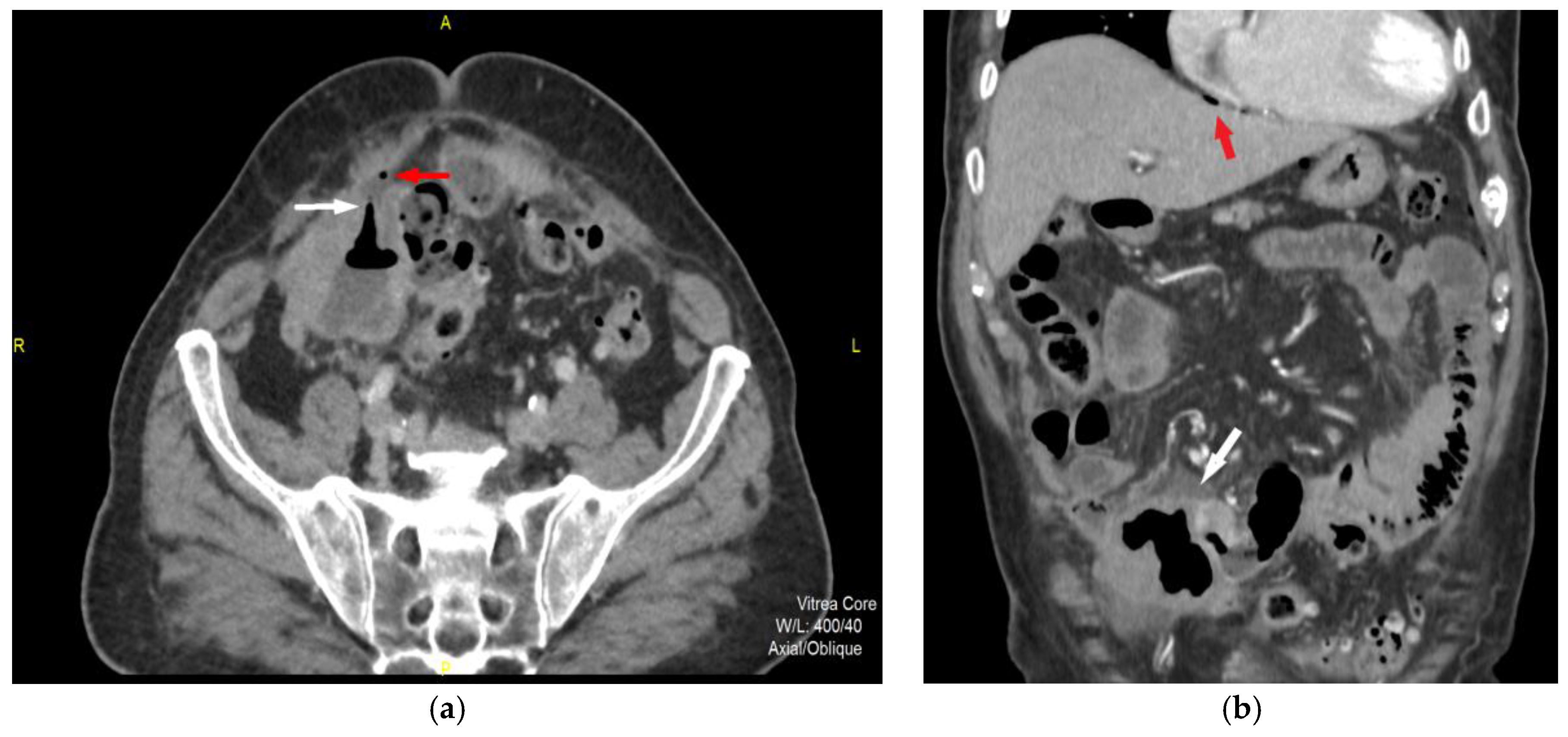
A 86-year-old male patient was admitted to the hospital presenting with severe, diffuse, stabbing abdominal pain that started several hours prior to admition. His medical history includes previous appendectomy and cholecystectomy for inflammatory benign diseases. The physical examination demonstrated a tender abdomen with rebound tenderness and rigidity, predominantly in the lower abdominal region. This was accompanied by high fever (up to 39°C) and a pulse rate of 103 bpm. The laboratory tests showed elevated inflammatory markers, including a total WBC count of 13.2 × 10^9/L with neutrophil predominance, an elevated CRP level of 167.1 mg/L, and a procalcitonin level of 2.170 ng/L, indicating a high risk of systemic infection. Abdominal ultrasound showed a large, heteroechoic, irregular formation in the right iliac region, closely associated with surrounding intestinal structures and laminar free fluid. Subsequently, the patient was referred to multidetector computerized tomography (MDCT) scan (
Figure 1).
Anteriorly, a gas-filled tubular tract (white arrow) is presented, which probably corresponds to the ileal wall rupture site with free gas extraluminally (red arrow). Coronal reconstruction (b) demonstrates wall irregularity with extensive reaction of the surrounding adipose tissue (white arrow) complicated by perforation due to direct sign of a pneumoperitoneum -free gas particle subphrenic (red arrow).
MDCT features of GIST are primarily a clear outer contour of the tumor, submucosal presentation and relative tissue homogeneity in smaller tumors. With the increase in diameter, the structure of the tumor stroma degrades towards cystic and necrotic, which damages the intestinal or stomach mucosa itself and can lead to bleeding. Moreover, the risk of tumor rupture is increased, that leads to a worse prognosis of the disease and the spread of malignancy (1). The main prognostic factors for disease recurrence based on several classification systems are the following: tumor diameter, mitotic index, tumor localization and disease stage (1–4). The modified National Institutes of Health consensus criteria adds tumor rupture as a new factor that classifies the tumor as high risk GIST (4). Detection of the tumor rupture is of great importance for planning surgical intervention and mainly for further oncological treatment (1).
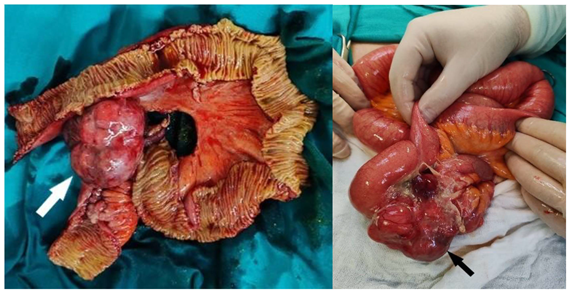
Intraoperative findings showed tumor-like alteration of the terminal ileum, involving several loops of the small intestine (Figure 2). A resection of approximately 60 cm of the small intestine, including the corresponding mesentery, was performed, followed by stapled entero-enteric anastomosis. The postoperative course was uneventful.
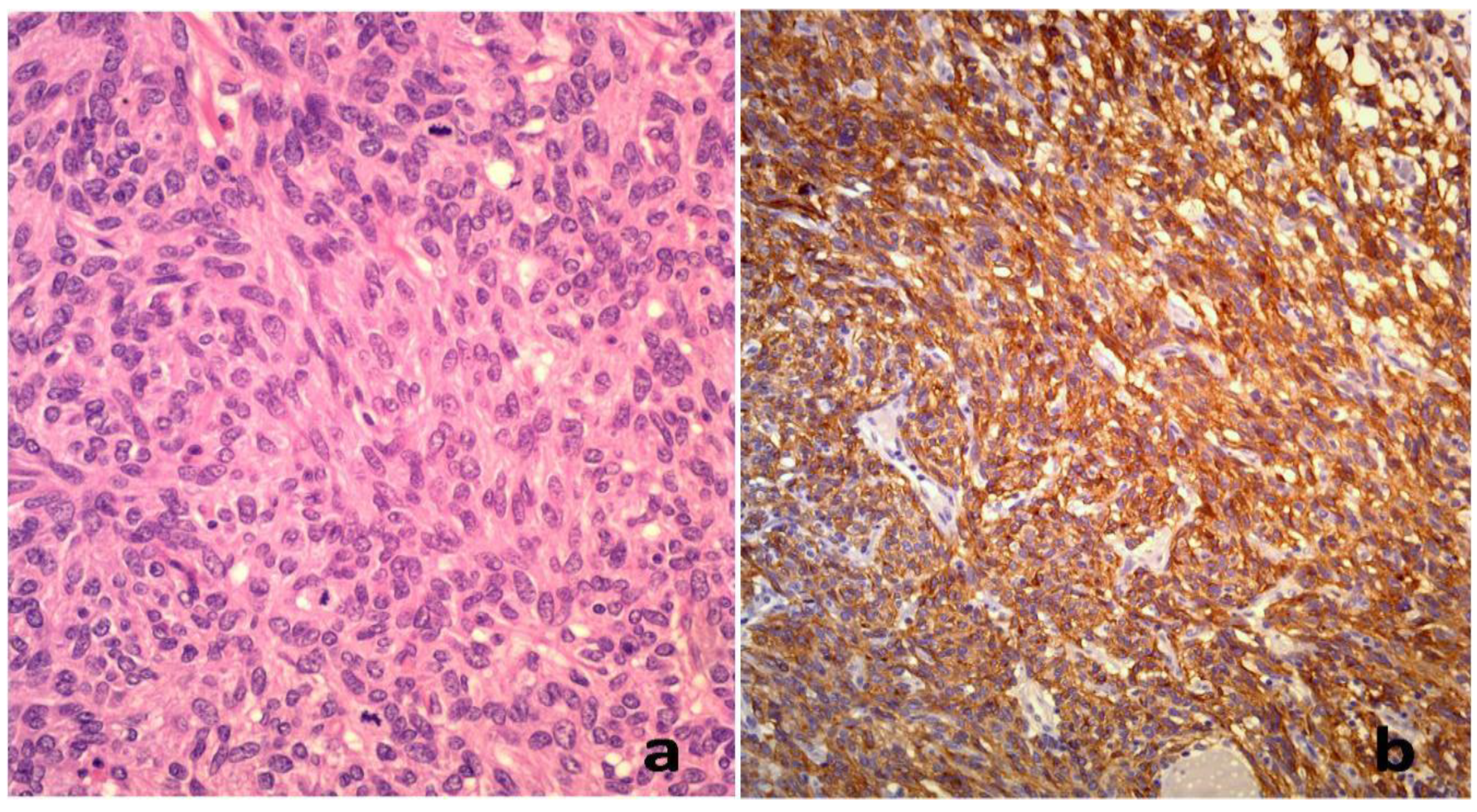
Pathohistological examination confirmed the diagnosis of terminal ileum gastrointestinal stromal tumor (GIST). These findings correspond to the atypical immunophenotype noted in this rare case (
Figure 3).
The available publications confirm the correlation between morphological MDCT features of GIST with high metastatic risk of these tumors (5,6). Tumor diameter, the presence of interrupted mucosa, tumor localization, degraded tissue structure, irregular margins and tumor shape as well as enlarged peritumoral vascular structures that feed and drain the tumor are significant predictive MDCT factors of high-risk GIST(7). Tumor rupture is an important factor that is considered to contribute to an increased risk of recurrence and a dismal prognosis of the disease. (8,9) It is certainly a condition that requires urgent surgical intervention because it leads to acute abdominal symptoms, the risk of bleeding and extensive peritonitis and sepsis. (10) The type of the tumor as well as the signs of tumor perforation were recognized by timely MDCT diagnosis, and further facilitated surgical and oncological treatment of the patient. (11)
Author Contributions
Conceptualization, Marko Zivanovic, Jovan Peric, Katarina Stosic; methodology, Nemanja Bidzic, Milan Zuvela; resources, Danijela Sekulic, Teodor Vasic; writing—original draft preparation, Marko Zivanovic, Milica Mitrovic, Katarina Stosic; writing—review and editing, Danijel Galun, Dragan Vasin, Milica Mitrovic; supervision, Danijel Galun. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of University Clinic for Digestive Surgery, University Clinical center of Serbia (256/25, February 14th, 2025).
Informed Consent Statement
The patient was consented for publication of the case report.
Data Availability Statement
The datasets used and analyzed in this paper are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Misawa, S.; Takeda, M.; Sakamoto, H.; Kirii, Y.; Ota, H.; Takagi, H. Spontaneous rupture of a giant gastrointestinal stromal tumor of the jejunum: a case report and literature review. World J Surg Oncol. 2014, 21, 153. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Keung, E.Z.; Raut, C.P. Management of Gastrointestinal Stromal Tumors. Surg Clin North Am. 2017, 97, 437–452. [Google Scholar] [CrossRef] [PubMed]
- Blay, J.Y.; Kang, Y.K.; Nishida, T.; von Mehren, M. Gastrointestinal stromal tumours. Nat Rev Dis Primers. 2021, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Joensuu, H.; Vehtari, A.; Riihimäki, J.; Nishida, T.; Steigen, S.E.; Brabec, P.; Bordoni, A.; Magnusson, M.K.; Linke, Z.; Sufliarsky, J.; et al. Risk of recurrence of gastrointestinal stromal tumour after surgery: An analysis of pooled population-based cohorts. Lancet Oncol. 2012, 13, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Judson, I.; Jones, R.L.; Wong, N.A.C.S.; Dileo, P.; Bulusu, R.; Smith, M.; Almond, M. Gastrointestinal stromal tumour (GIST): British Sarcoma Group clinical practice guidelines. Br J Cancer. 2025, 132, 1–10. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Judson, I.; Bulusu, R.; Seddon, B.; Dangoor, A.; Wong, N.; Mudan, S. UK clinical practice guidelines for the management of gastrointestinal stromal tumours (GIST). Clin Sarcoma Res. 2017, 7, 6. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mitrovic-Jovanovic, M.; Djuric-Stefanovic, A.; Ebrahimi, K.; Dakovic, M.; Kovac, J.; Šarac, D.; Saponjski, D.; Jankovic, A.; Skrobic, O.; Sabljak, P.; et al. The Utility of Conventional CT, CT Perfusion and Quantitative Diffusion-Weighted Imaging in Predicting the Risk Level of Gastrointestinal Stromal Tumors of the Stomach: A Prospective Comparison of Classical CT Features, CT Perfusion Values, Apparent Diffusion Coefficient and Intravoxel Incoherent Motion-Derived Parameters. Diagnostics 2022, 12, 2841. [Google Scholar] [CrossRef] [PubMed]
- Peparini, N. Impact of tumour rupture risk on the oncological rationale for the surgical treatment choice of gastrointestinal stromal tumours. World J Gastrointest Surg. 2023, 15, 1559–1563. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Joensuu, H.; Reichardt, A.; Eriksson, M.; Hohenberger, P.; Boye, K.; Cameron, S.; Lindner, L.H.; Jost, P.J.; Bauer, S.; Schütte, J.; Lindskog, S.; Kallio, R.; Jaakkola, P.M.; Goplen, D.; Wardelmann, E.; Reichardt, P. Survival of patients with ruptured gastrointestinal stromal tumour treated with adjuvant imatinib in a randomised trial. Br J Cancer. 2024, 131, 299–304. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meneses, E.; Elkbuli, A.; Baroutjian, A.; McKenney, M.; Boneva, D. Perforated proximal jejunal gastrointestinal stromal tumor pT4N0M0 presenting with severe sepsis: A case report and literature review. Ann Med Surg (Lond). 2020, 57, 76–81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Asare, E.A.; Davis, C.H.; Chiang, Y.J.; Sabir, S.; Rajkot, N.F.; Phillips, P.R.; Roland, C.L.; Torres, K.E.; Hunt, K.K.; Feig, B.W. Management and outcomes of ruptured, perforated or fistulized tumors of mesenchymal origin. J Surg Oncol. 2020, 121, 474–479. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
 (1)
(1)