1. Introduction
Human respiratory syncytial virus (RSV) is the primary cause of lower respiratory tract infections, such as pneumonia and bronchiolitis, in children under two years old and the elderly. In younger populations, RSV infection leads to high hospitalization rates in infants and even healthy children without significant comorbidities, regardless of their baseline health conditions, resulting in elevated morbidity and mortality. Consequently, there is a pressing global demand for RSV vaccines, particularly to safeguard infants and elderly individuals [
1].
Growing evidence indicates that respiratory syncytial virus infections may be linked to neurological complications including meningoencephalitis, encephalopathy, seizures, and status epilepticus [
2]. The most prevalent pediatric neurological condition is febrile seizure, which is a serious health issue with both immediate and long-term consequences. It is characterized as a seizure occurrence that is accompanied by fever in a child who has never experienced an afebrile seizure, an infection or inflammation of the central nervous system (CNS), acute systemic metabolic abnormalities, or other acute symptomatic events [
3]. Central apnea, seizures, lethargy, altered swallowing, strabismus, hypotonia, and encephalopathy are the most common manifestations [
4]. Sometimes injury to the brain, especially at the hippocampus, cerebellum, brainstem, or other parts of the cerebral cortex may be related to various neurological symptoms [
5,
6]. Central apnea is the most prevalent neurologic manifestation (NM) among newborns infected with RSV, with reported rates varying from 1.2% to 23.8%, depending on the research sample. According to recent findings, children who get meningitis, pneumonia, or convulsions brought on by RSV have RNA material in their bodies [
7,
8]. Acute encephalopathy, sudden infant death syndrome, and Central Nervous System (CNS) symptoms like convulsions can all be linked to a Respiratory Syncytial Virus (RSV) infection in children [
9,
10].
Although recent systematic reviews have been published on the occurrence of Central Nervous System complications due to Respiratory Syncytial Virus [
2], to the best of our knowledge, there is a gap in the literature regarding a focused review of well-designed prospective clinical trials in younger populations. Therefore, the aim of this scoping review was to explore the literature for prospective clinical trials involving infants, children, and adolescents up to 17 years of age, specifically addressing neurological and cognitive complications associated with respiratory syncytial virus infection.
2. Materials and Methods
This scoping review was conducted according to the recommendations of the PRISMA-ScR checklist (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) [
11]. The neurologic and cognitive complications of the RSV disease represent the aim of the review. A comprehensive literature research was conducted to identify the available data from prospective clinical trials that correlate the virus with any neurological and/or cognitive symptoms. The protocol is registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (registration number: INPLASY202510017, DOI number 10.37766/inplasy2025.1.0017INPALSY).
2.1. Inclusion and Exclusion Criteria
Studies reporting results in infants, children and adolescents up to 17 years of age were considered eligible. Any neurological or cognitive outcome potentially associated with a positive RSV infection was considered as outcome of interest. Language and study type restrictions were applied, including only articles published in English and prospective clinical trials. Other types of trials were excluded, as well as reports referring to the peripheral and autonomic nervous system. Studies that did not report neurological or cognitive outcomes were excluded. No additional restrictions were applied.
2.2. Search Strategy
To identify relevant studies, MEDLINE (via PubMed), Scopus, the Cochrane Library, and PsycINFO were queried. The research was last updated on 26th November 2024. The search algorithm included a combination of the keywords and their synonyms which are presented in the supplementary materials.
2.3. Data Analysis and Synthesis
Articles not written in English were excluded to ensure linguistic consistency for analysis. Titles and abstracts were screened for relevance and a full-text control was applied for all potentially eligible studies by one individual author with confirmation by a second author. Duplicate articles were removed. Two studies described a common subset of the same patients and in this case the most recent study was included. Data from the included studies were extracted into a Microsoft Word document in the form of a table. All data on neurological or cognitive outcomes regardless of the initial reporting method in the included studies were extracted. Additionally, the number of participants and the population age distribution were outcomes of interest. A narrative synthesis of the data was then performed, describing the current knowledge derived from prospective trials in relation to the expression of respiratory syncytial virus in the central nervous system. The findings are presented in full in a tabular format.
3. Results
3.1. Results of the Literature Search
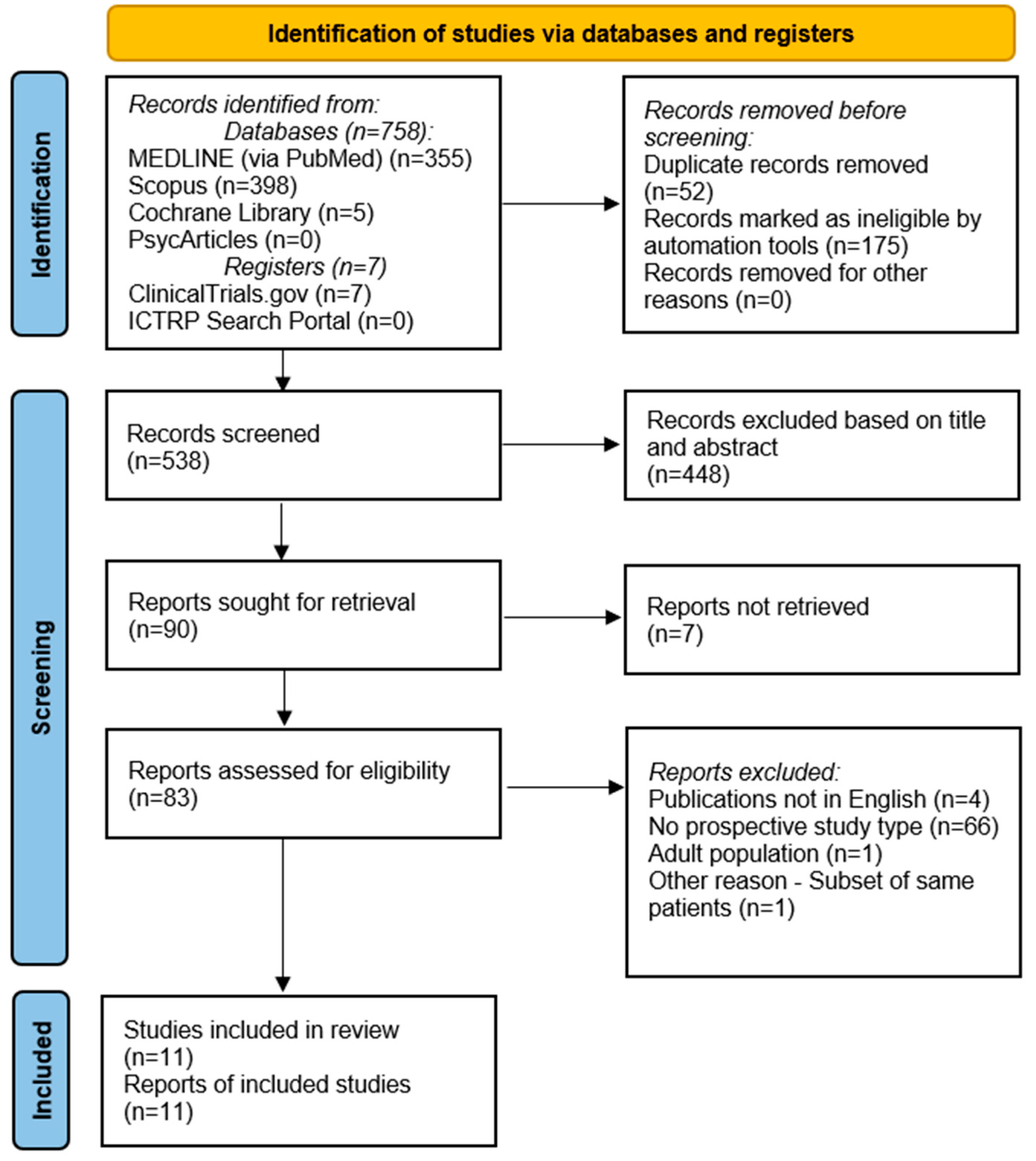
A total of 765 reports emerged from the initial search across the databases. After excluding duplicate records, ineligible records by automation tool in Scopus, and reports that did not meet the inclusion criteria, a final total number of 11 articles were analyzed in the review. The study selection process is depicted in the PRISMA flow diagram (
Figure 1). A summary of the included studies is presented in
Table 1.
The prospective study conducted by Savić et al. [
12] between November 2008 and March 2009 reported the clinical manifestations of RSV infection in children under 12 months of age. Fifteen out of 91 participants (16.5%) developed complications, including apnea, significant atelectasis and/or encephalopathy. The authors did not provide specific information regarding the clinical symptoms and signs associated with these complications.
Nygaard et al. [
13] researched clinical severity factors in RSV-positive children up to the age of 5 years during 2021-2022 RSV season and the pre-COVID-19 RSV seasons (2016-2020), differentiating outcomes for children with and without risk factors. The study design was divided in a retrospective analysis of the pre-COVID-19 seasons analysis and a prospective analysis of the 2021-2022 RSV season. The retrospective data of the study are not presented in the current review. According to the results, a total of 54 children required assisted ventilation support during the RSV period of 2021-2022. More than half of these children (n=35) were categorized as being at high-risk for severe RSV disease, while the remaining 19 children had no risk factors for severe disease. The reported rates of neurological complications among these children were 14% in the high-risk group, and 21% in the group without risk factors. Prolonged or complex febrile seizures were documented in 3 children (16%) in the group of participants without risk factors, while the corresponding rate in the high-risk group was 3 (9%). One child in each group developed acute encephalopathy/encephalitis (5% in the group without risk factors and 3% in the group with risk factors). In the high-risk group, one case (3%) of hyponatremia-related seizures was reported. Overall, a substantial percentage of patients required intubation and mechanical ventilation due to CNS complications with most cases occurring in patients without risk factors for severe disease.
The EFES multicenter study [
14], conducted between March 2016 and April 2017, enrolled 174 children 2 to 60 months who presented with febrile seizures. The majority of episodes (69.5%) were characterized as simple febrile seizures, with a recurrence rate of 41.4% for febrile seizures. Viral detection from nasopharyngeal samples was performed to identify potential viral causality. RSV was identified in 16% of the nasopharyngeal swabs. The RSV B strain was more common, with a prevalence of 9.7%, while the RSV A strain was identified in 6.25% of the nasopharyngeal swabs. Additionally, a higher prevalence of the RSV A strain was connected to simple febrile seizures, a finding characterized by statistical significance (p<0.05).
An additional prospective trial reported by Erez et al. [
15], conducted between 2011 and 2012, enrolled and analyzed 14 infants with RSV-positive infection and symptoms of central nervous system involvement. Most of the infants experienced central apneas, whereas 3 presented with encephalopathy. No evidence of RSV RNA positivity in the CSF samples was found. The authors emphasize that this finding does not support direct viral replication in the CNS, suggesting that further mechanisms should be investigated.
A total of 8 children up to 3 years old with confirmed RSV infection and CNS symptoms were investigated by Kawashima et al. [
16]. Six cases of excitotoxic encephalopathy, 1 case of hypoxic encephalopathy and 1 case of cytokine-storm encephalopathy were reported, with a variety of clinical presentations. Most patients experienced generalized convulsions, including one case following cardiopulmonary arrest. Additionally, cases of cerebellar ataxia, cyanosis followed by clonic seizures and a partial seizure were each reported in a single patient. Mental retardation was an outcome in 2 patients, and quadriplegia was reported in one patient.
Peña et al. [
17] investigated the impact of severe RSV infection on learning ability in 89 infants. Difficulties in acquiring native phonemes and communicating at 1 year of age were identified, with a statistically significant difference observed in the infants’ vocabulary and comprehension at 12 months. The authors highlight potential disorders with the process of linguistic development and the possibility of memory impairments.
In a long-term prospective clinical trial conducted between 2016 and 2022, reported by Jiang et al. [
18], the clinical manifestations of RSV infection were investigated. Eligible patients for this study were children and adolescents up to the age of 16 years. The data were presented separately for the pre-pandemic period and the COVID-19 period. A total number of 376 RSV-positive patients required ICU therapy between 2016 and 2020. In the pandemic year 2021, 66 patients were admitted to the ICU. Meningitis occurred at a rate of 1.1% in the pre-pandemic patients and 1.5% for the patients admitted within 2021. RSV infection was complicated by seizures in 1.1% of participants in the pre-pandemic period, with an increase of the rate by 3% in the 2021 cohort. Apnea as a complication was reported at a rate of 3.2% for the patients in the pre-pandemic period and 3% for the patients in 2021.
In the study by Pokorn et al. [
19], the RSV positivity rate among other viruses was tested in children under 6 years of age with febrile seizures, with healthy children as a control group. A statistically significant difference in RSV rates was observed between participants with febrile seizures and healthy controls. Specifically, the positive RSV nasopharyngeal samples within the patients with febrile seizures were detected at a rate of 10.9%, compared to 1.3% of healthy participants, with an age-adjusted odds ratio (OR) of 7.2. Additionally, the detection rate of the virus in patients with simple febrile seizures was 11.4%, and 10% in cases of complex febrile seizures.
Another prospective study, published by Tang et al. [
20], included children within the age spectrum of 6 months to 6 years with febrile seizures, enrolling participants between 2010 and 2011. The study results indicated that RSV was detected in 4.8% of patients with febrile seizures, compared to 17.8% in the control group, with statistical significance. Outcomes related to the seizures were reported for both the influenza and non-influenza groups of the study, but no additional specific information for RSV can be extracted from the results.
Wilkesmann et al. [
21] conducted a multicenter prospective study enrolling RSV-infected children over six seasons from 1999 until 2005. The participants were categorized into two groups: children with known neuromuscular impairments and those without. The group of participants with existing neuromuscular impairments experienced seizures at a statistically significant higher rate, with 15 out of 73 patients reporting seizures, compared to 2 cases of seizures among the 1,495 participants without preexisting neurological conditions.
The study by Hautala et al. [
22] included children 6 months to 6 years of age and assessed RSV incidence in two groups of patients: those with febrile seizures and those without. A total of 145 study participants tested positive for RSV. Among children aged 6 months to 3 years, RSV was detected in 6% for the patients presenting with febrile seizures and 8% for those without febrile seizures. In the age group of 3 years to 6 years, the rates were 11% and 8%, respectively. RSV was identified in 5% of the cases with simple febrile seizures, compared to a 10% incidence in cases of complex febrile seizures, with a relative risk of 1.56.
4. Discussion
This scoping review summarized the study characteristics reported in the reviewed literature for the neurologic and cognitive manifestations of the respiratory syncytial virus (RSV) disease through studies involving infants, children and adolescents up to 17 years of age. We identified a knowledge gap for studies of neurologic and cognitive manifestations in adolescents and in cognitive manifestations. Overall, neurologic and cognitive manifestations of the respiratory syncytial virus (RSV) disease studies had a greater emphasis on younger children under six years of age.
The results from this scoping literature review showed a notable gap in studies of adolescents. Only one study involved adolescents up to 16 years of age [
18]. Utilizing studies in adolescents would complement the knowledge regarding the effects of RSV on the neurological and cognitive state of children. For older patients, who are more likely than younger adults to be hospitalized from an RSV infection, this may be especially crucial [
23]. However, with respect to RSV, this review identified only one published study available on cognitive manifestations [
17]. There was a statistically significant difference in the infants' vocabulary and comprehension at 12 months, indicating that they had trouble learning local phonemes and communicating at 1 year of age. Attention is drawn to possible memory deficits and diseases related to the language development process.
The neurologic and cognitive manifestations of Respiratory Syncytial Virus (RSV) infection in children and adolescents represent a complex and multifaceted challenge in pediatric healthcare. RSV, a leading cause of acute respiratory infections, often leads to severe complications, particularly in younger populations. Manifestations such as febrile seizures, apnea, encephalopathy, and developmental delays highlight the virus's potential to impact the central nervous system (CNS) directly or indirectly. Early-life RSV infections frequently result in lower respiratory tract symptoms, conditions that are often associated with neurologic outcomes like seizures and altered consciousness [
12,
13]. Evidence suggests that mechanisms such as inflammation, cytokine responses, or hypoxia may underlie these neurologic effects, as findings regarding direct viral invasion of the CNS remain inconsistent [
15,
16].
4.1. Neurologic Manifestations
A range of studies have documented the neurologic complications linked to RSV. Savić et al. [
12] documented complications such as apnea and encephalopathy in 16.5% of infants under 12 months, underscoring the clinical challenges posed by severe RSV cases. Nygaard et al. [
13] reported febrile seizures and encephalopathy among children during the 2021-2022 RSV season, noting a significant prevalence of seizures even among children without predisposing risk factors. This unpredictability highlights RSV’s potential for severe neurologic consequences across diverse clinical profiles.
Studies such as Kawashima et al. [
16] and Wilkesmann et al. [
21] reported more severe neurologic outcomes, including excitotoxic and cytokine-storm encephalopathy, seizures, and even permanent disabilities like quadriplegia and mental retardation. Children with pre-existing neuromuscular impairments experienced significantly higher rates of seizures compared to their healthy counterparts [
21]. Similarly, Jiang et al. [
18] investigated long-term trends in RSV complications, observing a marked increase in neurologic symptoms during the COVID-19 pandemic compared to earlier years. The intersection of RSV dynamics and pandemic-altered healthcare likely exacerbated these neurologic outcomes.
4.2. Cognitive and Developmental Outcomes
Cognitive and developmental impacts of RSV were explored in fewer studies, but the findings remain critical. Peña et al. [
17] identified significant delays in language acquisition and phoneme recognition among infants with severe RSV infections. These results suggest that RSV may disrupt early neurodevelopmental processes, potentially resulting in long-term cognitive deficits. The cognitive dimension of RSV infection, although underexplored, aligns with concerns about broader neurodevelopmental sequelae and their implications for affected children’s academic and social trajectories.
4.3. Febrile Seizures
The association between RSV and febrile seizures was a recurring theme. The EFES study [
14] linked RSV infections with febrile seizures in children aged 2-60 months, identifying the RSV A strain as significantly associated with simple febrile seizures. Pokorn et al. [
19] similarly found higher rates of RSV detection among children presenting with febrile seizures compared to healthy controls, emphasizing the virus’s potential role in febrile seizure pathogenesis. Hautala et al. [
22] and Tang et al. [
20] provided additional evidence for this association, with results highlighting RSV’s role across both simple and complex febrile seizure cases. These findings reinforce the need for careful monitoring of febrile seizures as a potential marker of RSV complications.
4.4. Mechanistic Insights
The mechanism of RSV-induced neurologic manifestations remains a critical area of inquiry. Erez et al. [
15] found no RSV RNA in cerebrospinal fluid samples of infants with central apnea and encephalopathy, suggesting that inflammatory responses or cytokine-driven processes, rather than direct CNS invasion, may mediate these symptoms. This hypothesis is supported by the diverse presentations reported in studies like Kawashima et al. [
16], where cytokine-storm encephalopathy and hypoxic events were observed.
4.5. Limitations
The included studies are characterized by heterogenous design methods and reporting strategies, leading to variability in the reported results. A direct and robust synthesis of all the data is challenging since there are no common outcomes in most of the studies. An additional limitation is the lack of evidence observed in the field of CNS complications after RSV infection, specifically in relation to prospective data collection in patients. Relatively small sample sizes limit the generalizability of the results and complicate the interpretation of the relationship between the virus and potential neurological symptoms. Another limitation is a potential underestimation of the CNS involvement in mild RSV cases, since many studies focus on the complications in patients that needed ICU therapy. Cognitive and behavioral symptoms may be underreported at a significant grade, particularly because specific assessment tools were not used by individual studies, and the follow-up periods do not provide a long-term observation. A language bias may also be present, as only articles in English and German were considered eligible.
5. Conclusions
This scoping review explored the neurologic and cognitive manifestations of Respiratory Syncytial Virus (RSV) infection in children and adolescents, highlighting critical findings and identifying research gaps. The results reveal a broad spectrum of neurologic complications, including apnea, febrile seizures, and encephalopathy, which are particularly prevalent in children under six years of age. The review also uncovered limited evidence on cognitive manifestations, such as language delays and potential memory deficits, with only one study addressing these outcomes in depth. These findings align with the review’s objectives, offering insights into the complex interplay between RSV and central nervous system (CNS) involvement.
Neurological manifestations were frequently associated with severe RSV infections, with studies emphasizing the indirect pathogenic mechanisms underlying CNS complications, such as excitotoxicity and immune-mediated damage. The significant association of febrile seizures with RSV, particularly the RSV A strain, underscores the need for heightened clinical vigilance in diagnosing and managing affected children. However, the scarcity of studies addressing adolescents and long-term cognitive outcomes presents a challenge, highlighting the need for more inclusive research to fully understand the age-related effects of RSV.
5.1. Implications and Next Steps
The findings emphasize the importance of early detection and tailored management strategies for RSV-related neurologic and cognitive complications. For clinicians, this involves integrating advanced diagnostic tools, such as neuroimaging and CSF analysis, to better identify and manage CNS involvement. Public health initiatives should prioritize preventive measures, including the development and widespread implementation of RSV vaccines and targeted antiviral therapies, to mitigate severe complications.
Future research should address the identified gaps, focusing on: i. Expanding studies include adolescents and their unique responses to RSV infection. ii. Conducting longitudinal studies to assess long-term cognitive and developmental impacts. iii. Standardizing methodologies and outcome measures across studies to improve comparability and generalizability of findings.
This review underscores the need for collaborative, multidisciplinary efforts to bridge the knowledge gaps and improve outcomes for children affected by RSV. By advancing our understanding of RSV’s neurologic and cognitive effects, these steps will enhance clinical care and inform public health strategies to reduce the global burden of this common pediatric infection.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Document S1: Search Algorithm;.
Author Contributions
Conceptualization, A.S., X.T. and G.P.; methodology, A.S., X.T., and G.P.; formal analysis, A.S. and X.T.; data curation, A.S. and X.T.; writing—original draft preparation, A.S.; writing—review and editing, X.T. and G.P.; supervision, G.P.; project administration, A.S.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Topalidou, X.; Kalergis, A.M.; Papazisis, G. Respiratory Syncytial Virus Vaccines: A Review of the Candidates and the Approved Vaccines. Pathog. (Basel, Switzerland) 2023, 12. [CrossRef]
- Riccò, M.; Cascio, A.; Corrado, S.; Bottazzoli, M.; Marchesi, F.; Gili, R.; Giuri, P.G.; Gori, D.; Manzoni, P. Occurrence of Central Nervous System Complications of Respiratory Syncytial Virus Infections: A Systematic Review with Meta-Analysis. Epidemiol. (Basel, Switzerland) 2024, 5, 421–455. [CrossRef]
- Pavlidou, E.; Hagel, C.; Panteliadis, C. Febrile Seizures: Recent Developments and Unanswered Questions. Childs. Nerv. Syst. 2013, 29, 2011–2017. [CrossRef]
- Morichi, S.; Kawashima, H.; Ioi, H.; Yamanaka, G.; Kashiwagi, Y.; Hoshika, A.; Nakayama, T.; Watanabe, Y. Classification of Acute Encephalopathy in Respiratory Syncytial Virus Infection. J. Infect. Chemother. 2011, 17, 776–781. [CrossRef]
- Miyamoto, K.; Fujisawa, M.; Hozumi, H.; Tsuboi, T.; Kuwashima, S.; Hirao, J.; Sugita, K.; Arisaka, O. Systemic Inflammatory Response Syndrome and Prolonged Hypoperfusion Lesions in an Infant with Respiratory Syncytial Virus Encephalopathy. J. Infect. Chemother. 2013, 19, 978–982. [CrossRef]
- Park, A.; Suh, S.; Son, G.-R.; Lee, Y.H.; Seo, H.S.; Eun, B.-L.; Lee, N.-J.; Seol, H.-Y. Respiratory Syncytial Virus-Related Encephalitis: Magnetic Resonance Imaging Findings with Diffusion-Weighted Study. Neuroradiology 2014, 56, 163–168. [CrossRef]
- Brinkman, I.D.; de Wit, J.; Smits, G.P.; Ten Hulscher, H.I.; Jongerius, M.C.; Abreu, T.C.; van der Klis, F.R.M.; Hahné, S.J.M.; Koopmans, M.P.G.; Rots, N.Y.; et al. Early Measles Vaccination During an Outbreak in the Netherlands: Short-Term and Long-Term Decreases in Antibody Responses Among Children Vaccinated Before 12 Months of Age. J. Infect. Dis. 2019, 220, 594–602. [CrossRef]
- Shirota, G.; Morozumi, M.; Ubukata, K.; Shiro, H. [Infantile Meningitis Caused by Respiratory Syncytial Virus]. Kansenshogaku Zasshi. 2011, 85, 682–685. [CrossRef]
- Bajanowski, T.; Rolf, B.; Jorch, G.; Brinkmann, B. Detection of RNA Viruses in Sudden Infant Death (SID). Int. J. Legal Med. 2003, 117, 237–240. [CrossRef]
- Rambaud, C.; Guibert, M.; Briand, E.; Grangeot-Keros, L.; Coulomb-L’Herminé, A.; Dehan, M. Microbiology in Sudden Infant Death Syndrome (SIDS) and Other Childhood Deaths. FEMS Immunol. Med. Microbiol. 1999, 25, 59–66. [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [CrossRef]
- Savić, N.; Janković, B.; Minić, P.; Vasiljević, Z.; Sovtić, A.; Pejić, K.; Sarajlija, A.; Gazikalović, S. Clinical Characteristics of Respiratory Syncytial Virus Infection in Neonates and Young Infants. Vojnosanit. Pregl. 2011, 68, 220–224. [CrossRef]
- Nygaard, U.; Hartling, U.B.; Nielsen, J.; Vestergaard, L.S.; Dungu, K.H.S.; Nielsen, J.S.A.; Sellmer, A.; Matthesen, A.T.; Kristensen, K.; Holm, M. Hospital Admissions and Need for Mechanical Ventilation in Children with Respiratory Syncytial Virus before and during the COVID-19 Pandemic: A Danish Nationwide Cohort Study. Lancet. Child Adolesc. Heal. 2023, 7, 171–179. [CrossRef]
- Carman, K.B.; Calik, M.; Karal, Y.; Isikay, S.; Kocak, O.; Ozcelik, A.; Yazar, A.S.; Nuhoglu, C.; Sag, C.; Kilic, O.; et al. Viral Etiological Causes of Febrile Seizures for Respiratory Pathogens (EFES Study). Hum. Vaccin. Immunother. 2019, 15, 496–502. [CrossRef]
- Erez, D.L.; Yarden-Bilavsky, H.; Mendelson, E.; Yuhas, Y.; Ashkenazi, S.; Nahum, E.; Berent, E.; Hindiyeh, M.; Bilavsky, E. Apnea Induced by Respiratory Syncytial Virus Infection Is Not Associated with Viral Invasion of the Central Nervous System. Pediatr. Infect. Dis. J. 2014, 33, 880–881. [CrossRef]
- Kawashima, H.; Kashiwagi, Y.; Ioi, H.; Morichi, S.; Oana, S.; Yamanaka, G.; Takekuma, K.; Hoshika, A.; Sawai, J.; Kato, Y. Production of Chemokines in Respiratory Syncytial Virus Infection with Central Nervous System Manifestations. J. Infect. Chemother. 2012, 18, 827–831. [CrossRef]
- Peña, M.; Jara, C.; Flores, J.C.; Hoyos-Bachiloglu, R.; Iturriaga, C.; Medina, M.; Carcey, J.; Espinoza, J.; Bohmwald, K.; Kalergis, A.M.; et al. Severe Respiratory Disease Caused by Human Respiratory Syncytial Virus Impairs Language Learning during Early Infancy. Sci. Rep. 2020, 10, 22356. [CrossRef]
- Jiang, W.; Chen, S.; Lv, M.; Zhang, Z.; Wang, Z.; Shao, X.; Hua, S.; Hao, C.; Wang, Y. Are We Ready to Face the next Wave of RSV Surge after the COVID-19 Omicron Pandemic in China? Front. Cell. Infect. Microbiol. 2023, 13, 1216536. [CrossRef]
- Pokorn, M.; Jevšnik, M.; Petrovec, M.; Steyer, A.; Mrvič, T.; Grosek, Š.; Lusa, L.; Strle, F. Respiratory and Enteric Virus Detection in Children. J. Child Neurol. 2017, 32, 84–93. [CrossRef]
- Tang, J.; Yan, W.; Li, Y.; Zhang, B.; Gu, Q. Relationship between Common Viral Upper Respiratory Tract Infections and Febrile Seizures in Children from Suzhou, China. J. Child Neurol. 2014, 29, 1327–1332. [CrossRef]
- Wilkesmann, A.; Ammann, R.A.; Schildgen, O.; Eis-Hübinger, A.M.; Müller, A.; Seidenberg, J.; Stephan, V.; Rieger, C.; Herting, E.; Wygold, T.; et al. Hospitalized Children with Respiratory Syncytial Virus Infection and Neuromuscular Impairment Face an Increased Risk of a Complicated Course. Pediatr. Infect. Dis. J. 2007, 26, 485–491. [CrossRef]
- Hautala, M.; Arvila, J.; Pokka, T.; Mikkonen, K.; Koskela, U.; Helander, H.; Glumoff, V.; Rantala, H.; Tapiainen, T. Respiratory Viruses and Febrile Response in Children with Febrile Seizures: A Cohort Study and Embedded Case-Control Study. Seizure 2021, 84, 69–77. [CrossRef]
- Watson, A.; Wilkinson, T.M.A. Respiratory Viral Infections in the Elderly. Ther. Adv. Respir. Dis. 2021, 15, 1753466621995050. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).